Development of Novel Oral Formulations of Disulfide Antioxidants Based on Porous Silica for Controlled Release of the Drugs
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Syntheses of LA and LM Composites with Different Silica Materials
2.3. Particle Size Analysis
2.4. In Vitro LA and LM Release Measurements and Mathematical Analysis of Release Data
2.4.1. Individual Release Profiles into the Media with pH 1.6, 6.8, and 7.4
2.4.2. Modeling the Release of LA and LM with Regard to the Change in pH and Residence Time of the Drugs in Different Segments of the GIT
2.4.3. Analysis of Release Data
2.5. In Vitro Antioxidant Activity Evaluation of LA and LM
2.6. Statistics
3. Results and Discussion
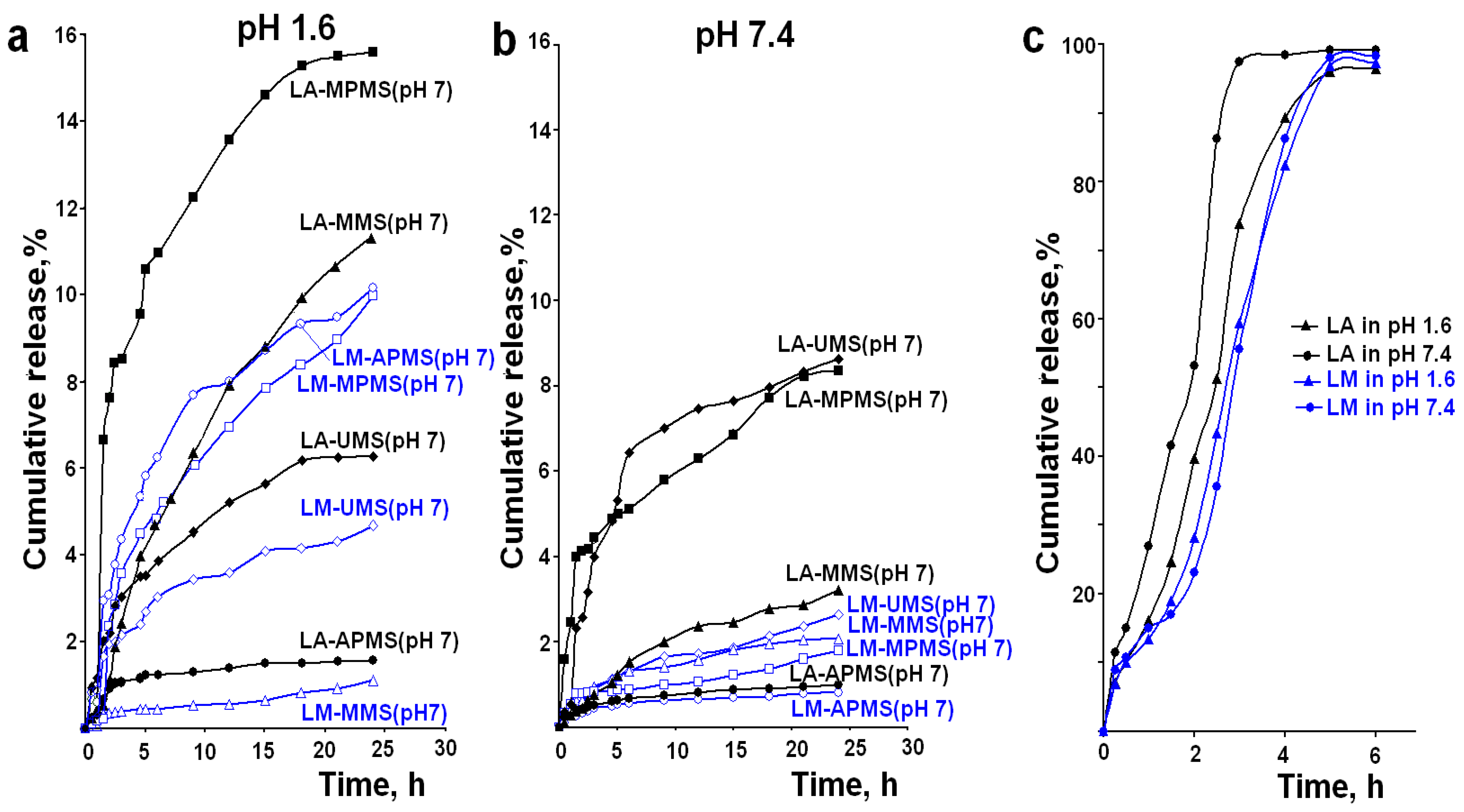
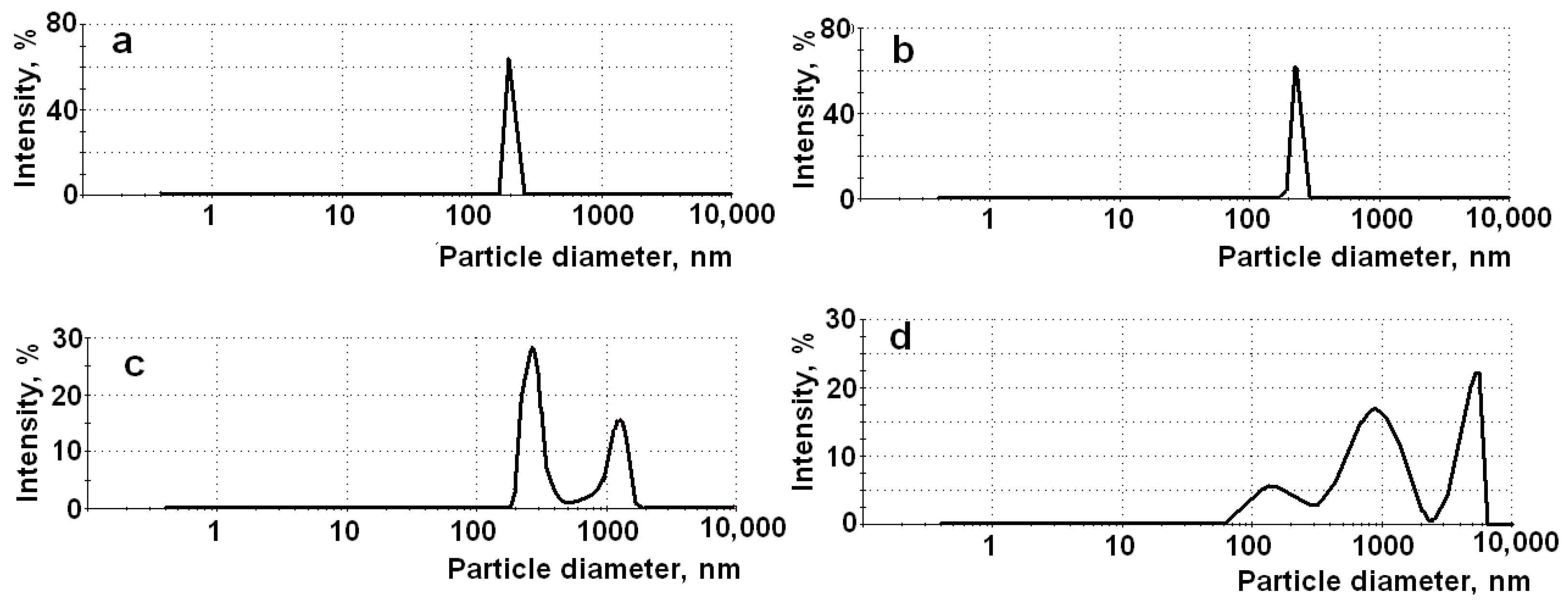
3.1. In Vitro Release Properties of Synthesized Composites in the Media with pH 1.6, 6.8, and 7.4
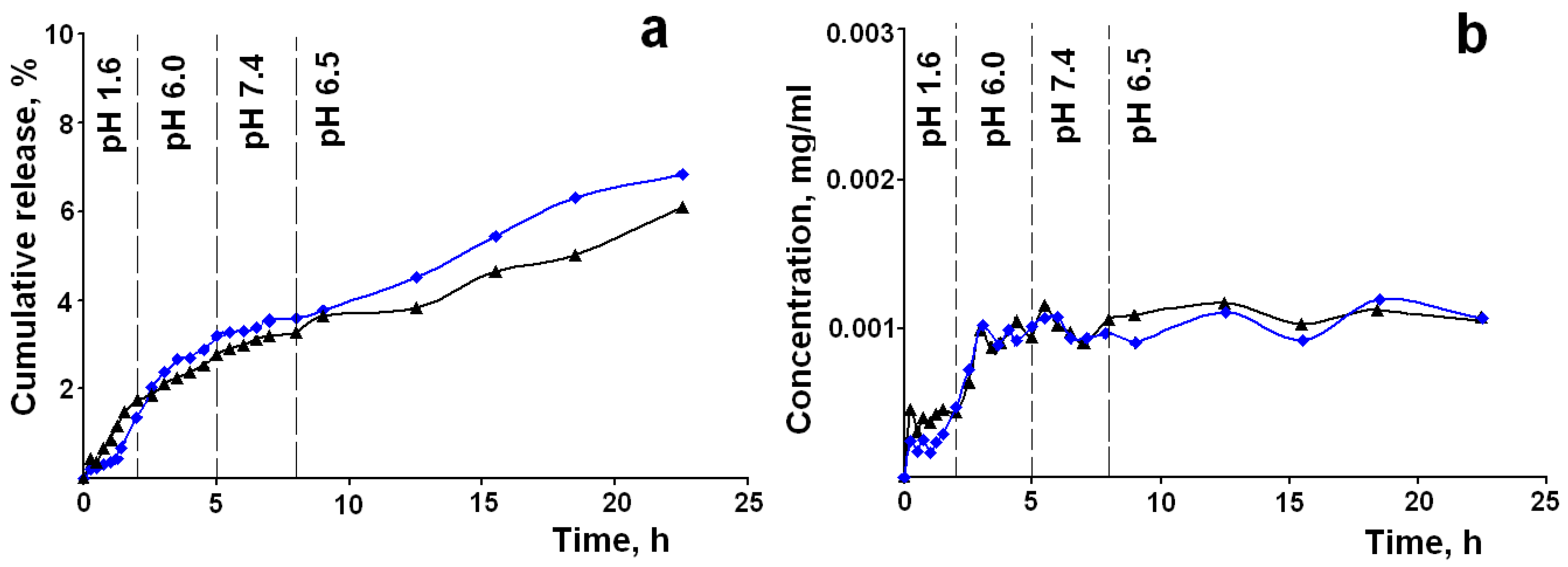
3.2. In Vitro Release Profiles and Antioxidant Activity in Accordance to the GIT Transit Conditions
- -
- the drug release from the composites follows the zero order kinetics in all tested media, i.e., the kinetic law of the release is uniform in all digestive fluids; the zero order release is ideal behavior for drug formulation, which allows for a constant quantity of drug to be released over an extended period of time, resulting in uniform and sustained drug delivery;
- -
- the drug release is controlled by anomalous diffusion; this means that the silica matrixes disintegrate/degrade during the release process, and this promotes their rapid elimination from the body;
- -
- the release rates in the medium with pH 6.8 and 7.4 are close, i.e., it is supposed that the drug release in intestine does not depend on pH; a higher release rate in the medium with pH 1.6 allows reaching a certain concentration level in the intestinal media.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative Stress, Aging, and Diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef] [PubMed]
- Ling, X.C.; Kuo, K.-L. Oxidative stress in chronic kidney disease. Ren. Replace. Ther. 2018, 4, 53. [Google Scholar] [CrossRef]
- Gracia, K.C.; Llanas-Cornejo, D.; Husi, H. CVD and Oxidative Stress. J. Clin. Med. 2017, 6, 22. [Google Scholar] [CrossRef]
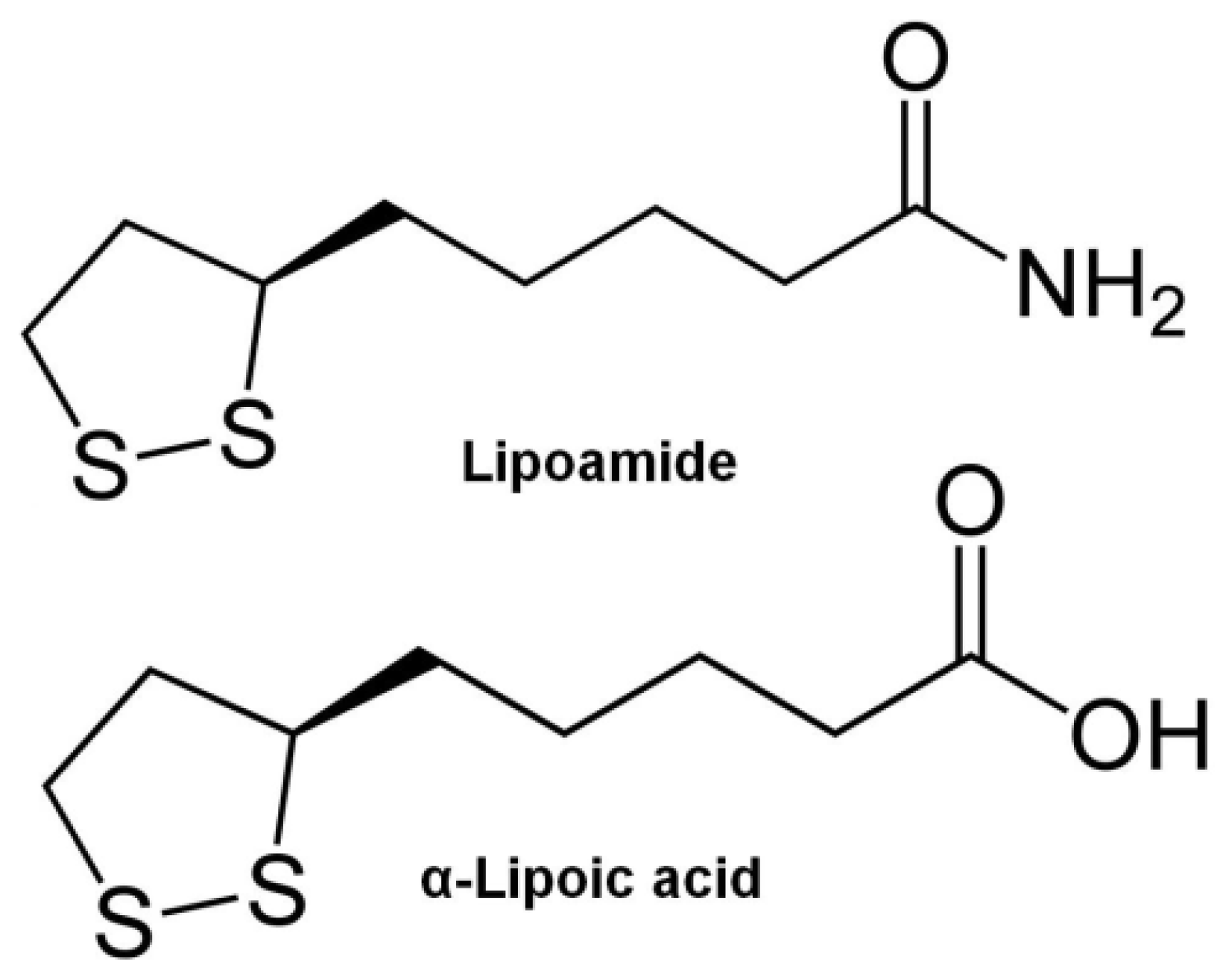
- Biewenga, G.P.; Haenen, G.R.; Bast, A. The Pharmacology of the Antioxidant Lipoic Acid. Gen. Pharmacol. Vasc. Syst. 1997, 29, 315–331. [Google Scholar] [CrossRef]
- Persson, H.L.; Svensson, A.I.; Brunk, U.T. α-Lipoic Acid And α-Lipoamide Prevent Oxidant-Induced Lysosomal Rupture and Apoptosis. Redox. Rep. 2001, 6, 327–334. [Google Scholar] [CrossRef]
- Singh, U.; Jialal, I. Retracted: Alpha-Lipoic Acid Supplementation and Diabetes. Nutr. Rev. 2008, 66, 646–657. [Google Scholar] [CrossRef] [PubMed]
- Rochette, L.; Ghibu, S.; Richard, C.; Zeller, M.; Cottin, Y.; Vergely, C. Direct and Indirect Antioxidant Properties of α-Lipoic Acid and Therapeutic Potential. Mol. Nutr. Food Res. 2013, 57, 114–125. [Google Scholar] [CrossRef]
- Liu, J.; Shen, W.; Tian, C. Use of Lipoamide in Preventing and Treating Insulin Resistance. Patent No. CN101396357B, 29 September 2007. [Google Scholar]
- Moura, F.A.; de Andrade, K.Q.; Farias dos Santos, J.C.; Goulart, M.O.F. Lipoic Acid: Its Antioxidant and Anti-Inflammatory Role and Clinical Applications. Curr. Top Med. Chem. 2015, 15, 458–483. [Google Scholar] [CrossRef]
- Gomes, M.B.; Negrat, C.A. Alpha-lipoic Acid as a Pleiotropic Compound with Potential Therapeutic Use in Diabetes and Other Chronic Diseases. Diabet. Metabol. Syndr. 2014, 6, 80. Available online: http://www.dmsjournal.com/content/6/1/80 (accessed on 15 February 2021). [CrossRef]
- Salehi, B.; Yılmaz, Y.B.; Antika, G.; Tumer, T.B.; Mahomoodally, M.F.; Lobine, D.; Akram, M.; Riaz, M.; Capanoglu, E.; Sharopov, F.; et al. Insights on the Use of α-Lipoic Acid for Therapeutic Purposes. Biomolecules 2019, 9, 356. [Google Scholar] [CrossRef] [PubMed]
- Teichert, J.; Hermann, R.; Ruus, P.; Preiss, R. Plasma Kinetics, Metabolism, and Urinary Excretion of Alpha-Lipoic Acid following Oral Administration in Healthy Volunteers. J. Clin. Pharmacol. 2003, 43, 1257–1267. [Google Scholar] [CrossRef]
- Di Martino, P. Human Bioavailability and Pharmacokinetic Profile of Different Formulations Delivering Alpha Lipoic Acid. J. Clin. Cell. Immunol. 2012, 1, 418. [Google Scholar] [CrossRef]
- Gorąca, A.; Huk-Kolega, H.; Piechota, A.; Kleniewska, P.; Ciejka, E.; Skibska, B. Lipoic Acid–Biological Activity and Therapeutic Potential. Pharmacol. Rep. 2011, 63, 849–858. [Google Scholar] [CrossRef]
- Emir, D.F.; Ozturan, I.U.; Yilmaz, S.; Yılmaz, S. Alpha Lipoic Acid Intoxicatıon: An Adult. Am. J. Emerg. Med. 2018, 36, 1125.e3–1125.e5. [Google Scholar] [CrossRef]
- Milašinović, N.; Čalija, B.; Vidović, B.; Sakač, M.C.; Vujić, Z.; Knežević-Jugović, Z. Sustained Release of α-Lipoic Acid from Chitosan Microbeads Synthetized by Inverse Emulsion Method. J. Taiwan Inst. Chem. Eng. 2016, 60, 106–112. [Google Scholar] [CrossRef]
- Bernkop-Schnürch, A.; Schuhbauer, H.; Clausen, A.E.; Hanel, R. Development of a Sustained Release Dosage Form for α-Lipoic Acid. I. Design and In Vitro Evaluation. Drug Dev. Ind. Pharm. 2004, 30, 27–34. [Google Scholar]
- Bernkop-Schnürch, A.; Reich-Rohrwig, E.; Marschütz, M.; Schuhbauer, H.; Kratzel, M. Development of a Sustained Release Dosage Form for α-Lipoic Acid. II. Evaluation in Human Volunteers. Drug Dev. Ind. Pharm. 2004, 30, 35–42. [Google Scholar] [CrossRef]
- Kofuji, K.; Isobe, T.; Murata, Y. Controlled Release of Alpha-Lipoic Acid Through Incorporation into Natural Polysaccharide-Based Gel Beads. Food Chem. 2009, 115, 483–487. [Google Scholar] [CrossRef]
- Zhang, Z.-Z.; Song, L.; Zhang, Z.-Y.; Lv, M.-M. Control-Released Alpha-Lipoic Acid-Loaded PLGA Microspheres Enhance Bone Formation in Type 2 Diabetic Rat Model. Int. J. Clin. Exp. Pathol. 2017, 10, 10019–10031. [Google Scholar]
- Lasoń, E.; Sikora, E.; Miastkowska, M.; Socha, P.; Ogonowski, J. NLC Delivery Systems for Alpha Lipoic Acid: Physicochemical Characteristics and Release Study. Colloids Surfaces A Physicochem. Eng. Asp. 2017, 532, 57–62. [Google Scholar] [CrossRef]
- Xia, N.; Liu, T.; Wang, Q.; Xia, Q.; Bian, X. In Vitro Evaluation of α-Lipoic Acid-Loaded Lipid Nanocapsules for Topical Delivery. J. Microencapsul. 2017, 34, 571–581. [Google Scholar] [CrossRef]
- Nishiura, H.; Sugimoto, K.; Akiyama, K.; Musashi, M.; Kubota, Y.; Yokoyama, T.; Yamashita, Y.; Kuriki, T.; Yamaguchi, Y. A Novel Nano-Capsule of α-Lipoic Acid as a Template of Core-Shell Structure Constructed by Self-Assembly. J. Nanomed. Nanotechnol. 2012, 4, 1–8. [Google Scholar] [CrossRef]
- Takahashi, H.; Bungo, Y.; Mikuni, K. The Aqueous Solubility and Thermal Stability of α-Lipoic Aid Are Enhanced by Cy-clodextrin. Biosci. Biotechnol. Biochem. 2011, 75, 633–637. [Google Scholar] [CrossRef]
- Overview of Food Ingradients, Additives & Colors. Available online: https://www.fda.gov/food/food-ingredients-packaging/overview-food-ingredients-additives-colors (accessed on 16 November 2020).
- Li, X.; Liu, Z.; Luo, C.; Jia, H.; Sun, L.; Hou, B.; Shen, W.; Packer, L.; Cotman, C.W.; Liu, J. Lipoamide Protects Retinal Pigment Epithelial Cells From Oxidative Stress and Mitochondrial Dysfunction. Free Radic. Biol. Med. 2008, 44, 1465–1474. [Google Scholar] [CrossRef]
- Dolinina, E.S.; Akimsheva, E.Y.; Parfenyuk, E.V. Development of Novel Silica-Based Formulation of α-Lipoic Acid: Evaluation of Photo and Thermal Stability of the Encapsulated Drug. Pharmaceutics 2020, 12, 228. [Google Scholar] [CrossRef]
- Dolinina, E.S.; Akimsheva, E.Y.; Parfenyuk, E.V. Study of Thermal Properties of Antioxidant Lipoamide and its Composites with Colloid Silica. J. Mater. Res. 2021, 1–9. [Google Scholar] [CrossRef]
- Nechikkattu, R.; Park, S.S.; Ha, C.-S. Zwitterionic Functionalised Mesoporous Silica Nanoparticles for Alendronate Release. Microporous Mesoporous Mater. 2019, 279, 117–127. [Google Scholar] [CrossRef]
- Zaharudin, N.S.; Mohamed Isa, E.D.; Ahmad, H.; Abdul Rahman, M.B.; Jumbri, K. Functionalized Mesoporous Silica Nanoparticles Templated by Pyridinium Ionic Liquid for Hydrophilic and Hydrophobic Drug Release Application. J. Saudi Chem. Soc. 2020, 24, 289–302. [Google Scholar] [CrossRef]
- Shi, Z.-G.; Guo, Q.-Z.; Liu, Y.-T.; Xiao, Y.-X.; Xu, L. Drug Delivery Devices Based on Macroporous Silica Spheres. Mater. Chem. Phys. 2011, 126, 826–831. [Google Scholar] [CrossRef]
- Rehman, F.; Ahmed, K.; Airoldi, C.; Gaisford, S.; Buanz, A.; Rahim, A.; Muhammad, N.; Volpe, P.L. Amine Bridges Grafted Mesoporous Silica, as a Prolonged/Controlled Drug Release System for the Enhanced Therapeutic Effect Of Short Life Drugs. Mater. Sci. Eng. C 2017, 72, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Manzano, J.S.; Singappuli-Arachchige, D.; Parikh, B.L.; Slowing, I.I. Fine-Tuning the Release of Molecular Guests from Mesopo-Rous Silicas by Controlling the Orientation and Mobility of Surface Phenyl Substituents. Chem. Eng. J. 2018, 340, 73–80. [Google Scholar] [CrossRef]
- Guerra, A.; Etienne-Mesmin, L.; Livrelli, V.; Denis, S.; Blanquet-Diot, S.; Alric, M. Relevance and challenges in modeling human gastric and small intestinal digestion. Trends Biotechnol. 2012, 30, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Koziolek, M.; Grimm, M.; Becker, D.; Iordanov, V.; Zou, H.; Shimizu, J.; Wanke, C.; Garbacz, G.; Weitschies, W. Investigation of pH and Temperature Profiles in the GI Tract of Fasted Human Subjects Using the Intellicap R System. J. Pharm. Sci. 2015, 104, 2855–2863. [Google Scholar] [CrossRef] [PubMed]
- Sciascia, Q.; Das, G.; Metges, C.C. REVIEW: The Pig as a Model for Humans: Effects of Nutritional Factors on Intestinal Function and health. J. Anim. Sci. 2016, 94, 441–452. [Google Scholar] [CrossRef]
- Dolinina, E.S.; Parfenyuk, E.V. Development of Novel Delivery System for Cardiovascular Drug Molsidomine: Influence of Synthesis Method and Conditions on Molsidomine Release from Its Composites with Hydrophilic Silica In Vitro. J. Pharm. Sci. 2016, 105, 1952–1959. [Google Scholar] [CrossRef]
- Bruschi, M.L. Strategies of Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Cambridge, UK, 2015; Chapter 5; pp. 63–86. [Google Scholar]
- Chai, T.; Draxler, R.R. Root mean square error (RMSE) or mean absolute error (MAE)? – Arguments against avoiding RMSE in the literature. Geosci. Model Dev. 2014, 7, 1247–1250. [Google Scholar] [CrossRef]
- Yamoaka, K.; Nakagawa, T.; Uno, T. Application of the Akaike Information Criterion (AIC) in the Evaluation of Linear Pharmaco-Kinetics Equations. J. Pharmacokinet. Biopharm. 1978, 6, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Pisani, S.; Dorati, R.; Chiesa, E.; Genta, I.; Modena, T.; Bruni, G.; Grisoli, P.; Conti, B. Release Profile of Gentamicin Sulfate from Polylactide-co-Polycaprolactone Electrospun Nanofiber Matrices. Pharmaceutics 2019, 11, 161. [Google Scholar] [CrossRef]
- Weiser, J.R.; Yueh, A.; Putnam, D. Protein Release from Dihydroxyacetone-Based Poly(Carbonate Ester) Matrices. Acta Biomater. 2013, 9, 8245–8253. [Google Scholar] [CrossRef]
- Legnoverde, M.S.; Basaldella, E.I. Influence of Particle Size on the Adsorption and Release of Cephalexin Encapsulated in mes-Oporous Silica SBA-15. Mater. Lett. 2016, 181, 331–334. [Google Scholar] [CrossRef]
- Xu, W.; Gao, Q.; Xu, Y.; Wu, N.; Sun, Y.; Shen, W.; Deng, F. Controllable Release of Ibuprofen from Size-Adjustable and Surface Hydrophobic Mesoporous Silica Spheres. Powder Technol. 2009, 191, 13–20. [Google Scholar] [CrossRef]
- Bouchoucha, M.; Côté, M.-F.; C.-Gaudreault, R.; Fortin, M.-A.; Kleitz, F. Size-Controlled Functionalized Mesoporous Silica Nanoparticles for Tunable Drug Release and Enhanced Anti-Tumoral Activity. Chem. Mater. 2016, 28, 4243–4258. [Google Scholar] [CrossRef]
- Thioctic Acid. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/864 (accessed on 16 November 2020).
- Homer, R.B.; Johnson, C.D. Acid-Base and Complexing Properties of amides. Amides (1970) 2010, 3, 187–243. [Google Scholar] [CrossRef]
- Lipoamide. Available online: https://www.medchemexpress.com/Lipoamide.html (accessed on 16 November 2020).
- Qu, H.; Bhattacharyya, S.; Ducheyne, P. Silicon Oxide Based Materials for Controlled Release in Orthopedic Procedures. Adv. Drug Deliv. Rev. 2015, 94, 96–115. [Google Scholar] [CrossRef]
- Zhang, S.; Chu, Z.; Yin, C.; Zhang, C.; Lin, G.; Li, Q. Controllable Drug Release and Simultaneously Carrier Decomposition of SiO2-Drug Composite Nanoparticles. J. Am. Chem. Soc. 2013, 135, 5709–5716. [Google Scholar] [CrossRef]
- Yilmaz, E.; Bengisu, M. Drug Entrapment in Silica Microspheres Through a Single Step Sol–Gel process Andin Vitro Release Behavior. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 77, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Tan, B.; Rankin, S.E. Study of the Effects of Progressive Changes in Alkoxysilane Structure on Sol−Gel Reactivity. J. Phys. Chem. B 2006, 110, 22353–22364. [Google Scholar] [CrossRef] [PubMed]
- Dong, H. Organic-Inorganic Hybrid Mesoporous Silica Materials and Their Application as Host Matrix for Protein Molecules. Ph.D. Thesis, Drexel University, Philadelphia, PA, USA, March 2002. [Google Scholar]
- Magnini, F.; Capacchietti, M.; Napolioni, V.; Reggiardo, G.; Fasani, R.; Ferrari, P. Single Dose Bioavailability and Pharmaco-Kinetic Study of a Innovative Formulation of α-Lipoic Acid (ALA600) in Healthy Volunteers. Minerva Med. 2011, 102, 475–482. [Google Scholar]
- Xie, Y.; Li, X.; Chen, J.; Deng, Y.; Lu, W.; Chen, D. pH Effect and Chemical Mechanisms of Antioxidant Higenamine. Molecules 2018, 23, 2176. [Google Scholar] [CrossRef]
- Ghosh, S.; Chakraborty, R.; Raychaudhuri, U. Determination of pH-Dependent Antioxidant Activity of Palm (Borassus Flabellifer) Polyphenol Compounds by Photoluminol and DPPH Methods: A Comparison of Redox Reaction Sensitivity. 3 Biotech 2015, 5, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Amorati, R.; Pedulli, G.F.; Cabrini, L.; Zambonin, A.L.; Landi‡, L. Solvent and pH Effects on the Antioxidant Activity of Caffeic and Other Phenolic Acids. J. Agric. Food Chem. 2006, 54, 2932–2937. [Google Scholar] [CrossRef] [PubMed]

| Designation of Samples | Antioxidant | Precursor | Synthesis pH |
|---|---|---|---|
| LA–UMS (pH 3) | α-lipoic acid | TEOS | 3 |
| LA–UMS (pH 7) | α-lipoic acid | TEOS | 7 |
| LA–MPMS (pH 3) | α-lipoic acid | TEOS + MPTMOS | 3 |
| LA–MPMS (pH 7) | α-lipoic acid | TEOS + MPTMOS | 7 |
| LA–APMS (pH 3) | α-lipoic acid | TEOS + APTEOS | 3 |
| LA–APMS (pH 7) | α-lipoic acid | TEOS + APTEOS | 7 |
| LA–MMS (pH 3) | α-lipoic acid | TEOS + MTMOS | 3 |
| LA–MMS (pH 7) | α-lipoic acid | TEOS + MTMOS | 7 |
| LM–UMS (pH 7) | lipoamide | TEOS | 7 |
| LM–MPMS (pH 7) | lipoamide | TEOS + MPTMOS | 7 |
| LM–APMS (pH 7) | lipoamide | TEOS + APTEOS | 7 |
| LM–MMS (pH 7) | lipoamide | TEOS + MTMOS | 7 |
| Composites | Drug Loading, mg/g a | pH 1.6 | pH 6.8 | pH 7.4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mb, % | tb, h | M∞, % | Mb, % | tb, h | M∞, % | Mb, % | tb, h | M∞, % | ||
| LA–UMS (pH 3) | 60 | 2.8 | 2.2 | 10.7 | 0.5 | 0.5 | 2.0 | 0.2 | 0.5 | 5.0 |
| LA–UMS (pH 7) | 57 | 1.2 | 1.1 | 6.2 | 1.7 | 0.9 | 4.1 | 0.6 | 1.2 | 8.6 |
| LA–MMS (pH 3) | 60 | 3.2 | 2.6 | 4.0 | 0.9 | 0.4 | 11.3 | 0.3 | 0.5 | 9.0 |
| LA–MMS (pH 7) | 61 | 1.3 | 1.4 | 10.5 | 0.4 | 0.5 | 2.5 | 0.1 | 0.4 | 3.2 |
| LA–MPMS (pH 3) | 59 | 0.2 | 0.5 | 4.4 | 0.5 | 0.5 | 12.1 | 0.6 | 0.5 | 3.8 |
| LA–MPMS (pH 7) | 58 | 0.6 | 0.9 | 15.6 | 1.0 | 1.5 | 2.4 | 3.9 | 1.5 | 8.4 |
| LA–APMS (pH 3) | 46 | 2.9 | 1.0 | 7.8 | 0.5 | 0.5 | 1.4 | 0.7 | 0.9 | 3.4 |
| LA–APMS (pH 7) | 56 | 0.7 | 1.4 | 1.6 | 0.2 | 1.5 | 0.5 | 0.3 | 1.1 | 1.0 |
| LM–UMS (pH 7) | 57 | 2.0 | 2.5 | 4.7 | 0.6 | 1.8 | 2.6 | 0.6 | 2.5 | 1.4 |
| LM–MMS (pH 7) | 44 | 0.1 | 1.1 | 1.1 | 0.4 | 1.5 | 2.1 | 1.0 | 2.1 | 1.8 |
| LM–MPMS (pH 7) | 46 | 0.3 | 1.5 | 9.8 | 0.8 | 1.9 | 1.8 | 0.6 | 2.0 | 1.3 |
| LM–APMS (pH 7) | 53 | 0.9 | 1.0 | 10.0 | 0.3 | 1.5 | 0.8 | 0.4 | 1.0 | 1.1 |
| Composite | Mean Diameter, nm | Composite | Mean Diameter, nm |
|---|---|---|---|
| LA–UMS (pH 3) | LA–APMS (pH 3) | ||
| 201 ± 18; | 189 ± 39; 1050 ± 98; | ||
| PDI 0.072 | PDI 0.639 | ||
| LA–UMS (pH 7) | LA–APMS (pH 7) | ||
| 201 ± 18; | 173 ± 61; 911 ± 291; 4628 ± 644; | ||
| PDI 0.072 | PDI 0.897 | ||
| LA–MMS (pH 3) | 190 ± 15; PDI 0.043 | LM–UMS (pH 7) | 264 ± 19; PDI 0.076 |
| LA–MMS (pH 7) | 218 ± 21; PDI 0.074 | LM–MMS (pH 7) | 202 ± 17; PDI 0.053 |
| LA–MPMS (pH 3) | 198 ± 15; PDI 0.039 | LM–MPMS (pH 7) | 222 ± 22: PDI 0.102 |
| LA–MPMS (pH 7) | 222 ± 19; PDI 0.051 | LM–APMS (pH 7) | |
| 165 ± 31; 863 ± 306; 6865 ± 716; | |||
| PDI 0.788 |
| pH 1.6 | pH 6.8 | pH 7.4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zero-order model | First-order model | Hixon–Crowell model | Korsmey er–Peppas model | Zero-order model | First-order model | Hixon–Crowell model | Korsmey- er–Peppas model | Zero-order mode | First-order model | Hixon– Crowell model | Korsmey- er–Peppas model | |
| LA–UMS (pH3) R2 RMSE AIC | k0 = 0.301 0.9509 5.38 65.44 | k1 = 0.0014 0.9351 1.35 35.04 | 0.9338 | k = 2.13 n = 0.44 0.9944 | k0 = 0.047 0.9525 0.18 −9.74 | k1 = 0.0002 0.9330 0.74 32.13 | 0.9588 | k = 2.28 n = 0.47 0.9919 | k0 = 0.151 9417 0.57 23.11 | k1 = 0.0007 0.9439 2.26 61.73 | 0.9557 | k = 1.91 n = 0.49 0.9872 |
| LA–UMS (pH 7) R2 RMSE AIC | k0 = 0.192 0.9480 2.471 58.86 | k1 = 0.0009 0.9465 0.789 27.16 | 0.9309 | k = 2.04 n = 0.43 0.9850 | k0 = 0.052 0.9211 0.634 23.48 | k1 = 0.0002 0.9618 0.213 −4.84 | 0.8987 | k = 1.72 n = 0.21 0.9779 | k0 = 0.270 0.9303 3.838 70.32 | k1 = 0.0012 0.9543 1.121 38.31 | 0.9245 | k = 1.92 n = 0.44 0.9717 |
| LA–MMS (pH 3) R2 RMSE AIC | k0 = 0.002 0.9245 0.399 6.69 | k1 = 0.0001 0.9500 0.101 −20.75 | 0.9034 | k = 1.85 n = 0.25 0.9548 | k0 = 0.470 0.9930 1.916 5.17 | k1 = 0.0022 0.9201 8.151 97.69 | 0.9889 | k = 4.13 n = 0.98 0.9884 | k0 = 0.198 0.9254 2.611 65.82 | k1 = 0.0009 0.9567 0.771 31.66 | 0.9054 | k = 1.38 n = 0.22 |
| LA–MMS (pH 7) R2 RMSE AIC | k0 = 0.417 0.9655 1.805 45.98 | k1 = 0.0019 0.9236 6.516 76.89 | 0.9755 | k = 2.43 n = 0.71 0.9677 | k0= 0.095 0.9855 0.336 8.42 | k1 = 0.0004 0.9845 1,226 44.68 | 0.9853 | k = 3.29 n = 0.77 0.9879 | k0 = 0.101 0.9667 0.486 18.76 | k1 = 0.0006 0.9409 1.886 56.81 | 0.9779 | k = 2.81 n = 0.78 0.9739 |
| LA–MPMS (pH 3) R2 RMSE AIC | k0 = 0.155 0.9452 0.579 26.24 | k1 = 0.0014 0.9488 2.384 68.68 | 0.9663 | k = 1.77 n = 0.46 0.9709 | k0 = 0.285 0.935 4.751 89.37 | k1 = 0.0008 0.9499 1.070 44.66 | 0.9004 | k = 1.43 n = 0.25 0.9949 | k0 = 0.135 0.9545 1.017 43.15 | k1 = 0.0006 0.9377 3.719 88,75 | 0.9677 | k = 2.92 n = 0.77 0.9837 |
| LA–MPMS (pH 7) R2 RMSE AIC | k0 = 0.392 0.9063 6.129 89.81 | k1 = 0.0019 0.9502 1.581 51.78 | 0.9088 | k = 1.42 n = 0.25 0.9850 | k0 = 0.059 0.9776 0.555 20.07 | k1 = 0.0003 0.9636 3.420 67.31 | 0.9734 | k = 3.59 n = 0.82 0.9749 | k0 = 0.202 0.9887 0.806 29.74 | k1 = 0.0009 0.9806 3.420 67.88 | 0.9891 | k = 4.53 n = 0.95 0.9855 |
| LA–APMS (pH 3) R2 RMSE AIC | k0 = 0.121 0.9099 2.022 53.64 | k1 = 0.0006 0.9608 0.501 17.36 | 0.9007 | k = 1.74 n = 0.25 0.9843 | k0 = 0.020 0.9099 0.329 7.815 | k1 = 0.0001 0.9536 0.080 −31.90 | 0.9034 | k = 1.82 n = 0.23 0.9749 | k0 = 0.116 0.9377 1.696 49.08 | k1 = 0.0003 0.9666 0.472 15.95 | 0.9111 | k = 1.33 n = 0.39 0.9855 |
| LA–APMS (pH 7) R2 RMSE AIC | k0 = 0.028 0.9079 0.352 6.79 | k1 = 0.0002 0.9577 0.116 −19.83 | 0.9101 | k = 1.98 n = 0.33 0.9803 | k0 = 0.011 0.9558 0.153 −13.13 | k1 = 0.0001 0.9565 0.048 −41.37 | 0.9259 | k = 2.10 n = 0.39 0.9588 | k0 = 0.026 0.9556 0.326 6.23 | k1 = 0.0001 0.9572 0.105 −23.36 | 0.9321 | k = 2.16 n = 0.41 0.9755 |
| LM–UMS (pH 7) R2 RMSE AIC | k0 = 0.113 0.9677 0.524 12.12 | k1 = 0.0005 0.9377 2.256 41.30 | 0.9801 | k = 3.28 n = 0.75 0.9675 | k0 = 0.079 0.9700 0.341 4.68 | k1 = 0.0003 0.9406 1.387 35.58 | 0.9704 | k = 2.67 n = 0.64 0.9865 | k0 = 0.037 0.9927 0.169 −10.47 | k1 = 0.0002 0.9472 0.407 7.07 | 0.9921 | k = 4.51 n = 0.92 0.9798 |
| LM–MMS (pH 7) R2 RMSE AIC | k0 = 0.307 0.9714 0.137 −16.42 | k1 = 0.0001 0.9344 0.480 10.18 | 0.9663 | k = 3.72 n = 0.76 0.9565 | k0 = 0.061 0.9600 0.262 −0.303 | k1 = 0.0003 0.9433 0.797 26.38 | 0.9633 | k = 2.13 n = 0.51 0.9677 | k0 = 0.037 0.9766 0.162 −11.70 | k1 = 0.0002 0.9703 0.495 12.92 | 0.9766 | k = 4.32 n = 0.84 0.9577 |
| LM–MPMS (pH 7) R2 RMSE AIC | k0 = 0.307 0.9688 1.330 38.67 | k1 = 0.0014 0.9207 5.272 71.71 | 0.9764 | k = 3.88 n = 0.79 0.9644 | k0= 0.041 0.9676 0.202 −6.86 | k1 = 0.0002 0.9601 0.939 26.53 | 0.9773 | k = 5.50 n= 0.98 0.9607 | k0= 0.035 0.9892 0.116 −17.94 | k1 = 0.0001 0. 9555 0.408 8.66 | 0.9893 | k = 2.95 n= 0.67 0.9612 |
| LM–APMS (pH 7) R2 RMSE AIC | k0 = 0.309 0.8984 3.968 71.18 | k1 = 0.0014 0.9716 1.297 42.11 | 0.9022 | k = 1.84 n = 0.42 0.9825 | k0 = 0.019 0.9104 0.247 1.73 | k1 = 0.0001 0.9660 0.084 −27.53 | 0.9107 | k = 2.26 n = 0.41 0.9650 | k0 = 0.025 0.9126 0.377 10.03 | k1 = 0.0001 0.9677 0.105 −23.23 | 0.9124 | k = 1.80 n = 0.30 0.9752 |
| Composite | Mb, % | Zero Order | First Order | Hixon-Crowell | Korsmeyer- |
|---|---|---|---|---|---|
| tb, h | Model | Model | Model | Peppas Model | |
| LA–MMS (pH 7) | 1.5 1.4 | k0 = 0.201 R2 = 0.9737 | k1 = 0.0011 R2 = 0.9194 | R2 = 0.9763 | k = 1.93 |
| n = 0.64 | |||||
| R2 = 0.9577 | |||||
| LM–MPMS (pH 7) | 0.5 1.3 | k0 = 0.244 R2 = 0.9577 | k1 = 0.0012 R2 = 0.9455 | R2 = 0.9661 | k = 2.28 |
| n = 0.66 | |||||
| R2 = 0.9585 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dolinina, E.S.; Parfenyuk, E.V. Development of Novel Oral Formulations of Disulfide Antioxidants Based on Porous Silica for Controlled Release of the Drugs. Materials 2021, 14, 963. https://doi.org/10.3390/ma14040963
Dolinina ES, Parfenyuk EV. Development of Novel Oral Formulations of Disulfide Antioxidants Based on Porous Silica for Controlled Release of the Drugs. Materials. 2021; 14(4):963. https://doi.org/10.3390/ma14040963
Chicago/Turabian StyleDolinina, Ekaterina S., and Elena V. Parfenyuk. 2021. "Development of Novel Oral Formulations of Disulfide Antioxidants Based on Porous Silica for Controlled Release of the Drugs" Materials 14, no. 4: 963. https://doi.org/10.3390/ma14040963
APA StyleDolinina, E. S., & Parfenyuk, E. V. (2021). Development of Novel Oral Formulations of Disulfide Antioxidants Based on Porous Silica for Controlled Release of the Drugs. Materials, 14(4), 963. https://doi.org/10.3390/ma14040963






