Comparison of the Fracture Resistance and Fracture Mode of Contemporary Restorative Materials to Overcome the Offset of Mandibular Implant-Supported, Cement-Retained Crowns
Abstract
:1. Introduction
2. Materials and Methods
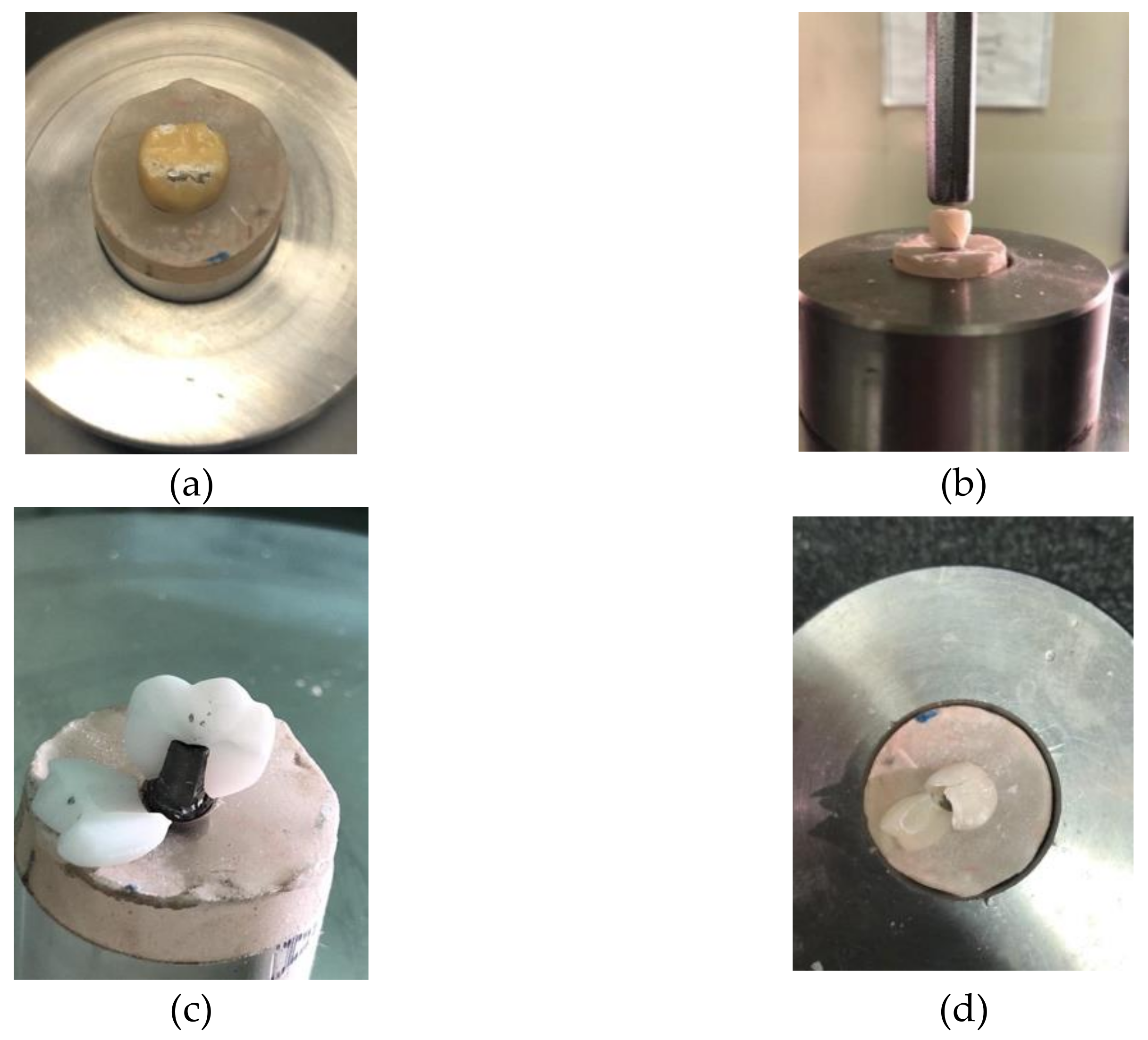
2.1. Implant Mounting and Metal Coping Fabrication
2.2. Fabrication of the Groups
2.2.1. Group A: Porcelain Fused to Metal Crowns
2.2.2. Group B: Monolithic Full Zirconia Crowns
2.2.3. Group C: Zirconia Copings with Ceramic Veneer
2.2.4. Group D: Full Contour Lithium Disilicate Crowns
2.3. Cementation of Crowns
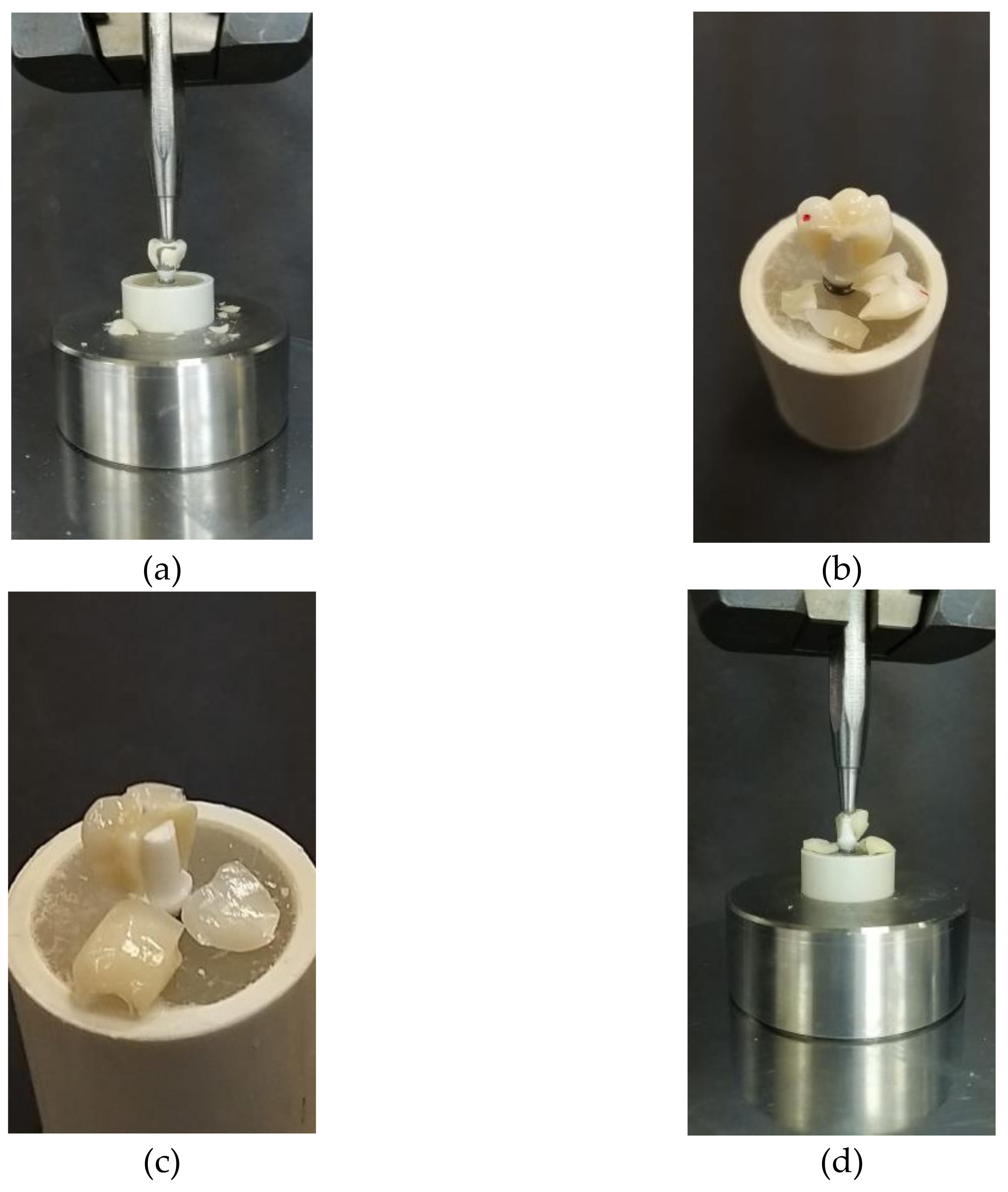
2.4. Fracture Load Testing
2.5. Data Analysis
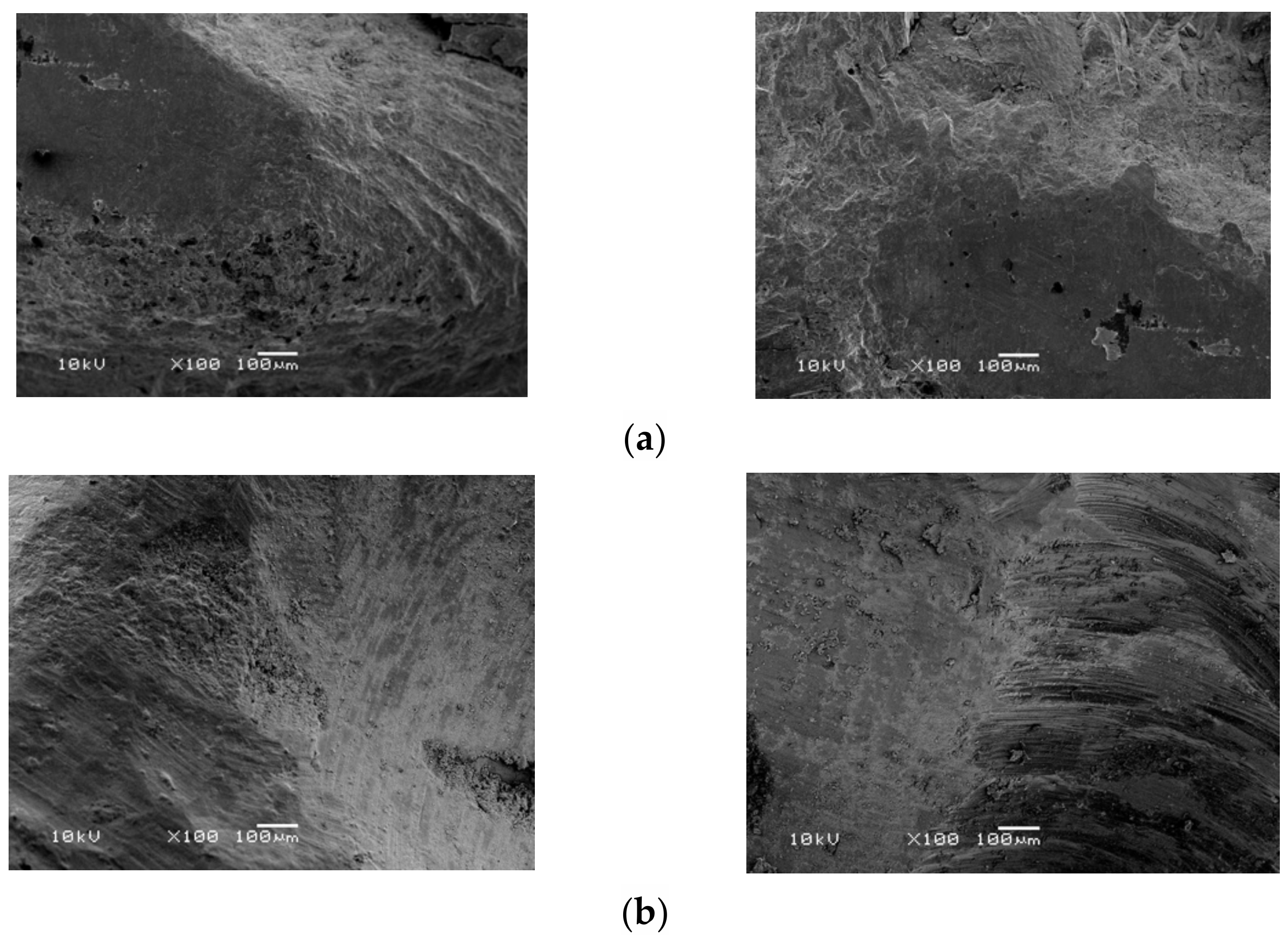
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Weigl, P.; Saarepera, K.; Hinrikus, K.; Wu, Y.; Trimpou, G.; Lorenz, J. Screw-retained monolithic zirconia vs. cemented porcelain-fused-to-metal implant crowns: A prospective randomized clinical trial in split-mouth design. Clin. Oral Investig. 2018, 23, 1067–1075. [Google Scholar] [CrossRef]
- Donati, M.; Ekestubbe, A.; Lindhe, J.; Wennström, J.L. Implant-supported single-tooth restorations. A 12-year prospective study. Clin. Oral Implant. Res. 2015, 27, 1207–1211. [Google Scholar] [CrossRef] [PubMed]
- Walton, T.R. An Up-to-15-Year Comparison of the Survival and Complication Burden of Three-Unit Tooth-Supported Fixed Dental Prostheses and Implant-Supported Single Crowns. Int. J. Oral Maxillofac. Implant. 2015, 30, 851–861. [Google Scholar] [CrossRef] [Green Version]
- Pariente, L.; Dada, K.; Daas, M.; Linder, S.; Dard, M. Evaluation of the Treatment of Partially Edentulous Patients with Bone Level Tapered Implants: 24-Month Clinical and Radiographic Follow-Up. J. Oral Implantol. 2020, 46, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Att, W.; Kurun, S.; Gerds, T.A.; Strub, J.R. Fracture resistance of single-tooth implant-supported all-ceramic restorations: An in vitro study. J. Prosthet. Dent. 2006, 95, 111–116. [Google Scholar] [CrossRef]
- Buser, D.; Janner, S.F.M.; Wittneben, J.-G.; Brägger, U.; Ramseier, C.A.; Salvi, G.E. 10-Year Survival and Success Rates of 511 Titanium Implants with a Sandblasted and Acid-Etched Surface: A Retrospective Study in 303 Partially Edentulous Patients. Clin. Implant. Dent. Relat. Res. 2012, 14, 839–851. [Google Scholar] [CrossRef]
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Gjelvold, B.; Chrcanovic, B.; Bagewitz, I.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Esthetic and Patient-Centered Outcomes of Single Implants: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 1065–1073. [Google Scholar] [CrossRef] [Green Version]
- El-S’Adany, A.; Masoud, G.; Kamel, M.; Korsel, A. Fracture resistance of all ceramic crowns supported by zirconia and alumina versus titanium implant abutments. Tanta Dent. J. 2013, 10, 103–111. [Google Scholar] [CrossRef] [Green Version]
- Monje, A.; Ravidà, A.; Wang, H.-L.; Helms, J.A.; Brunski, J.B. Relationship Between Primary/Mechanical and Secondary/Biological Implant Stability. Int. J. Oral Maxillofac. Implant. 2019, 34, s7–s23. [Google Scholar] [CrossRef]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.F.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin. Oral Implant. Res. 2012, 23, 163–201. [Google Scholar] [CrossRef] [PubMed]
- Lucchese, A.; Gherlone, E.; Portelli, M.; Bertossi, D. Tooth Orthodontic Movement after Maxillofacial Surgery. Eur. J. Inflamm. 2012, 10, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Scarano, A.; Murmura, G.; Sinjiari, B.; Sollazzo, V.; Spinelli, G.; Carinci, F. Analysis and Structural Examination of Screw Loosening in Oral Implants. Int. J. Immunopathol. Pharmacol. 2011, 24, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Sinjari, B.; D’Addazio, G.; Traini, T.; Varvara, G.; Scarano, A.; Murmura, G.; Caputi, S. A 10-year retrospective comparative human study on screw-retained versus cemented dental implant abutments. J. Biol. Regul. Homeost. Agents 2019, 33, 787–797. [Google Scholar]
- Raigrodski, A.J.; Hillstead, M.B.; Meng, G.K.; Chung, K.H. Survival and Complications of Zirconia—Based Fixed Dental Prostheses: A Systematic Review. Smile Dent. J. 2014, 9, 36. [Google Scholar] [CrossRef]
- Sorrentino, R.; De Simone, G.; Tetè, S.; Russo, S.; Zarone, F. Five-year prospective clinical study of posterior three-unit zirconia-based fixed dental prostheses. Clin. Oral Investig. 2011, 16, 977–985. [Google Scholar] [CrossRef]
- Al-Omari, W.M.; Shadid, R.; Abu-Naba’A, L.; El Masoud, B. Porcelain Fracture Resistance of Screw-Retained, Cement-Retained, and Screw-Cement-Retained Implant-Supported Metal Ceramic Posterior Crowns. J. Prosthodont. 2010, 19, 263–273. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Eichberger, M.; Kappert, H.F.; Gernet, W.; Edelhoff, D. High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings—A new fabrication mode for all-ceramic restorations. Dent. Mater. 2009, 25, 121–128. [Google Scholar] [CrossRef]
- Senyilmaz, D.P.; Canay, S.; Heydecke, G.; Strub, J.R. Influence of thermomechanical fatigue loading on the fracture resistance of all-ceramic posterior crowns. Eur. J. Prosthodont. Restor. Dent. 2010, 18, 50–54. [Google Scholar]
- Obermeier, M.; Ristow, O.; Erdelt, K.; Beuer, F. Mechanical performance of cement– and screw–retained all–ceramic single crowns on dental implants. Clin. Oral Investig. 2017, 22, 981–991. [Google Scholar] [CrossRef]
- Rosentritt, M.; Hahnel, S.; Engelhardt, F.; Behr, M.; Preis, V. In vitro performance and fracture resistance of CAD/CAM-fabricated implant supported molar crowns. Clin. Oral Investig. 2016, 21, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Bichacho, N.; Landsberg, C.J. Single implant restorations: Prosthetically induced soft tissue topography. Pract. Periodontics Aesthetic Dent. 1997, 9, 745–752. [Google Scholar]
- Cheng, C.-W.; Chien, C.-H.; Chen, C.-J.; Papaspyridakos, P. Randomized Controlled Clinical Trial to Compare Posterior Implant-Supported Modified Monolithic Zirconia and Metal-Ceramic Single Crowns: One-Year Results. J. Prosthodont. 2018, 28, 15–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rao, S.; Chowdhary, R. Comparison of Fracture Toughness of All-Ceramic and Metal–Ceramic Cement Retained Implant Crowns: An In Vitro Study. J. Indian Prosthodont. Soc. 2014, 14, 408–414. [Google Scholar] [CrossRef]
- Staubli, N.; Walter, C.; Schmidt, J.C.; Weiger, R.; Zitzmann, N.U. Excess cement and the risk of peri-implant disease—A systematic review. Clin. Oral Implant. Res. 2016, 28, 1278–1290. [Google Scholar] [CrossRef]
- de Kok, P.; Kleverlaan, C.J.; de Jager, N.; Kuijs, R.; Feilzer, A.J. Mechanical performance of implant-supported posterior crowns. J. Prosthet. Dent. 2015, 114, 59–66. [Google Scholar] [CrossRef]
- Elshiyab, S.H.; Nawafleh, N.; Öchsner, A.; George, R. Fracture resistance of implant-supported monolithic crowns cemented to zirconia hybrid-abutments: Zirconia-based crowns vs. lithium disilicate crowns. J. Adv. Prosthodont. 2018, 10, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Hussien, A.N.M.; Rayyan, M.; Sayed, N.M.; Segaan, L.G.; Goodacre, C.J.; Kattadiyil, M.T. Effect of screw-access channels on the fracture resistance of 3 types of ceramic implant-supported crowns. J. Prosthet. Dent. 2016, 116, 214–220. [Google Scholar] [CrossRef]
- Honda, J.; Komine, F.; Kamio, S.; Taguchi, K.; Blatz, M.B.; Matsumura, H. Fracture resistance of implant-supported screw-retained zirconia-based molar restorations. Clin. Oral Implant. Res. 2016, 28, 1119–1126. [Google Scholar] [CrossRef]
- Taguchi, K.; Fushiki, R.; Kamio, S.; Komine, F.; Blatz, M.B.; Matsumura, H. Fracture resistance of single-tooth implant-supported zirconia-based indirect composite-layered molar restorations. Clin. Oral Implant. Res. 2013, 25, 983–991. [Google Scholar] [CrossRef] [PubMed]
- Capparé, P.; Vinci, R.; Di Stefano, D.A.; Traini, T.; Pantaleo, G.; Gherlone, E.F.; Gastaldi, G. Correlation between Initial BIC and the Insertion Torque/Depth Integral Recorded with an Instantaneous Torque-Measuring Implant Motor: An in vivo Study. Clin. Implant. Dent. Relat. Res. 2015, 17, e613-20. [Google Scholar] [CrossRef] [PubMed]


| Group | Material | |
|---|---|---|
| Group A | Coping | Veneering Ceramic |
| Metal coping: Wiron® 99 (BEGO USA Inc. Lincoln, RI, USA) | Vita feldspathic porcelain: (Vita, Zahnfabrik, Bad Sackingen, Switzerland.) | |
| Group B | Monolithic Zirconia: Ceramill Zolid fx multilayer (Amann Girrbach AG, Koblach, Austria) | |
| Group C | Bilayered Zirconia: Ceramill Zolid fx multilayer (Amann Girrbach AG, Koblach, Austria) | Lithium disilicate: IPS e.max Ceram. (Ivoclar Vivadent, Liechenstein, Switzerland) |
| Group D | Lithium Disilicate: IPS e.max Press (Ivoclar Vivadent, Liechenstein, Switzerland) | |
| Implant System | Abutments | |
| OsseoSpeed® TX (Astra Tech®, Dentsply Sirona, Charlotte, NC, USA) | TiDesignTM (Astra Tech®, Dentsply Sirona, Charlotte, NC, USA) | |
| ZirDesignTM (Astra Tech®, Dentsply Sirona, Charlotte, NC, USA) | ||
| Abutment | Group | N | * Mean (MPa) | Std. Deviation | ANOVA p-Value | 95% Confidence Interval for Mean | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Titanium | PFM | 10 | 3.029 | 0.262 | 0.000 | 2.842 | 3.216 |
| Monolithic Zirconia | 10 | 2.417 | 0.341 | 2.173 | 2.661 | ||
| Layered Zirconia | 10 | 1.955 | 0.187 | 1.821 | 2.088 | ||
| Lithium Disilicate | 10 | 1.135 | 0.305 | 0.917 | 1.353 | ||
| Zirconia | PFM | 10 | 2.59 | 0.39 | 0.000 | 2.310 | 2.880 |
| Monolithic Zirconia | 10 | 2.47 | 0.31 | 2.253 | 2.697 | ||
| Layered Zirconia | 10 | 1.99 | 0.40 | 1.698 | 2.285 | ||
| Lithium Disilicate | 10 | 1.68 | 0.13 | 1.594 | 1.781 | ||
| Abutment | Group | PFM | Monolithic Zirconia | Layered Zirconia | Lithium Disilicate |
|---|---|---|---|---|---|
| Titanium | PFM | 1 | 0.000 | 0.000 | 0.000 |
| Monolithic Zirconia | 0.000 | 1 | 0.004 | 0.000 | |
| Layered Zirconia | 0.000 | 0.004 | 1 | 0.000 | |
| Lithium Disilicate | 0.000 | 0.000 | 0.000 | 1 | |
| Zirconia | PFM | 1 | 0.850 | 0.001 | 0.000 |
| Monolithic Zirconia | 0.850 | 1 | 0.012 | 0.000 | |
| Layered Zirconia | 0.001 | 0.012 | 1 | 0.190 | |
| Lithium Disilicate | 0.000 | 0.000 | 0.190 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bajunaid, S.O.; Alshiddi, I.; Alhomaidhi, L.; Almutairi, R.; Alolayan, S.; Habib, S.R. Comparison of the Fracture Resistance and Fracture Mode of Contemporary Restorative Materials to Overcome the Offset of Mandibular Implant-Supported, Cement-Retained Crowns. Materials 2021, 14, 4838. https://doi.org/10.3390/ma14174838
Bajunaid SO, Alshiddi I, Alhomaidhi L, Almutairi R, Alolayan S, Habib SR. Comparison of the Fracture Resistance and Fracture Mode of Contemporary Restorative Materials to Overcome the Offset of Mandibular Implant-Supported, Cement-Retained Crowns. Materials. 2021; 14(17):4838. https://doi.org/10.3390/ma14174838
Chicago/Turabian StyleBajunaid, Salwa Omar, Ibraheem Alshiddi, Lamya Alhomaidhi, Rania Almutairi, Shoq Alolayan, and Syed Rashid Habib. 2021. "Comparison of the Fracture Resistance and Fracture Mode of Contemporary Restorative Materials to Overcome the Offset of Mandibular Implant-Supported, Cement-Retained Crowns" Materials 14, no. 17: 4838. https://doi.org/10.3390/ma14174838
APA StyleBajunaid, S. O., Alshiddi, I., Alhomaidhi, L., Almutairi, R., Alolayan, S., & Habib, S. R. (2021). Comparison of the Fracture Resistance and Fracture Mode of Contemporary Restorative Materials to Overcome the Offset of Mandibular Implant-Supported, Cement-Retained Crowns. Materials, 14(17), 4838. https://doi.org/10.3390/ma14174838






