Bonding States of In Vitro Class 2 Direct Resin Composite Restoration Applied by Various Incremental Techniques
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Material
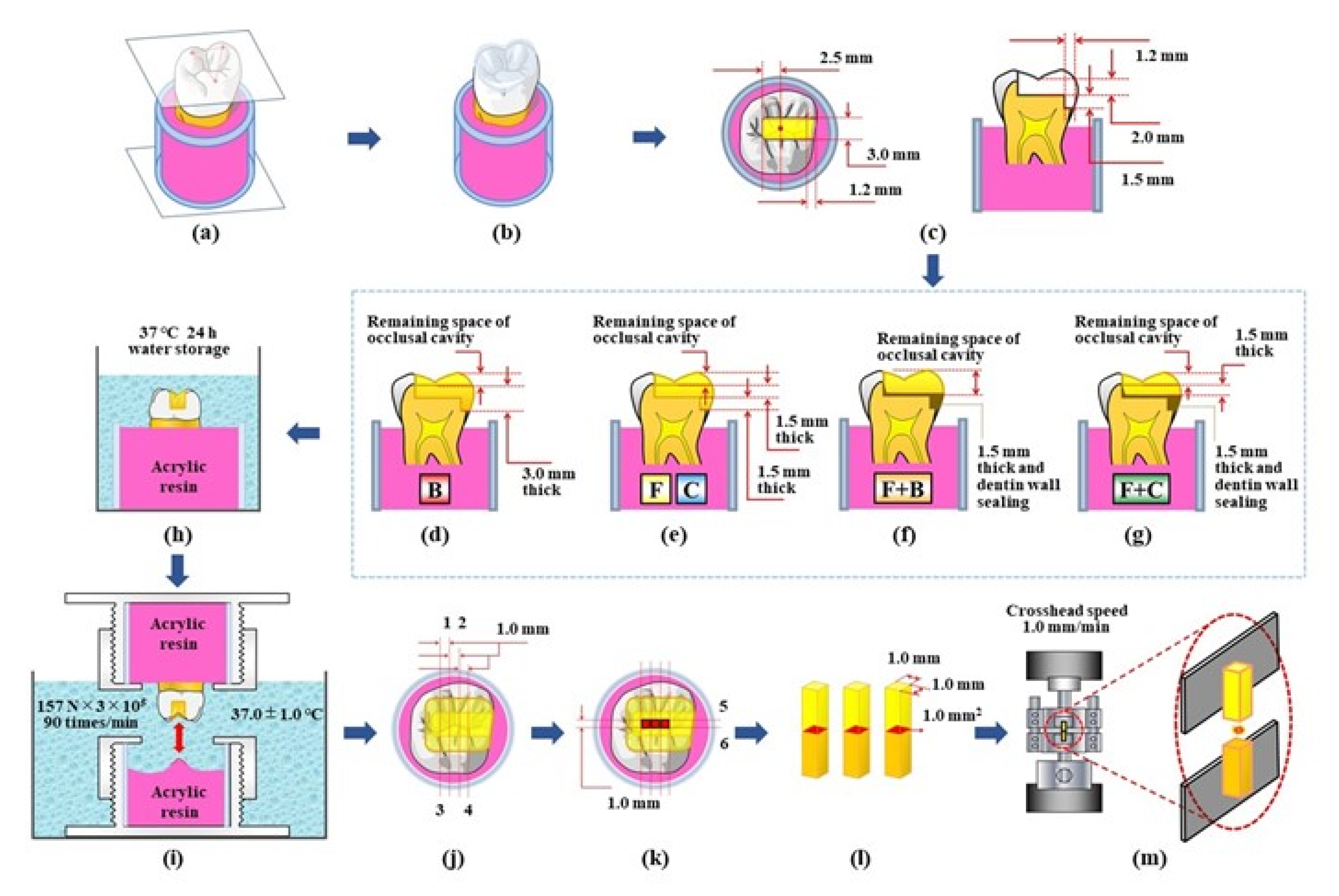
2.2. Tooth Selection and Experimental Procedures
2.3. Cyclic Loading and Micro-Tensile Bond Strength Test
2.4. Statistical Analysis
2.5. Fracture Mode Observation
2.6. Basic Physical Properties of Three Resin Composite Materials
3. Results
3.1. Differences in the Mean Values of µ-TBS among Five Types of Resin Restoration
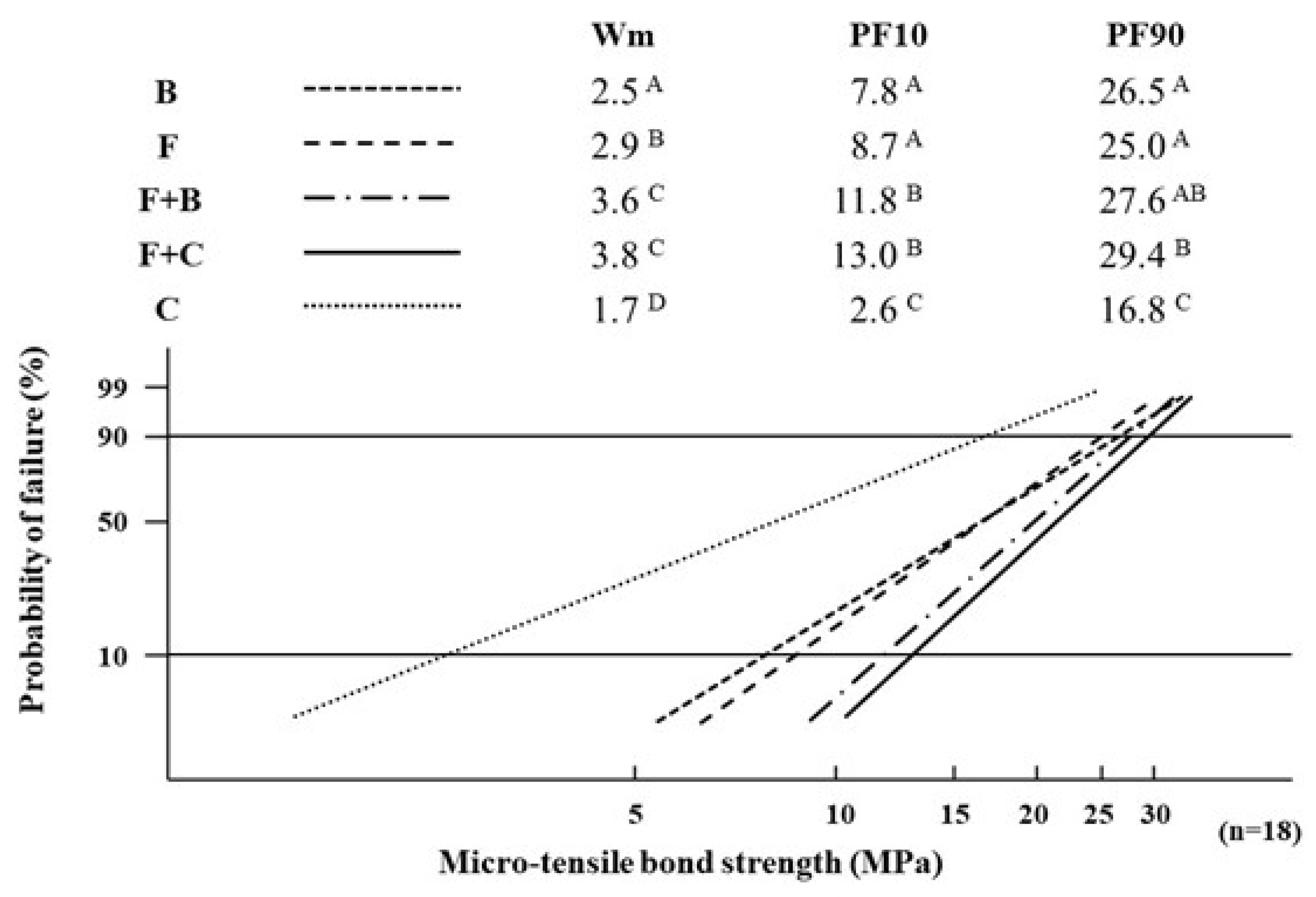
3.2. Differences in the Values of Weibull Parameters among Five Types of Resin Restoration
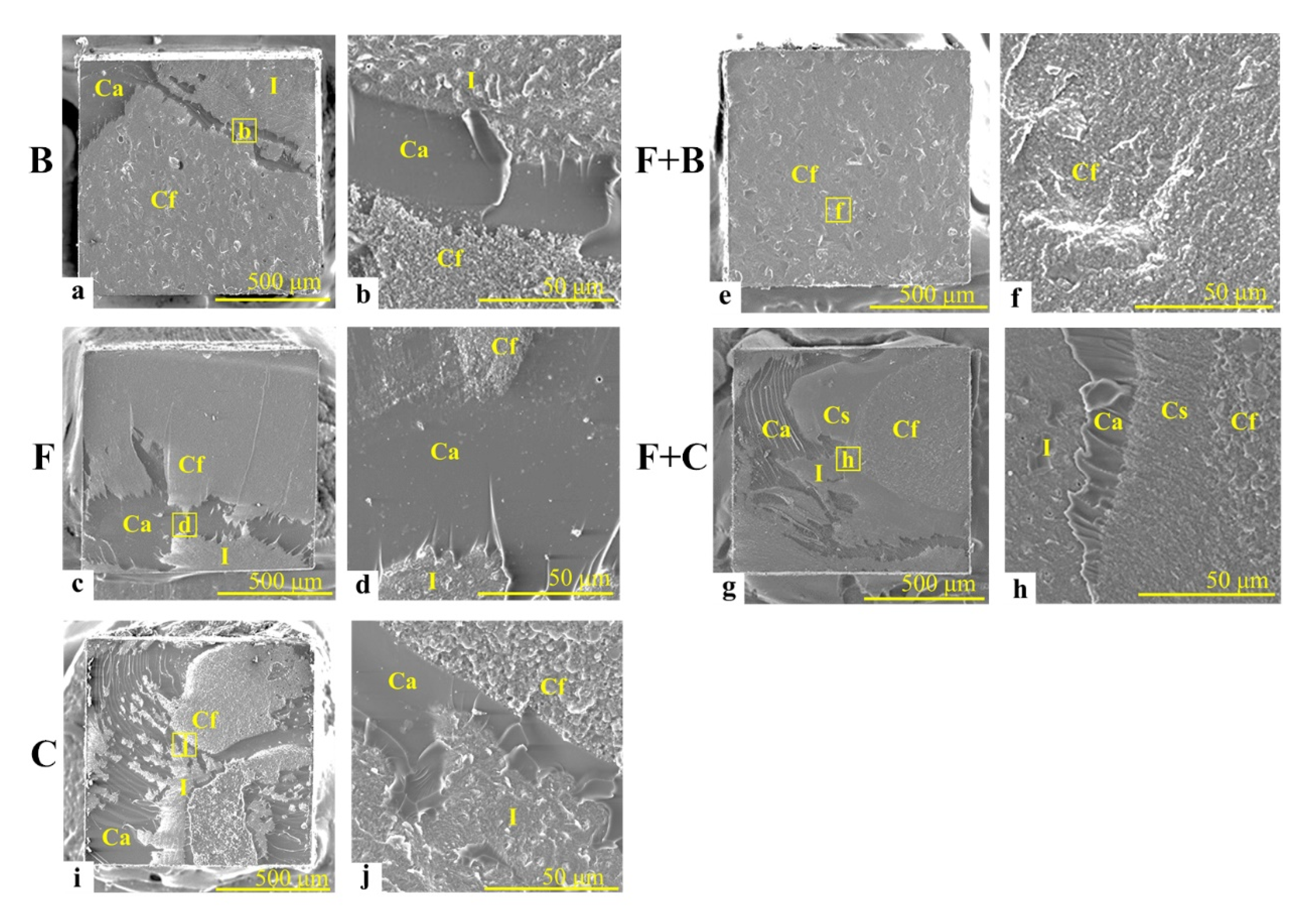
3.3. Fracture Mode Distribution of the Post-bond Test Specimens
3.4. Basic Properties of Three Resin Composite Materials
4. Discussion
4.1. Differences in the Mean Values of µ-TBS among Five Types of Resin Restoration
4.2. Differences in the Values of Weibull Parameters among Five Types of Resin Restoration
4.3. Fracture Mode Distribution of the Measured Specimens
5. Conclusions
- (1)
- Single-resin incremental restorations with a bulk-fill resin composite (B) or a flowable resin composite (F) and bi-resin incremental restorations with F + B and F + C demonstrated superior quantitative and qualitative abilities in achieving the bond strength, bonding reliability, and durability compared with single-resin incremental restorations with the conventional resin composite C (as control)
- (2)
- The bi-resin incremental restorations with F + B and F + C, where F was employed as the first-layered restorative, indicated excellent performance in bonding reliability and durability compared with the single-resin incremental restorations with B, F, and C
- (3)
- F + C-restoration, which indicates not only the maximum mean µ-TBS, but also the highest values of the Weibull parameters, supplied the most appropriate bonding states within the five types of resin restoration.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FDI World Dental Federation. FDI policy statement on Minimal Intervention Dentistry (MID) for Managing Dental Caries. Int. Dent. J. 2017, 67, 6–7. [Google Scholar] [CrossRef]
- Ritter, A.V.; Boushell, L.W.; Walter, R. Sturdevant’s Art and Science of Operative Dentistry, 7th ed.; Elsevier: St. Louis, MO, USA, 2019; pp. 175, 469–473. [Google Scholar]
- Lawson, N.C.; Radhakrishnan, R.; Givan, D.A.; Ramp, L.C.; Burgess, J.O. Two-year Randomized, Controlled Clinical Trial of a Flowable and Conventional Composite in Class I Restorations. Oper. Dent. 2015, 40, 594–602. [Google Scholar] [CrossRef]
- Ruivo, M.A.; Pacheco, R.R.; Sebold, M.; Giannini, M. Surface roughness and filler particles characterization of resin-based composites. Microsc. Res. Tech. 2019, 82, 1756–1767. [Google Scholar] [CrossRef]
- Ólafsson, V.G.; Ritter, A.V.; Swift, E.J., Jr.; Boushell, L.W.; Ko, C.C.; Jackson, G.R.; Ahmed, S.N.; Donovan, T.E. Effect of composite type and placement technique on cuspal strain. J. Esthet. Restor. Dent. 2018, 30, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.; Lima, D.A.N.L.; Giorgi, M.C.C.; Marchi, G.M.; Aguiar, F.H.B. Evaluation of Bond Strength, Nanoleakage, and Marginal Adaptation of Bulk-fill Composites Submitted to Thermomechanical Aging. J. Adhes Dent. 2019, 21, 255–264. [Google Scholar] [CrossRef]
- Al-Nahedh, H.N.; Alawami, Z. Fracture Resistance and Marginal Adaptation of Capped and Uncapped Bulk-fill Resin-based Materials. Oper. Dent. 2020, 45, E43–E56. [Google Scholar] [CrossRef] [PubMed]
- Rizzante, F.A.P.; Duque, J.A.; Duarte, M.A.H.; Mondelli, R.F.L.; Mendonça, G.; Ishikiriama, S.K. Polymerization shrinkage, microhardness and depth of cure of bulk fill resin composites. Dent. Mater. J. 2019, 38, 403–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, M.H. Update on Dental Nanocomposites. J. Dent. Res. 2010, 89, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Bayne, S.C.; Thompson, J.Y.; Swift, E.J., Jr.; Stamatiades, P.; Wilkerson, M. A characterization of first-generation flowable composites. J. Am. Dent. Assoc. 1998, 129, 567–577. [Google Scholar] [CrossRef]
- Rocha, G.T.C.; Rêgo, H.M.; Perote, L.C.; Santos, L.F.; Kamozaki, M.B.; Gutierrez, N.C.; Di, N.R.; Borges, A.B. A split-mouth randomized clinical trial of conventional and heavy flowable composites in class II restorations. J. Dent. 2014, 42, 793–799. [Google Scholar] [CrossRef]
- Hilton, T.J.; Ferracane, J.L.; Broome, J.C. Summitt’s Fundamentals of Operative Dentistry: A Contemporary Approach, 4th ed.; Quintessence Pub Co.: Hanover Park, IL, USA, 2013; p. 261. [Google Scholar]
- Lee, M.R.; Cho, B.H.; Son, H.H.; Um, C.M.; Lee, I.B. Influence of cavity dimension and restoration methods on the cusp deflection of premolars in composite restoration. Dent. Mater. 2007, 23, 288–295. [Google Scholar] [CrossRef]
- Park, J.; Chang, J.; Ferracane, J.; Lee, I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008, 24, 1501–1505. [Google Scholar] [CrossRef]
- He, Z.; Shimada, Y.; Tagami, J. The effects of cavity size and incremental technique on micro-tensile bond strength of resin composite in Class I cavities. Dent. Mater. 2007, 23, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, R.L.; Ferracane, J.L.; Powers, J.M. Craig’s Restorative Dental Materials, 14th ed.; Elsevier: St. Louis, MO, USA, 2019; pp. 35–36, 154–164. [Google Scholar]
- Banerjee, A.; Watson, T.F. Pickard’s Guide to Minimally Invasive Operative Dentistry, 10th ed.; Oxford University Press Inc.: New York, NY, USA, 2015; p. 112. [Google Scholar]
- Hardan, L.; Sidawi, L.; Akhundov, M.; Bourgi, R.; Ghaleb, M.; Dabbagh, S.; Sokolowski, K.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M. One-Year Clinical Performance of the Fast-Modelling Bulk Technique and Composite-Up Layering Technique in Class I Cavities. Polymers 2021, 13, 1873. [Google Scholar] [CrossRef]
- Scotti, N.; Cavalli, G.; Gagliani, M.; Breschi, L. New adhesives and bonding techniques. Why and when? Int. J. Esthet. Dent. 2017, 12, 524–535. [Google Scholar] [PubMed]
- Miyasaka, T.; Okamura, H. Dimensional change measurements of conventional and flowable composite resins using a laser displacement sensor. Dent. Mater. J. 2009, 28, 544–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Organization for Standardization. Dentistry: Polymer-Based Restorative Materials. ISO Standard No. 4049:2019. Available online: https://www.iso.org/standard/67596.html (accessed on 19 August 2021).
- Anderson, D.J. Measurement of stress in mastication. II. J. Dent. Res. 1956, 35, 671–673. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, C.; Relova-Quinterio, J.L. Mastication. In Oxford Handbook of Applied Dental Science; Scully, C., Ed.; Oxford University Press Inc.: New York, NY, USA, 2002; Chapter 11; pp. 149–156. [Google Scholar]
- Neill, D.J. Studies of tooth contact in complete dentures. Br. Dent. J. 1967, 123, 369–378. [Google Scholar]
- Shepherd, R.W. A further report on mandibular movement. Aust. Dent. J. 1960, 5, 337–342. [Google Scholar] [CrossRef]
- Sakaguchi, R.L.; Douglas, W.H.; DeLong, R.; Pintado, M.R. The wear of a posterior composite in an artificial mouth: A clinical correlation. Dent. Mater. 1986, 2, 235–240. [Google Scholar] [CrossRef]
- Ishii, N.; Maseki, T.; Nara, Y. Bonding state of metal-free CAD/CAM onlay restoration after cyclic loading with and without immediate dentin sealing. Dent. Mater. J. 2017, 36, 357–367. [Google Scholar] [CrossRef] [Green Version]
- Shinkai, K.; Suzuki, S. Effect of cyclic impact loading on the surface properties of flowable resin composites. Dent. Mater. J. 2014, 33, 874–879. [Google Scholar] [CrossRef] [Green Version]
- Weibull, W. A statistical Distribution Function of Wide Applicability. J. Appl. Mech. 1951, 18, 293–297. [Google Scholar] [CrossRef]
- International Organization for Standardization. Dentistry: Testing of Adhesion to Tooth Structure. ISO/TS Standard No. 11405:2015. Available online: https://www.iso.org/standard/62898.html (accessed on 19 August 2021).
- Robin, C.; Scherrer, S.S.; Wiskott, H.W.; de Rijk, W.G.; Belser, U.C. Weibull parameters of composite resin bond strengths to porcelain and noble alloy using the Rocatec system. Dent. Mater. 2002, 18, 389–395. [Google Scholar] [CrossRef]
- Inokoshi, M.; Kameyama, A.; De Munck, J.; Minakuchi, S.; Van Meerbeek, B. Durable bonding to mechanically and/or chemically pre-treated dental zirconia. J. Dent. 2013, 41, 170–179. [Google Scholar] [CrossRef]
- Kawai, T.; Maseki, T.; Nara, Y. Bonding of flowable resin composite restorations to class 1 occlusal cavities with and without cyclic load stress. Dent. Mater. J. 2016, 35, 408–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosa, L.L.; Bossardi, M.; Silveira, M.W.J.; Galbiatti, C.F.; Carlo, H.L.; Piva, E.; Münchow, E.A. New generation bulk-fill resin composites: Effects on mechanical strength and fracture reliability. J. Mech. Behav. Biomed. Mater. 2019, 96, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Gallo, S.; Poggio, C.; Ricaldone, V.; Arciola, C.R.; Scribante, A. New Resin-Based Bulk-Fill Composites: In Vitro Evaluation of Micro-Hardness and Depth of Cure as Infection Risk Indexes. Materials 2020, 13, 1308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lins, R.B.E.; Aristilde, S.; Osório, J.H.; Cordeiro, C.M.B.; Yanikian, C.R.F.; Bicalho, A.A.; Stape, T.H.S.; Soares, C.J.; Martins, L.R.M. Biomechanical behaviour of bulk-fill resin composites in class II restorations. J. Mech. Behav. Biomed. Mater. 2019, 98, 255–261. [Google Scholar] [CrossRef]
- Feilzer, A.J.; De Gee, A.J.; Davidson, C.L. Setting stress in composite resin in relation to configuration of the restoration. J. Dent. Res. 1987, 66, 1636–1639. [Google Scholar] [CrossRef]

| Resin Composite Material | Composition | Lot Number | Manufacturer | |
|---|---|---|---|---|
| Bulk-Fill resin composite [Code: B] | Tetric N-Ceram Bulk Fill (Shade: IVA) | Barium glass filler, Bis-EMA, Bis-GMA, UDMA, ytterbium trifluoride | Z001JF | Ivoclar vivadent |
| Flowable resin composite [Code: F] | G-aenial Universal Injectable (Shade: A2) | Barium glass filler, Bis-MEPP, Bis-EMA, bismethacrylate, dimethacrylate, UV-light absorber, UDMA, dimethacrylate component | 2003161 | GC |
| Conventional resin composite [Code: C] | Filtek Supreme Ultra Universal Restorative (Shade: A2) | Silane treated ceramic, Bis-EMA, Bis-GMA, UDMA, Silane treated silica, PEGDMA, Silane treated zirconia, Triethylene glycol dimethacrylate | NC00725 | 3M |
| Resin Adhesive System | Composition | Lot Number | Manufacturer | |
| All-in-one adhesive system | Prime & Bond universal | Phosphoric acid modified acrylate resin, Initiaor, Stabilizer, Multifunctional acrylate, Isopropanol, Bifunctional acrylate, Acidic acrylate, Water | 1909000418 | Dentsply Sirona |
| Classification | Fracture Mode Composition | Five Types of Class 2 Resin Composite Restoration | ||||
|---|---|---|---|---|---|---|
| B | F | F + B | F + C | C | ||
| Cohesive failure | Cf | 6 | 7 | 8 | 5 | 4 |
| Cs | — | — | 0 | 0 | — | |
| Interfacial failure | I | 1 | 0 | 0 | 0 | 0 |
| Mixed failure | CF + Cs | — | — | 4 | 2 | — |
| CF + Cs + Ca + I | — | — | 4 | 7 | — | |
| Cs + Ca + I | — | — | 2 | 4 | — | |
| CF + Ca + I | 11 | 11 | — | — | 14 | |
| Resin Composite Material | Linear Polymerization Shrinkage (%) | Flexural Strength (MPa) | Mean Value (SD) (n = 5) |
|---|---|---|---|
| Flexural Modulus (GPa) | |||
| B | 1.7 (0.3) A | 131.0 (11.7) A | 8.1 (0.9) A |
| F | 2.3 (0.2) B | 180.8 (22.6) B | 6.3 (0.9) B |
| C | 1.6 (0.3) A | 186.5 (18.1) B | 11.7 (0.9) C |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okada, M.; Maeno, M.; Nara, Y. Bonding States of In Vitro Class 2 Direct Resin Composite Restoration Applied by Various Incremental Techniques. Materials 2021, 14, 6037. https://doi.org/10.3390/ma14206037
Okada M, Maeno M, Nara Y. Bonding States of In Vitro Class 2 Direct Resin Composite Restoration Applied by Various Incremental Techniques. Materials. 2021; 14(20):6037. https://doi.org/10.3390/ma14206037
Chicago/Turabian StyleOkada, Misato, Masahiko Maeno, and Yoichiro Nara. 2021. "Bonding States of In Vitro Class 2 Direct Resin Composite Restoration Applied by Various Incremental Techniques" Materials 14, no. 20: 6037. https://doi.org/10.3390/ma14206037
APA StyleOkada, M., Maeno, M., & Nara, Y. (2021). Bonding States of In Vitro Class 2 Direct Resin Composite Restoration Applied by Various Incremental Techniques. Materials, 14(20), 6037. https://doi.org/10.3390/ma14206037





