1. Introduction
Dental implants have become increasingly common as a method for replacing missing teeth in recent decades [
1,
2,
3,
4]. However, while some studies have reported an implant success rate as high as 78–100% [
5], other studies have indicated that single tooth replacement failures may occur for a variety of reasons [
6], including implant surface, implant design, and bone quality factors [
7] and early bone loss in the dental implant region [
8]. In practice, the bio-structure of dental implants is of critical importance in determining the success rate of the implant procedure since it affects the bone directly and causes the stress distribution to change from constant to a variable, thereby putting both the implant and the bone at risk of biomechanical overload failure [
9]. The success rate of dental implants is also crucially dependent on the efficiency of the stress transfer from the implant to the supporting bone [
10,
11,
12], which depends in turn on many factors, including the loading condition [
9], the implant thread design [
2,
13,
14], and the bone material properties [
15].
The Finite Element Method (FEM) provides an extremely efficient approach for analyzing biomechanical problems [
16,
17,
18,
19,
20,
21,
22]. FEM is particularly attractive for the analysis of biomechanical processes, which are difficult (if not impossible) to examine in vivo or in vitro. As a result, it has been used extensively in the literature to evaluate the stress and deformation behavior of dental implants to improve their success rate [
3,
12,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34]. Tribst et al. examined the mechanical performance of an alternate design for producing an implant-supported full-arch dental prosthesis (IFDP) with limited occlusal height using a finite element method (FEM) [
35]. Additionally, a linear static structural finite element method (FEM) simulation was used to evaluate entire tooth models (enamel, dentin, and pulp) which is constructed with an efficient and new method using micro-computed tomography (CT) data [
36]. The study by Mosavar et al. was inspired by a paucity of numerical models of bone-implant interactions for diverse osseointegration and the simplification of bone as an isotropic material in prior investigations. Further, four different thread form implants were modeled and subjected to static occlusal load and varied osseointegration conditions of the bone-implant interface using finite element analysis. It is found that the cervical cortical bone region received the most stress, as did the first thread [
37].
During their service lives, dental implants are subjected to both static and dynamic loads [
38]. Static loads are exerted on the rigid maxilla from the unmoving mandible, and the intensity is not varied over time [
39]. One of the many shortcomings in Finite Element analysis is the assumption of unrealistic (static) loads in dental implants [
40]. Most previous studies only consider the effects of static loads applied to a single point on the implant surface [
24,
41,
42,
43]. As a result, the induced stress does not usually exceed the yield strength of the dental implant material (e.g., 550 MPa for titanium, [
44]) or bone (190 MPa for cortical bone, and 10 MPa for cancellous bone [
44]). Therefore, in comparison to more realistic cyclic loading, static loads are associated with a less critical effect, creating less stress in the dental implant system [
45]. Similarly, quasi-static loading has no significant influence on both implant and surrounding bone. Gehrke et al. [
46] investigated one-piece and two-piece sintered dental implants subjected to quasi-static loading at a 30 degrees angle to the implant axis. The results showed that both implants could resist the loads produced during mastication.
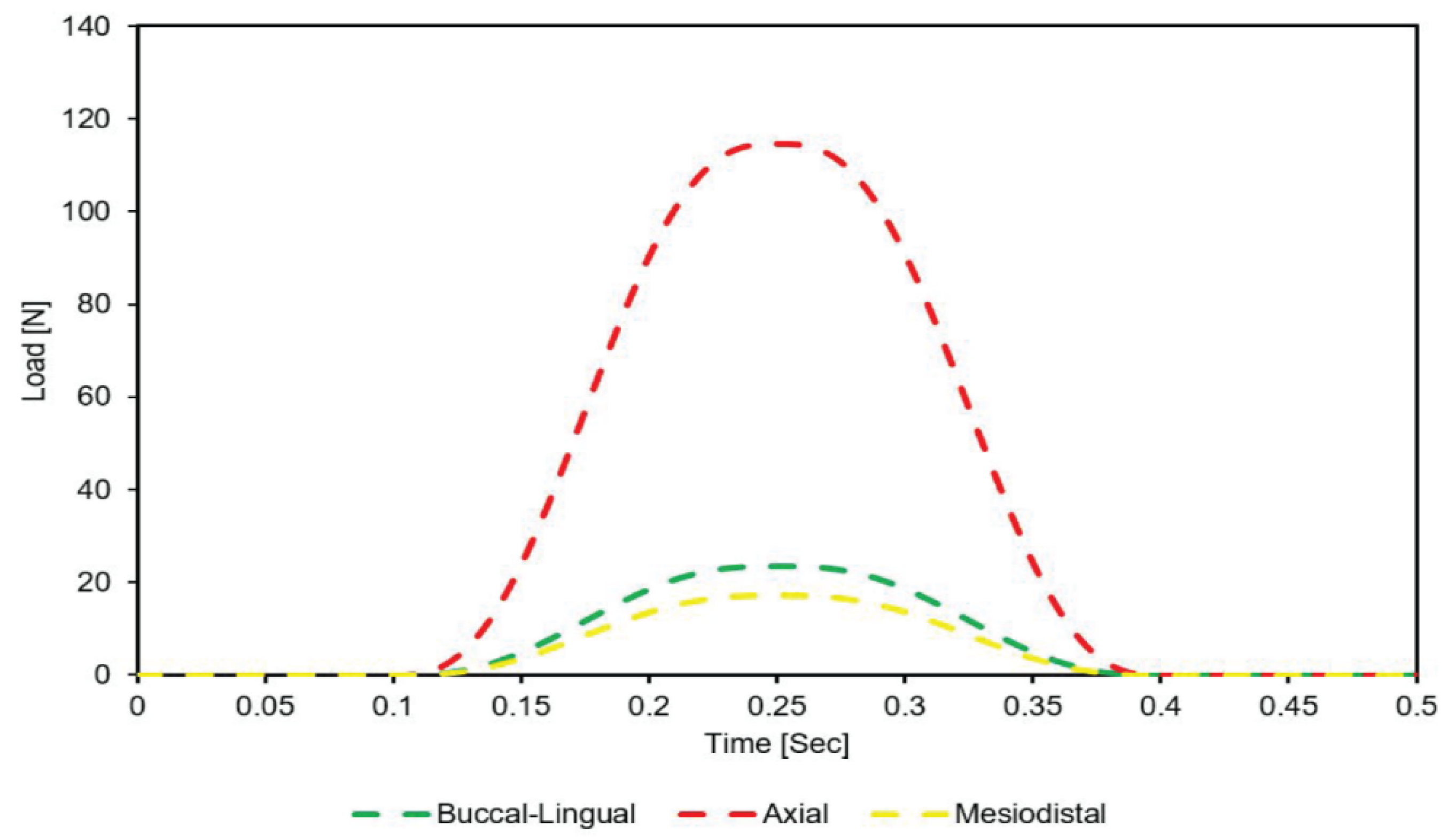
However, to mimic the actual mandible movement for FEM simulation, the masticatory occlusal load applied to the crown surface must be cyclic, repeatable, and dynamic with time [
47]. Furthermore, cyclic loading increases stress, which was already at a peak in static loading conditions. Hence, increasing the possibility of implant fatigue and fracture during clinical service. Regardless of those consequences, not many studies about the effect of dynamic loading on the performance of dental implants and bone. Gotfredsen et al. [
48,
49,
50] showed that in practical implant situations, high dynamic loads are much more destructive than static loads, and therefore have a critical effect on the implant success rate. The results showed that dynamic loading produced higher maximum stress than static loading and had a greater effect on the stress range as the elastic modulus varied. Bulaqi et al. [
44] showed that for short dental implants subject to dynamic loads, a greater crown height space (CHS) contributed to screw loosening and fatigue fracture. Kayabaşi et al. [
51] showed that for dental implants with a buttress thread shape, dynamic loading increased the stress within the implant by as much as 10–20%.
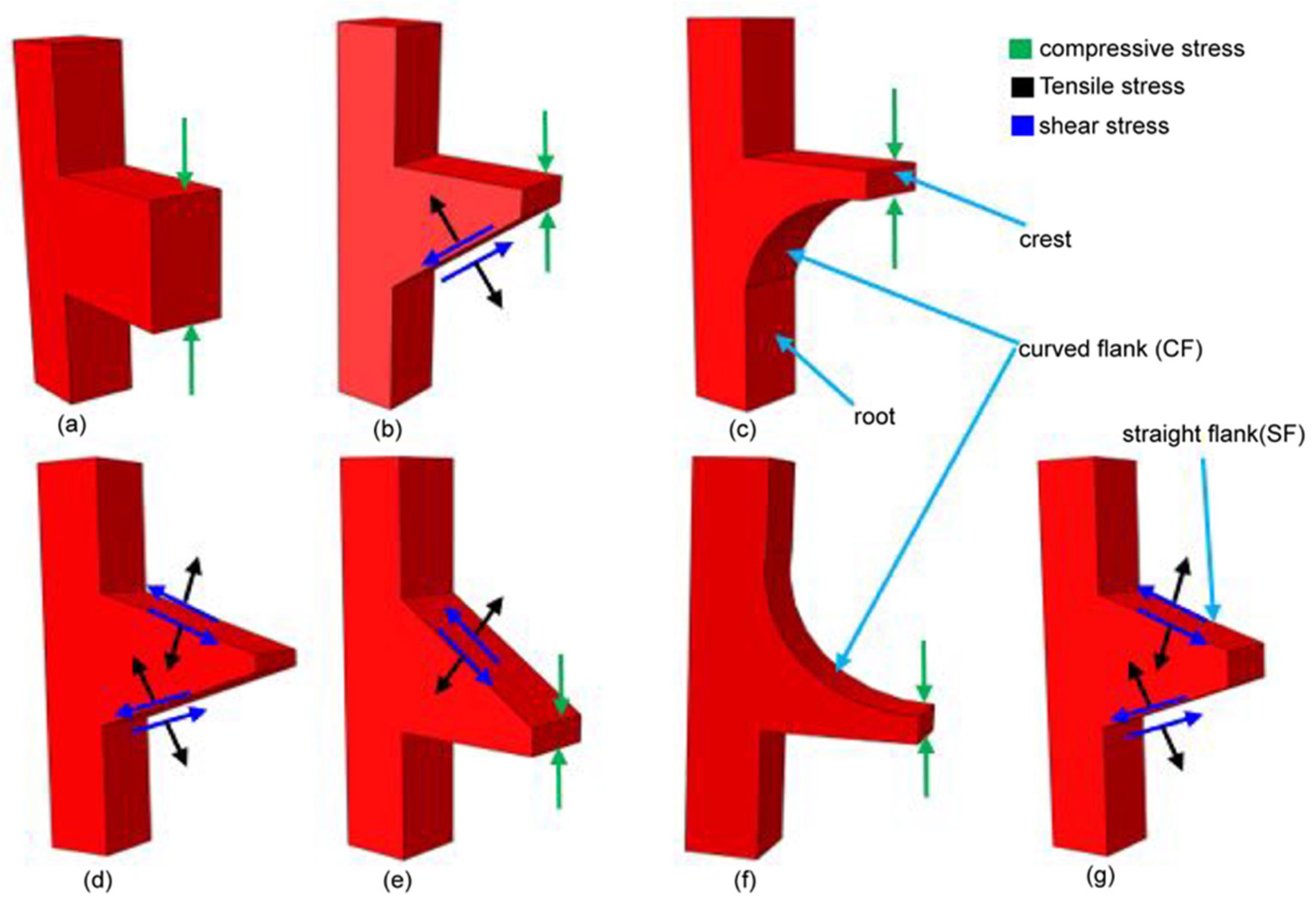
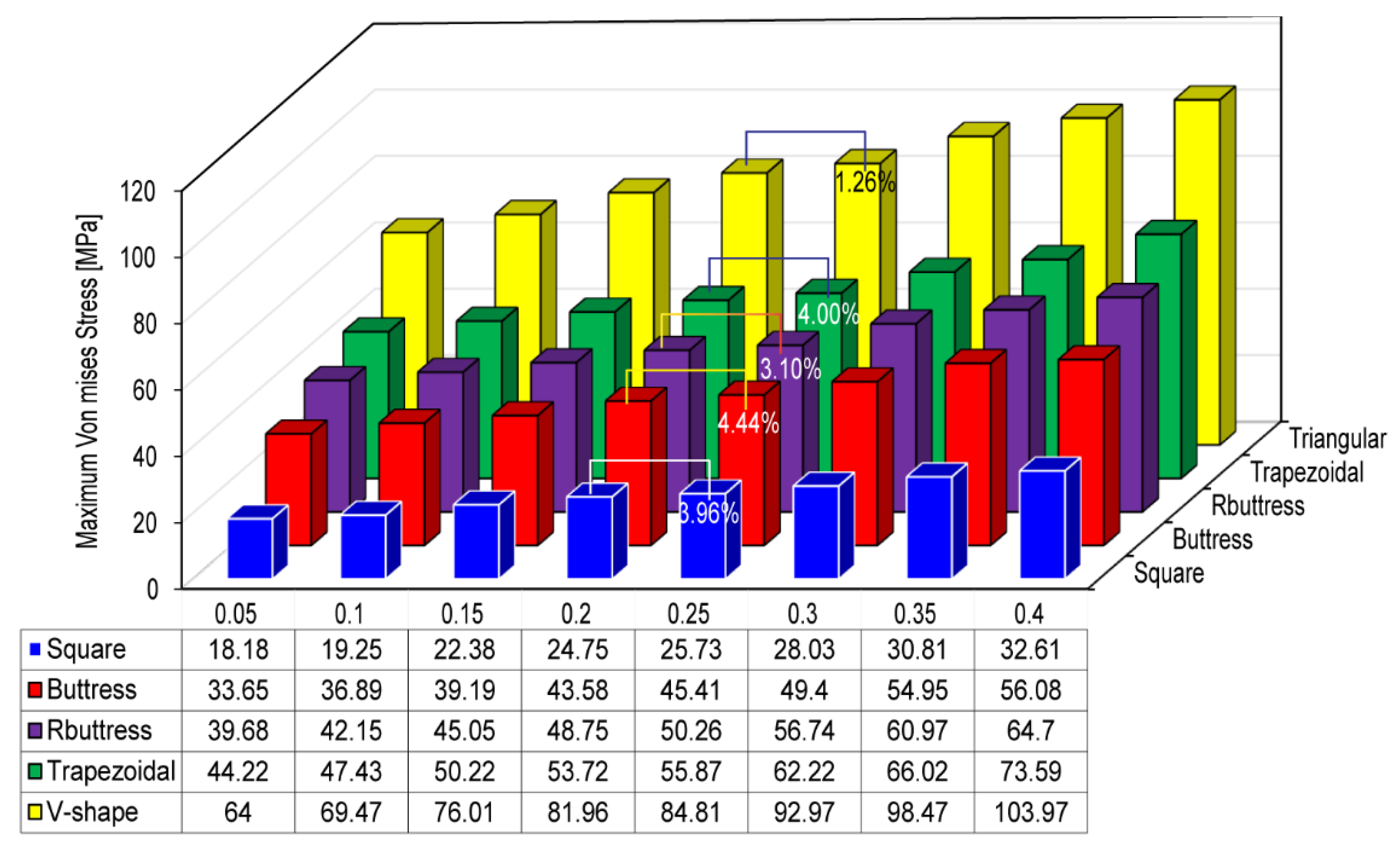
The shape of the implant thread has a significant effect on both the stress distribution within the implant and the marginal bone rehabilitation [
10]. Accordingly, an appropriate design of the thread pattern is essential to improve the uniformity of the stress distribution and reduce the stress intensity at the bone-implant interface (BII) [
13,
52]. Mosovar et al. [
37] examined the effects of four different thread shapes on the stress distribution in the anisotropic bone under static loading conditions and found that a square thread resulted in improved performance. Many thread designs are available for dental implants, including square, triangular, buttress, reverse buttress, and trapezoidal. The thread design and associated parameters (e.g., face angle, thread width, thread pitch, and so on) have a critical effect on both the type of force produced at the BII (i.e., tensile, compressive, or shear) and the efficiency with which the load is transferred to the bone [
37,
53]. For example, triangular threads generate a higher shear force, while square-shaped threads produce a lower shear force and higher compressive force [
52]. For square and buttress threads, the axial load is dissipated mainly through compressive forces [
37,
54,
55]. However, for triangular and reverse buttress threads, the load is transferred through a combination of shear forces, compressive forces, and tensile forces [
53]. Among the various thread designs, the square design reduces the maximum von Mises stress [
56]. Albrektsson et al. [
57] showed that the stress concentration of dental implants can be further reduced by curving the tops of the threads. Hansson and Werke [
52] similarly showed that the maximum stress induced in the bone, and the ability of the implant to bear the load depends not only on the thread design (e.g., triangular, square, buttress, and so on) but also on the detailed parameters of the thread design, including the pitch, thread width, and face angle.
The bone material property also has an important effect on the stress distribution in dental implant systems. However, the accurate modeling of bone-related organs using finite element modeling (FEM) methods is challenging due to their inherent inhomogeneous and anisotropic characteristics [
1,
4,
37,
58]. As a result, almost all previous studies consider the implanted bone to be isotropic, homogeneous, and linearly elastic [
3,
4,
25,
41,
59,
60,
61,
62,
63]. However, such a simplification results in significantly lower stress predictions for the peri-implant bone than those observed in practice [
8]. Consequently, the usefulness of the simulation results for practical clinical purposes is greatly impaired.
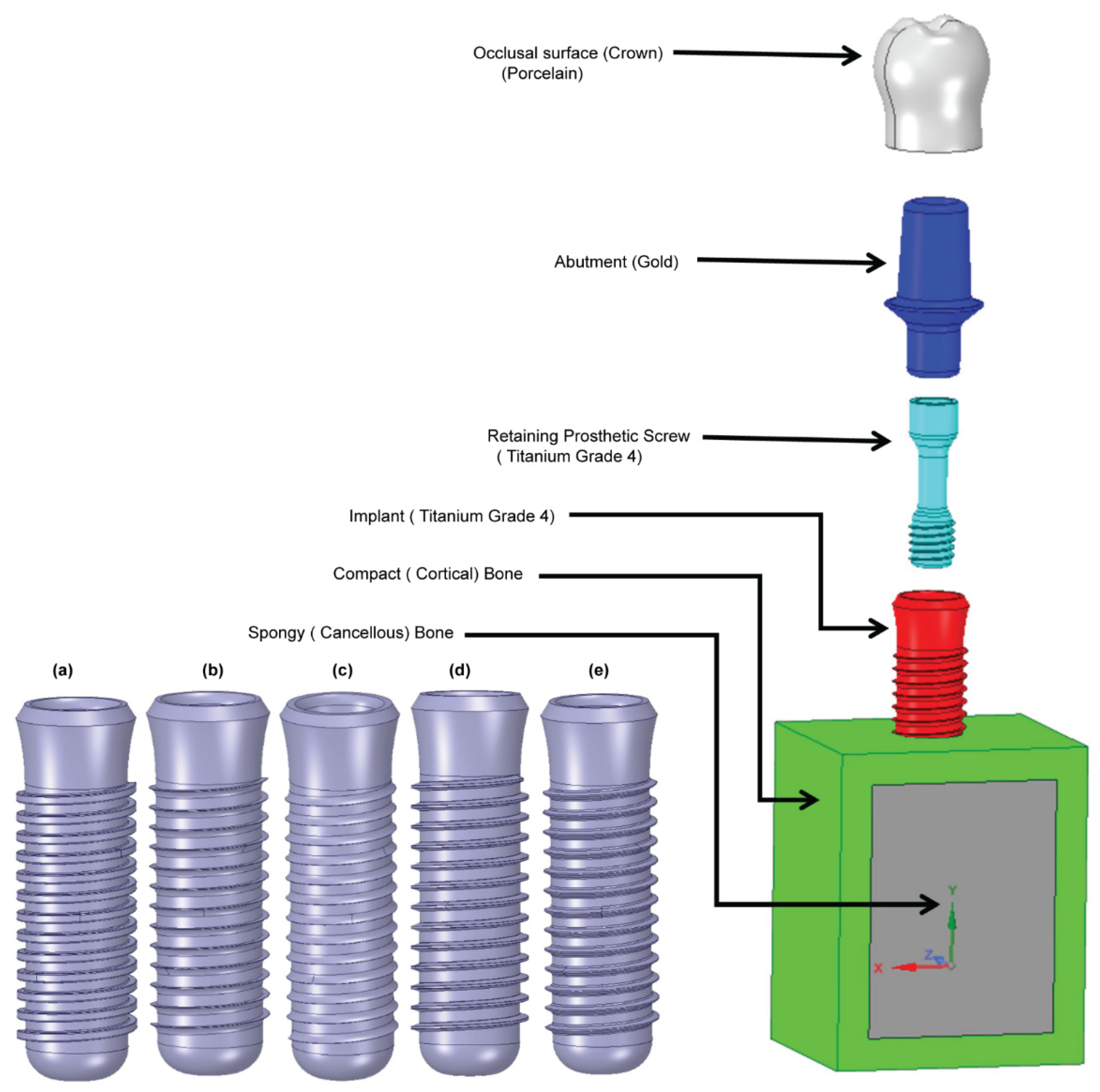
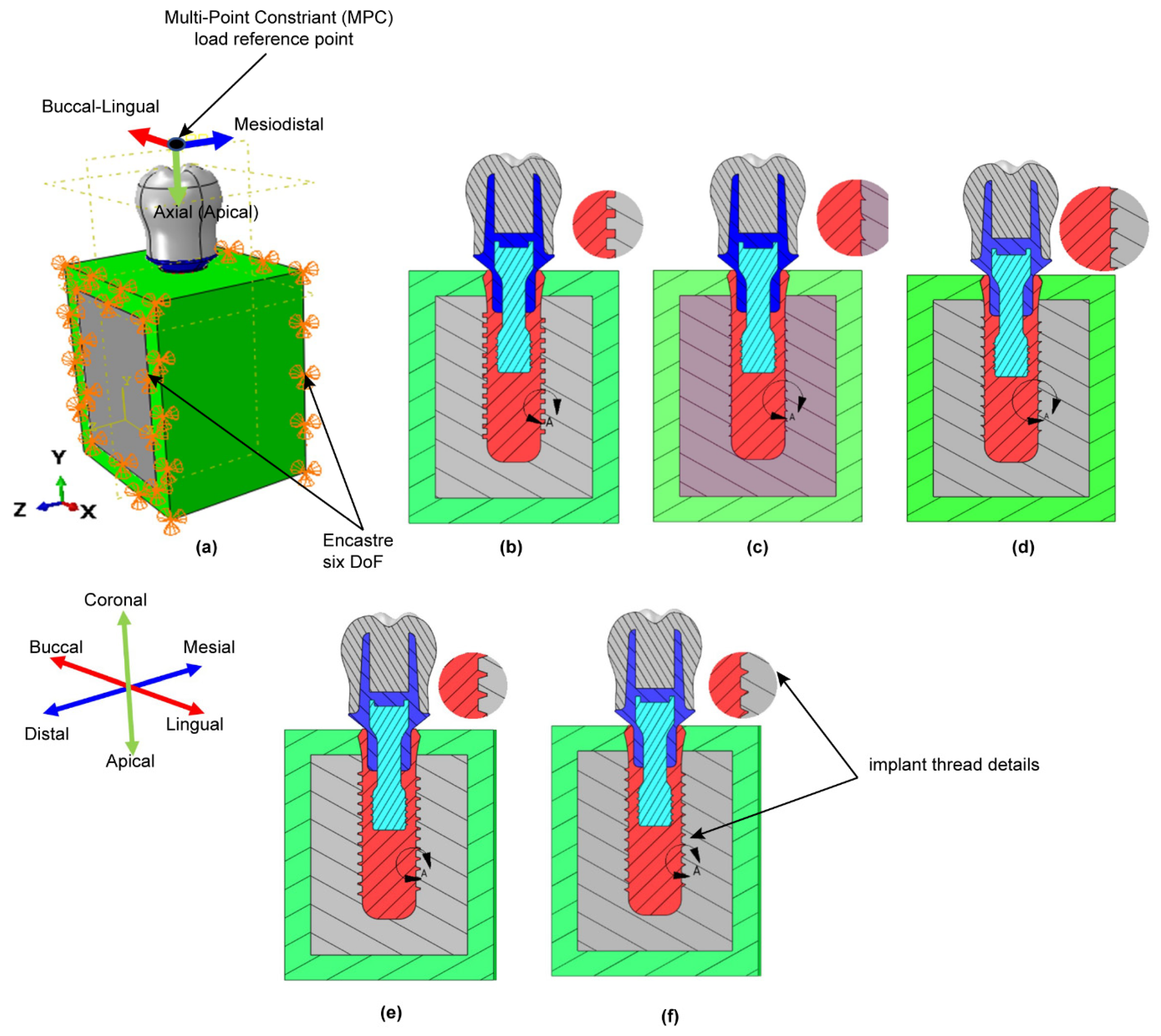
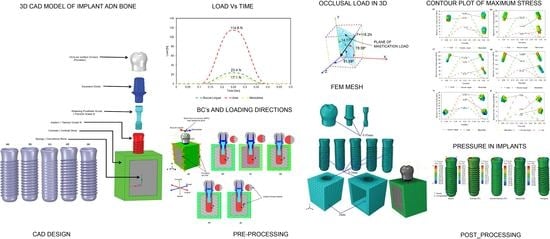
This study aims to investigate the biomechanical behavior of five dental implants with varied thread designs when loaded under three different loading rates, as well as the impact on implant stress distribution and surrounding anisotropic bone. Additionally, we will investigate whether dynamic load will noticeably increase stresses and deformation in all five implant models and bone compared to static and quasi-static loading conditions.
4. Discussion
Based on the ONE WAY ANOVA statistical analysis result
p-value was greater than 5%, indicating that the result is statistically non-significant (
Table 3). In other words, there is a remarkable increase in stress magnitude in the case of dynamic loading compared to that of quasi-static and static loading conditions in all five implant models. Also from the FEA result and based on the approach used in this study, the dynamic load applied to the crown surface increased the stresses by 30–60% compared to unrealistic (static) loading (
Table 4,
Table 5 and
Table 6) which is highly significant. Dynamic mechanical loading can damage the surface morphology and chemistry of dental implants [
68] and can result in the penetration of micro-organisms down to the threaded region of the fixture-abutment interface [
69]. Furthermore, cyclic loading can increase the stress induced in the implant by around 10–20% compared to that observed under static loading [
51]. Previous studies have shown that the stress induced in the implant and surrounding bone region depends not only on the nature of the applied load (i.e., static or dynamic) but also on the design of the implant thread [
70,
71].
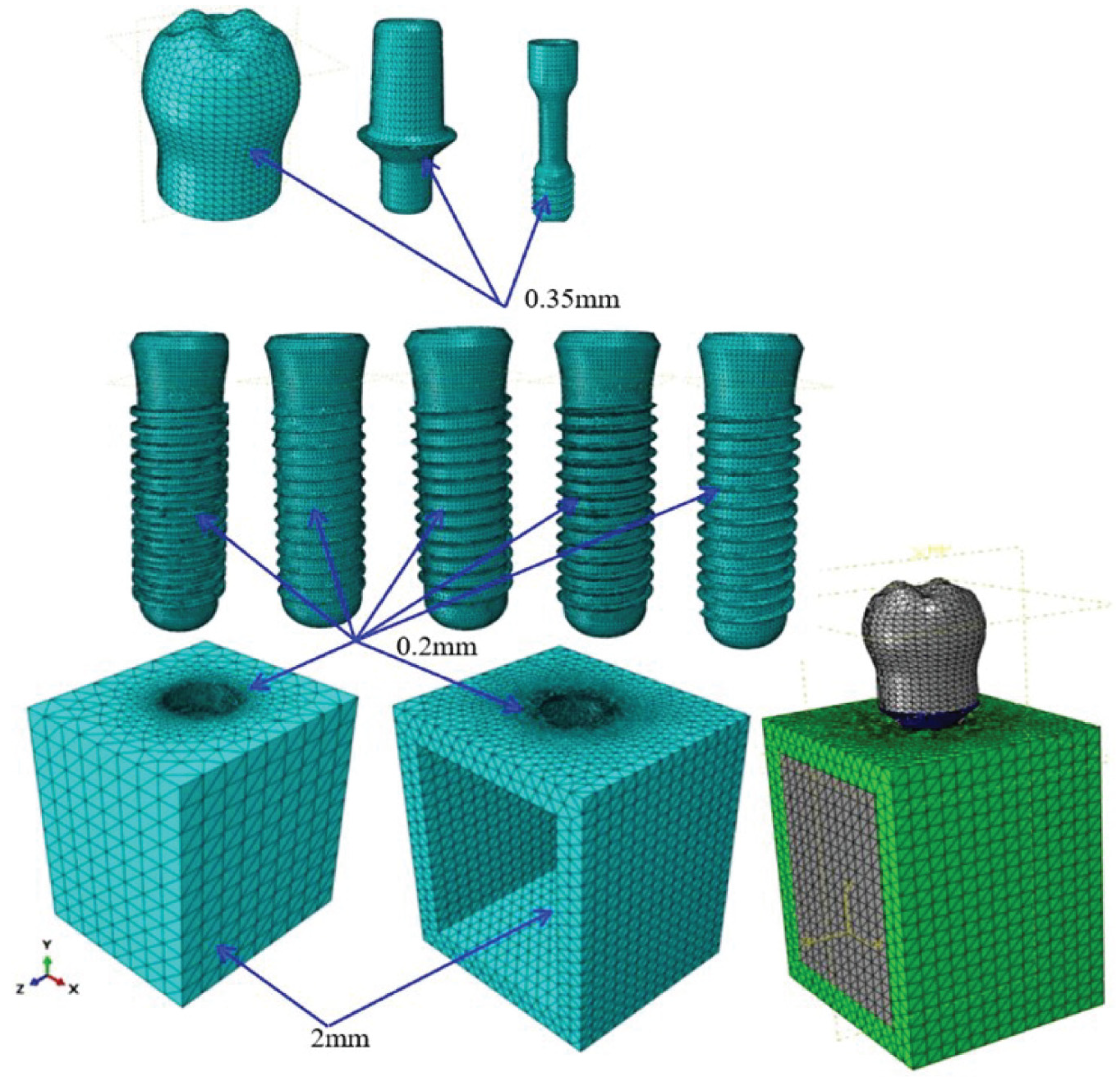
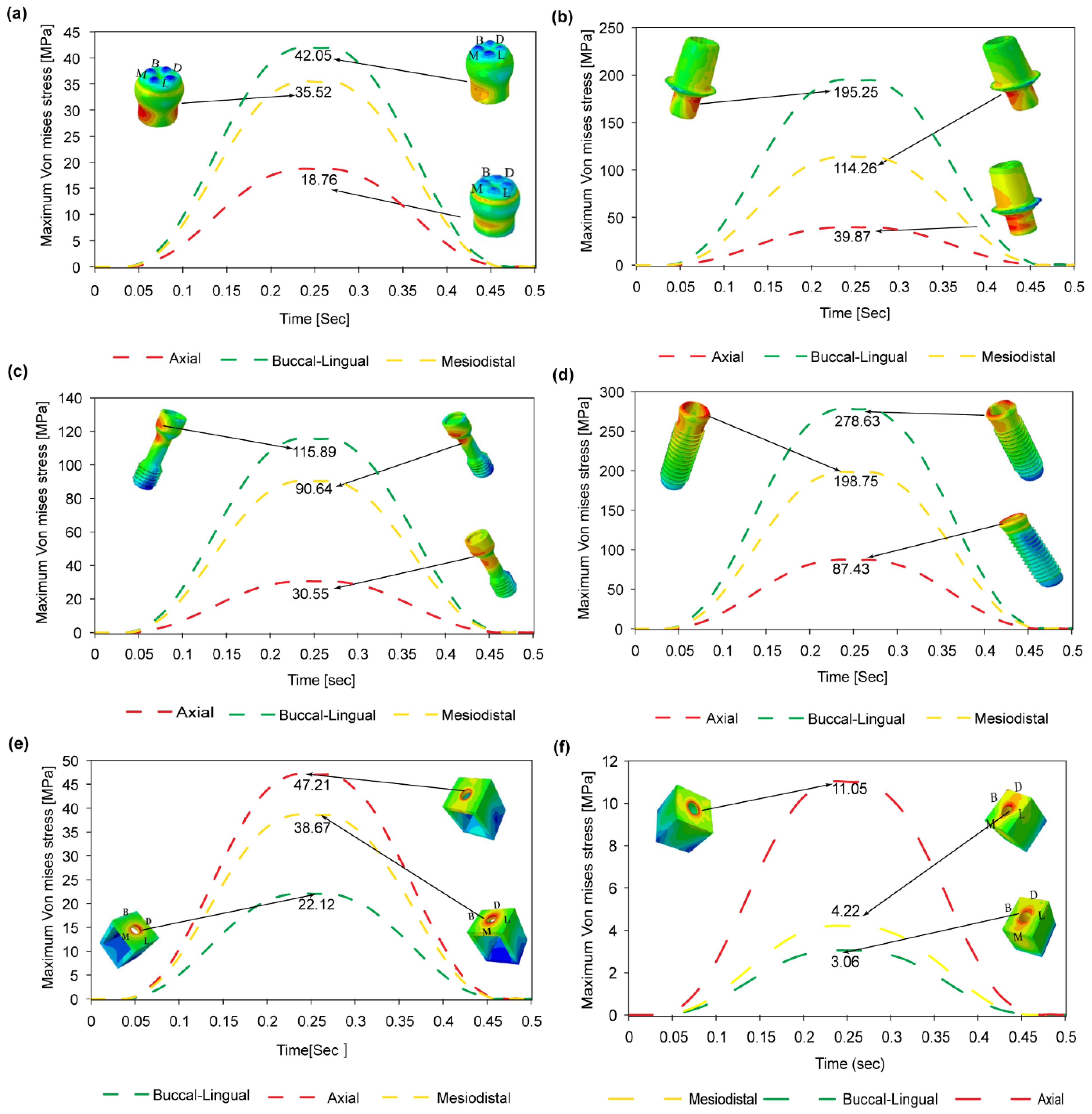
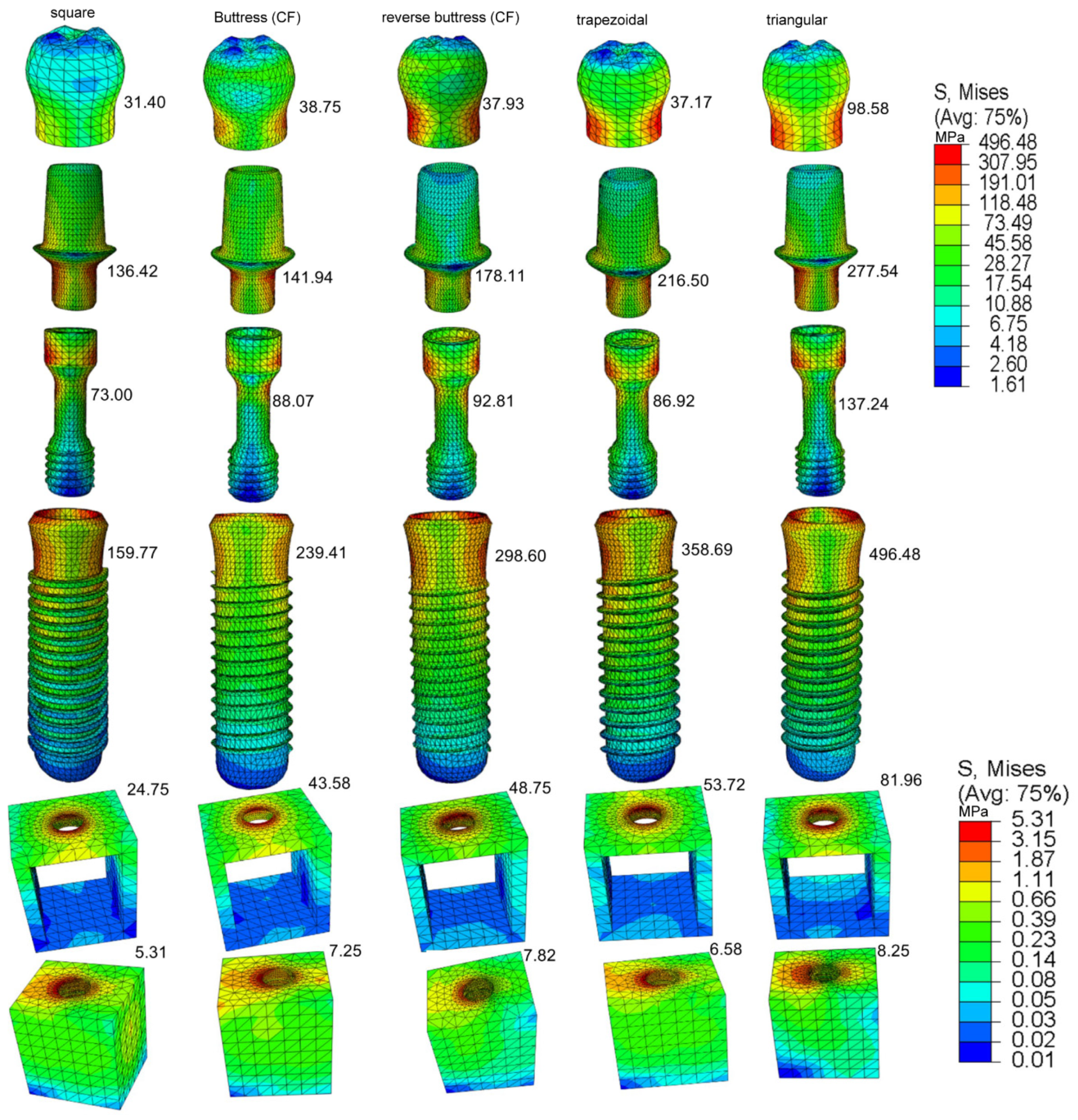
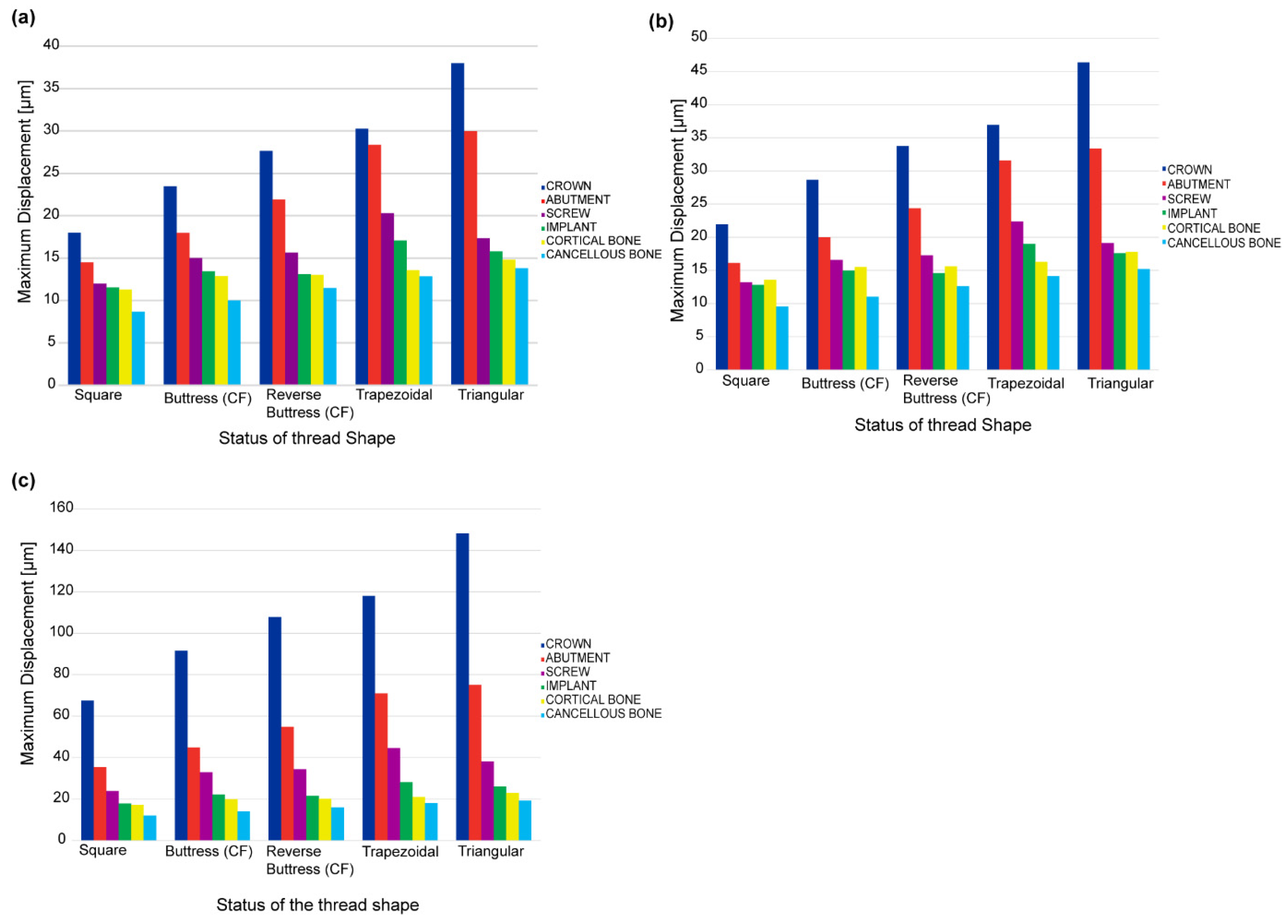
It has been shown that for all five thread design models, the von Mises stress, shear stress, compressive stress, and displacement all increase significantly under a dynamic load compared to a static or quasi-static load. However, little difference has been observed in the stress response of the implant under static and quasi-static loads, respectively. In general, the results have shown that the maximum stress is concentrated in the contact areas of the implant-bone models, e.g., at the abutment-screw, abutment-implant, and bone-implant interfaces (see
Figure 7 and
Figure 9). Accordingly, for all thread designs, there is a risk of micromotion, which may cause screw loosening, crestal bone loss, and implant fracture. The present results have shown that, under dynamic loading, the maximum von Mises stress in the prosthetic components is higher under buccal-lingual loading than under axial or mesiodistal loading (see
Figure 7a–d). By contrast, in the cortical and spongy bone regions, the maximum von Mises stress is produced under axial compressive loading (see
Figure 7e,f). In the case of trabecular bone, its yield strength threshold is exceeded under dynamic stress in the axial direction. This increase indicates that trabecular tissue yield strength is higher in compression than in tension. This could result in bone resorption and mineral redistribution to help with bone remodeling. Due to higher stress carrying in the implant, followed by cortical bone, the Von Mises stress is lower in spongy bone for all loading rates.
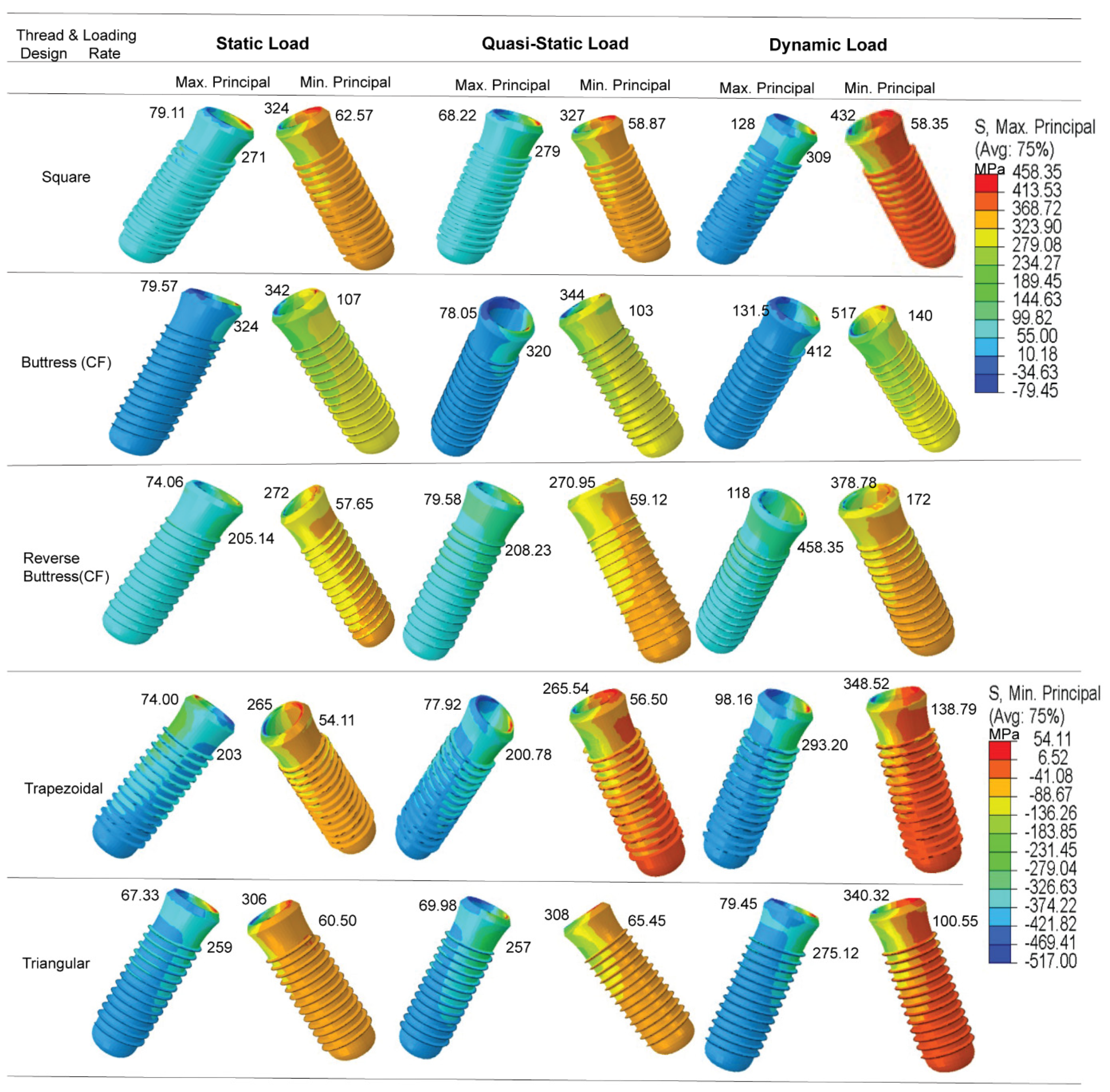
The results presented in
Figure 9b have shown that the maximum principal stress is concentrated in the first thread of the implant in the tip bevel region where it contacts the crestal part of the cortical bone. This prediction is consistent with the findings of Sun et al. [
72] that the abutment screw commonly breaks at the first thread and the implant breaks in the neck region. The simulation results obtained for the maximum shear stress (
Table 6) have shown no significant differences in the stress response behaviors of the five thread models under static loads and quasi-static loads, respectively. However, for each model, the stress increases significantly under dynamic loading. When all implant models were considered, it increased by 30–60% (see
Table 4 and
Figure 9c). This is extremely important because it implies that such cyclic loading rates must be closely monitored, since they may cause implant and bone fatigue and fracture. Many previous studies have reported that dynamic loading can have a greater effect on the implant success rate than static loading. For example, Yagihara et al. [
65] found that the attachment strength was significantly improved following the application of a dynamic load for four weeks compared to that obtained under a static load after four or eight weeks. Likewise, Duyck et al. [
73] reported that under dynamic stress situations, peri-implant bone resorption performance in rabbit tibias was significantly better than it was under static load scenarios.
Furthermore, previous studies have generally considered only a static masticatory load, [
37,
74,
75,
76,
77,
78,
79,
80,
81,
82]. However, in addition to static load, the current study considered quasi-static and dynamic loading rates. As a result, this research yields better results and a more reliable conclusion. This also reveals that dynamic loading considerably increases stress in all five models and cortical bone, potentially leading to bone fatigue and fracture. The results obtained in the present study have shown that the application of dynamic loading can increase the stress of dental implants and cortical bone by as much as 30–60% compared to static loading (see
Table 4 and
Figure 9c). This percentage increment is obtained when considering all the five implant models. And most importantly, including buttress and reverse buttress implants with CF thread profiles. Kayabaşi et al. [
51] considered only a single dental thread design (reverse buttress), whereas the present study has considered five different models. The present results have shown that while dynamic loading yields an effective increase in the compressive stress in the implant and bone region and is therefore beneficial in improving the implant success rate, the thread design should be carefully chosen to avoid failure in the first thread region of the implant.
The FEA results obtained in the present study have shown that, for all the loading rates and thread designs, the maximum von Mises stress is concentrated in the implant region of the prosthetic (see
Table 4 and
Figure 9c). As a result, the minimum stress is transferred to the bone, and the uniformity of the stress distribution within the bone is improved. The present results are thus in good general agreement with those of previous studies [
37,
51,
83,
84,
85,
86]. However, most previous studies did not consider the crown and abutment screw components of the prosthetic [
37,
83,
85,
86], and hence, the clinical application of the FEA findings is somewhat limited. Adding the mechanical retaining screw and occlusal surface enhanced the reliability of the result from FEM and mimicking the clinical situation during mastication load is applied by the patient.
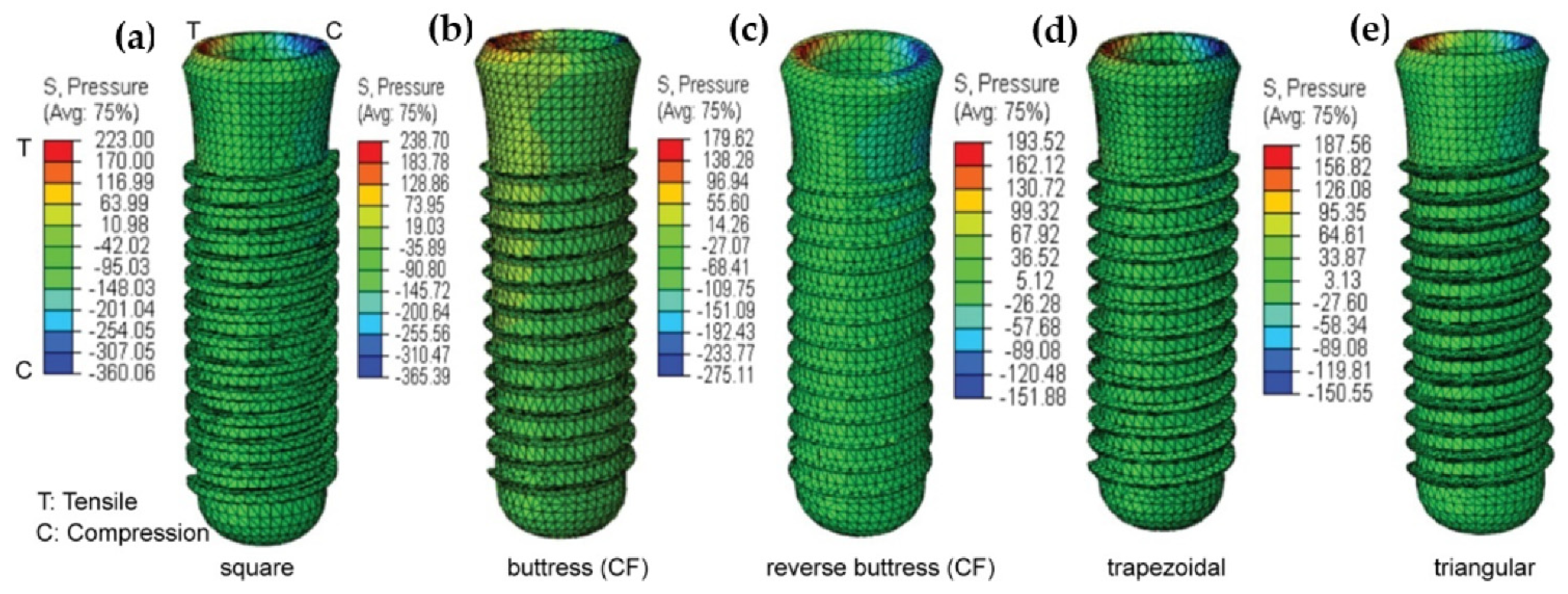
The present results have shown that the implant thread design affects both the magnitude and the distribution of the stress induced in the cortical bone under all three loading rates (see
Table 4 and
Figure 9c). They are thus in good agreement with the findings of Hansson and Werke [
52]. In particular, the results have shown that for the buttress and reverse buttress thread models, the application of curved flanks reduces the maximum von Mises stress by up to 50% compared to straight flanks (
Table 5), curved flank provides more bone contact area by decreasing the shear stress and tensile stress. Hence, more bone contact area has been proven to offer increased initial stability and stress resistance [
87]. Among the various thread designs considered in the present study, the square thread design results in the lowest von Mises stress, shear stress, and displacement, and the highest compressive stress (see
Figure 8 and
Figure 9b,
Table 4 and
Table 6). In general, the masticatory load acting on the crown occlusal surface results in three different stresses, namely tensile, compressive, and shear. Tensile stresses tend to pull objects apart, and if it becomes more than the yield strength, it may cause failure in implant and bone loss, while shear forces promote sliding. By contrast, compressive stresses maintain the integrity of the bone-implant interface. Furthermore, cortical bone is the strongest in compression and the weakest in shear [
88]. Thus, the present results suggest that the square thread design, which enhances the compressive stress, is the most suitable for dental implant applications. However, the buttress and reverse buttress designs with curved flanks also reduce the tensile and shear stress, while also promoting compressive stress (see
Figure 9 and
Table 5). Consequently, the buttress thread designs with curved flanks also represent a favorable design for dental implants. Furthermore, for each design, the maximum displacement, von Mises stress, and shear stress are significantly lower in the spongy bone region than in the cortical bone region (see
Figure 8 and
Figure 9, and
Table 6).
The other factor that directly affects the biomechanical behavior of dental implants is a bone material property. Unlike this study, most previous studies considered bone as an isotropic model. Martins et al. designed 2D computational axisymmetric models of isotropic bone implants and used varied thread profile shapes to anticipate the effect of material stiffness in dental implants [
16]. However, human bone is appearing to be highly anisotropic and is directional dependent. Consequently, for the case of isotropic bone, the resulting stress and strain from the FEM might not represent the actual stress during clinical service. Anisotropy, according to O’Mahony et al. [
89], would increase the already high levels of stress and strain in the cortical crest by 20 to 30% in the isotropic scenario. And further reported, anisotropy increased what were previously minimal levels of interface tensile and radial-hoop shear stresses in cancellous bone by three to four times along the lingual side, exceeding bond strength [
89]. And As per Xi et al., percentage increases in maximum stresses of cortical bone surrounding implant in the orthotropic model were up to 13.2 percent higher than those in the functionally isotropic model, but those on the cancellous bone surrounding implant were up to 226.7 percent higher [
90]. The findings of this study are consistent with previous research results.
Although FEM is a powerful and efficient way to solve biomechanical problems, there are limitations during the analysis of this study. Dynamic analysis in this study is computationally intensive both in terms of calculation time and computer memory usage. It is a heavy task for the testing of the convergence for different element sizes against maximum stress. Quad finite element type yields excellent FEM outcome with less numerical error. But our study has employed modified quadratic tetrahedral finite element type with 10-nodes (C3D10M) due to the complexity of the implant geometry and 3D model, limited computer RAM, and convergence time.