The Development of Filler Morphology in Dental Resin Composites: A Review
Abstract
:1. Introduction
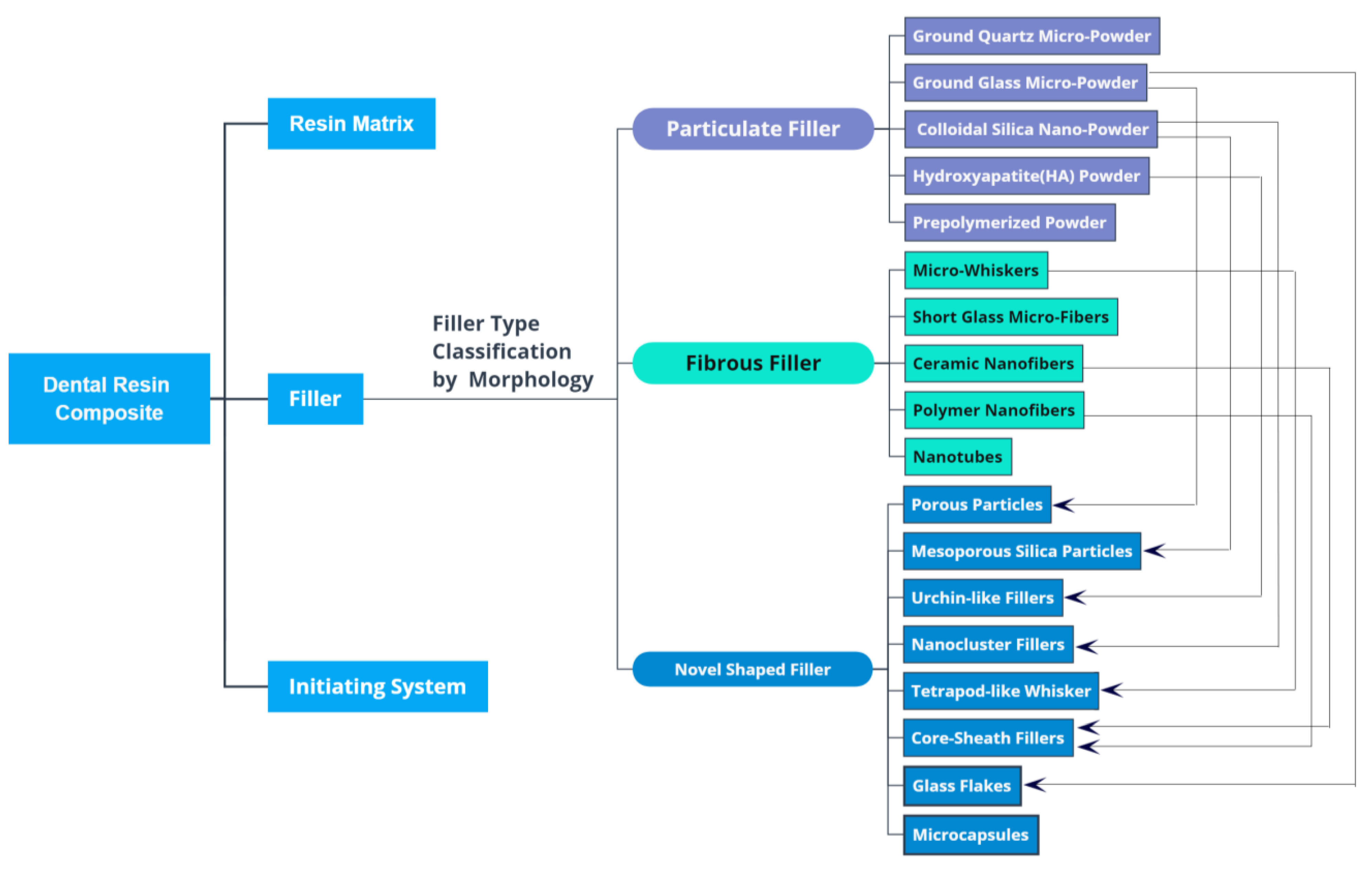
2. Filler Type Classification by Morphology
3. Particulate Fillers and Their Development
3.1. Ground Quartz Micropowder
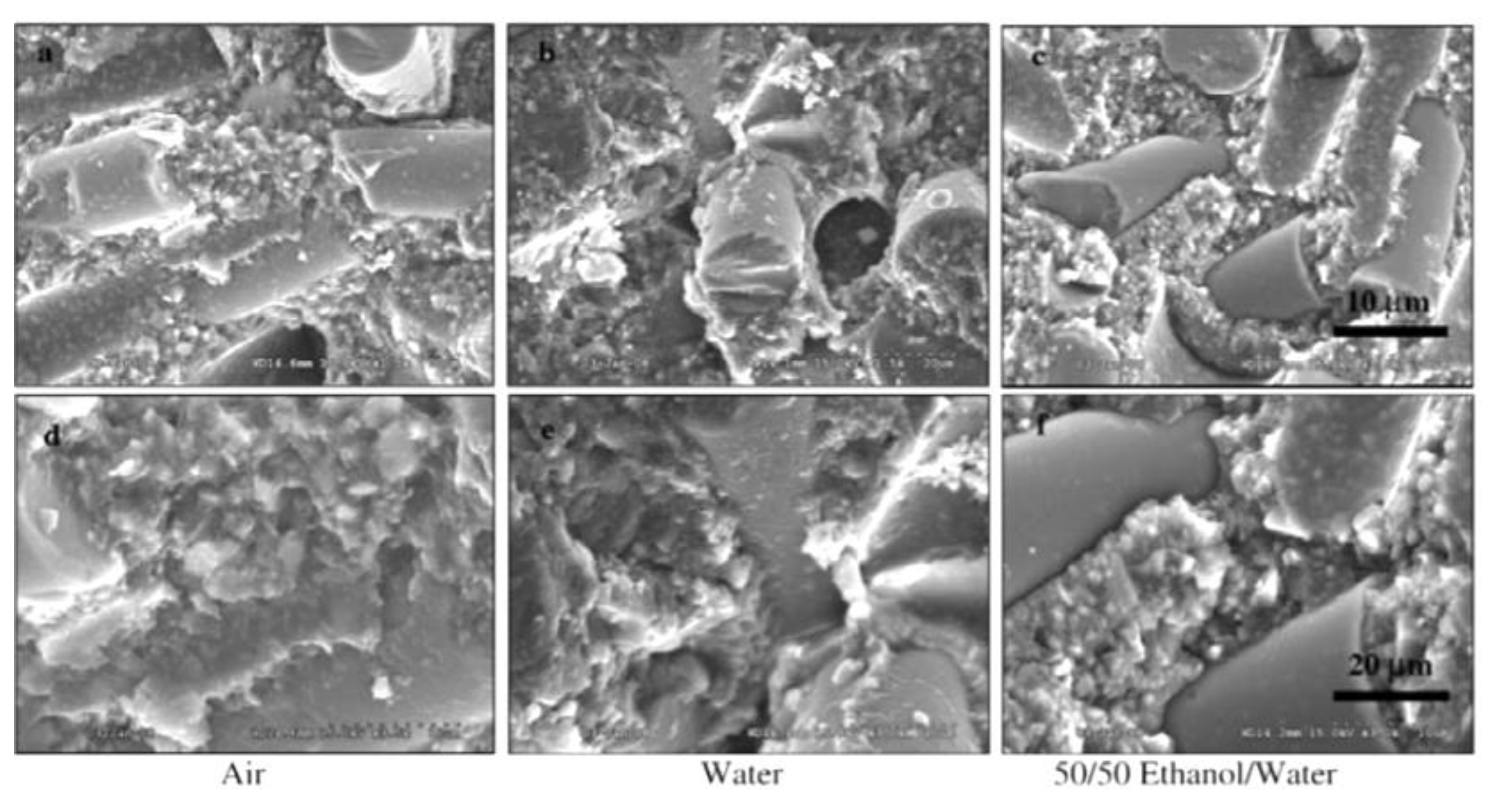
3.2. Ground Glass Micropowder
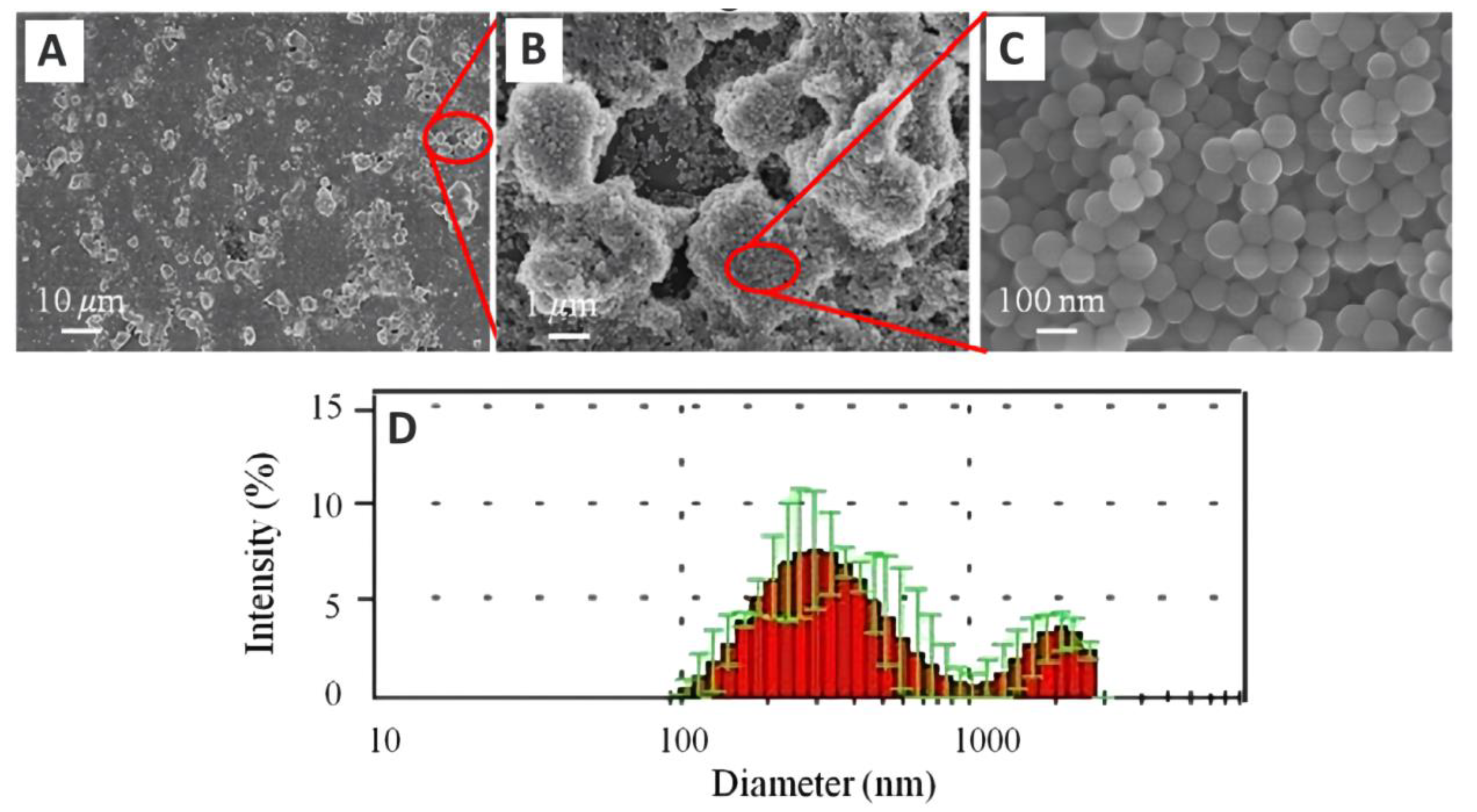
3.3. Colloidal Silica Nanopowder
3.4. Hydroxyapatite (HA) Powder
3.5. Prepolymerized Powders
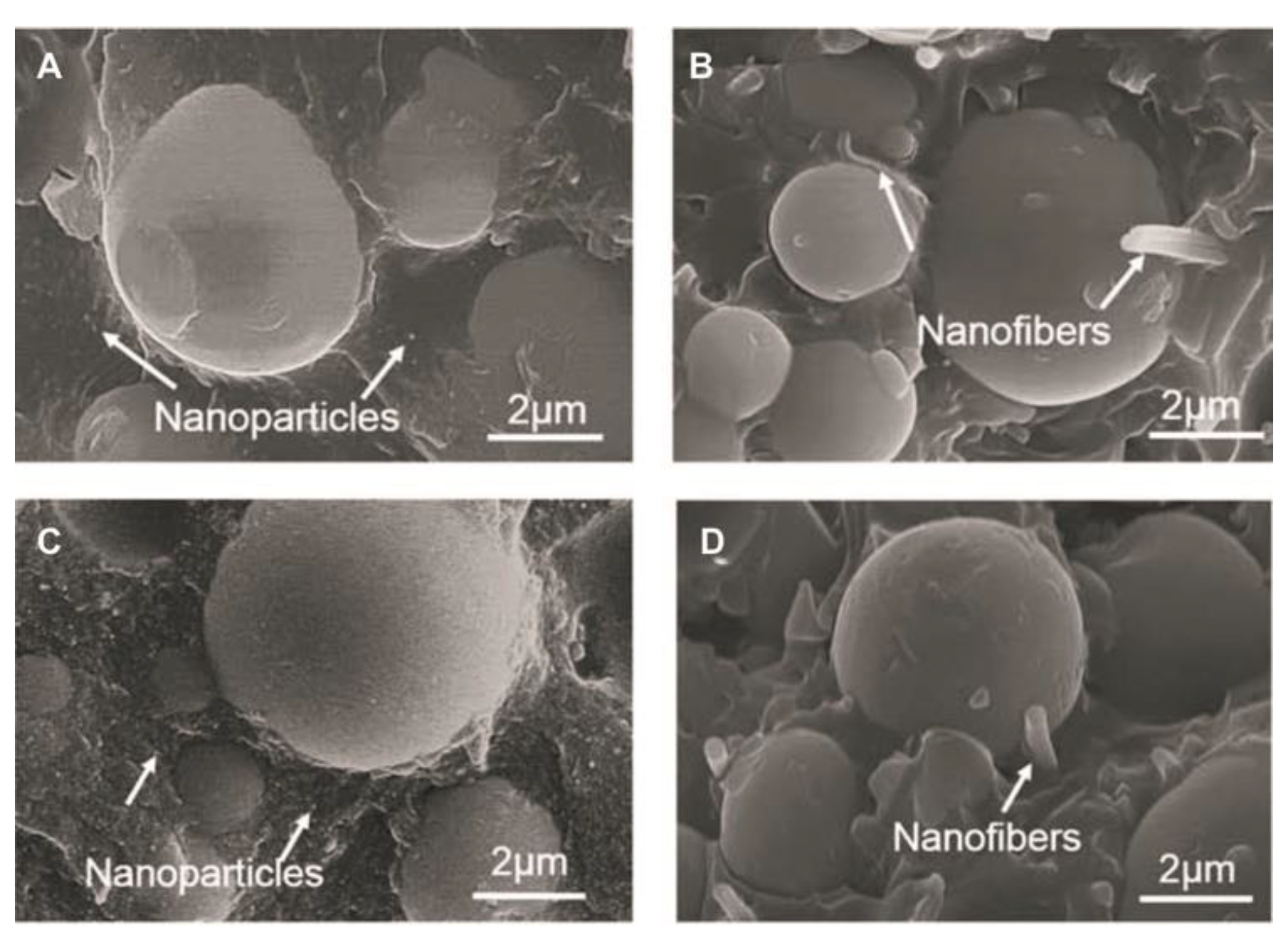
4. Fibrous Fillers and Their Development
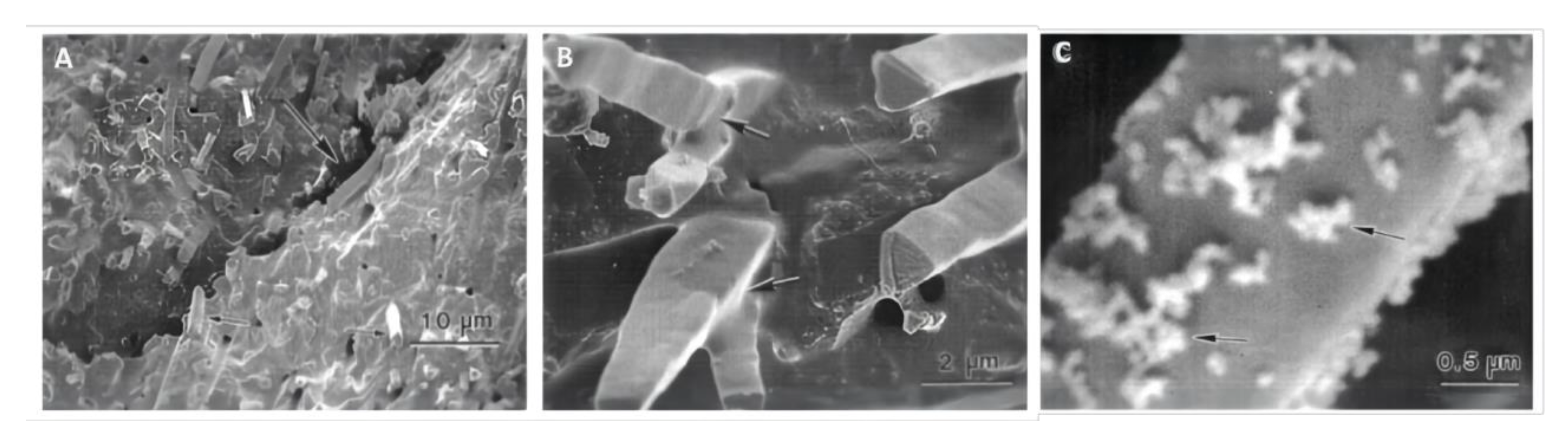
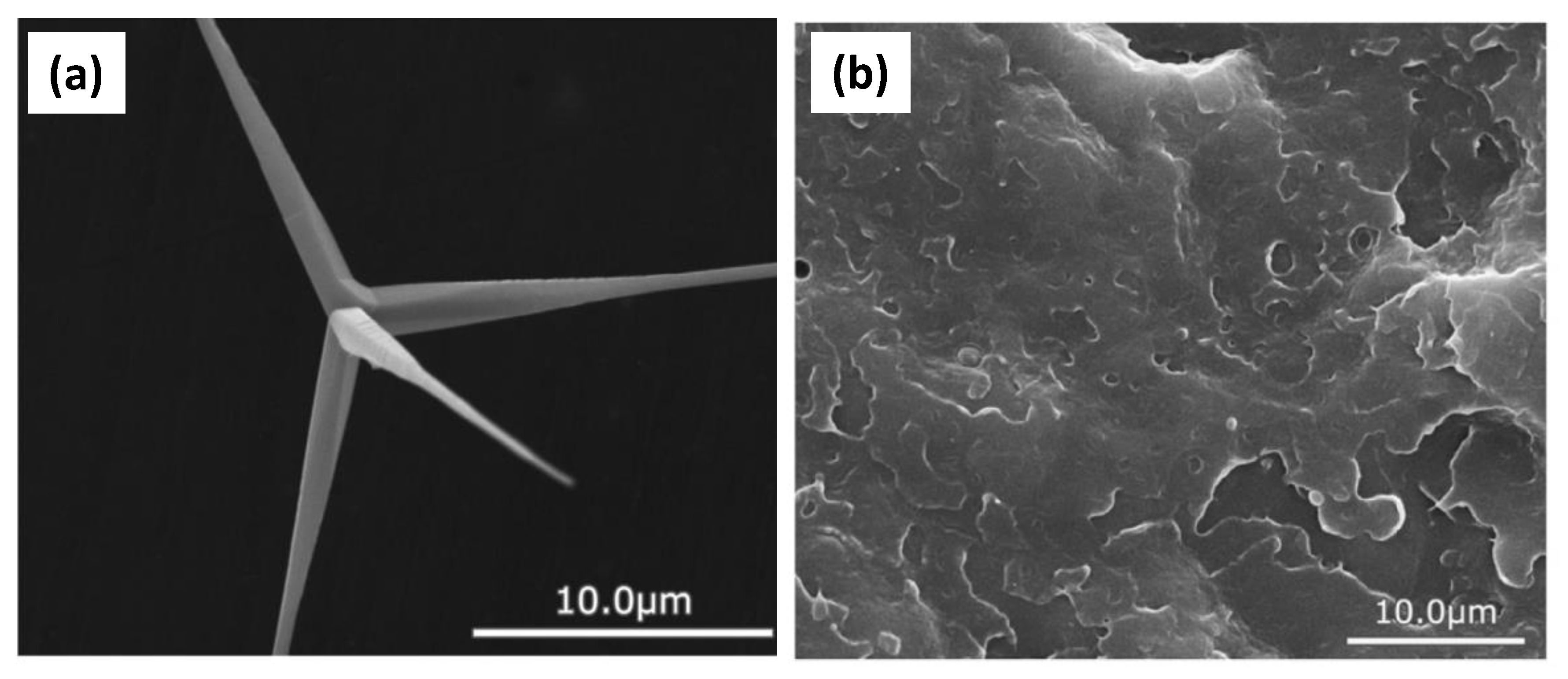
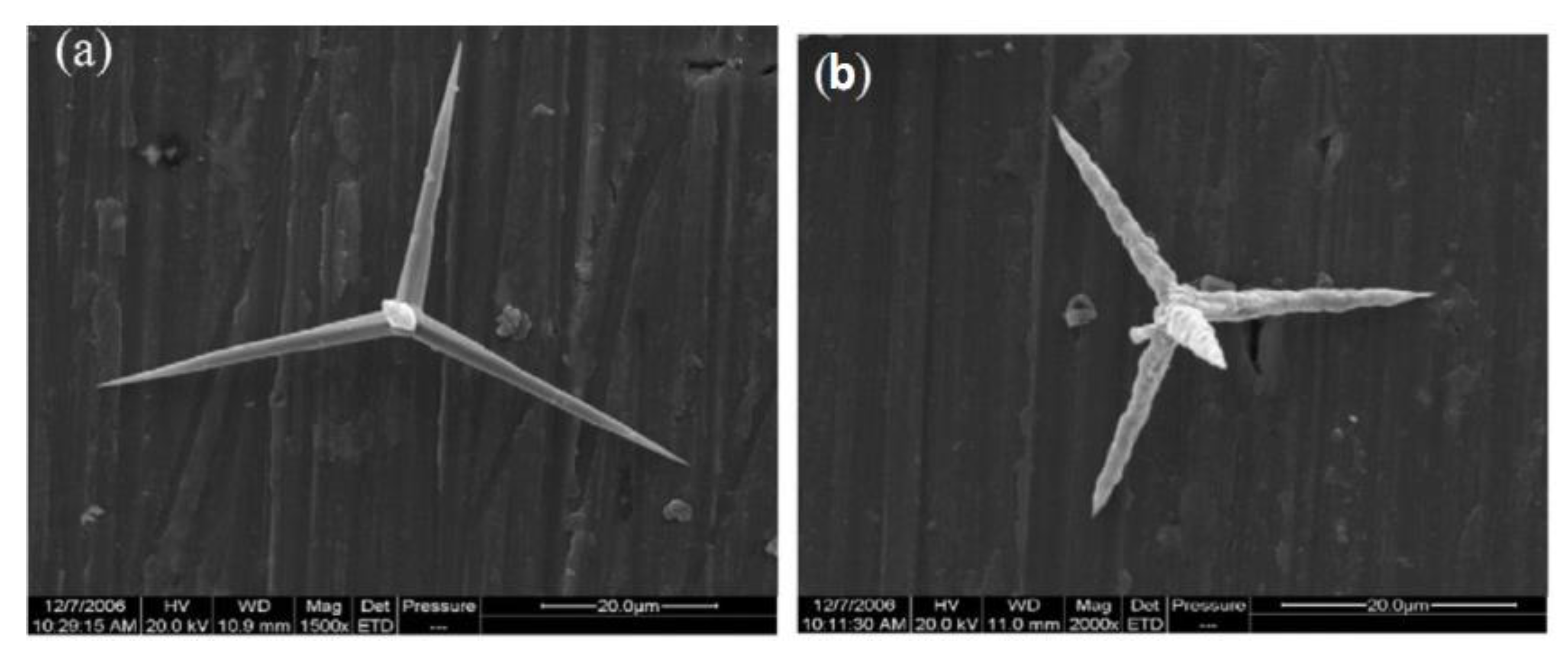
4.1. Microwhisker
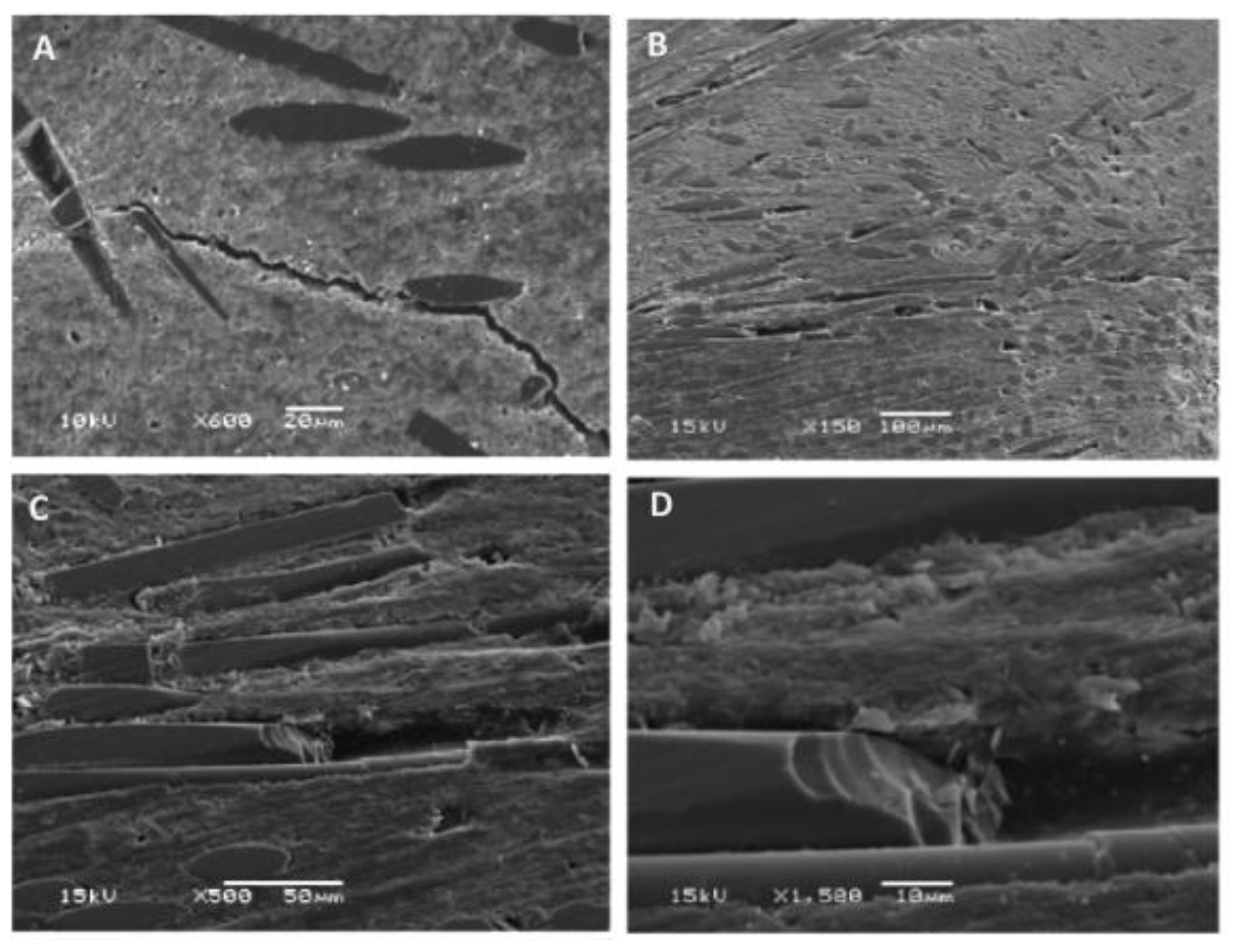
4.2. Short Glass Microfiber
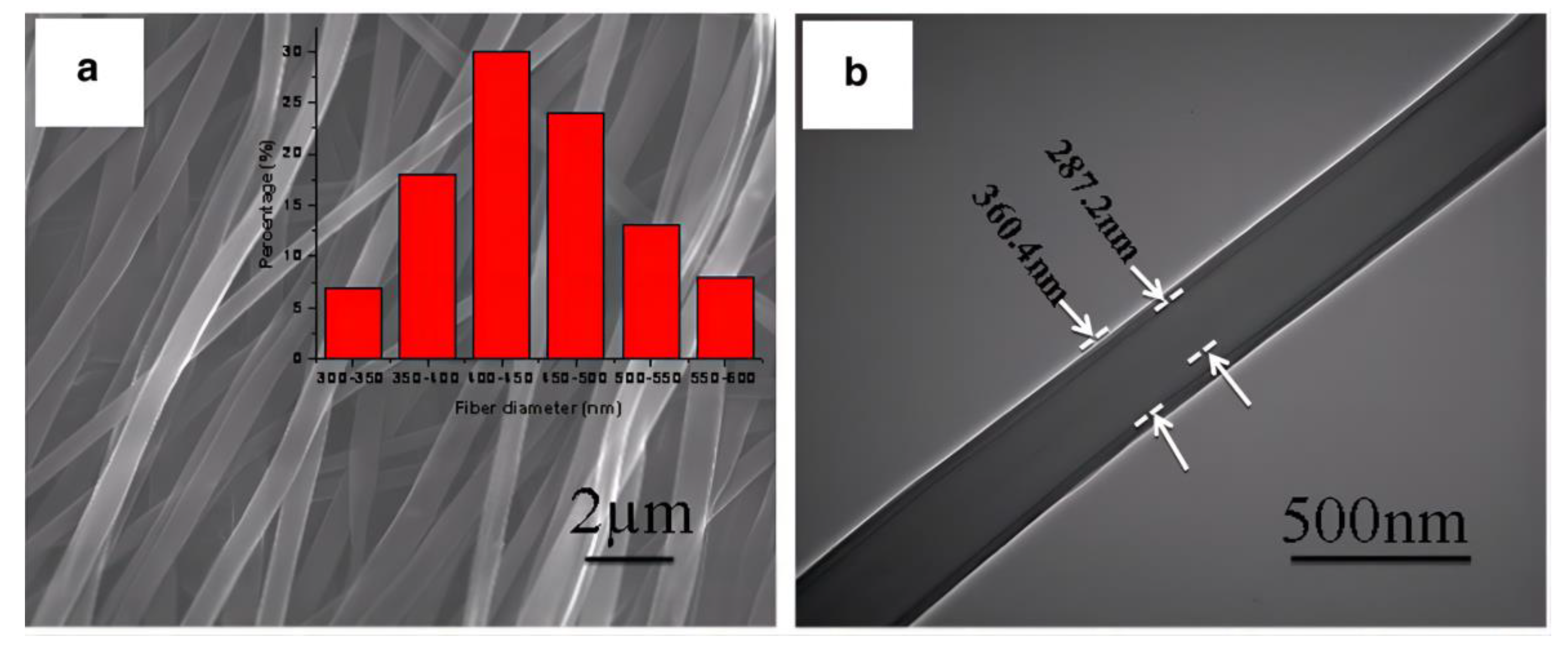
4.3. Ceramic Nanofibers
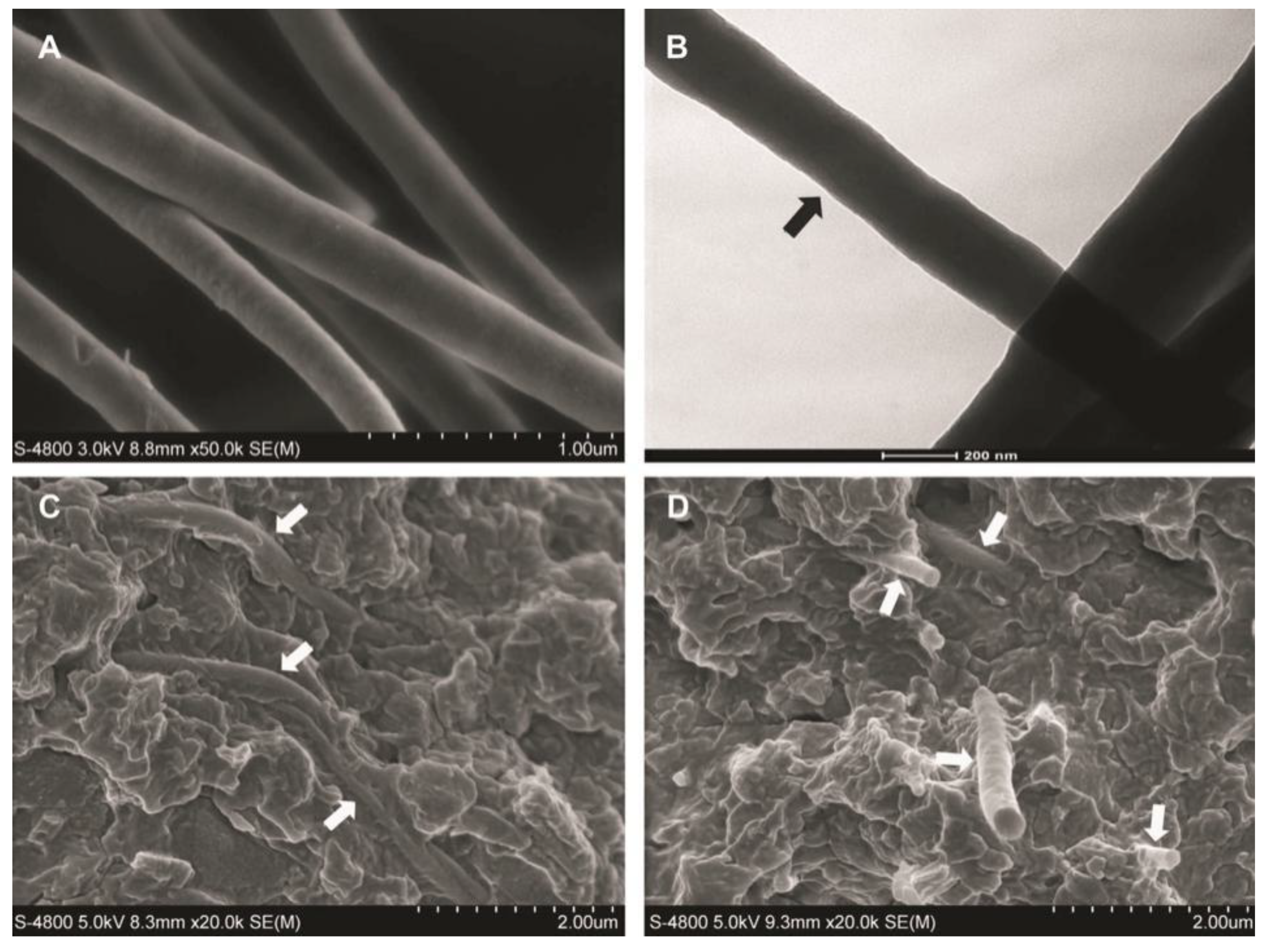
4.4. Polymer Nanofibers
4.5. Nanotubes
5. Novel-Shaped Fillers and Their Development
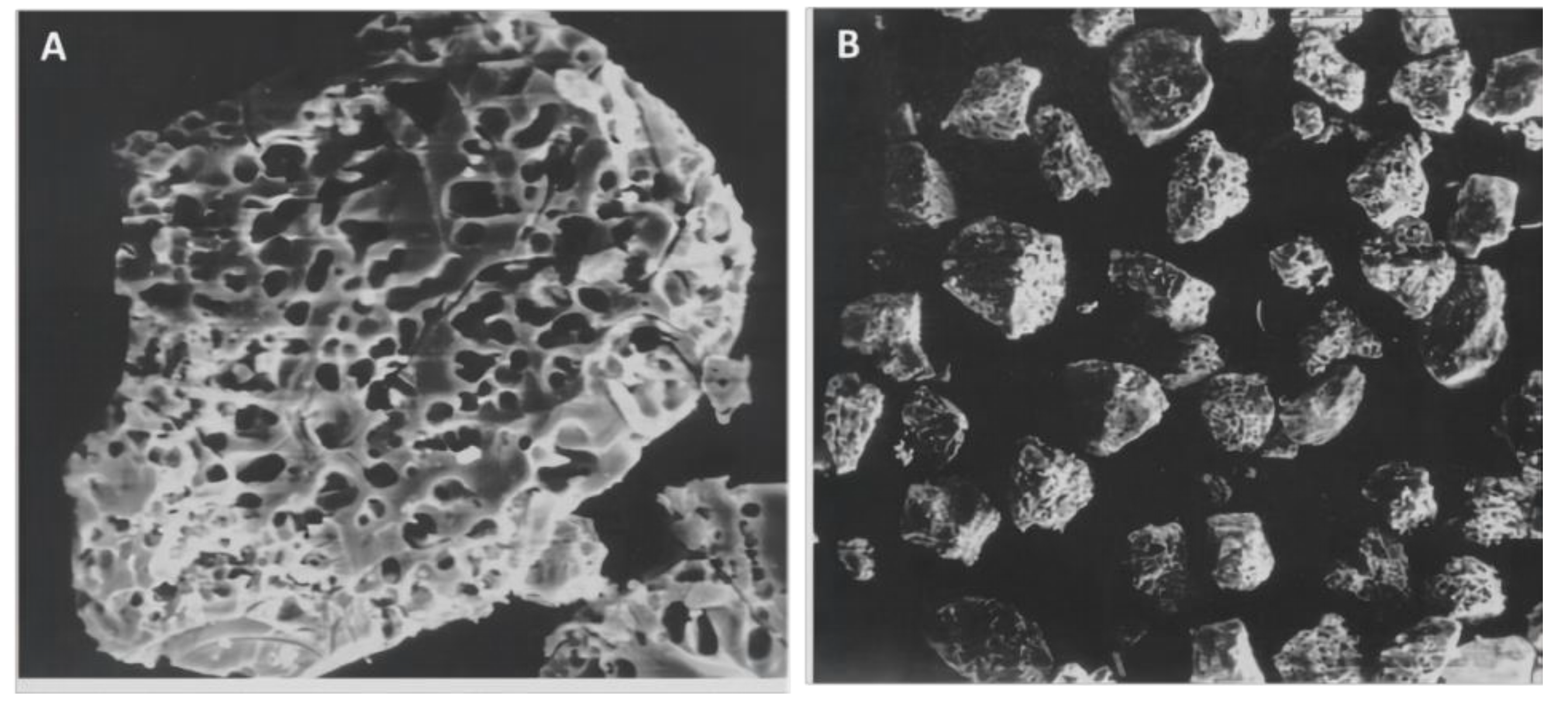
5.1. Porous Particles
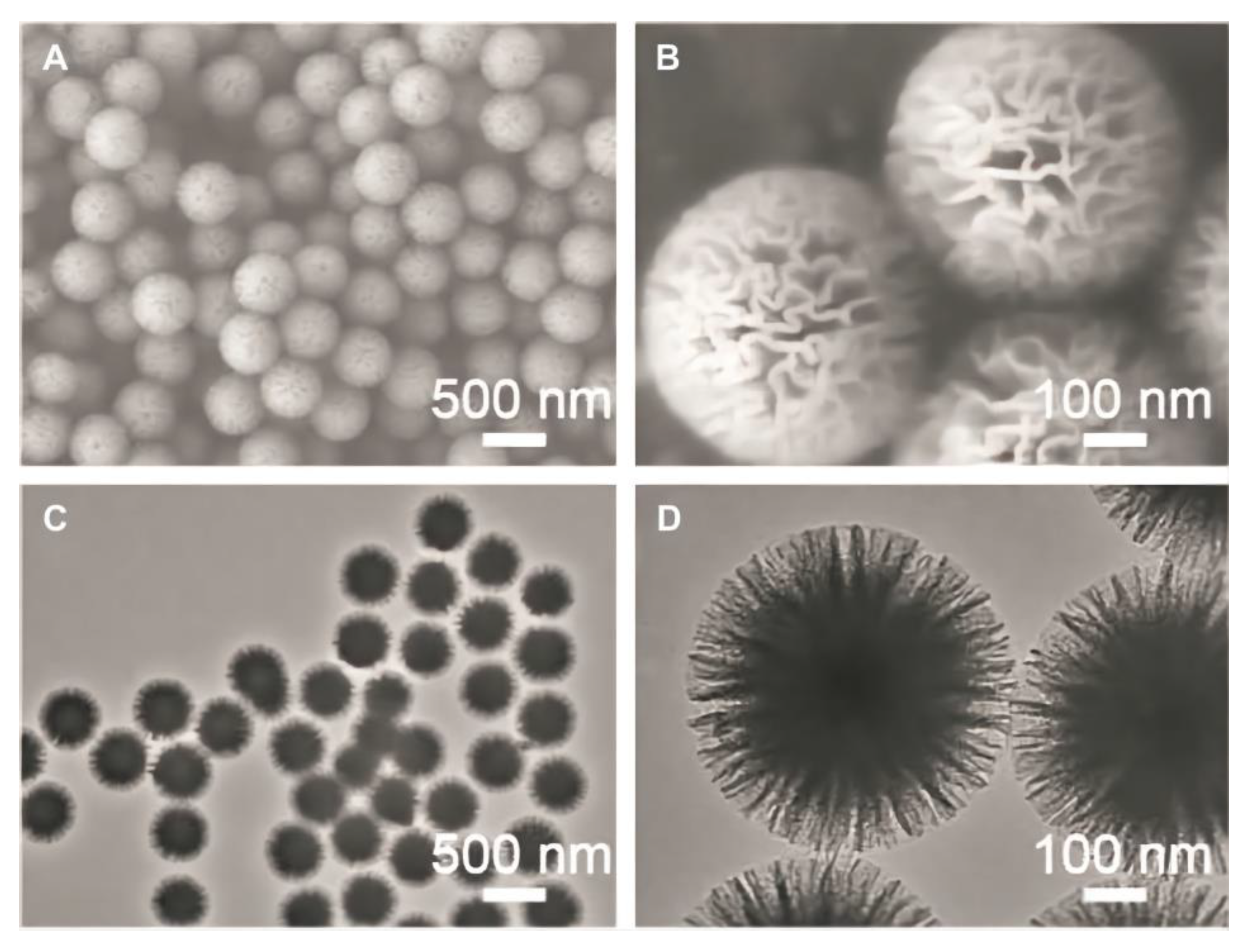
5.2. Mesoporous Silica Particles
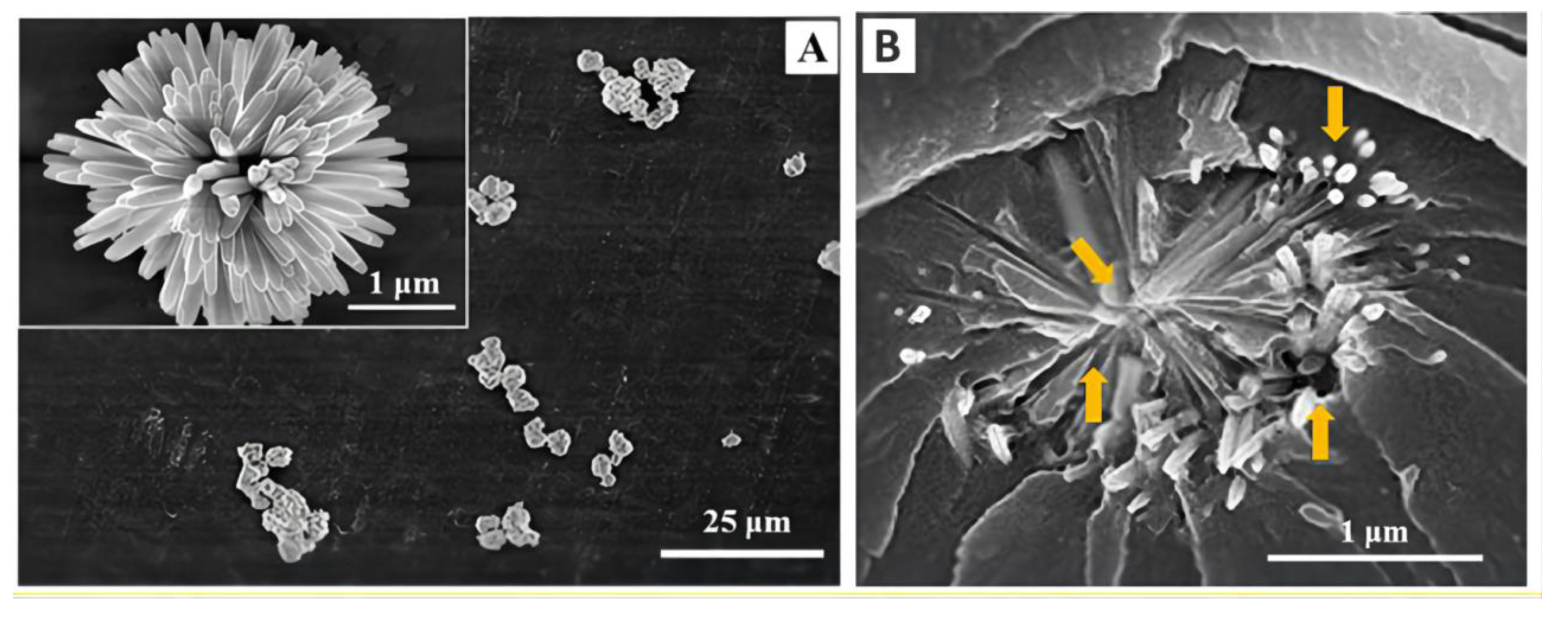
5.3. Urchin-like Fillers
5.4. Nanocluster Fillers
5.5. Tetrapod-like Whiskers
5.6. Core-Sheath Fillers
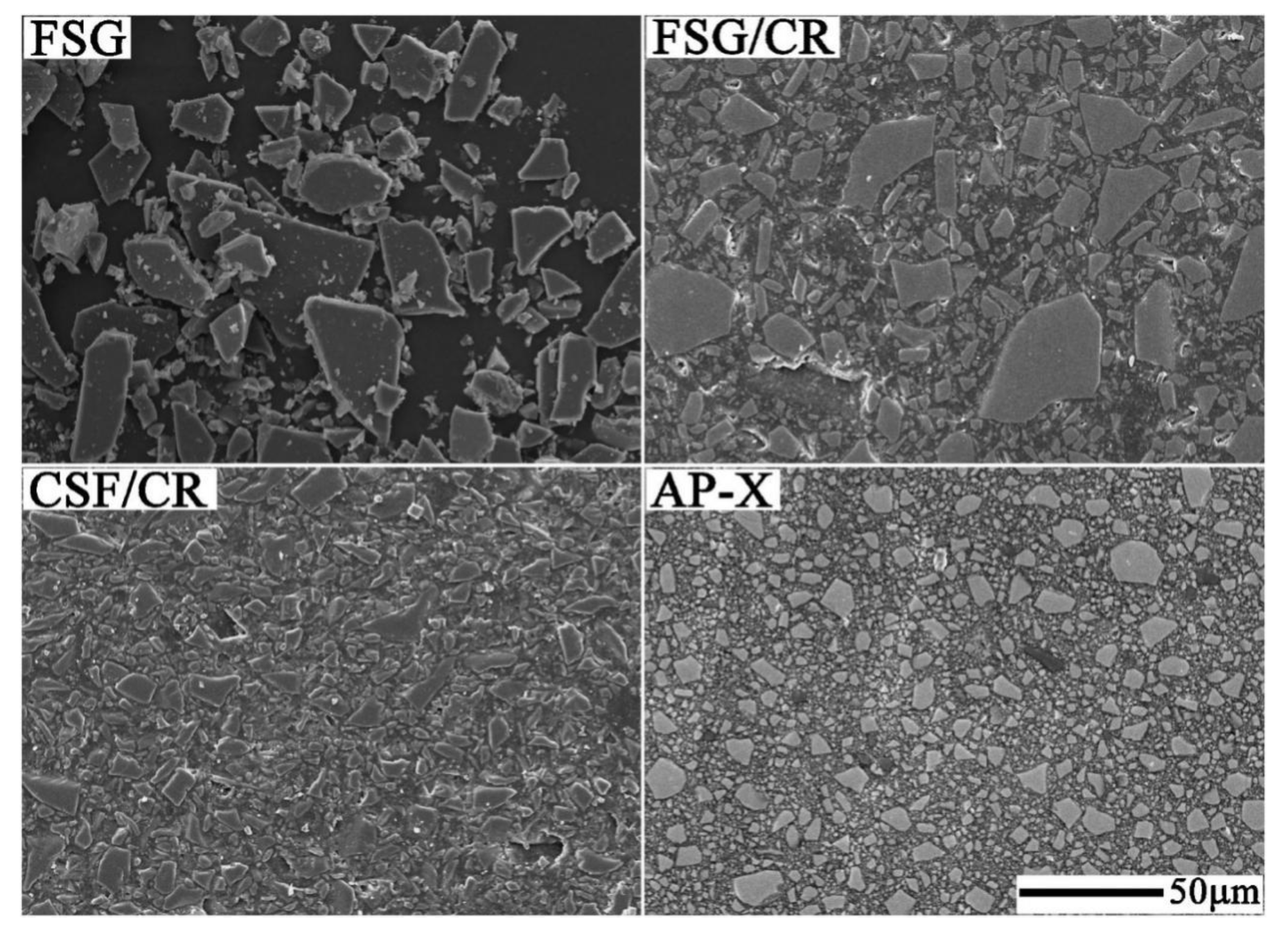
5.7. Glass Flakes
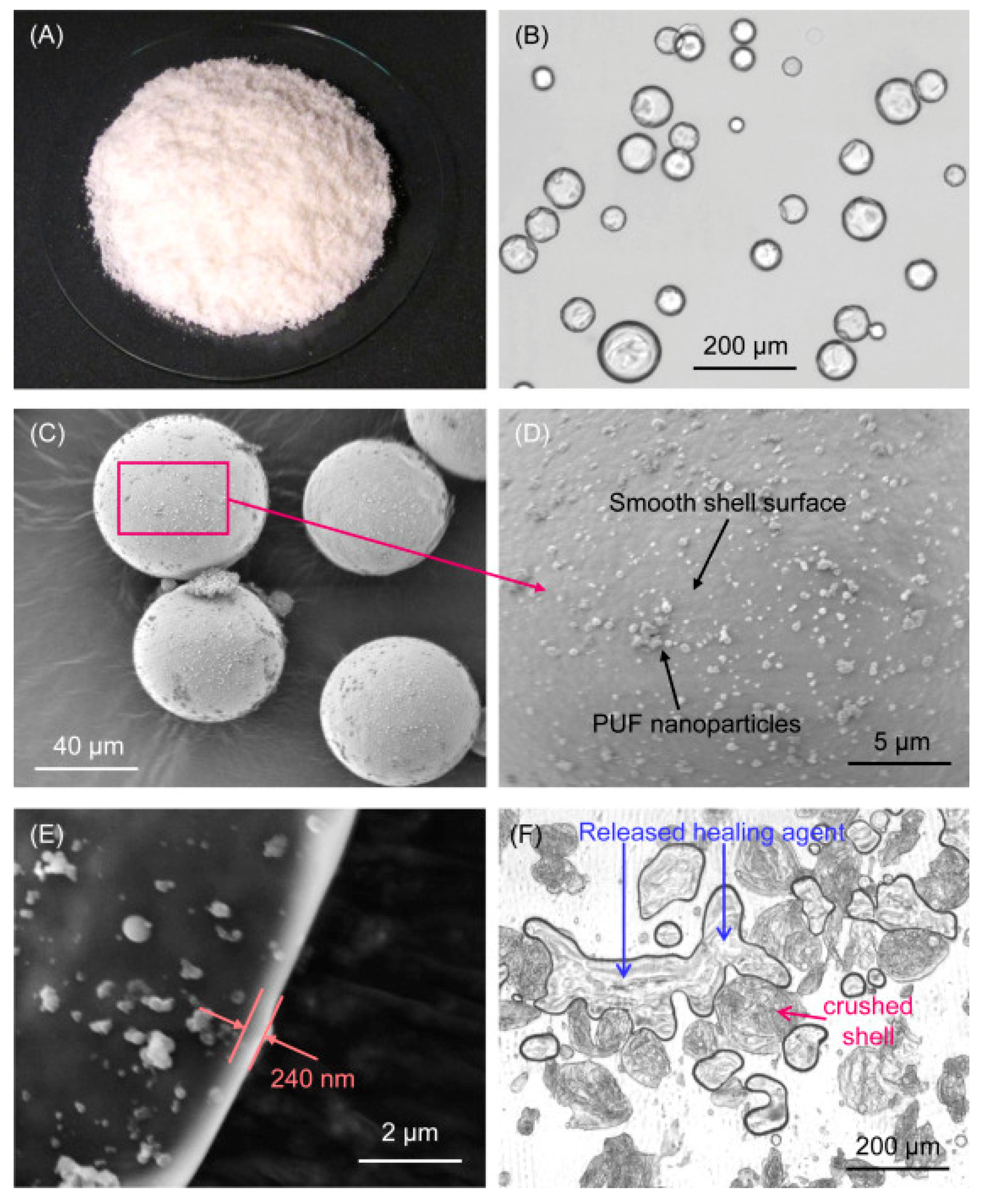
5.8. Microcapsules
6. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rasines Alcaraz, M.G. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.; Wei, S.; Wang, R.; Zhu, M. Improving the Physical–Mechanical Property of Dental Composites by Grafting Methacrylate-Polyhedral Oligomeric Silsesquioxane onto a Filler Surface. ACS Biomater. Sci. Eng. 2021, 7, 1428–1437. [Google Scholar] [CrossRef]
- Aminoroaya, A.; EsmaeelyNeisiany, R.; Nouri Khorasani, S.; Panahi, P.; Das, O.; Ramakrishna, S. A Review of Dental Composites: Methods of Characterizations. ACS Biomater. Sci. Eng. 2020, 6, 3713–3744. [Google Scholar] [CrossRef] [PubMed]
- Zabrovsky, A.; Neeman Levy, T.; Bar-On, H.; Beyth, N.; Ben-Gal, G. Next generation of dentists moving to amalgam-free dentistry: Survey of posterior restorations teaching in North America. Eur. J. Dent. Educ. 2019, 23, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Verde, A.V.; Ramos, M.M.D.; Stoneham, A.M. Benefits in Cost and Reduced Discomfort of New Techniques of Minimally Invasive Cavity Treatment. J. Dent. Res. 2009, 88, 297–299. [Google Scholar] [CrossRef]
- Weng, Y.; Howard, L.; Guo, X.; Chong, V.J.; Gregory, R.L.; Xie, D. A novel antibacterial resin composite for improved dental restoratives. J. Mater. Sci. Mater. Med. 2012, 23, 1553–1561. [Google Scholar] [CrossRef]
- Pérez-Mondragón, A.A.; Cuevas-Suárez, C.E.; Trejo-Carbajal, N.; Piva, E.; da Fernandes Silva, A.; Herrera-González, A.M. Evaluation of monomers derived from resorcinol as eluents of bisphenol A glycidyl dimethacrylate for the formulation of dental composite resins. J. Appl. Polym. Sci. 2020, 137, 48576. [Google Scholar] [CrossRef]
- He, J.; Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. The effect of adding a new monomer “Phene” on the polymerization shrinkage reduction of a dental resin composite. Dent. Mater. 2019, 35, 627–635. [Google Scholar] [CrossRef]
- Bai, X.; Lin, C.; Wang, Y.; Ma, J.; Wang, X.; Yao, X.; Tang, B. Preparation of Zn doped mesoporous silica nanoparticles (Zn-MSNs) for the improvement of mechanical and antibacterial properties of dental resin composites. Dent. Mater. 2020, 36, 794–807. [Google Scholar] [CrossRef]
- Herrera-González, A.M.; Pérez-Mondragón, A.A.; Cuevas-Suárez, C.E. Evaluation of bio-based monomers from isosorbide used in the formulation of dental composite resins. J. Mech. Behav. Biomed. Mater. 2019, 100, 103371. [Google Scholar] [CrossRef]
- Kim, K.-H.; Ong, J.L.; Okuno, O. The effect of filler loading and morphology on the mechanical properties of contemporary composites. J. Prosthet. Dent. 2002, 87, 642–649. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, M.; Zhu, X.X. Functional fillers for dental resin composites. Acta Biomater. 2021, 122, 50–65. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.-L.; Sun, Q.; Niu, H.; Wang, R.-L.; Wang, D.; Wang, J.-X. The properties of dental resin composites reinforced with silica colloidal nanoparticle clusters: Effects of heat treatment and filler composition. Compos. Part B Eng. 2020, 186, 107791. [Google Scholar] [CrossRef]
- Maran, B.M.; de Geus, J.L.; Gutiérrez, M.F.; Heintze, S.; Tardem, C.; Barceleiro, M.O.; Reis, A.; Loguercio, A.D. Nanofilled/nanohybrid and hybrid resin-based composite in patients with direct restorations in posterior teeth: A systematic review and meta-analysis. J. Dent. 2020, 99, 103407. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hua, H.; Liu, H.; Zhu, M.; Zhu, X.X. Surface Modification of ZrO2 Nanoparticles and Its Effects on the Properties of Dental Resin Composites. ACS Appl. Bio Mater. 2020, 3, 5300–5309. [Google Scholar] [CrossRef]
- Habib, E.; Wang, R.; Wang, Y.; Zhu, M.; Zhu, X.X. Inorganic Fillers for Dental Resin Composites: Present and Future. ACS Biomater. Sci. Eng. 2016, 2, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 32, 1586–1599. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Zhang, M.; Liu, F.; Bao, S.; Wu, T.; Jiang, X.; Zhang, Q.; Zhu, M. Investigation on the physical-mechanical properties of dental resin composites reinforced with novel bimodal silica nanostructures. Mater. Sci. Eng. C 2015, 50, 266–273. [Google Scholar] [CrossRef]
- Alvarado, J.A.; Maldonado, A.; Juarez, H.; Pacio, M. Synthesis of Colloidal ZnO Nanoparticles and Deposit of Thin Films by Spin Coating Technique. J. Nanomater. 2013, 2013, 903191. [Google Scholar] [CrossRef]
- Shi, J.; Wang, Y.; Gao, Y.; Bai, H. Effects of coupling agents on the impact fracture behaviors of T-ZnOw/PA6 composites. Compos. Sci. Technol. 2008, 68, 1338–1347. [Google Scholar] [CrossRef]
- Zhou, J.P.; Qiu, K.Q.; Fu, W.L. The Surface Modification of ZnOw and its Effect on the Mechanical Properties of Filled Polypropylene Composites. J. Compos. Mater. 2005, 39, 1931–1941. [Google Scholar] [CrossRef]
- Chen, X.; Zhou, Z.; Lv, W.; Huang, T.; Hu, S. Preparation of core–shell structured T-ZnOw/polyaniline composites via graft polymerization. Mater. Chem. Phys. 2009, 115, 258–262. [Google Scholar] [CrossRef]
- Cheng, L.; Zhou, X.; Zhong, H.; Deng, X.; Cai, Q.; Yang, X. NaF-loaded core—Shell PAN–PMMA nanofibers as reinforcements for Bis-GMA/TEGDMA restorative resins. Mater. Sci. Eng. C 2014, 34, 262–269. [Google Scholar] [CrossRef]
- Wang, X.; Cai, Q.; Zhang, X.; Wei, Y.; Xu, M.; Yang, X.; Ma, Q.; Cheng, Y.; Deng, X. Improved performance of Bis-GMA/TEGDMA dental composites by net-like structures formed from SiO2 nanofiber fillers. Mater. Sci. Eng. C 2016, 59, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, S.; Dowling, A.H.; El-Safty, S.; Fleming, G.J.P. The influence of monomeric resin and filler characteristics on the performance of experimental resin-based composites (RBCs) derived from a commercial formulation. Dent. Mater. 2012, 28, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Rüttermann, S.; Dluzhevskaya, I.; Großsteinbeck, C.; Raab, W.H.M.; Janda, R. Impact of replacing Bis-GMA and TEGDMA by other commercially available monomers on the properties of resin-based composites. Dent. Mater. 2010, 26, 353–359. [Google Scholar] [CrossRef]
- Musanje, L.; Ferracane, J.L. Effects of resin formulation and nanofiller surface treatment on the properties of experimental hybrid resin composite. Biomaterials 2004, 25, 4065–4071. [Google Scholar] [CrossRef] [PubMed]
- Bociong, K.; Szczesio, A.; Krasowski, M.; Sokolowski, J. The influence of filler amount on selected properties of new experimental resin dental composite. In Open Chemistry; Springer: Berlin, Germany, 2018; Volume 16, p. 905. [Google Scholar]
- Ilie, N. Comparative Effect of Self- or Dual-Curing on Polymerization Kinetics and Mechanical Properties in a Novel, Dental-Resin-Based Composite with Alkaline Filler. Running Title: Resin-Composites with Alkaline Fillers. Materials 2018, 11, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, W.J. Dental Materials and Their Selection, 3rd ed.; Quintessence Publishing Co, Inc.: Berlin, German, 2002. [Google Scholar]
- Watts, D.C. Radiopacity vs. composition of some barium and strontium glass composites. J. Dent. 1987, 15, 38–43. [Google Scholar] [CrossRef]
- Stencel, R.; Kasperski, J.; Pakieła, W.; Mertas, A.; Bobela, E.; Barszczewska-Rybarek, I.; Chladek, G. Properties of Experimental Dental Composites Containing Antibacterial Silver-Releasing Filler. Materials 2018, 11, 1031. [Google Scholar] [CrossRef] [Green Version]
- Chiari, M.D.S.; Rodrigues, M.C.; Xavier, T.A.; de Souza, E.M.N.; Arana-Chavez, V.E.; Braga, R.R. Mechanical properties and ion release from bioactive restorative composites containing glass fillers and calcium phosphate nano-structured particles. Dent. Mater. 2015, 31, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Söderholm, K.J. Degradation of Glass Filler in Experimental Composites. J. Dent. Res. 1981, 60, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
- Soderholm, K.J.M.; Mukherjee, R.; Longmate, J. Filler Leachability of Composites Stored in Distilled Water or Artificial Saliva. J. Dent. Res. 1996, 75, 1692–1699. [Google Scholar] [CrossRef] [PubMed]
- Soderholm, K.J.M. Leaking of Fillers in Dental Composites. J. Dent. Res. 1983, 62, 126–130. [Google Scholar] [CrossRef]
- Söderholm, K.J.; Zigan, M.; Ragan, M.; Fischlschweiger, W.; Bergman, M. Hydrolytic Degradation of Dental Composites. J. Dent. Res. 1984, 63, 1248–1254. [Google Scholar] [CrossRef]
- Yao, S.; Li, T.; Zhou, C.; Weir, M.D.; Melo, M.A.S.; Tay, F.R.; Lynch, C.D.; Imazato, S.; Wu, J.; Xu, H.H.K. Novel antibacterial and therapeutic dental polymeric composites with the capability to self-heal cracks and regain mechanical properties. Eur. Polym. J. 2020, 129, 109604. [Google Scholar] [CrossRef]
- Miao, X.; Li, Y.; Zhang, Q.; Zhu, M.; Wang, H. Low shrinkage light curable dental nanocomposites using SiO2 microspheres as fillers. Mater. Sci. Eng. C 2012, 32, 2115–2121. [Google Scholar] [CrossRef]
- Masalov, V.M.; Sukhinina, N.S.; Kudrenko, E.A.; Emelchenko, G.A. Mechanism of formation and nanostructure of Stöber silica particles. Nanotechnology 2011, 22, 275718. [Google Scholar] [CrossRef] [PubMed]
- Drummond, J.L. Degradation, Fatigue, and Failure of Resin Dental Composite Materials. J. Dent. Res. 2008, 87, 710–719. [Google Scholar] [CrossRef] [Green Version]
- Zhang, M.; Matinlinna, J.P. E-Glass Fiber Reinforced Composites in Dental Applications. Silicon 2012, 4, 73–78. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Y.; Ning, R.; Zheng, Y. Study of SiO2 Nanoparticles on the Improved Performance of Epoxy and Fiber Composites. J. Reinf. Plast. Compos. 2005, 24, 223–233. [Google Scholar] [CrossRef]
- Beun, S.; Glorieux, T.; Devaux, J.; Vreven, J.; Leloup, G. Characterization of nanofilled compared to universal and microfilled composites. Dent. Mater. 2007, 23, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Arcís, R.W.; López-Macipe, A.; Toledano, M.; Osorio, E.; Rodríguez-Clemente, R.; Murtra, J.; Fanovich, M.A.; Pascual, C.D. Mechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restoration. Dent. Mater. 2002, 18, 49–57. [Google Scholar] [CrossRef]
- Hicks, J.; Garcia-Godoy, F.; Flaitz, C. Biological factors in dental caries: Role of saliva and dental plaque in the dynamic process of demineralization and remineralization (part 1). J. Clin. Pediatr. Dent. 2003, 28, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Abdulrahman, A.B.; Anmar, A.K.; Denise, H.; Michael, D.W.; Hockin, H.K.X.; Mary Anne, S.M. Toward dental caries: Exploring nanoparticle-based platforms and calcium phosphate compounds for dental restorative materials. Bioact. Mater. 2019, 4, 43–55. [Google Scholar]
- Li, S.; Zhang, L.; Kim, J.; Pan, M.; Shi, Z.; Zhang, J. Synthesis of carbon-supported binary FeCo–N non-noble metal electrocatalysts for the oxygen reduction reaction. Electrochim. Acta 2010, 55, 7346–7353. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Jiang, X.; Zhang, Q.; Zhu, M. Strong and bioactive dental resin composite containing poly(Bis-GMA) grafted hydroxyapatite whiskers and silica nanoparticles. Compos. Sci. Technol. 2014, 101, 86–93. [Google Scholar] [CrossRef]
- Liu, F.; Wang, R.; Cheng, Y.; Jiang, X.; Zhang, Q.; Zhu, M. Polymer grafted hydroxyapatite whisker as a filler for dental composite resin with enhanced physical and mechanical properties. Mater. Sci. Eng. C 2013, 33, 4994–5000. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Darvell, B.W. Mechanical properties of hydroxyapatite whisker-reinforced bis-GMA-based resin composites. Dent. Mater. 2012, 28, 824–830. [Google Scholar] [CrossRef]
- Chen, L.; Yu, Q.; Wang, Y.; Li, H. BisGMA/TEGDMA dental composite containing high aspect-ratio hydroxyapatite nanofibers. Dent. Mater. 2011, 27, 1187–1195. [Google Scholar] [CrossRef] [Green Version]
- Taheri, M.M.; Abdul Kadir, M.R.; Shokuhfar, T.; Hamlekhan, A.; Shirdar, M.R.; Naghizadeh, F. Fluoridated hydroxyapatite nanorods as novel fillers for improving mechanical properties of dental composite: Synthesis and application. Mater. Des. 2015, 82, 119–125. [Google Scholar] [CrossRef]
- Liu, F.; Sun, B.; Jiang, X.; Aldeyab, S.S.; Zhang, Q.; Zhu, M. Mechanical properties of dental resin/composite containing urchin-like hydroxyapatite. Dent. Mater. 2014, 30, 1358–1368. [Google Scholar] [CrossRef]
- Suzuki, S.; Ori, T.; Saimi, Y. Effects of filler composition on flexibility of microfilled resin composite. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 74, 547–552. [Google Scholar] [CrossRef]
- Yukitani, W.; Hasegawa, T.; Itoh, K.; Hisamitsu, H.; Wakumoto, S.J.O.D. Marginal adaptation of dental composites containing prepolymerized filler. Oper. Dent. 1997, 22, 242–248. [Google Scholar] [PubMed]
- Blackham, J.T.; Vandewalle, K.S.; Lien, W. Properties of Hybrid Resin Composite Systems Containing Prepolymerized Filler Particles. Oper. Dent. 2009, 34, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Nee, A.Y.C. Handbook of Manufacturing Engineering and Technology; Springer: Berlin, Germany, 2015. [Google Scholar]
- Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent. Mater. 2013, 29, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Krause, W.R.; Park, S.-H.; Straup, R.A. Mechanical properties of BIS-GMA resin short glass fiber composites. J. Biomed. Mater. Res. 1989, 23, 1195–1211. [Google Scholar] [CrossRef] [PubMed]
- Ruddell, D.E.; Maloney, M.M.; Thompson, J.Y. Effect of novel filler particles on the mechanical and wear properties of dental composites. Dent. Mater. 2002, 18, 72–80. [Google Scholar] [CrossRef]
- Vallittu, P.K. High-aspect ratio fillers: Fiber-reinforced composites and their anisotropic properties. Dent. Mater. 2015, 31, 1–7. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Martin, T.A.; Antonucci, J.M.; Eichmiller, E.C. Ceramic Whisker Reinforcement of Dental Resin Composites. J. Dent. Res. 1999, 78, 706–712. [Google Scholar] [CrossRef]
- Debnath, S.; Ranade, R.; Wunder, S.L.; McCool, J.; Boberick, K.; Baran, G. Interface effects on mechanical properties of particle-reinforced composites. Dent. Mater. 2004, 20, 677–686. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Short glass fiber reinforced restorative composite resin with semi-inter penetrating polymer network matrix. Dent. Mater. 2007, 23, 1356–1362. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Lassila, L.V.J.; Tezvergil, A.; Vallittu, P.K. Load bearing capacity of fibre-reinforced and particulate filler composite resin combination. J. Dent. 2006, 34, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.H.K.; Sun, L.; Weir, M.D.; Antonucci, J.M.; Takagi, S.; Chow, L.C.; Peltz, M. Nano DCPA-Whisker Composites with High Strength and Ca and PO4 Release. J. Dent. Res. 2006, 85, 722–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, H.H.K.; Quinn, J.B.; Smith, D.T.; Giuseppetti, A.A.; Eichmiller, F.C. Effects of different whiskers on the reinforcement of dental resin composites. Dent. Mater. 2003, 19, 359–367. [Google Scholar] [CrossRef]
- Lassila, L.; Garoushi, S.; Vallittu, P.K.; Säilynoja, E. Mechanical properties of fiber reinforced restorative composite with two distinguished fiber length distribution. J. Mech. Behav. Biomed. Mater. 2016, 60, 331–338. [Google Scholar] [CrossRef]
- Lastumäki, T.M.; Lassila, L.V.; Vallittu, P.K. Flexural properties of the bulk fiber-reinforced composite DC-tell used in fixed partial dentures. Int. J. Prosthodont. 2001, 14, 22–26. [Google Scholar]
- Liu, Y.; Sagi, S.; Chandrasekar, R.; Zhang, L.; Hedin, N.E.; Fong, H. Preparation and Characterization of Electrospun SiO2 Nanofibers. J. Nanosci. Nanotechnol. 2008, 8, 1528–1536. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Quinn, J.B.; Smith, D.T.; Antonucci, J.M.; Schumacher, G.E.; Eichmiller, F.C. Dental resin composites containing silica-fused whiskers—Effects of whisker-to-silica ratio on fracture toughness and indentation properties. Biomaterials 2002, 23, 735–742. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Watts, D.C.; Lassila, L.V.J. Polymerization shrinkage of experimental short glass fiber-reinforced composite with semi-inter penetrating polymer network matrix. Dent. Mater. 2008, 24, 211–215. [Google Scholar] [CrossRef]
- Bijelic-Donova, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Mechanical properties, fracture resistance, and fatigue limits ofshort fiber reinforced dental composite resin. J. Prosthet. Dent. 2016, 115, 95–102. [Google Scholar] [CrossRef]
- Guo, G.; Fan, Y.; Zhang, J.-F.; Hagan, J.L.; Xu, X. Novel dental composites reinforced with zirconia—Silica ceramic nanofibers. Dent. Mater. 2012, 28, 360–368. [Google Scholar] [CrossRef] [Green Version]
- Gao, Y.; Sagi, S.; Zhang, L.; Liao, Y.; Cowles, D.M.; Sun, Y.; Fong, H. Electrospun nano-scaled glass fiber reinforcement of bis-GMA/TEGDMA dental composites. J. Appl. Polym. Sci. 2008, 110, 2063–2070. [Google Scholar] [CrossRef]
- Tian, M.; Gao, Y.; Liu, Y.; Liao, Y.; Hedin, N.E.; Fong, H. Fabrication and evaluation of Bis-GMA/TEGDMA dental resins/composites containing nano fibrillar silicate. Dent. Mater. 2008, 24, 235–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fong, H. Electrospun nylon 6 nanofiber reinforced BIS-GMA/TEGDMA dental restorative composite resins. Polymer 2004, 45, 2427–2432. [Google Scholar] [CrossRef]
- Zhu, J.; Peng, H.; Rodriguez-Macias, F.; Margrave, J.L.; Khabashesku, V.N.; Imam, A.M.; Lozano, K.; Barrera, E.V. Reinforcing Epoxy Polymer Composites Through Covalent Integration of Functionalized Nanotubes. Adv. Funct. Mater. 2004, 14, 643–648. [Google Scholar] [CrossRef]
- Zhang, F.; Xia, Y.; Xu, L.; Gu, N. Surface modification and microstructure of single-walled carbon nanotubes for dental resin-based composites. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 86, 90–97. [Google Scholar] [CrossRef]
- Borges, A.L.S.; Münchow, E.A.; de Oliveira Souza, A.C.; Yoshida, T.; Vallittu, P.K.; Bottino, M.C. Effect of random/aligned nylon-6/MWCNT fibers on dental resin composite reinforcement. J. Mech. Behav. Biomed. Mater. 2015, 48, 134–144. [Google Scholar] [CrossRef]
- Chen, Q.; Zhao, Y.; Wu, W.; Xu, T.; Fong, H. Fabrication and evaluation of Bis-GMA/TEGDMA dental resins/composites containing halloysite nanotubes. Dent. Mater. 2012, 28, 1071–1079. [Google Scholar] [CrossRef] [Green Version]
- Cunha, D.A.; Rodrigues, N.S.; Souza, L.C.; Lomonaco, D.; Rodrigues, F.P.; Degrazia, F.W.; Collares, F.M.; Sauro, S.; Saboia, V.P.A. Physicochemical and Microbiological Assessment of an Experimental Composite Doped with Triclosan-Loaded Halloysite Nanotubes. Materials 2018, 11, 1080. [Google Scholar] [CrossRef] [Green Version]
- Horcajada, P.; Chalati, T.; Serre, C.; Gillet, B.; Sebrie, C.; Baati, T.; Eubank, J.F.; Heurtaux, D.; Clayette, P.; Kreuz, C.; et al. Porous metal—Organic-framework nanoscale carriers as a potential platform for drug deliveryand imaging. Nat. Mater. 2009, 9, 172. [Google Scholar] [CrossRef]
- Salerno, M.; Loria, P.; Matarazzo, G.; Tomè, F.; Diaspro, A.; Eggenhöffner, R. Surface Morphology and Tooth Adhesion of a Novel Nanostructured Dental Restorative Composite. Materials 2016, 9, 203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zandinejad, A.A.; Atai, M.; Pahlevan, A. The effect of ceramic and porous fillers on the mechanical properties of experimental dental composites. Dent. Mater. 2006, 22, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Atai, M.; Pahlavan, A.; Moin, N. Nano-porous thermally sintered nano silica as novel fillers for dental composites. Dent. Mater. 2012, 28, 133–145. [Google Scholar] [CrossRef]
- Liu, Y.; Tan, Y.; Lei, T.; Xiang, Q.; Han, Y.; Huang, B. Effect of porous glass–ceramic fillers on mechanical properties of light-cured dental resin composites. Dent. Mater. 2009, 25, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Rapp, M.; Thomspon, J.; Bayne, S.; Rathbun, K. Development of Pre-Polymerized Branched-Fiber Filler Particles. In Journal of Dental Research; Amer Assoc Dental Research: Alexandria, VA, USA, 1998; p. 170. [Google Scholar]
- Jandt, K.D.; Al-Jasser, A.M.O.; Al-Ateeq, K.; Vowles, R.W.; Allen, G.C. Mechanical properties and radiopacity of experimental glass-silica-metal hybrid composites. Dent. Mater. 2002, 18, 429–435. [Google Scholar] [CrossRef]
- Wang, R.; Habib, E.; Zhu, X.X. Synthesis of wrinkled mesoporous silica and its reinforcing effect for dental resin composites. Dent. Mater. 2017, 33, 1139–1148. [Google Scholar] [CrossRef]
- Rodríguez, H.A.; Giraldo, L.F.; Casanova, H. Formation of functionalized nanoclusters by solvent evaporation and their effect on the physicochemical properties of dental composite resins. Dent. Mater. 2015, 31, 789–798. [Google Scholar] [CrossRef]
- Mitra, S.B.; Wu, D.; Holmes, B.N. An application of nanotechnology in advanced dental materials. J. Am. Dent. Assoc. 2003, 134, 1382–1390. [Google Scholar] [CrossRef] [Green Version]
- Curtis, A.R.; Palin, W.M.; Fleming, G.J.P.; Shortall, A.C.C.; Marquis, P.M. The mechanical properties of nanofilled resin-based composites: The impact of dry and wet cyclic pre-loading on bi-axial flexure strength. Dent. Mater. 2009, 25, 188–197. [Google Scholar] [CrossRef]
- Curtis, A.R.; Palin, W.M.; Fleming, G.J.P.; Shortall, A.C.C.; Marquis, P.M. The mechanical properties of nanofilled resin-based composites: Characterizing discrete filler particles and agglomerates using a micromanipulation technique. Dent. Mater. 2009, 25, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Bao, S.; Liu, F.; Jiang, X.; Zhang, Q.; Sun, B.; Zhu, M. Wear behavior of light-cured resin composites with bimodal silica nanostructures as fillers. Mater. Sci. Eng. C 2013, 33, 4759–4766. [Google Scholar] [CrossRef]
- Zhou, Z.; Deng, H.; Yi, J.; Liu, S. A new method for preparation of zinc oxide whiskers. Mater. Res. Bull. 1999, 34, 1563–1567. [Google Scholar] [CrossRef]
- Li, S.; Zhang, J.-F.; Chen, J.; Zhao, Y.; Zhao, X.; Xu, X. Core-sheath zirconia/silica microfibers for dental composites reinforcement. Mater. Lett. 2015, 142, 204–206. [Google Scholar] [CrossRef]
- Glassflake Ltd. What is Glassflake? Available online: https://www.glassflake.com/what-is-glassflake/ (accessed on 7 June 2021).
- Akiko, S.; Fumio, W.; Juichi, I.N.O.; Junko, M.; Motohiro, U.O. Application of flake shaped glass (Glass Flake®) filler for dental composite resin. J. Ceram. Soc. Jpn. 2010, 118, 425. [Google Scholar]
- Mohseni, M.; Atai, M.; Sabet, A.; Beigi, S. Effect of plate-like glass fillers on the mechanical properties of dental nanocomposites. Iran. Polym. J. 2016, 25, 129. [Google Scholar] [CrossRef]
- Benedikt, S.; Sebastian, L.; Thorsten, G.; Dieter, B. Optical and Mechanical Properties of Highly Transparent Glass-Flake Composites. J. Compos. Sci. 2019, 3, 101. [Google Scholar]
- Amini, A.; Khavari, A.; Molter, C.; Ehrlicher, A.J. A bioinspired optically transparent tough glass composite. arXiv 2020, arXiv:2003.13863. [Google Scholar]
- Wu, J.; Xie, X.; Zhou, H.; Tay, F.R.; Weir, M.D.; Melo, M.A.S.; Oates, T.W.; Zhang, N.; Zhang, Q.; Xu, H.H.K. Development of a new class of self-healing and therapeutic dental resins. Polym. Degrad. Stab. 2019, 163, 87–99. [Google Scholar] [CrossRef]
- Zhu, D.Y.; Rong, M.Z.; Zhang, M.Q. Self-healing polymeric materials based on microencapsulated healing agents: From design to preparation. Prog. Polym. Sci. 2015, 49, 175–220. [Google Scholar] [CrossRef]
- Bekas, D.G.; Tsirka, K.; Baltzis, D.; Paipetis, A.S. Self-healing materials: A review of advances in materials, evaluation, characterization and monitoring techniques. Compos. Part B 2016, 87, 92–119. [Google Scholar] [CrossRef]
- Then, S.; Neon, G.S.; Abu Kasim, N.H. Performance of Melamine Modified Urea-Formaldehyde Microcapsules in a Dental Host Material. J. Appl. Polym. Sci. 2011, 122, 2557–2562. [Google Scholar] [CrossRef] [Green Version]
- Wertzberger, B.E.; Steere, J.T.; Pfeifer, R.M.; Nensel, M.A.; Latta, M.A.; Gross, S.M. Physical Characterization of a Self-Healing Dental Restorative Material. J. Appl. Polym. Sci. 2010, 118, 428–434. [Google Scholar] [CrossRef]
- Yahyazadehfar, M.; Huyang, G.; Wang, X.; Fan, Y.; Arola, D.; Sun, J. Durability of self-healing dental composites: A comparison of performance under monotonic and cyclic loading. Mater. Sci. Eng. C 2018, 93, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Huyang, G.; Debertin, A.E.; Sun, J. Design and development of self-healing dental composites. Mater. Des. 2016, 94, 295–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Weir, M.D.; Zhang, Q.; Zhou, C.; Melo, M.A.S.; Xu, H.H.K. Novel self-healing dental resin with microcapsules of polymerizable triethylene glycol dimethacrylate and N,N-dihydroxyethyl-p-toluidine. Dent. Mater. 2016, 32, 294–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Filler Types | Chemical Composition | Size (μm) | Shape | Commercial Composites |
|---|---|---|---|---|
| Ground quartz micropowder | SiO2 | 10–50 | Irregular | Aelite Aesthetic Enamel (Bisco) |
| Ground glass micropowder | SiO2 + BaO + SrO2 + TiO2 | 0.6–10 | Irregular | Admira (Voco) Artemis (Ivoclarvivadent) |
| Air colloid silica ultra-fine nanopowder | SiO2 | 0.04–0.4 | Spherical | Enamel Plus HFO (Micerium) Fitek Supreme (3M ESPE) |
| Hydroxyapatite particle (HA) | Ca5(PO4)3(OH) | N.I. b | Irregular | N.I. |
| Prepolymerization particle | SiO2 + resin matrix | 0.04 + (0.6–1.0) | Spherical + irregular | Clearfil Majesty (Kuraray) TerticEvoCeram (Ivoclar North America) |
| Filler Types | Chemical Composition | Dimension |
|---|---|---|
| Microwhisker | Silicon nitride Silicon carbide | Diameter: 0.1–2 μm; mean = 0.4 μm Length: 2–30 μm; mean = 5 μm Diameter: 0.1–3 μm; mean = 0.7 μm Length: 2–100 μm; mean = 14 μm |
| Short glass microfiber | Silica | Diameter: 10–17 μm Length: 14–2400 μm |
| Ceramic nanofiber | Silica, zirconia, zirconia-silica zirconia-yttria-silica | Diameter: 160–390 nm Length: 5–10 μm |
| Polymer nanofiber | Nylon-6 | Diameter: 100–900 mm |
| Nanotube | Carbon | Diameter: 50–100 nm |
| Filler Types | Chemical Composition | Shape | Size |
|---|---|---|---|
| Porous particle | Glass-ceramic | Particle-like | 2–4 μm |
| Mesoporous particle | Silica | N.I. a | Average 496 nm |
| UHA particle | Hydroxyapatite | Sea urchin | 2–3 µm |
| Nanocluster particle | SiO2, ZrO2 | Particlelike | 0.07–2.7 µm |
| T-ZnO whisker | ZnO | Tetra-needle | 0.18–0.21 μm |
| Core–sheath fiber | Zirconia/Silica, PAN-PMMA, T-ZnOw/PANI | Fibrous | Diameter: 220–300 nm Diameter: 300–400 nm N.I. |
| Glass flake | SiO2, Al2O3, CaO, et al. | Flakes | Diameter: 15–160 μm |
| Microcapsule | Polymer shell with healing liquid inside | Capsules | Diameter: 10–300 μm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Zhang, H.; Sun, H.; Liu, Y.; Liu, W.; Su, B.; Li, S. The Development of Filler Morphology in Dental Resin Composites: A Review. Materials 2021, 14, 5612. https://doi.org/10.3390/ma14195612
Liu J, Zhang H, Sun H, Liu Y, Liu W, Su B, Li S. The Development of Filler Morphology in Dental Resin Composites: A Review. Materials. 2021; 14(19):5612. https://doi.org/10.3390/ma14195612
Chicago/Turabian StyleLiu, Jiani, Hao Zhang, Huijun Sun, Yanru Liu, Wenlin Liu, Bo Su, and Shibao Li. 2021. "The Development of Filler Morphology in Dental Resin Composites: A Review" Materials 14, no. 19: 5612. https://doi.org/10.3390/ma14195612
APA StyleLiu, J., Zhang, H., Sun, H., Liu, Y., Liu, W., Su, B., & Li, S. (2021). The Development of Filler Morphology in Dental Resin Composites: A Review. Materials, 14(19), 5612. https://doi.org/10.3390/ma14195612









