Numerical Modeling of a New Type of Prosthetic Restoration for Non-Carious Cervical Lesions
Abstract
:1. Introduction
1.1. Research Objectives
- -
- the creation of parametrized models of teeth with and without the NCCL;
- -
- the creation of parametrized models with the restoration of the NCCL in the form of a new prosthetic inlay;
- -
- the implementation of a series of numerical experiments on strain of the tooth before and after restoration;
- -
- the analysis of the impact of prosthetic inlay materials on strained teeth.
1.2. Problem Context
1.3. Problem Description
- -
- polymerization shrinkage;
- -
- dependence on the manual skills of a particular specialist;
- -
- short service life;
- -
- pigmentation;
- -
- the inability to ensure reconstruction of the periodontal attachment between the artificial material and the gum.
2. Materials and Methods
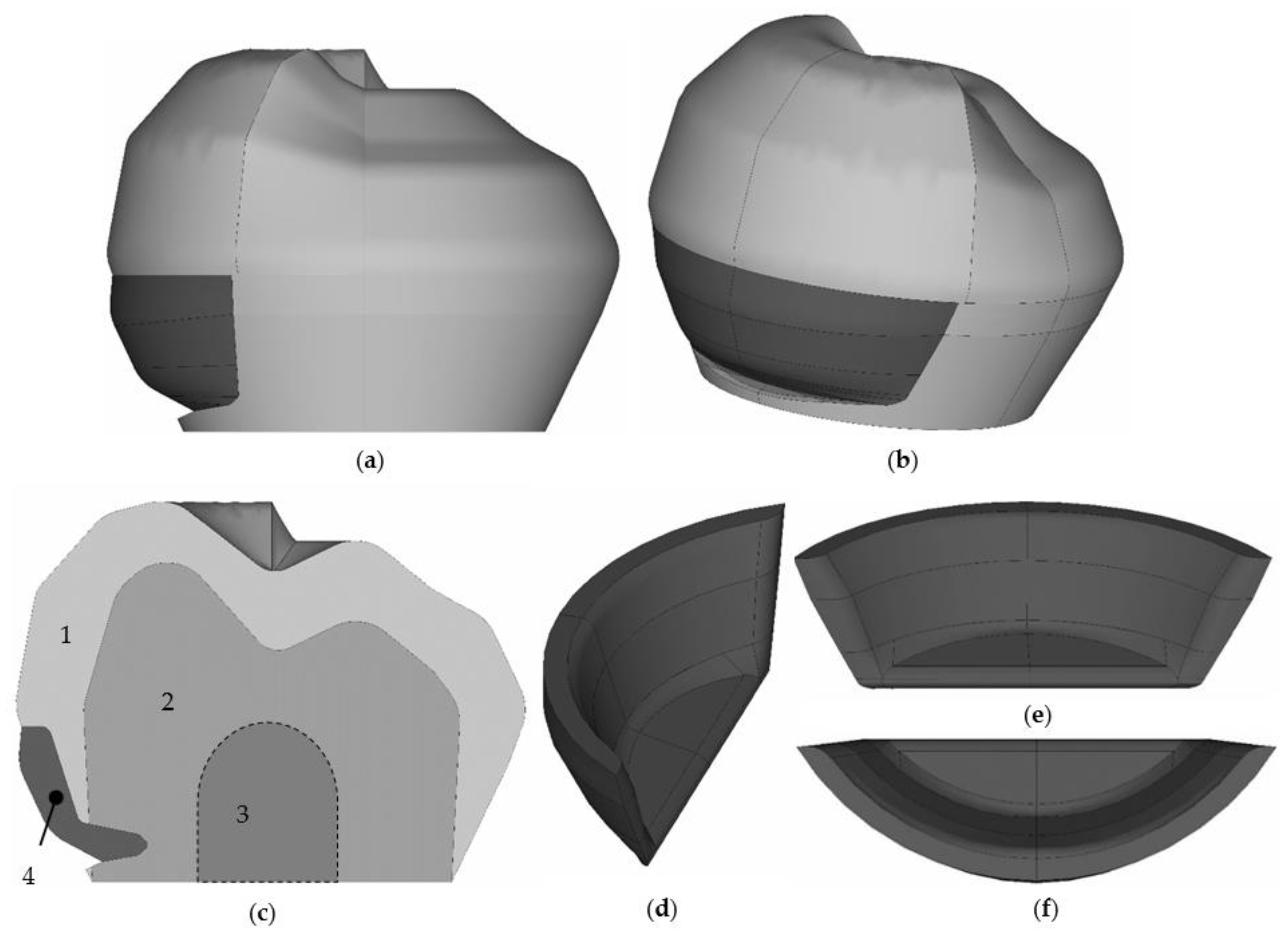
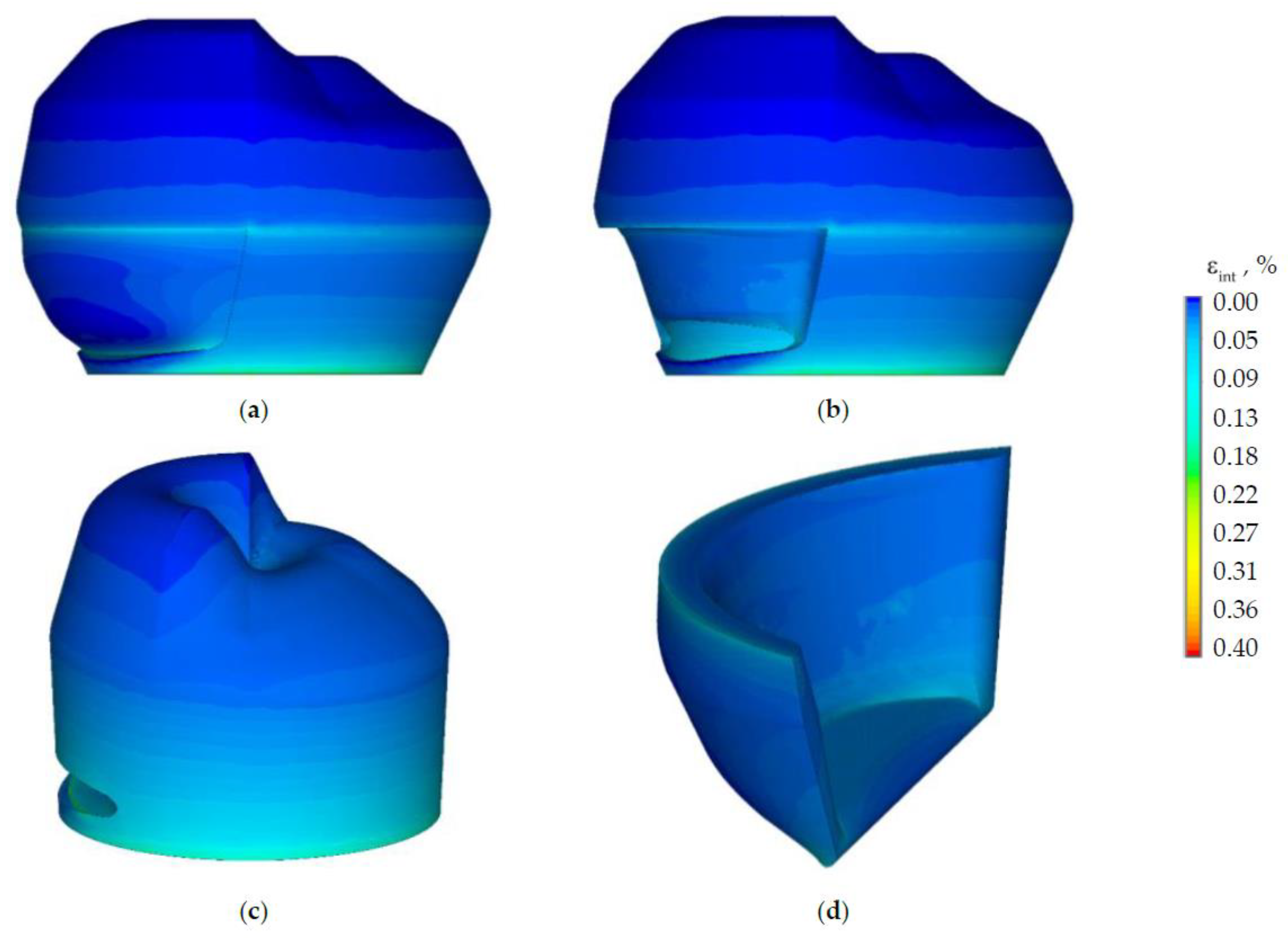
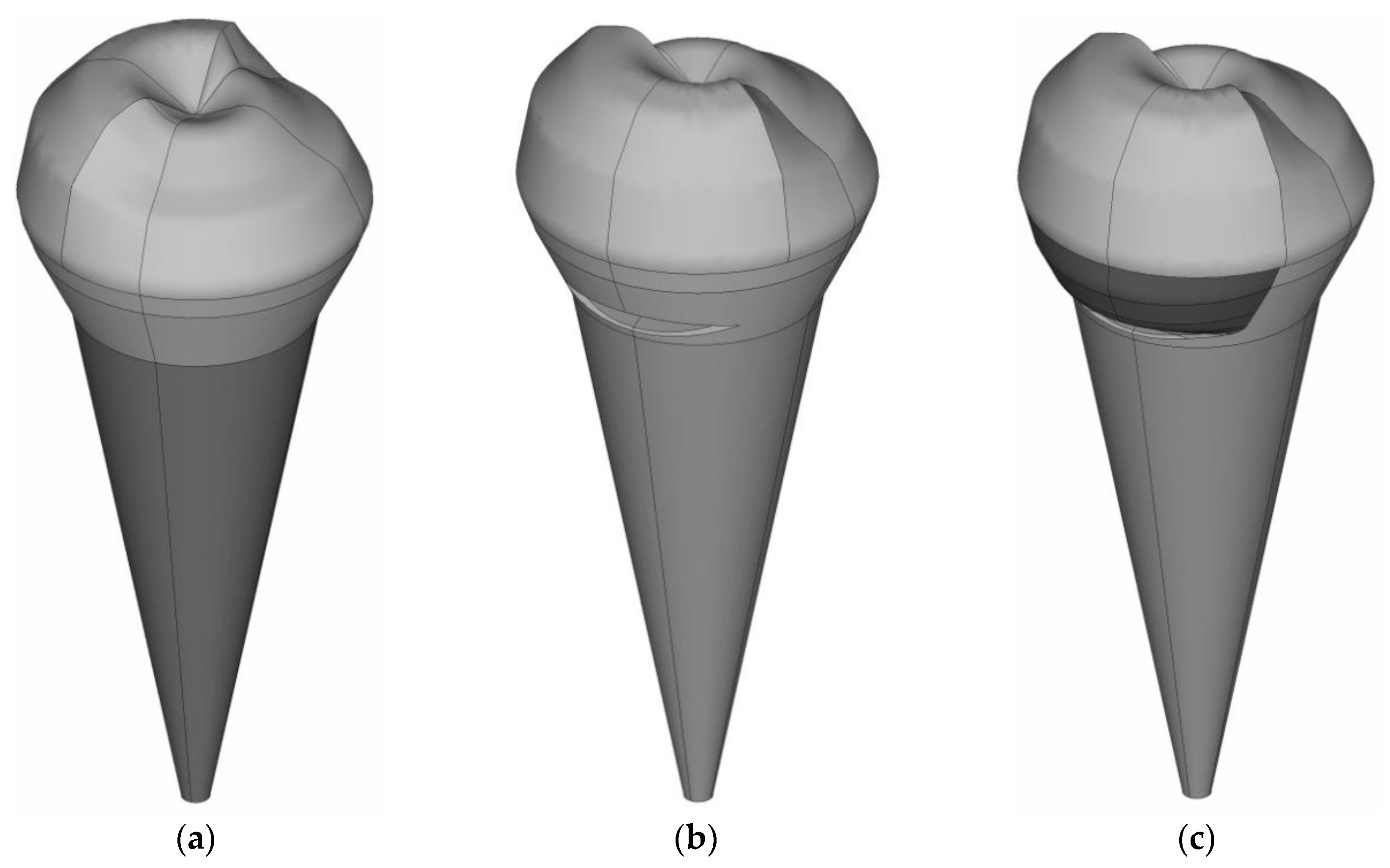
2.1. Model
- -
- is to create a gingival fold;
- -
- is to create the main cavity;
- -
- is to create an additional retention point with an additional platform at the top of the cavity for fixing the veneer part of the inlay.
- -
- roots and gingiva are not taken into account in the model to save computational resources and a detailed study of the tooth-inlay contact zone;
- -
- only the vertical load from the antagonist tooth in a wide range is considered;
- -
- only the case of complete adhesion of the inlay and tooth is considered, although in reality sliding is possible;
- -
- the elastic deformation behavior of materials is considered at this stage. It is planned to study the effect of heat shrinkage on the stress state of the biomechanical unit and refine the behavior model of the system materials in the future;
- -
- the degradation of materials is not taken into account, as well as the formation of cracks due to the complexity of such mechanical models.
2.2. Mechanical Properties of the Mouthguard Components
2.3. Numerical Finite Element (FE) Solution and Convergence
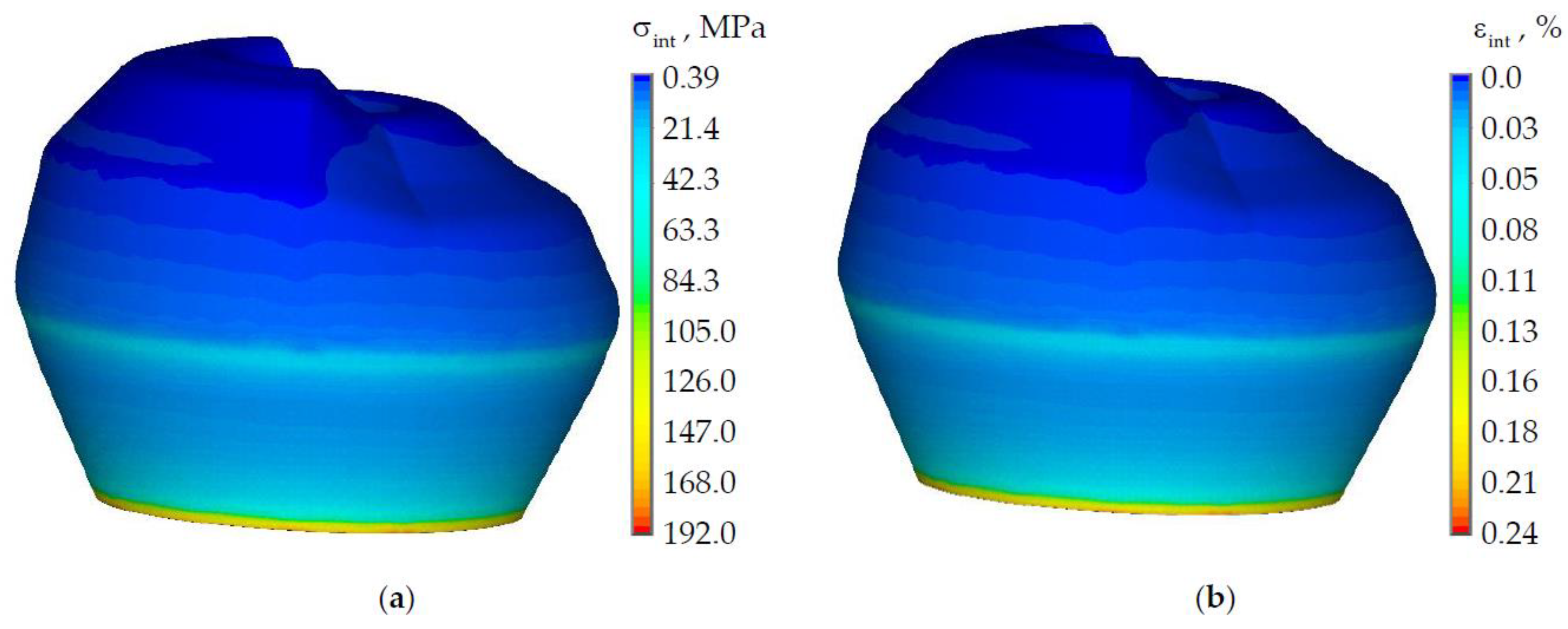
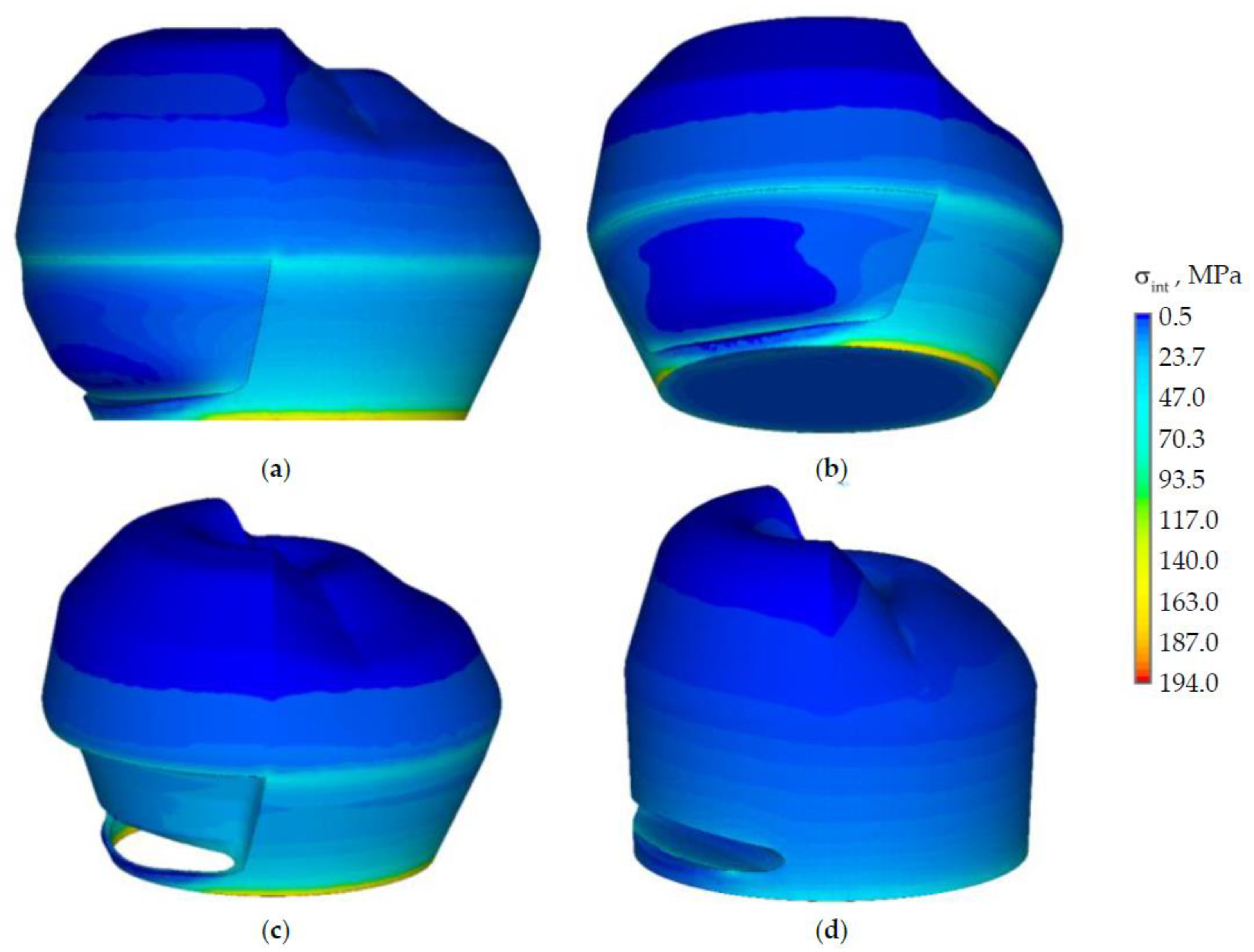
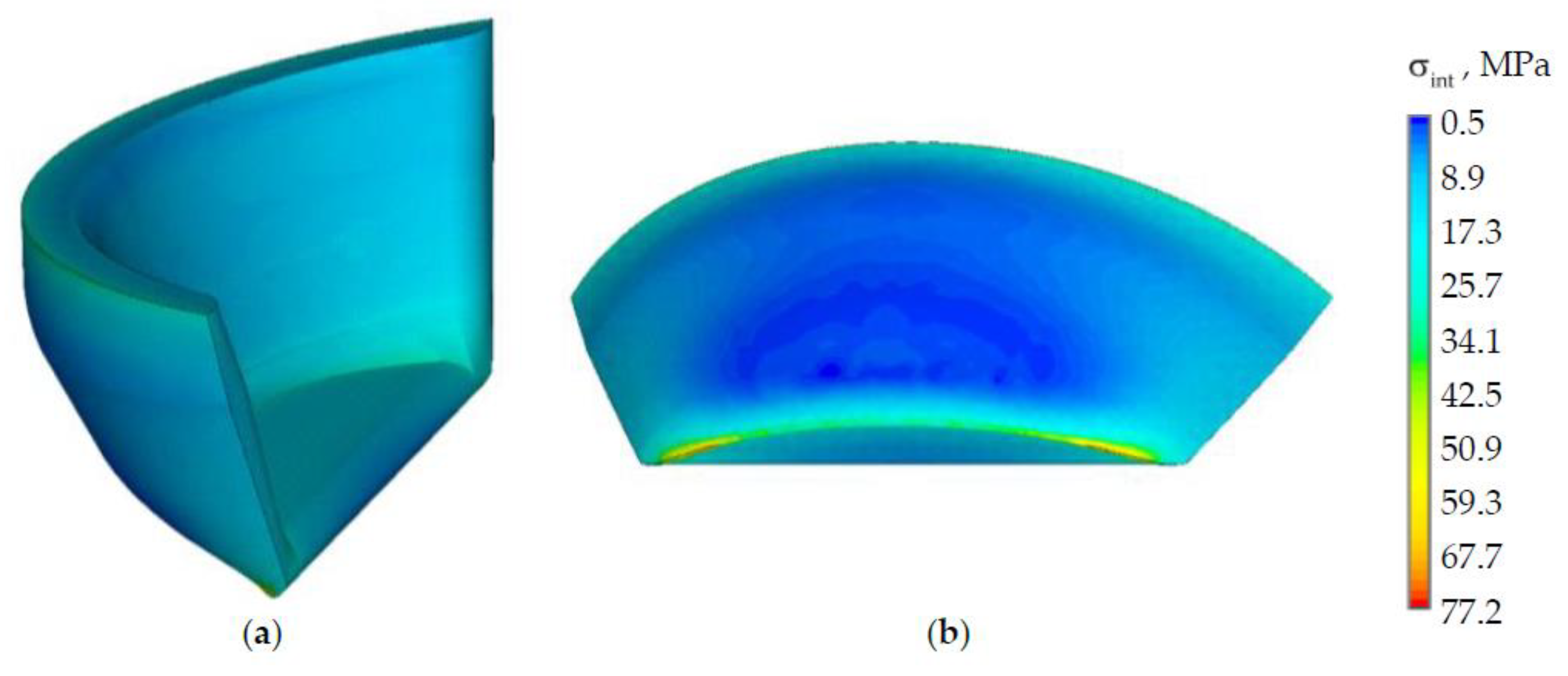
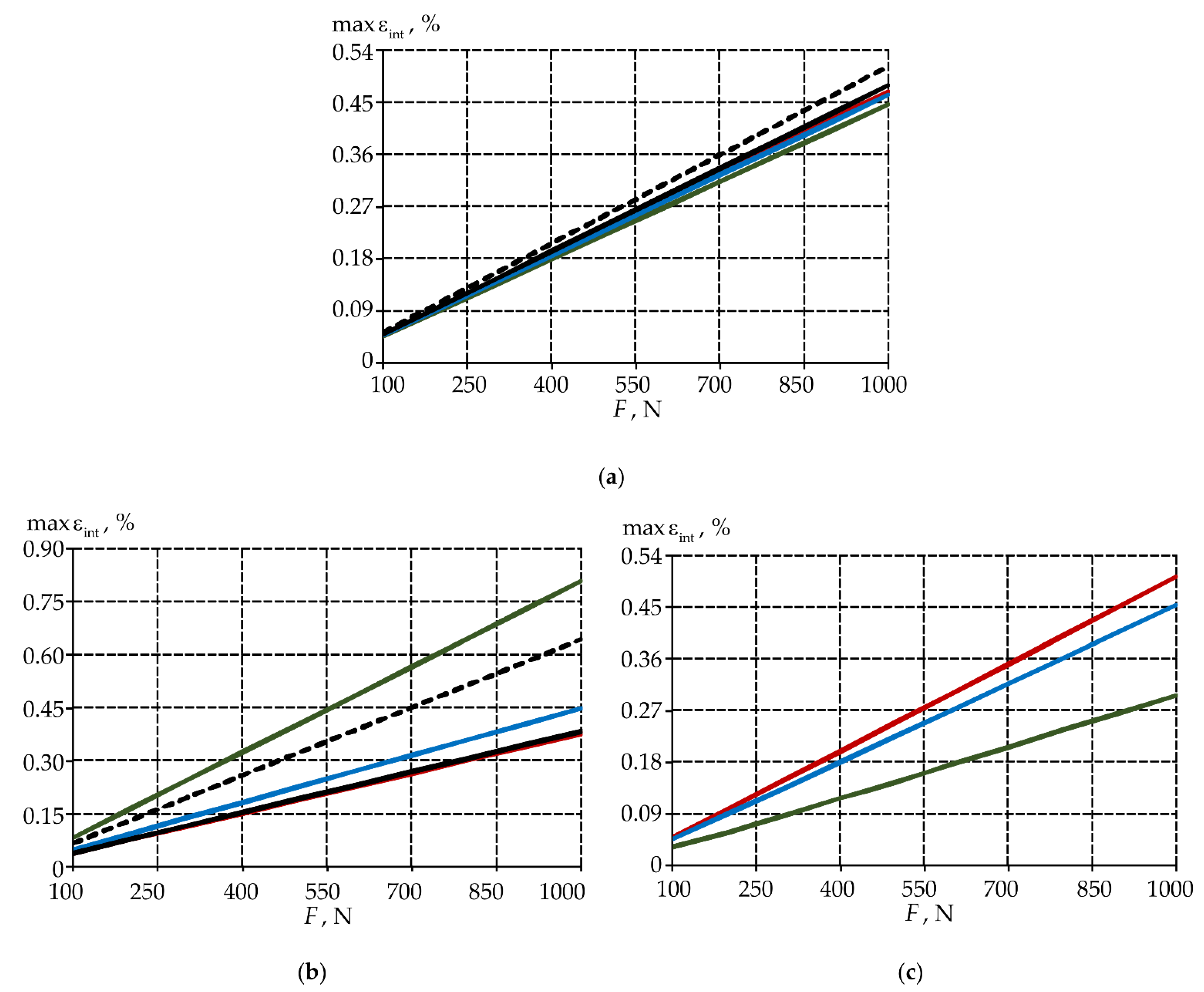
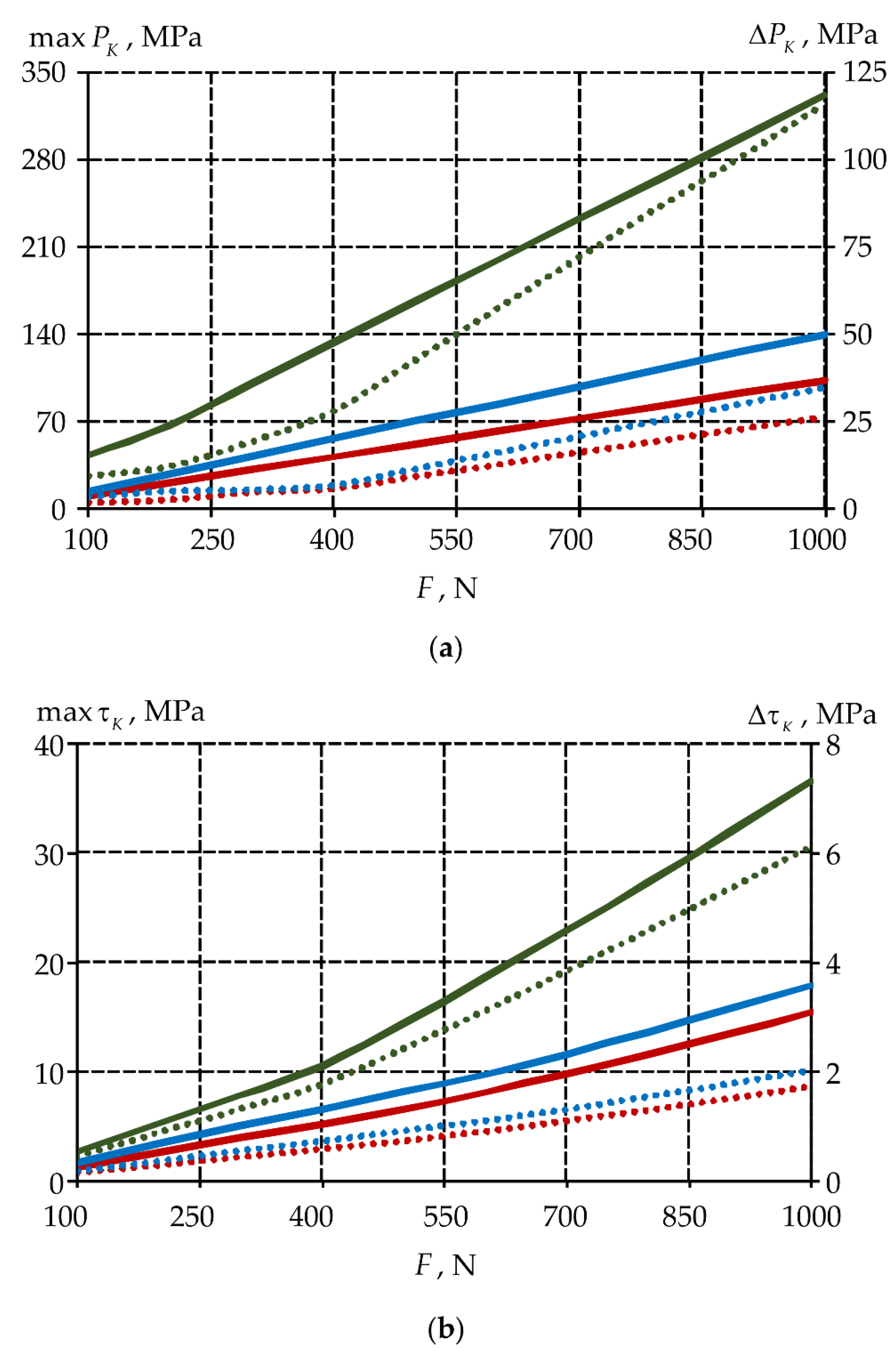
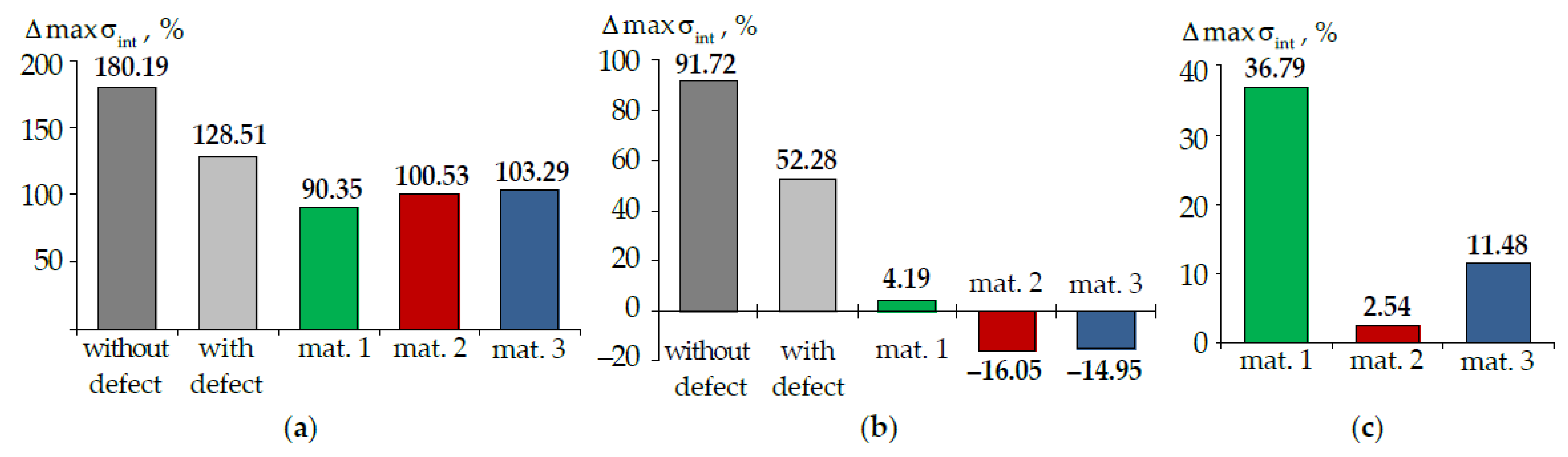
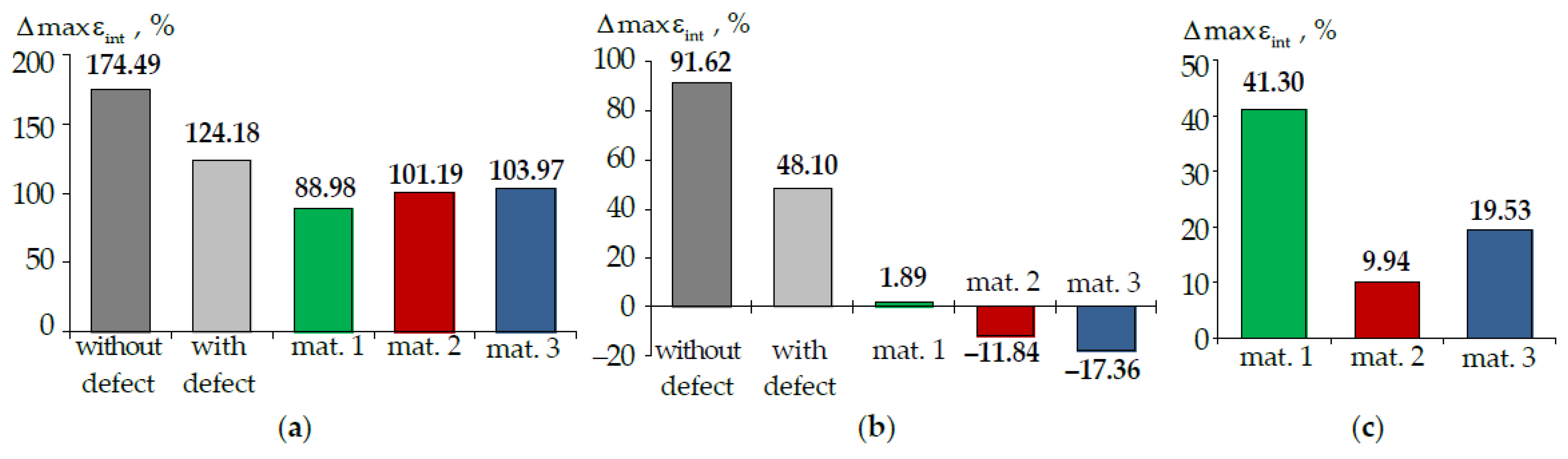
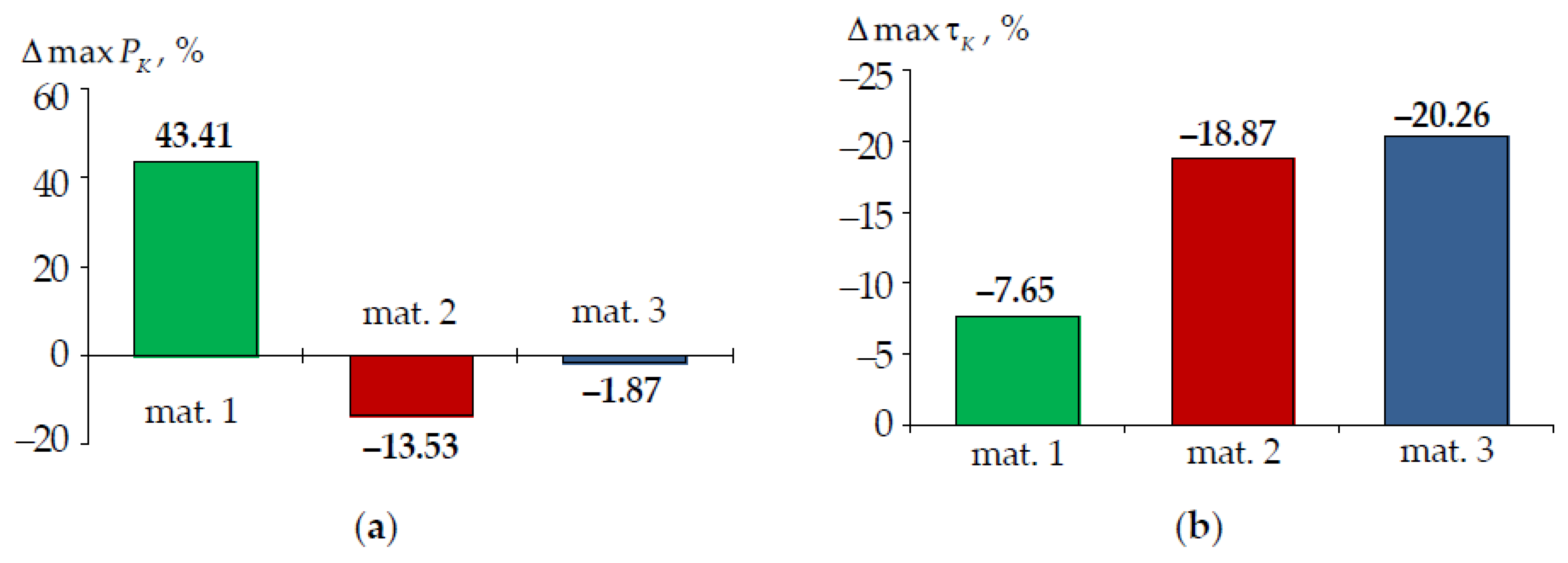
3. Results
4. Discussion
4.1. Limitation Statement
- -
- tooth root system in the model is discarded;
- -
- interaction with gums is not taken into account;
- -
- dental pulp is not modeled;
- -
- enamel and dentin are deformed together;
- -
- contact interaction is modeled as a complete adhesion of mating surfaces.
- -
- the behavior is described as isotropic elastic;
- -
- materials shrinkage is not taken into account.
- -
- the refinement of design schemes and finite element modeling of a biomechanical assembly;
- -
- the analysis of the effect of the polymerization shrinkage of restorative composites on the total deformation of the tooth;
- -
- the analysis of the influence of the cavity geometry for the prosthetic inlay in the NCCL;
- -
- the analysis of the influence of materials for the restoration of an NCCL with different tooth configurations and cavities according to the prosthetic design;
- -
- the analysis of the influence of loads from the antagonist tooth acting at an angle to the biomechanical system;
- -
- the analysis of the influence of the nature of the tooth elements conjugation and the tooth-inlay system.
4.2. Materials
4.3. Influence of Taking into Account the Root System on the Tooth Deformation
4.4. Main Results
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Olesova, V.N.; Ivanov, A.S.; Olesov, E.E.; Romanov, A.S.; Zaslavskiy, R.S. Biomechanical comparison of ceramic, titanium and chrome cobalt post inlays in post-traumatic dental defects repair. Disaster Med. 2022, 1, 53–58. [Google Scholar] [CrossRef]
- Krupnin, A.E.; Kharakh, Y.N.; Gribov, D.A.; Arutyunov, S.D. Biomechanical analysis of new constructions of adhesive bridge prostheses. Russ. J. Biomech. 2019, 23, 423–434. [Google Scholar] [CrossRef]
- Ichim, I.P.; Schmidlin, P.R.; Li, Q.; Kieser, J.A.; Swain, M.V. Restoration of non-carious cervical lesions: Part II. Restorative material selection to minimise fracture. Dent. Mater. 2007, 23, 1562–1569. [Google Scholar] [CrossRef]
- Dikova, T.; Vasilev, T.; Hristova, V.; Panov, V. Finite element analysis of V-shaped tooth defects filled with universal nanohybrid composite using incremental technique. J. Mech. Behav. Biomed. Mater. 2021, 118, 104425. [Google Scholar] [CrossRef]
- Ceruti, P.; Menicucci, G.; Mariani, G.; Pittoni, D.; Gassino, G. Non carious cervical lesions. A review. Minerva Stomatol. 2006, 55, 43–57. [Google Scholar]
- Sarode, G.; Sarode, S. Abfraction: A review. J. Oral Maxillofac. Pathol. 2013, 17, 222–227. [Google Scholar] [CrossRef]
- Elmarakby, A.; Sabri, F.; Alharbi, S.; Halawani, S. Noncarious Cervical Lesions as Abfraction: Etiology, Diagnosis, and Treatment Modalities of Lesions: A Review Article. Dentistry 2017, 7, 1000438. [Google Scholar] [CrossRef]
- Noda, N.-A.; Chen, K.-K.; Tajima, K.; Takase, Y.; Yamaguchi, K.; Nagano, H. Intensity of Singular Stress Field due to Wedge-Shaped Defect in Human Tooth after Restored with Composite Resins. Trans. Jpn. Soc. Mech. Eng. Part A 2009, 75, 1209–1216. [Google Scholar] [CrossRef]
- Jakupović, S.; Anić, I.; Ajanović, M.; Korać, S.; Konjhodžić, A.; Džanković, A.; Vuković, A. Biomechanics of cervical tooth region and noncarious cervical lesions of different morphology; three-dimensional finite element analysis. Eur. J. Dent. 2016, 10, 413–418. [Google Scholar] [CrossRef]
- Soares, P.V.; Souza, L.V.; Veríssimo, C.; Zeola, L.F.; Pereira, A.G.; Santos-Filho, P.C.; Fernandes-Neto, A.J. Effect of root morphology on biomechanical behaviour of premolars associated with abfraction lesions and different loading types. J. Oral Rehabil. 2014, 41, 108–114. [Google Scholar] [CrossRef]
- Srirekha, A.; Bashetty, K. A comparative analysis of restorative materials used in abfraction lesions in tooth with and without occlusal restoration: Three-dimensional finite element analysis. J. Conserv. Dent. 2013, 16, 157–161. [Google Scholar] [CrossRef] [Green Version]
- Vandana, K.L.; Deepti, M.; Shaimaa, M.; Naveen, K.; Rajendra, D. A finite element study to determine the occurrence of abfraction and displacement due to various occlusal forces and with different alveolar bone height. J. Indian Soc. Periodontol. 2016, 20, 12–16. [Google Scholar] [CrossRef]
- Rees, J.S.; Hammadeh, M.; Jagger, D.C. Abfraction lesion formation in maxillary incisors, canines and premolars: A finite element study. Eur. J. Oral Sci. 2003, 111, 149–154. [Google Scholar] [CrossRef]
- Du, J.K.; Wu, J.H.; Chen, P.H.; Ho, P.S.; Chen, K.K. Influence of cavity depth and restoration of non-carious cervical root lesions on strain distribution from various loading sites. BMC Oral Health 2020, 20, 98. [Google Scholar] [CrossRef]
- Jakupovic, S.; Cerjakovic, E.; Topcic, A.; Ajanovic, M.; Prcic, A.K.; Vukovic, A. Analysis of the abfraction lesions formation mechanism by the finite element method. Acta Inform. Med. 2014, 22, 241–245. [Google Scholar] [CrossRef] [Green Version]
- Haralur, S.B.; Alqahtani, A.S.; AlMazni, M.S.; Alqahtani, M.K. Association of non-carious cervical lesions with oral hygiene habits and dynamic occlusal parameters. Diagnostics 2019, 9, 43. [Google Scholar] [CrossRef] [Green Version]
- Romeed, S.A.; Malik, R.; Dunne, S.M. Stress analysis of occlusal forces in canine teeth and their role in the development of non-carious cervical lesions: Abfraction. Int. J. Dent. 2012, 2012, 234845. [Google Scholar] [CrossRef]
- Ahmić Vuković, A.; Jakupović, S.; Zukić, S.; Bajsman, A.; Gavranović Glamoč, A.; Šečić, S. Occlusal stress distribution on the mandibular first premolar—FEM analysis. Acta Med. Acad. 2019, 48, 255–261. [Google Scholar] [CrossRef] [Green Version]
- Rogozhnikov, G.I.; Nemenatov, I.G.; Astashina, N.B.; Shulyatnikova, O.A.; Rogozhnikov, A.G.; Olshanskii, E.V. Orthopedic treatment of patients with clinoid defects of premolars and molars hard tissues. Actual Probl. Dent. 2010, 3, 24–27. [Google Scholar]
- Zeola, L.F.; Pereira, F.A.; Machado, A.C.; Reis, B.R.; Kaidonis, J.; Xie, Z.; Townsend, G.C.; Ranjitkar, S.; Soares, P.V. Effects of non-carious cervical lesion size, occlusal loading and restoration on biomechanical behaviour of premolar teeth. Aust. Dent. J. 2016, 61, 408–417. [Google Scholar] [CrossRef] [Green Version]
- Meredith, N.; Sherriff, M.; Setchell, D.J.; Swanson, S.A.V. Measurement of the microhardness and Young’s modulus of human enamel and dentine using an indentation technique. Arch. Oral Biol. 1996, 41, 539–545. [Google Scholar] [CrossRef]
- Benazzi, S.; Grosse, I.R.; Gruppioni, G.; Weber, G.W.; Kullmer, O. Comparison of occlusal loading conditions in a lower second premolar using three-dimensional finite element analysis. Clin. Oral Investig. 2014, 18, 369–375. [Google Scholar] [CrossRef]
- Lee, H.E.; Lin, C.L.; Wang, C.H.; Cheng, C.H.; Chang, C.H. Stresses at the cervical lesion of maxillary premolar—A finite element investigation. J. Dent. 2002, 30, 283–290. [Google Scholar] [CrossRef]
- Grippo, J.O.; Masai, J.V. Role of biodental engineering factors (BEF) in the etiology of root caries. J. Esthet. Dent. 1991, 3, 71–76. [Google Scholar] [CrossRef]
- Leal, N.M.S.; Silva, J.L.; Benigno, M.I.M.; Bemerguy, E.A.; Meira, J.B.C.; Ballester, R.Y. How mechanical stresses modulate enamel demineralization in non-carious cervical lesions? J. Mech. Behav. Biomed. Mater. 2017, 66, 50–57. [Google Scholar] [CrossRef]
- Xhonga, F.A. Bruxism and its effect on the teeth. J. Oral Rehabil. 1977, 4, 65–76. [Google Scholar] [CrossRef]
- Telles, D.; Pegoraro, L.F.; Pereira, J.C. Prevalence of noncarious cervicai lesions and their relation to occiusal aspects: A clinical study. J. Esthet. Restor. Dent. 2000, 12, 10–15. [Google Scholar] [CrossRef]
- Geramy, A.; Sharafoddin, F. Abfraction: 3D analysis by means of the finite element method. Quintessence Int. 2003, 34, 526–533. [Google Scholar]
- Vasudeva, G.; Bogra, P. The effect of occlusal restoration and loading on the development of abfraction lesions: A finite element study. J. Conserv. Dent. 2008, 11, 117–120. [Google Scholar] [CrossRef]
- Dikova, T.; Vasilev, T.; Hristova, V.; Panov, V. Finite Element Analysis in Setting of Fillings of V-Shaped Tooth Defects Made with Glass-Ionomer Cement and Flowable Composite. Processes 2020, 8, 363. [Google Scholar] [CrossRef] [Green Version]
- Beresescu, G.; Ormenisan, A.; Raluca Monica, C.; Veliscu, A.; Manea, M.; Ion, R. FEM Analysis of Stress in Non-carious Cervical Lesion Restoration with Four Different Restorative Materials. Mater. Plast. 2018, 55, 42–45. [Google Scholar] [CrossRef]
- Czerwiński, M.; Żmudzki, J.; Kwieciński, K.; Kowalczyk, M. Finite element analysis of the impact of the properties of dental wedge materials on functional features. Arch. Mater. Sci. Eng. 2021, 112/1, 32–41. [Google Scholar] [CrossRef]
- Ichim, I.; Li, Q.; Loughran, J.; Swain, M.; Kieser, J. Restoration of non-carious cervical lesions. Part, I. Modelling of restorative fracture. Dent. Mater. 2007, 23, 1553–1561. [Google Scholar] [CrossRef]
- Brailko, N.N.; Tkachenko, I.M.; Kovalenko, V.V.; Lemeshko, A.V.; Fenko, A.G.; Kozak, R.V.; Kalashnikov, D.V. Investigation of stress-strain state of “restoration & tooth” system in wedge-shaped defects by computed modeling method. Wiadomości Lek. 2021, 74, 2112–2117. [Google Scholar]
- Kichenko, A.A.; Kiryukhin, V.Y.; Rogozhnikov, G.I.; Neminatov, I.G.; Astashina, N.B.; Shulyatnikova, O.A. Finite element analysis of wedge-shaped defect restoration at the first molar of a patient. Russ. J. Biomech. 2008, 2, 80–96. [Google Scholar]
- Kasuya, A.V.B.; Favarão, I.N.; Machado, A.C.; Spini, P.H.R.; Soares, P.V.; Fonseca, R.B. Development of a fiber-reinforced material for fiber posts: Evaluation of stress distribution, fracture load, and failure mode of restored roots. J. Prosthet. Dent. 2020, 123, 829–838. [Google Scholar] [CrossRef]
- Tajima, K.; Chen, K.K.; Takahashi, N.; Noda, N.; Nagamatsu, Y.; Kakigawa, H. Three-dimensional finite element modeling from CT images of tooth and its validation. Dent. Mater. J. 2009, 28, 219–226. [Google Scholar] [CrossRef] [Green Version]
- Magne, P.; Oganesyan, T. CT scan-based finite element analysis of premolar cuspal deflection following operative procedures. Int. J. Periodontics Restor. Dent. 2009, 29, 361–369. [Google Scholar]
- Shimada, Y.; Yoshiyama, M.; Tagami, J.; Sumi, Y. Evaluation of dental caries, tooth crack, and age-related changes in tooth structure using optical coherence tomography. Jpn. Dent. Sci. Rev. 2020, 56, 109–118. [Google Scholar] [CrossRef]
- Sarycheva, I.; Yanushevich, O.; Minakov, D. Diagnostics of non-carious lesions of dental hard tissues with the methods of optical spectroscopy and radiography. Braz. Dent. Sci. 2020, 23, 1–8. [Google Scholar] [CrossRef]
- Aw, T.C.; Lepe, X.; Johnson, G.H.; Mancl, L. Characteristics of noncarious cervical lesions: A clinical investigation. J. Am. Dent. Assoc. 2002, 133, 725–733. [Google Scholar] [CrossRef]
- Mercu, V.; Popescu, Ţ.S.M.; Scrieciu, M.; Amărăscu, M.O.; Vătu, M.; Diaconu, O.A.; Osiac, E.; Ghelase, Ş.M. Optical coherence tomography applications in tooth wear diagnosis. Rom. J. Morphol. Embryol. 2017, 58, 99–106. [Google Scholar]
- Abdalla, R.; Mitchell, R.J.; Ren, Y. Non-carious cervical lesions imaged by focus variation microscopy. J. Dent. 2017, 63, 14–20. [Google Scholar] [CrossRef]
- Karan, K.; Yao, X.; Xu, C.; Wang, Y. Chemical profile of the dentin substrate in non-carious cervical lesions. Dent. Mater. 2009, 25, 1205–1212. [Google Scholar] [CrossRef] [Green Version]
- Sakoolnamarka, R.; Burrow, M.F.; Prawer, S.; Tyas, M.J. Raman spectroscopic study of noncarious cervical lesions. Odontology 2005, 93, 35–40. [Google Scholar] [CrossRef]
- Kantardzić, I.; Vasiljević, D.; Blazić, L.; Luzanin, O. Influence of cavity design preparation on stress values in maxillary premolar: A finite element analysis. Croat. Med. J. 2012, 53, 568–576. [Google Scholar] [CrossRef] [Green Version]
- Babaei, B.; Cella, S.; Farrar, P.; Prentice, L.; Prusty, B.G. The influence of dental restoration depth, internal cavity angle, and material properties on biomechanical resistance of a treated molar tooth. J. Mech. Behav. Biomed. Mater. 2022, 133, 105305. [Google Scholar] [CrossRef]
- CEREC Blocs—For CEREC/InLab: Operating Instructions; Imprime en Allemagne: Bensheim, Germany, 2006.
- Hussein, L.A. 3-D finite element analysis of different composite resin MOD inlays. Am. J. Sci. 2013, 9, 422–428. [Google Scholar]
- Oneț, D.B.; Tudoran, L.B.; Delean, A.G.; Șurlin, P.; Ciurea, A.; Roman, A.; Bolboacă, S.D.; Gasparik, C.; Muntean, A.; Soancă, A. Adhesion of flowable resin composites in simulated wedge-shaped cervical lesions: An in vitro pilot study. Appl. Sci. 2021, 11, 3173. [Google Scholar] [CrossRef]
- Battancs, E.; Fráter, M.; Sáry, T.; Gál, E.; Braunitzer, G.; Szabó, P.B.; Garoushi, S. Fracture behavior and integrity of different direct restorative materials to restore noncarious cervical lesions. Polymers 2021, 13, 4170. [Google Scholar] [CrossRef]
- MacHado, A.C.; Soares, C.J.; Reis, B.R.; Bicalho, A.A.; Raposo, L.H.A.; Soares, P.V. Stress-strain analysis of premolars with non-carious cervical lesions: Influence of restorative material, loading direction and mechanical fatigue. Oper. Dent. 2017, 42, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Siegel, S. The Dental Reference Manual: A Daily Guide for Students and Practitioners; Springer: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Tamimi, F.; Hirayama, H. Digital Restorative Dentistry A Guide to Materials, Equipment, and Clinical Procedures: A Guide to Materials, Equipment, and Clinical Procedures; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Colombo, M.; Gallo, S.; Padovan, S.; Chiesa, M.; Poggio, C.; Scribante, A. Influence of different surface pretreatments on shear bond strength of an adhesive resin cement to various zirconia ceramics. Materials 2020, 13, 652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tatullo, M.; Codispoti, B.; Paduano, F.; Nuzzolese, M.; Makeeva, I. Strategic tools in regenerative and translational dentistry. Int. J. Mol. Sci. 2019, 20, 1879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukherjee, K.; Visakan, G.; Phark, J.H.; Moradian-Oldak, J. Enhancing collagen mineralization with amelogenin peptide: Towards the restoration of dentin. ACS Biomater. Sci. Eng. 2020, 6, 2251–2262. [Google Scholar] [CrossRef] [PubMed]
- Tatullo, M.; Genovese, F.; Aiello, E.; Amantea, M.; Makeeva, I.; Zavan, B.; Rengo, S.; Fortunato, L. Phosphorene is the new graphene in biomedical applications. Materials 2019, 12, 2301. [Google Scholar] [CrossRef] [Green Version]
- Kamenskikh, A.; Kuchumov, A.G.; Baradina, I. Modeling the contact interaction of a pair of antagonist teeth through individual protective mouthguards of different geometric configuration. Materials 2021, 14, 7331. [Google Scholar] [CrossRef]
- Baraka, M.M.; Geigerb, S.; Lev-Tov Chattaha, N.; Shaharc, R.; Weiner, S. Enamel dictates whole tooth deformation: A finite element model study validated by a metrology method. J. Struct. Biol. 2009, 168, 511–520. [Google Scholar] [CrossRef]
- Ausielloa, P.; Ciaramellab, S.; Fabianellic, A.; Gloriad, A.; Martorellib, M.; Lanzottib, A.; Wattse, D.C. Mechanical behavior of bulk direct composite versus block composite and lithium disilicate indirect Class II restorations by CAD-FEM modeling. Dent. Mater. 2017, 33, 690–701. [Google Scholar] [CrossRef] [Green Version]
- Rivera, J.L.V.; Gonçalves, E.; Soares, P.V.; Milito, G.; Perez, J.O.R.; Roque, G.F.P.; Fernández, M.V.; Losada, H.F.; Pereira, F.A.; del Pino, G.G.; et al. The Restored Premolars Biomechanical Behavior: FEM and Experimental Moiré Analyses. Appl. Sci. 2022, 12, 6768. [Google Scholar] [CrossRef]
- Laohachaiaroon, P.; Samruajbenjakun, B.; Chaichanasiri, E. Initial Displacement and Stress Distribution of Upper Central Incisor Extrusion with Clear Aligners and Various Shapes of Composite Attachments Using the Finite Element Method. Dent. J. 2022, 10, 114. [Google Scholar] [CrossRef]
- Bonaba, M.F.; Mojraa, A.; Shirazi, M. A numerical-experimental study on thermal evaluation of orthodontic tooth movement during initial phase of treatment. J. Therm. Biol. 2019, 80, 45–55. [Google Scholar] [CrossRef] [PubMed]




| Parameter | Enamel | Dentine |
|---|---|---|
| , GPa | 72.7 | 18.6 |
| 0.33 | 0.31 |
| Parameter | Material 1 | Material 2 | Material 3 |
|---|---|---|---|
| , GPa | 45.0 | 9.5 | 14.1 |
| 0.3 | 0.24 | 0.24 |
| Model | Element | Model Accounting for Prosthetic Inlay | ||
|---|---|---|---|---|
| Material 1 | Material 2 | Material 3 | ||
| Not taking into account the NCCL | Enamel | <by 16.00% | <by 11.86% | <by 12.93% |
| Dentine | >by 154.62% | >by 15.17% | >by 38.83% | |
| Taking into account the NCCL | Enamel | <by 10.65% | <by 6.24% | <by 7.38% |
| Dentine | >by 23.39% | <by 44.19% | <by 32.72% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamenskikh, A.A.; Sakhabutdinova, L.; Astashina, N.; Petrachev, A.; Nosov, Y. Numerical Modeling of a New Type of Prosthetic Restoration for Non-Carious Cervical Lesions. Materials 2022, 15, 5102. https://doi.org/10.3390/ma15155102
Kamenskikh AA, Sakhabutdinova L, Astashina N, Petrachev A, Nosov Y. Numerical Modeling of a New Type of Prosthetic Restoration for Non-Carious Cervical Lesions. Materials. 2022; 15(15):5102. https://doi.org/10.3390/ma15155102
Chicago/Turabian StyleKamenskikh, Anna A., Lyaysan Sakhabutdinova, Nataliya Astashina, Artem Petrachev, and Yuriy Nosov. 2022. "Numerical Modeling of a New Type of Prosthetic Restoration for Non-Carious Cervical Lesions" Materials 15, no. 15: 5102. https://doi.org/10.3390/ma15155102
APA StyleKamenskikh, A. A., Sakhabutdinova, L., Astashina, N., Petrachev, A., & Nosov, Y. (2022). Numerical Modeling of a New Type of Prosthetic Restoration for Non-Carious Cervical Lesions. Materials, 15(15), 5102. https://doi.org/10.3390/ma15155102






