Stress Concentration of Endodontically Treated Molars Restored with Transfixed Glass Fiber Post: 3D-Finite Element Analysis
Abstract
1. Introduction
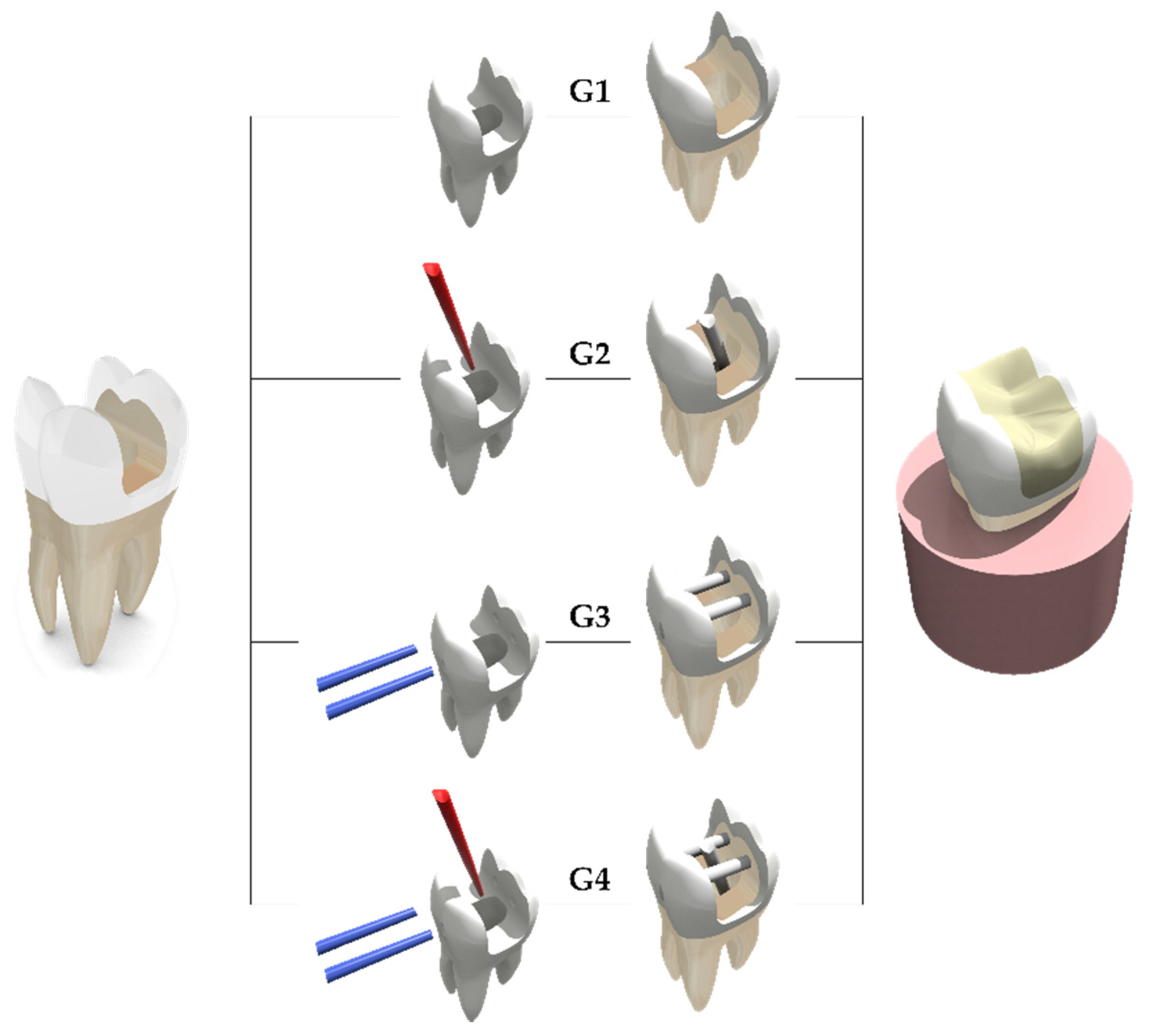
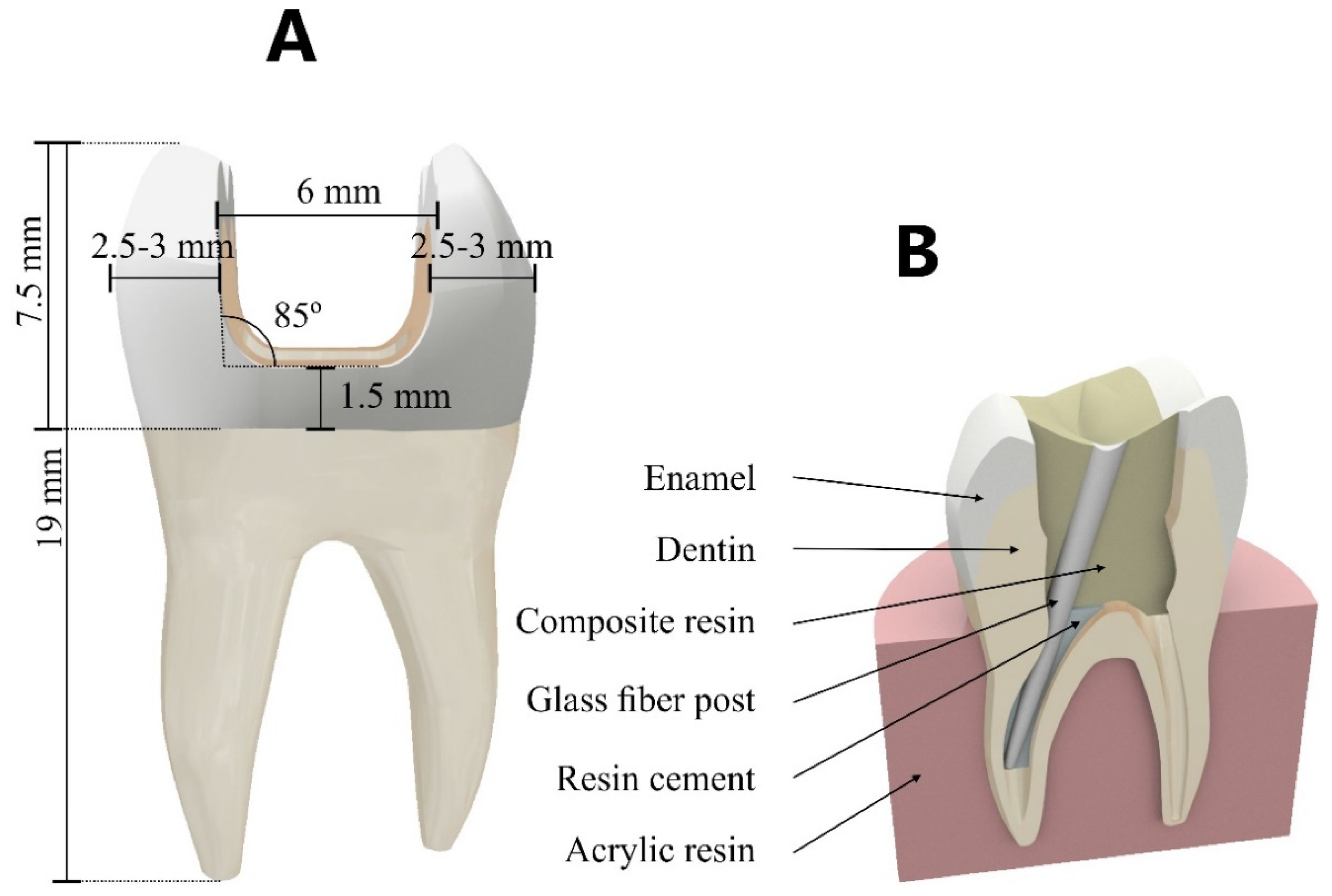
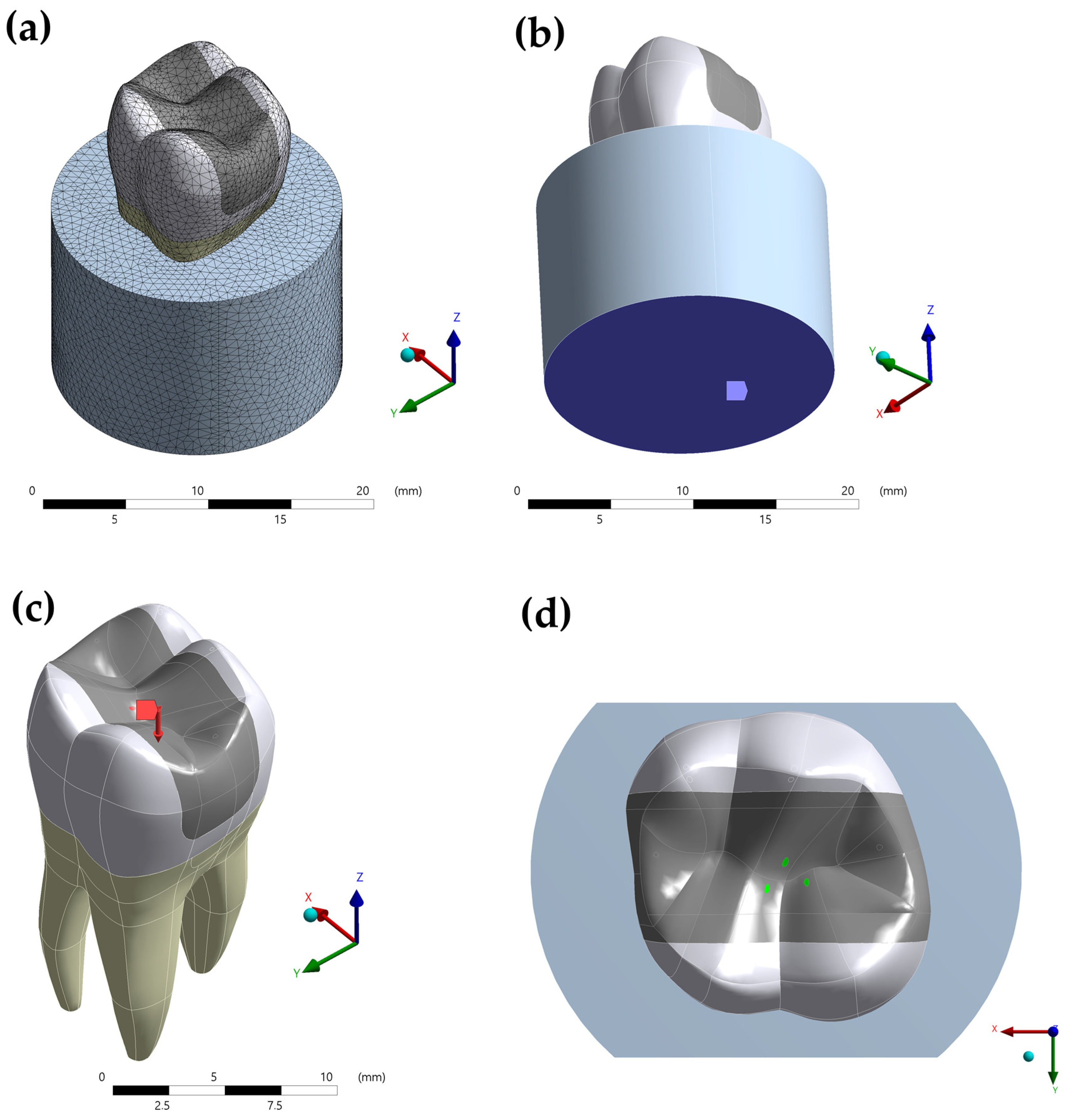
2. Materials and Methods
2.1. Modelling
2.2. Pre-Processing
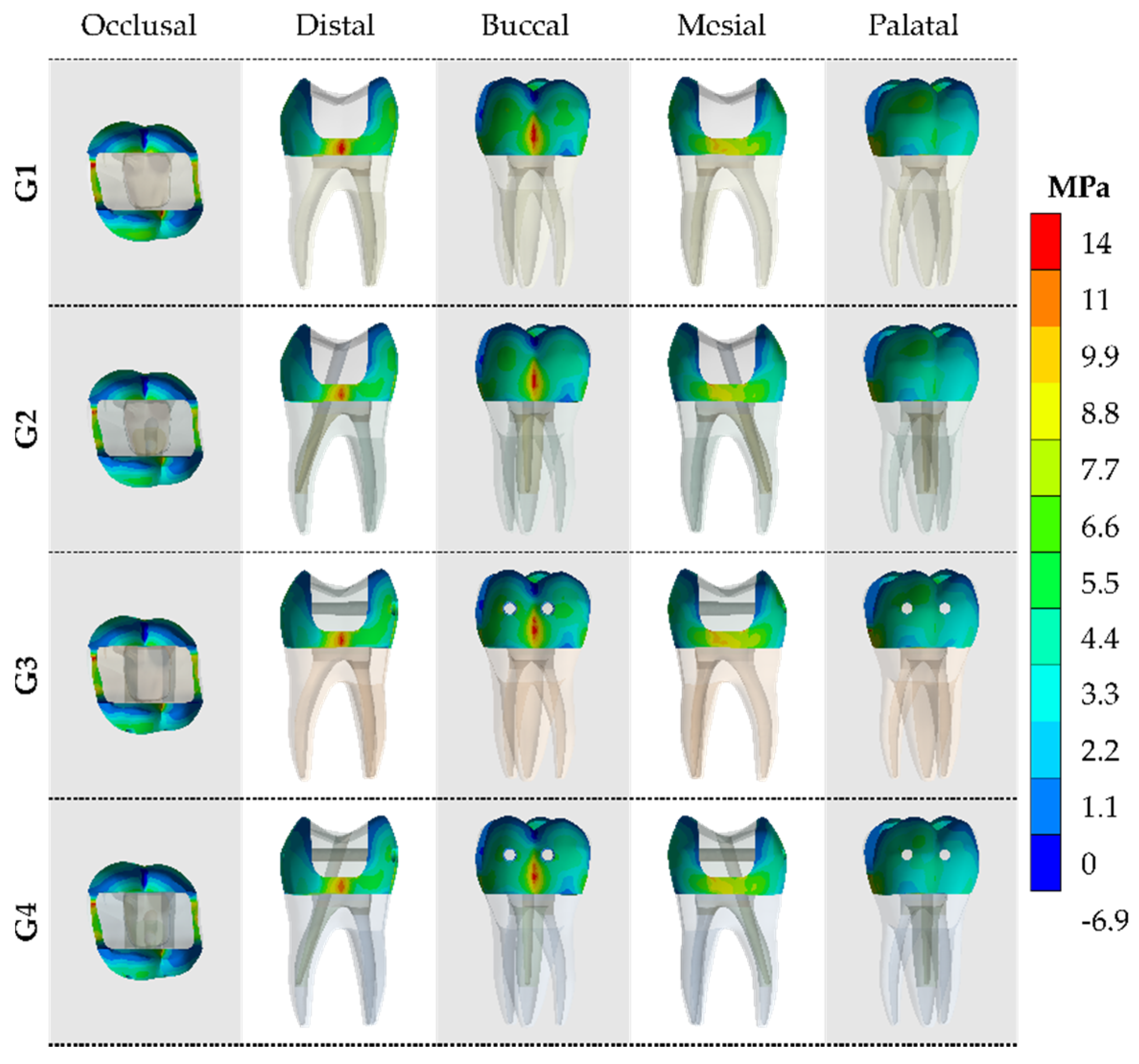
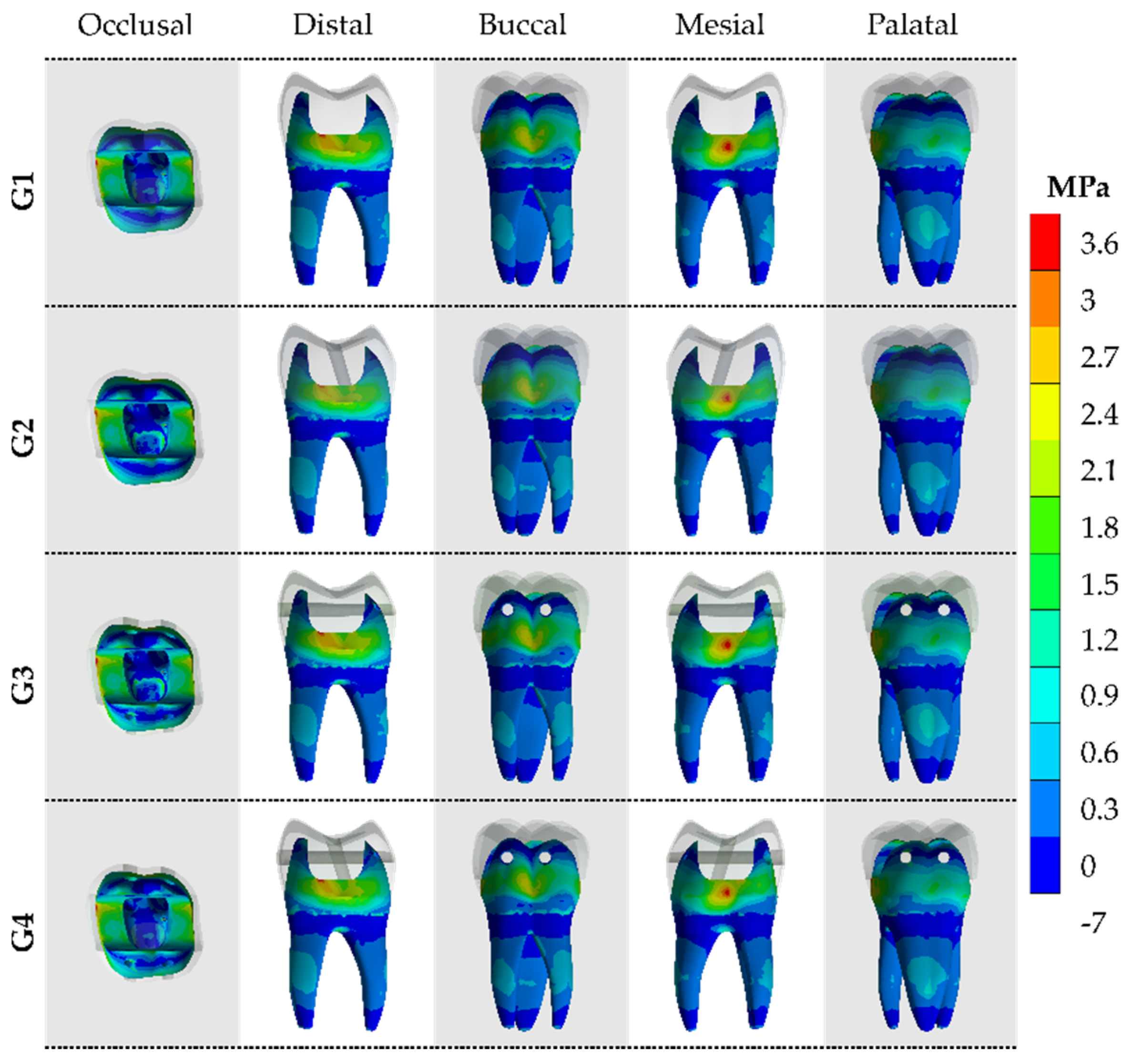
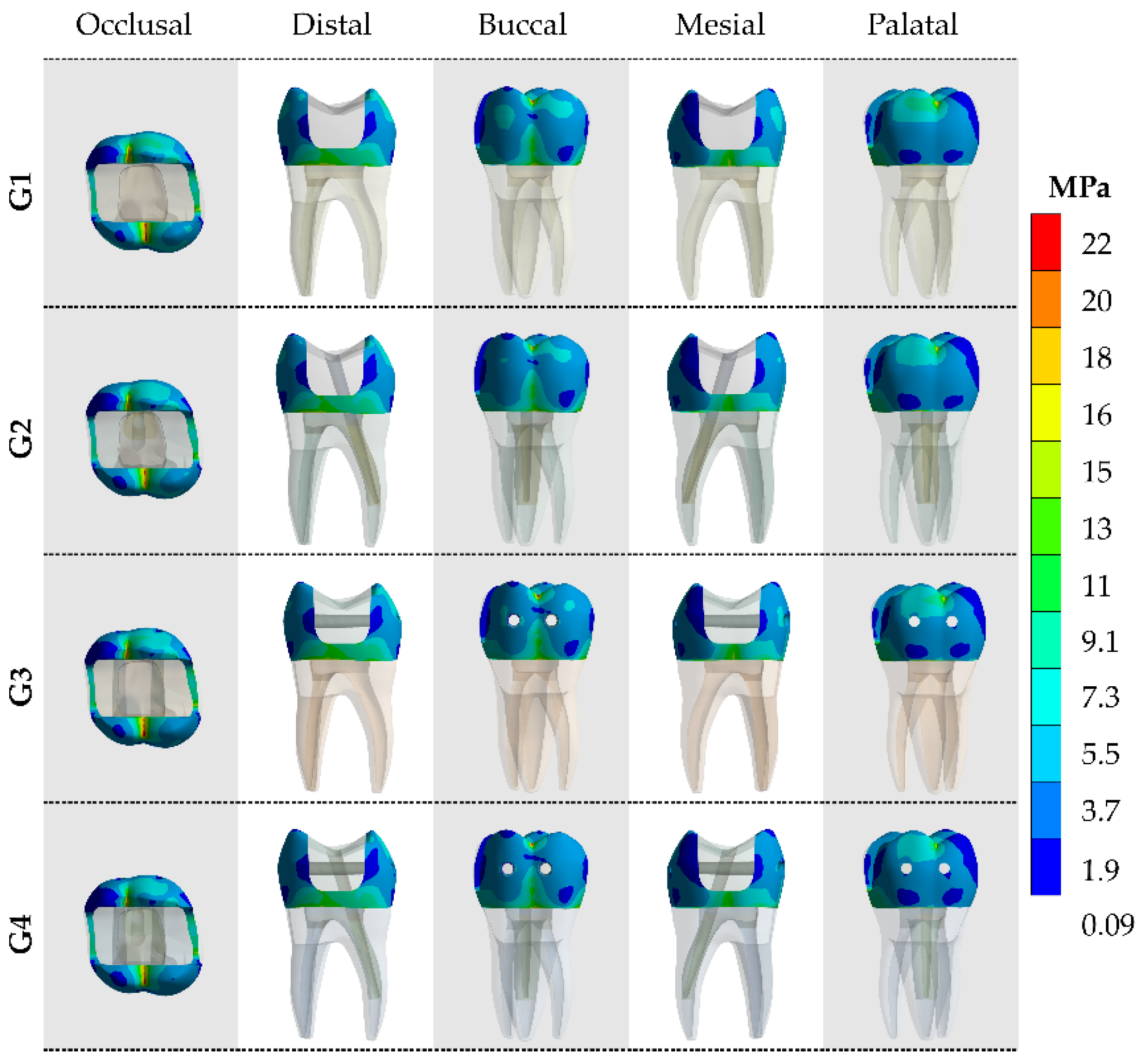
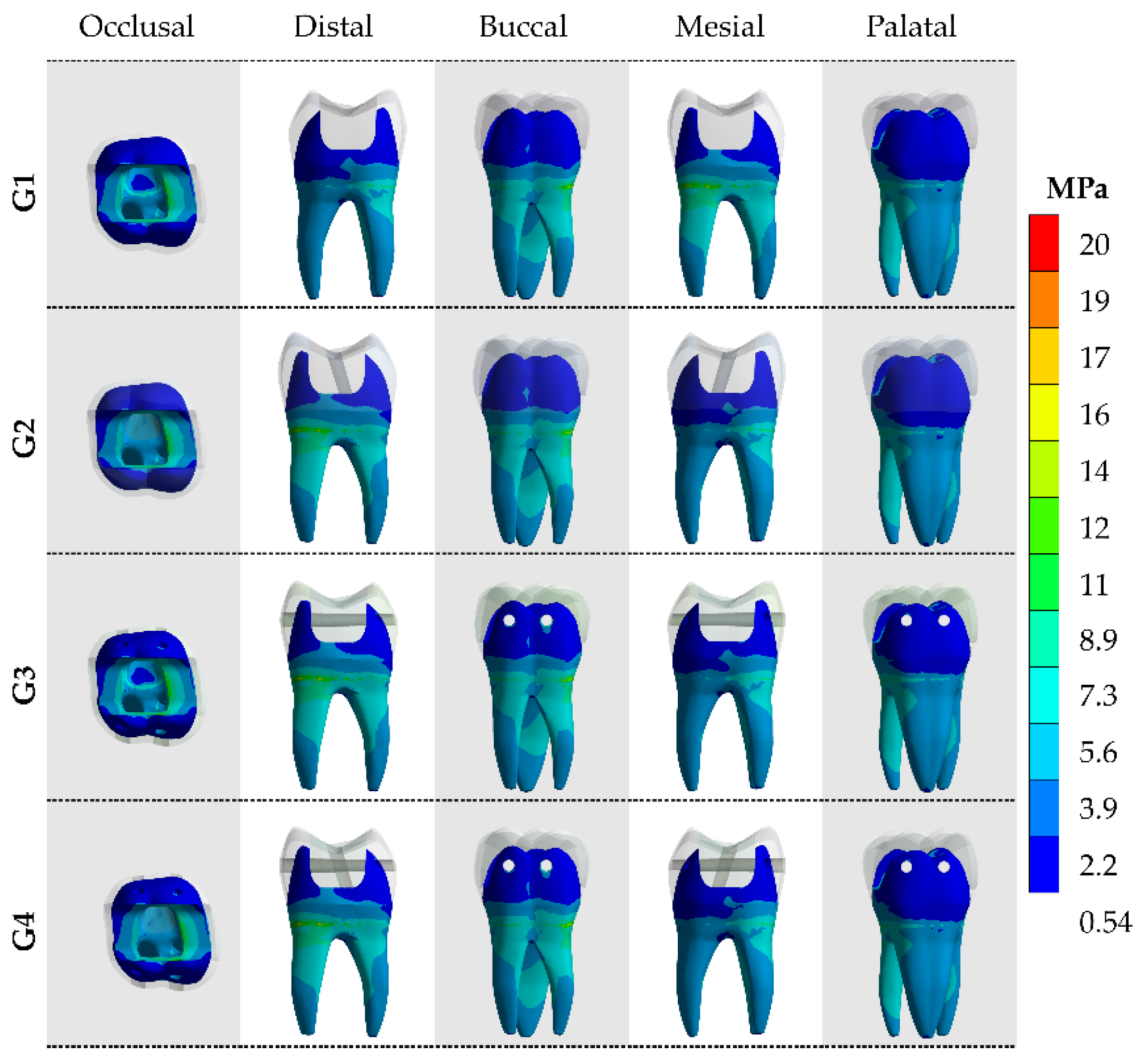
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- da Silva, P.B.; Duarte, S.F.; Alcalde, M.P.; Duarte, M.A.H.; Vivan, R.R.; da Rosa, R.A.; Só, M.V.R.; do Nascimento, A.L. Influence of cervical preflaring and root canal preparation on the fracture resistance of endodontically treated teeth. BMC Oral Health 2020, 20, 111. [Google Scholar] [CrossRef]
- Fernandes, A.S.; Dessai, G.S. Factors affecting the fracture resistance of post-core reconstructed teeth: A review. Int. J. Prosthodont. 2001, 14, 355–363. [Google Scholar]
- Göktürk, H.; Karaarslan, E.Ş.; Tekin, E.; Hologlu, B.; Sarıkaya, I. The effect of the different restorations on fracture resistance of root-filled premolars. BMC Oral Health 2018, 18, 196. [Google Scholar] [CrossRef]
- Scotti, N.; Michelotto Tempesta, R.; Pasqualini, D.; Baldi, A.; Vergano, E.A.; Baldissara, P.; Alovisi, M.; Comba, A. 3D Interfacial Gap and Fracture Resistance of Endodontically Treated Premolars Restored with Fiber-reinforced Composites. J. Adhes. Dent. 2020, 22, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Thakur, A.; Ramarao, S. A comparative evaluation of fracture resistance of endodontically treated premolar teeth reinforced with different prefabricated and custom-made fiber-reinforced post system with two different post lengths: An in vitro study. J. Conserv. Dent. 2019, 22, 376. [Google Scholar] [CrossRef]
- Pierrisnard, L.; Bohin, F.; Renault, P.; Barquins, M. Corono-radicular reconstruction of pulpless teeth: A mechanical study using finite element analysis. J. Prosthet. Dent. 2002, 88, 442–448. [Google Scholar] [CrossRef]
- da Rocha, D.M.; Tribst, J.P.M.; Ausiello, P.; Dal Piva, A.M.D.O.; da Rocha, M.C.; Di Nicoló, R.; Borges, A.L.S. Effect of the restorative technique on load-bearing capacity, cusp deflection, and stress distribution of endodontically-treated premolars with MOD restoration. Restor. Dent. Endod. 2019, 44, e33. [Google Scholar] [CrossRef] [PubMed]
- Scotti, N.; Forniglia, A.; Michelotto Tempesta, R.; Comba, A.; Saratti, C.M.; Pasqualini, D.; Alovisi, M.; Berutti, E. Effects of fiber-glass-reinforced composite restorations on fracture resistance and failure mode of endodontically treated molars. J. Dent. 2016, 53, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Karzoun, W.; Abdulkarim, A.; Samran, A.; Kern, M. Fracture Strength of Endodontically Treated Maxillary Premolars Supported by a Horizontal Glass Fiber Post: An In Vitro Study. J. Endod. 2015, 41, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Kim, S.S.; Levine, J.L.; Piracha, Y.S.; Solomon, C.S. A Novel Approach to Fracture Resistance Using Horizontal Posts after Endodontic Therapy: A Case Report and Review of Literature. J. Endod. 2020, 46, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Reeh, E.S.; Ross, G.K. Tooth stiffness with composite veneers: A strain gauge and finite element evaluation. Dent. Mater. 1994, 10, 247–252. [Google Scholar] [CrossRef]
- Cobankara, F.K.; Unlu, N.; Cetin, A.R.; Ozkan, H.B. The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper. Dent. 2008, 33, 526–533. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, A.B.G.; de Andrade, G.S.; Tribst, J.P.M.; Grassi, E.D.A.; Ausiello, P.; Saavedra, G.D.S.F.A.; Bressane, A.; de Melo, R.M.; Borges, A.L. Mechanical behavior of different restorative materials and onlay preparation designs in endodontically treated molars. Materials 2021, 14, 1923. [Google Scholar] [CrossRef] [PubMed]
- Favero, F.J.; De Melo, T.A.F.; Stona, D.; Mota, E.G.; Spohr, A.M.; Burnett, L.H. Strengthening effect of horizontally placed fiberglass posts in endodontically-treated teeth restored with direct resin composite. Am. J. Dent. 2015, 28, 143–149. [Google Scholar] [PubMed]
- Daher, R.; Feilzer, A.J.; Krejci, I. Novel non-invasive reinforcement of MOD cavities on endodontically treated teeth. J. Dent. 2016, 54, 77–85. [Google Scholar] [CrossRef][Green Version]
- Cantó-Navés, O.; Medina-Galvez, R.; Marimon, X.; Ferrer, M.; Figueras-Álvarez, Ó.; Cabratosa-Termes, J. A 3D Finite Element Analysis Model of Single Implant-Supported Prosthesis under Dynamic Impact Loading for Evaluation of Stress in the Crown, Abutment and Cortical Bone Using Different Rehabilitation Materials. Materials 2021, 14, 3519. [Google Scholar] [CrossRef]
- Lee, J.-H.; Jang, H.Y.; Lee, S.Y. Finite Element Analysis of Dental Implants with Zirconia Crown Restorations: Conventional Cement-Retained vs. Cementless Screw-Retained. Materials 2021, 14, 2666. [Google Scholar] [CrossRef]
- Cicciù, M. Bioengineering Methods of Analysis and Medical Devices: A Current Trends and State of the Art. Materials 2020, 13, 797. [Google Scholar] [CrossRef]
- Nabih, S.M.; Ibrahim, N.I.M.; Elmanakhly, A.R. Mechanical and thermal stress analysis of hybrid ceramic and lithium disilicate based ceramic CAD-CAM inlays using 3-D finite element analysis. Braz. Dent. Sci. 2021, 24. [Google Scholar] [CrossRef]
- Ausiello, P.; Ciaramella, S.; Garcia-Godoy, F.; Martorelli, M.; Sorrentino, R.; Gloria, A. Stress distribution of bulk-fill resin composite in class II restorations. Am. J. Dent. 2017, 30, 227–232. [Google Scholar]
- Martorelli, M.; Ausiello, P. A novel approach for a complete 3D tooth reconstruction using only 3D crown data. Int. J. Interact. Des. Manuf. 2013, 7, 125–135. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Araújo, R.M.; da Silva, J.M.F.; Bottino, M.A.; Kleverlaan, C.J.; de Jager, N. Effect of different materials and undercut on the removal force and stress distribution in circumferential clasps during direct retainer action in removable partial dentures. Dent. Mater. 2020, 36, 179–186. [Google Scholar] [CrossRef]
- Pałka, K.; Bieniaś, J.; Dębski, H.; Niewczas, A. Finite element analysis of thermo-mechanical loaded teeth. Comput. Mater. Sci. 2012, 64, 289–294. [Google Scholar] [CrossRef]
- Holmes, D.C.; Diaz-Arnold, A.M.; Leary, J.M. Influence of post dimension on stress distribution in dentin. J. Prosthet. Dent. 1996, 75, 140–147. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Borges, A.L.S.; Silva-Concílio, L.R.; Bottino, M.A.; Özcan, M. Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D-FEA Study. Materials 2021, 14, 649. [Google Scholar] [CrossRef] [PubMed]
- Lanza, A.; Aversa, R.; Rengo, S.; Apicella, D.; Apicella, A. 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent. Mater. 2005, 21, 709–715. [Google Scholar] [CrossRef]
- Skupien, J.A.; Opdam, N.; Winnen, R.; Bronkhorst, E.; Kreulen, C.; Pereira-Cenci, T.; Huysmans, M.-C. A Practice-based Study on the Survival of Restored Endodontically Treated Teeth. J. Endod. 2013, 39, 1335–1340. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.M.; Santiago, S.L.; Fernandes, C.A.; Suh, B.I.; Pashley, D.H. Effects of prism orientation on tensile strength of enamel. J. Adhes. Dent. 2000, 2, 251–257. [Google Scholar] [PubMed]
- Staninec, M.; Marshall, G.W.; Hilton, J.F.; Pashley, D.H.; Gansky, S.A.; Marshall, S.J.; Kinney, J.H. Ultimate tensile strength of dentin: Evidence for a damage mechanics approach to dentin failure. J. Biomed. Mater. Res. 2002, 63, 342–345. [Google Scholar] [CrossRef]
- Bromberg, C.R.; Alves, C.B.; Stona, D.; Spohr, A.M.; Rodrigues-Junior, S.A.; Melara, R.; Burnett, L.H. Fracture resistance of endodontically treated molars restored with horizontal fiberglass posts or indirect techniques. J. Am. Dent. Assoc. 2016, 147, 952–958. [Google Scholar] [CrossRef]
- De Andrade, G.S.; Tribst, J.P.M.; Orozco, E.I.; Augusto, M.G.; Bottino, M.A.; Borges, A.L.; Anami, L.C.; Saavedra, G.D. Influence of different post-endodontic restorations on the fatigue survival and biomechanical behavior of central incisors. Am. J. Dent. 2020, 33, 227–234. [Google Scholar] [PubMed]
- Stricker, E.J.; Göhring, T.N. Influence of different posts and cores on marginal adaptation, fracture resistance, and fracture mode of composite resin crowns on human mandibular premolars. An in vitro study. J. Dent. 2006, 34, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Abou-Elnaga, M.Y.; Alkhawas, M.-B.A.M.; Kim, H.-C.; Refai, A.S. Effect of Truss Access and Artificial Truss Restoration on the Fracture Resistance of Endodontically Treated Mandibular First Molars. J. Endod. 2019, 45, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Pantvisai, P.; Messer, H.H. Cuspal deflection in molars in relation to endodontic and restorative procedures. J. Endod. 1995, 21, 57–61. [Google Scholar] [CrossRef]
- Mohammadi, N.; Kahnamoii, M.A.; Yeganeh, P.K.; Navimipour, E.J. Effect of Fiber Post and Cusp Coverage on Fracture Resistance of Endodontically Treated Maxillary Premolars Directly Restored with Composite Resin. J. Endod. 2009, 35, 1428–1432. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Qualtrough, A.J.E.; Worthington, H.V.; Watson, T.F.; Pitt Ford, T.R. Randomized clinical comparison of endodontically treated teeth restored with amalgam or with fiber posts and resin composite: Five-year results. Oper. Dent. 2005, 30, 9–15. [Google Scholar] [PubMed]
- Scotti, N.; Eruli, C.; Comba, A.; Paolino, D.S.; Alovisi, M.; Pasqualini, D.; Berutti, E. Longevity of class 2 direct restorations in root-filled teeth: A retrospective clinical study. J. Dent. 2015, 43, 499–505. [Google Scholar] [CrossRef]
- Zarow, M.; Vadini, M.; Chojnacka-Brozek, A.; Szczeklik, K.; Milewski, G.; Biferi, V.; D’Arcangelo, C.; De Angelis, F. Effect of Fiber Posts on Stress Distribution of Endodontically Treated Upper Premolars: Finite Element Analysis. Nanomaterials 2020, 10, 1708. [Google Scholar] [CrossRef]
- Alp, Ş.; Gulec Alagoz, L.; Ulusoy, N. Effect of Direct and Indirect Materials on Stress Distribution in Class II MOD Restorations: A 3D-Finite Element Analysis Study. BioMed Res. Int. 2020, 2020, 7435054. [Google Scholar] [CrossRef]
- Ausiello, P.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Lanzotti, A.; Zamparini, F.; Epifania, E.; Mendes Tribst, J.P. Effect of Shrinking and No Shrinking Dentine and Enamel Replacing Materials in Posterior Restoration: A 3D-FEA Study. Appl. Sci. 2021, 11, 2215. [Google Scholar] [CrossRef]
- Matuda, A.G.N.; Silveira, M.P.M.; Andrade, G.S.D.; Piva, A.M.D.O.D.; Tribst, J.P.M.; Borges, A.L.S.; Testarelli, L.; Mosca, G.; Ausiello, P. Computer Aided Design Modelling and Finite Element Analysis of Premolar Proximal Cavities Restored with Resin Composites. Materials 2021, 14, 2366. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Borges, A.L.S.; Anami, L.C.; Kleverlaan, C.J.; Bottino, M.A. Survival Probability, Weibull Characteristics, Stress Distribution, and Fractographic Analysis of Polymer-Infiltrated Ceramic Network Restorations Cemented on a Chairside Titanium Base: An In Vitro and In Silico Study. Materials 2020, 13, 1879. [Google Scholar] [CrossRef] [PubMed]
| Material | Elastic Modulus (GPa) | Shear Modulus (GPa) | Poisson Ratio | Tensile Strength (MPa) |
|---|---|---|---|---|
| enamel | 84 [23] | - | 0.3 [23] | 15.1–34.3 [28] |
| dentin | 18.6 [24] | - | 0.3 [24] | 44.4–97.8 [29] |
| resin composite | 8.0 [25] | - | 0.25 [25] | - |
| glass fiber post | x = 37 [26] y = 9.5 [26] z = 9.5 [26] | xy = 3.1 [20] xz = 3.5 [20] yz = 3.1 [20] | xy = 0.27 [26] xz = 0.34 [26] yz = 0.27 [26] | - |
| resin cement | 7 [25] | - | 0.24 [25] | - |
| acrylic resin | 2.2 [25] | - | 0.3 [25] | - |
| Model | Glass Fiber Post Approach | Enamel Stress | Dentin Stress |
|---|---|---|---|
| G1 | No-post | 14.5 | 3.7 |
| G2 | Glass fiber in the palatal root canal | 13.9 | 3.2 |
| G3 | Two transfixed glass fiber posts | 14.2 | 3.4 |
| G4 | Two transfixed glass fiber posts and one glass fiber post in the palatal root canal. | 14.0 | 3.3 |
| Model | Glass Fiber Post Approach | Enamel Stress | Dentin Stress |
|---|---|---|---|
| G1 | No-post | 18.17 | 11.68 |
| G2 | Glass fiber in the palatal root canal | 17.58 | 11.18 |
| G3 | Two transfixed glass fiber posts | 17.87 | 11.38 |
| G4 | Two transfixed glass fiber posts and one glass fiber post in the palatal root canal. | 17.68 | 11.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borges, A.L.S.; Grangeiro, M.T.V.; de Andrade, G.S.; de Melo, R.M.; Baroudi, K.; Silva-Concilio, L.R.; Tribst, J.P.M. Stress Concentration of Endodontically Treated Molars Restored with Transfixed Glass Fiber Post: 3D-Finite Element Analysis. Materials 2021, 14, 4249. https://doi.org/10.3390/ma14154249
Borges ALS, Grangeiro MTV, de Andrade GS, de Melo RM, Baroudi K, Silva-Concilio LR, Tribst JPM. Stress Concentration of Endodontically Treated Molars Restored with Transfixed Glass Fiber Post: 3D-Finite Element Analysis. Materials. 2021; 14(15):4249. https://doi.org/10.3390/ma14154249
Chicago/Turabian StyleBorges, Alexandre Luiz Souto, Manassés Tercio Vieira Grangeiro, Guilherme Schmitt de Andrade, Renata Marques de Melo, Kusai Baroudi, Laís Regiane Silva-Concilio, and João Paulo Mendes Tribst. 2021. "Stress Concentration of Endodontically Treated Molars Restored with Transfixed Glass Fiber Post: 3D-Finite Element Analysis" Materials 14, no. 15: 4249. https://doi.org/10.3390/ma14154249
APA StyleBorges, A. L. S., Grangeiro, M. T. V., de Andrade, G. S., de Melo, R. M., Baroudi, K., Silva-Concilio, L. R., & Tribst, J. P. M. (2021). Stress Concentration of Endodontically Treated Molars Restored with Transfixed Glass Fiber Post: 3D-Finite Element Analysis. Materials, 14(15), 4249. https://doi.org/10.3390/ma14154249









