Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow
Abstract
1. Introduction
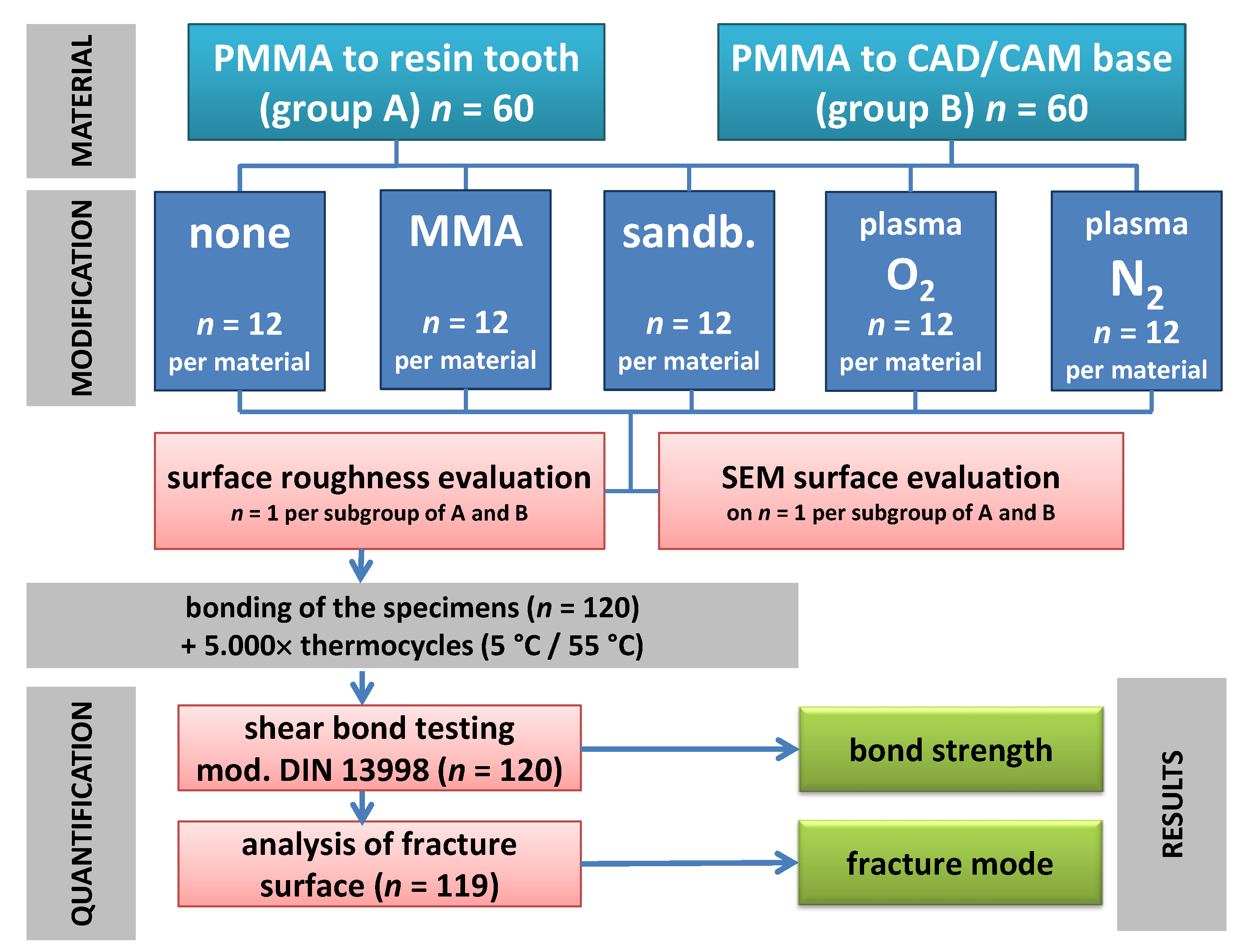
2. Materials and Methods
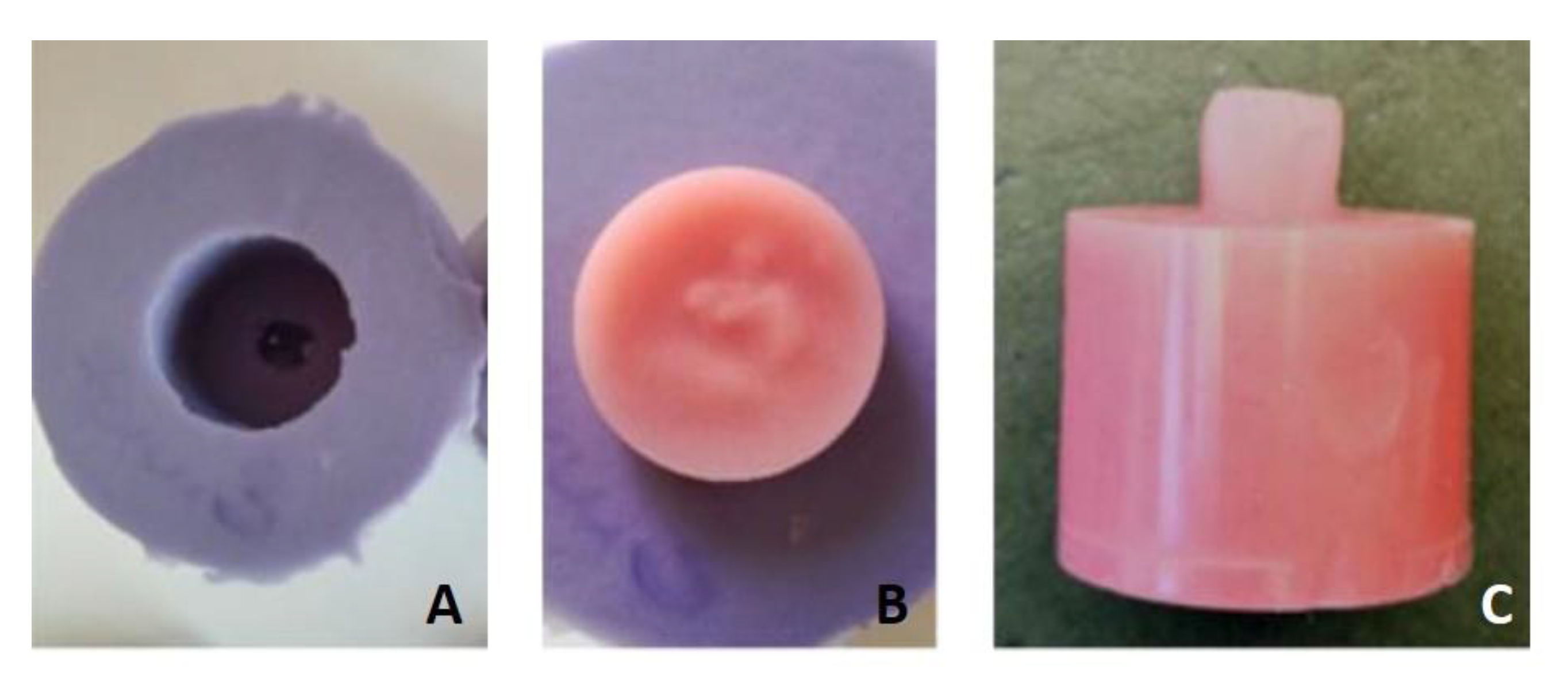
2.1. Arrangements for the Specimens in Group A (Conventional PMMA to Resin Tooth)
2.2. Arrangements for the Specimens in Group B (CAD/CAM PMMA to Conventional PMMA)
2.3. Surface Conditioning, Mating, and Ageing of Specimens
2.4. Surface Characterization
2.5. Assessment of the Bonding Strength and Failure Mode
2.6. Statistical Analysis
3. Results
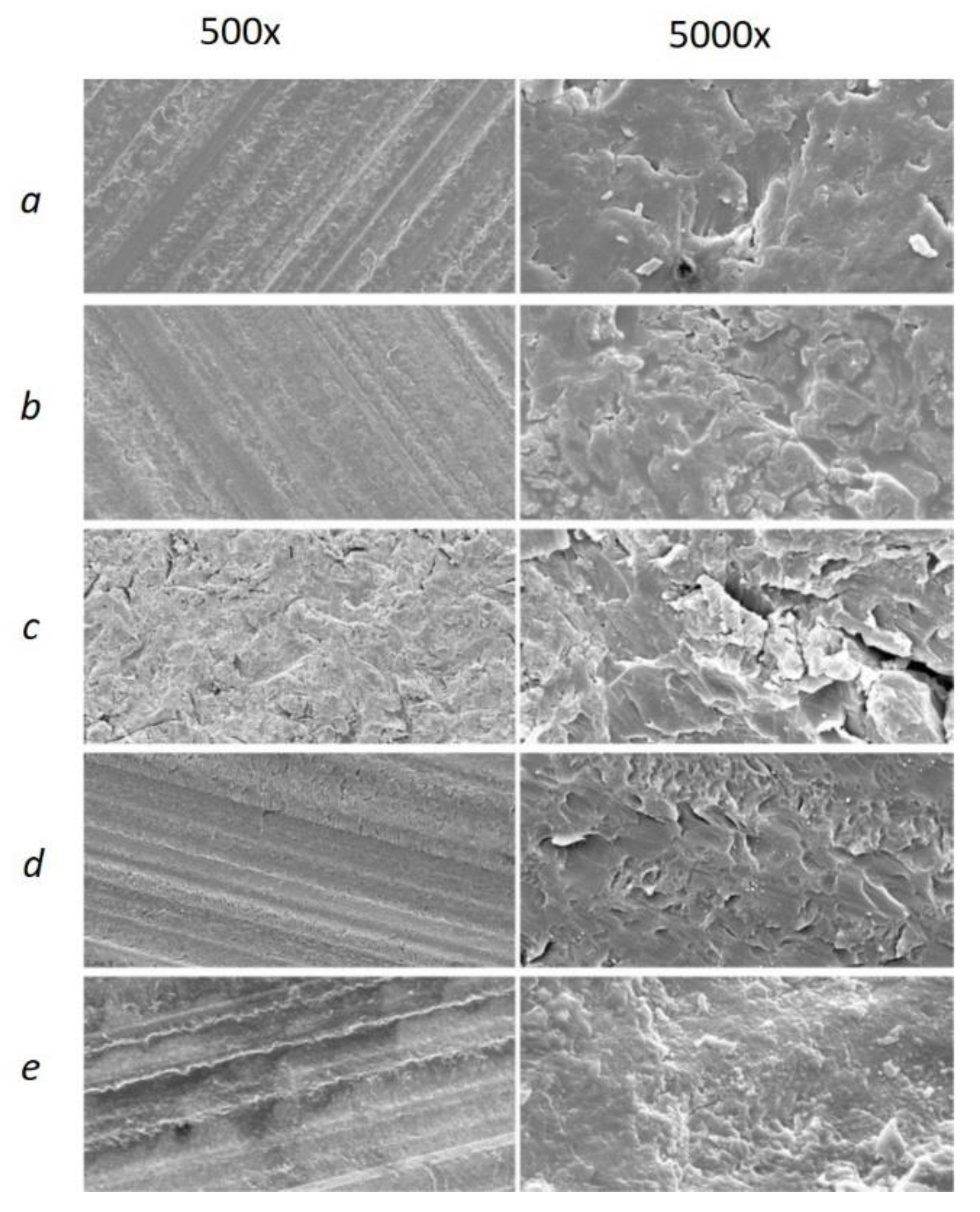
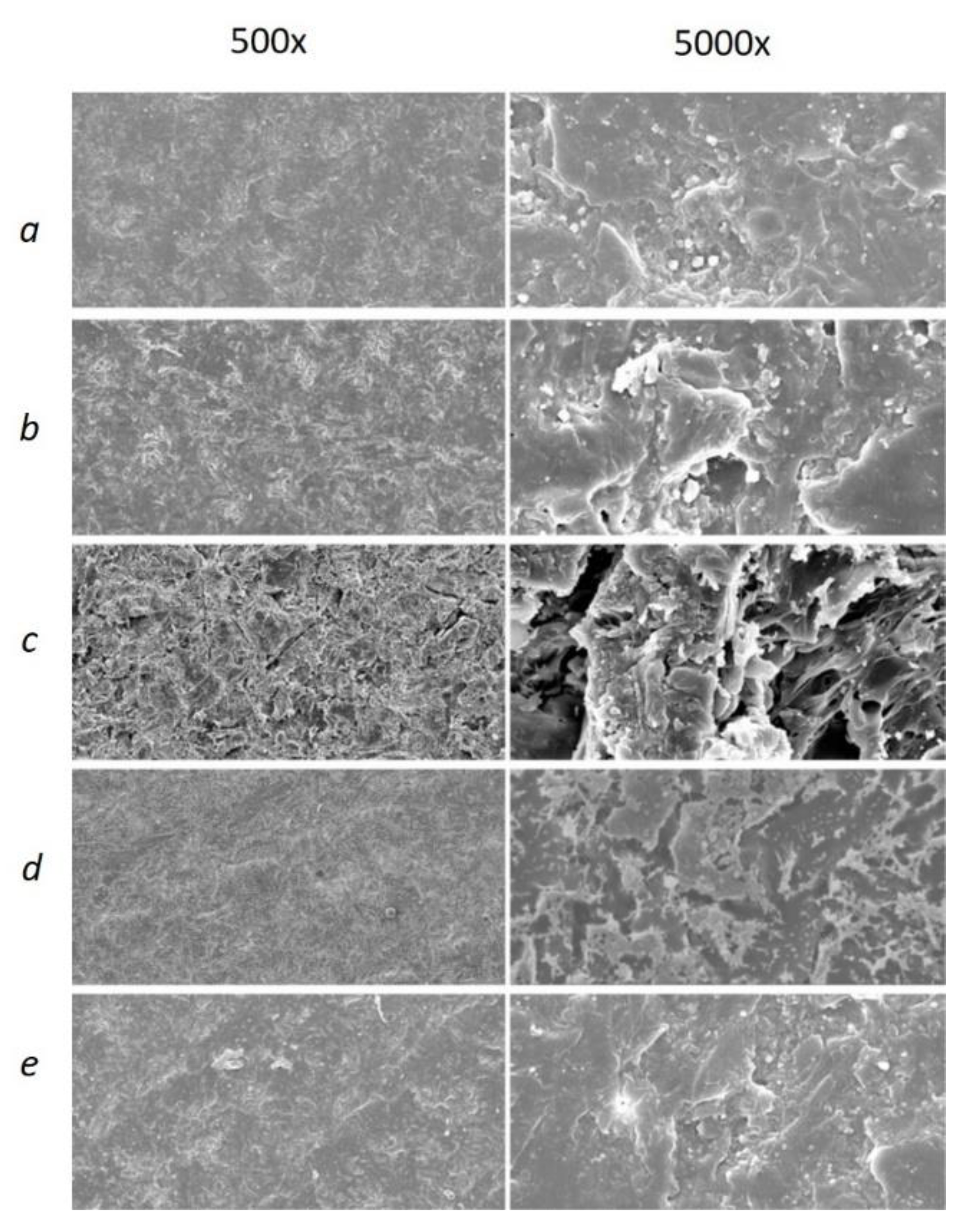
3.1. Initial Surface Characteristics
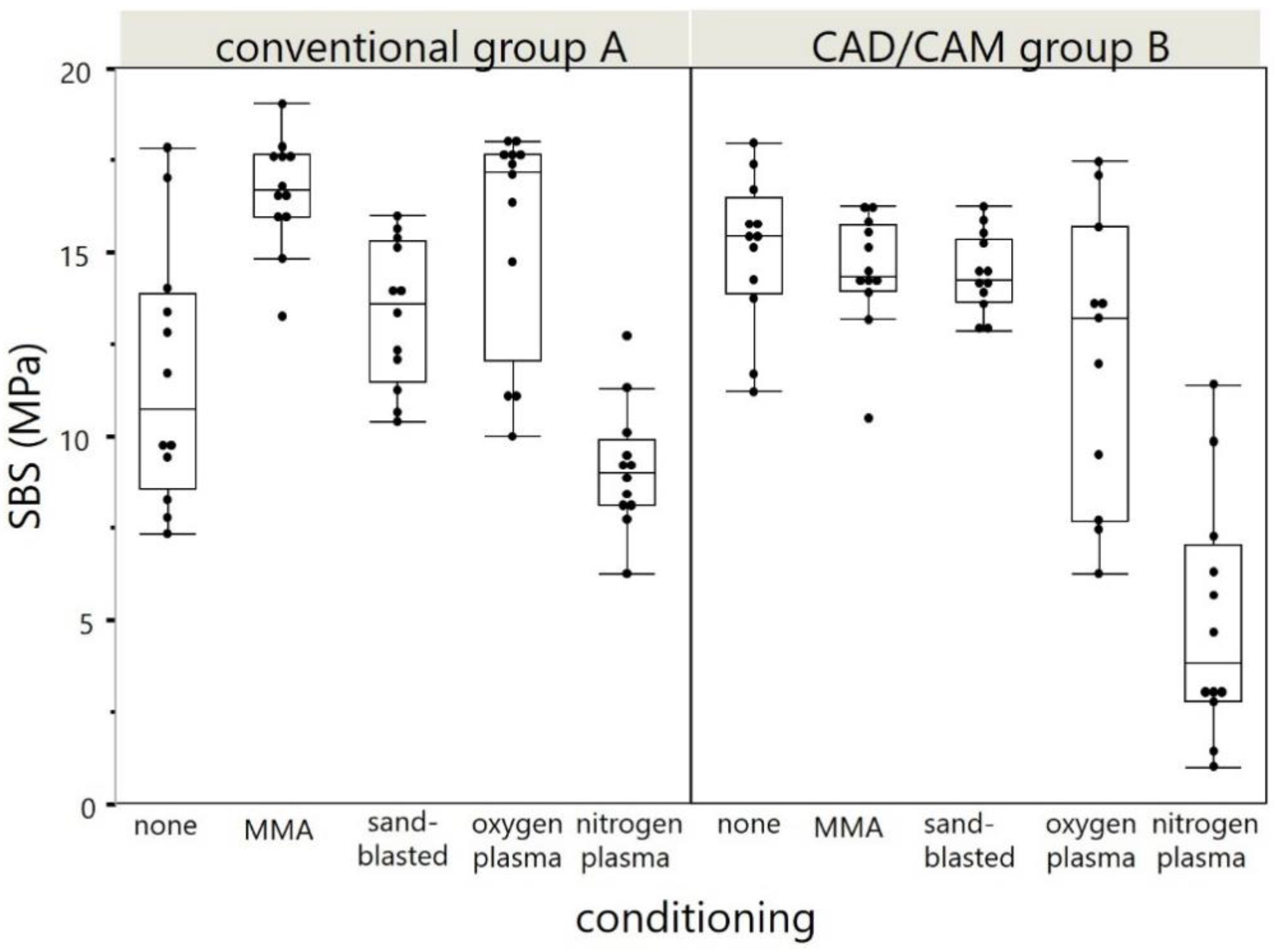
3.2. Shear Bond Strength
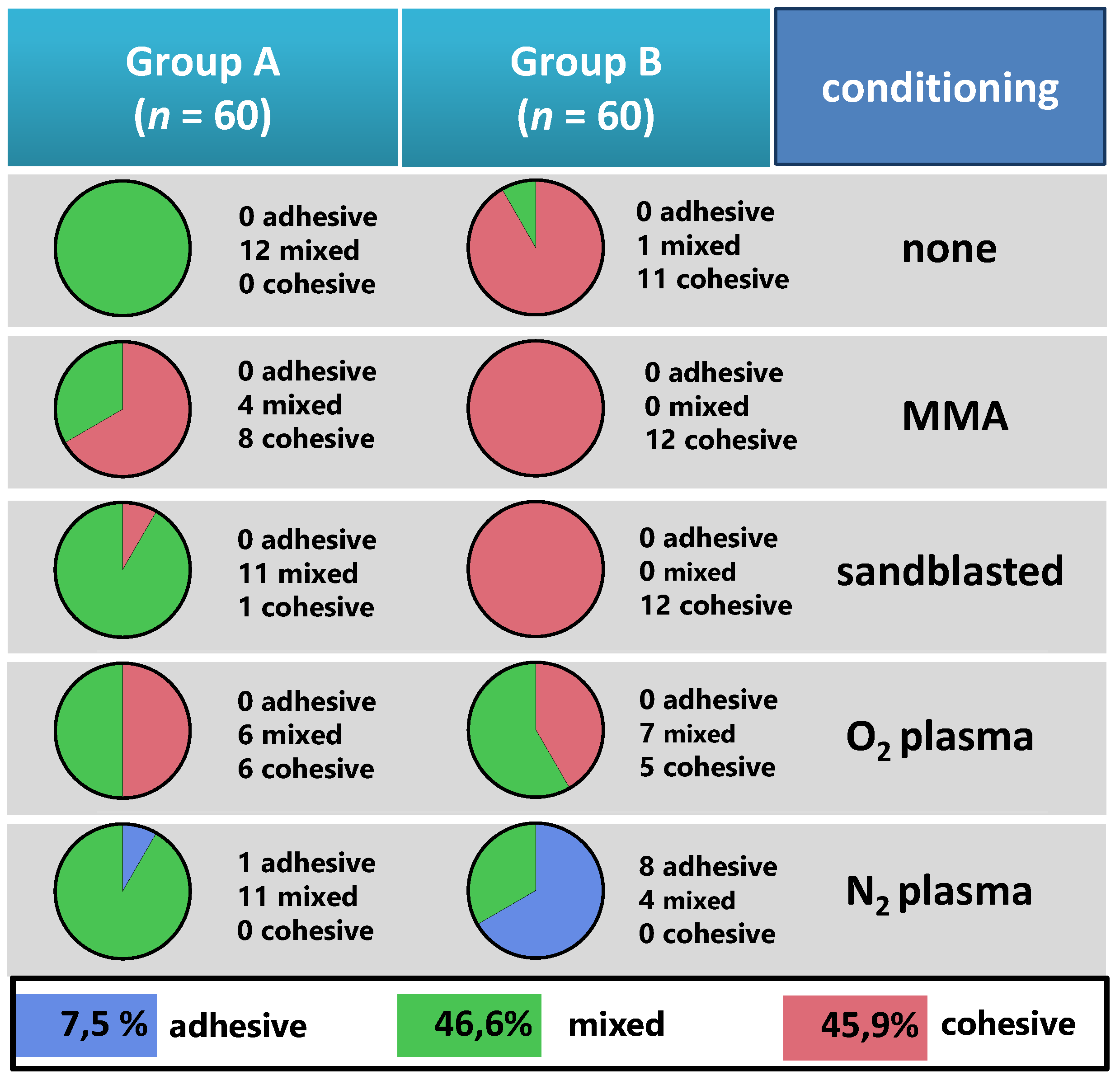
3.3. Modes of Fracture
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Brand Name | Company, City, Country | Composition Given by Manufacturer |
|---|---|---|
| Mondial 6 R483 | Kulzer, Hanau, Germany | NanoPearls®-Material, PMMA based |
| megaCRYL N (liquid & powder) | Megadental, Büdingen, Germany | Powder: PMMA-Copolymer, dibenzoylperoxide, phenylbenzylbarbiturateacid, butyl-barbiturateacid, titanium dioxide, ferric oxide, peri-dinaphthylen. Liquid: MMA: butandioldimethacrylate, copper naphtenic acid, dilauryldimethylammoniumchloride, hydrochinone |
| Pink Blank U | Anaxdent, Stuttgart, Germany | polymethyl methacrylate, pigments |
| Korox 250 | Bego, Bremen, Germany | 250 µm Al2O3 |
| Dublisil 30 | Dreve Dentamid, Unna, Germany | addition-vulcanizing polyvinylsiloxane |
References
- Schwendicke, F.; Nitschke, I.; Stark, H.; Micheelis, W.; Jordan, R.A. Epidemiological trends, predictive factors, and projection of tooth loss in Germany 1997–2030: Part II. Edentulism in seniors. Clin. Oral Investig. 2020, 24, 3997–4003. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.R.; Stark, H.; Nitschke, I.; Micheelis, W.; Schwendicke, F. Epidemiological trends, predictive factors, and projection of tooth loss in Germany 1997–2030: Part I. missing teeth in adults and seniors. Clin. Oral Investig. 2021, 25, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Bernabé, E.; Marcenes, W.; Hernandez, C.R.; Bailey, J.; Abreu, L.G.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z.; Arora, A.; et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar] [CrossRef]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-aided technology for fabricating complete dentures: Systematic review of historical background, current status, and future perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef]
- Millet, C.; Virard, F.; Dougnac-Galant, T.; Ducret, M. CAD-CAM immediate to definitive complete denture transition: A digital dental technique. J. Prosthet. Dent. 2020, 124, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Schweigera, J.; Stumbaumb, J.; Edelhoffc, D.; Güthd, J. Systematics and concepts for the digital production of complete dentures: Risks and opportunities. Int. J. Comput. Dent. 2018, 21, 41–56. [Google Scholar]
- Unkovskiy, A.; Wahl, E.; Zander, A.T.; Huettig, F.; Spintzyk, S. Intraoral scanning to fabricate complete dentures with functional borders: A proof-of-concept case report. BMC Oral Health 2019, 19, 1–7. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. CAD/CAM produces dentures with improved fit. Clin. Oral Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef]
- Infante, L.; Yilmaz, B.; McGlumphy, E.; Finger, I. Fabricating complete dentures with CAD/CAM technology. J. Prosthet. Dent. 2014, 111, 351–355. [Google Scholar] [CrossRef]
- Engler, M.L.P.D.; Güth, J.-F.; Keul, C.; Erdelt, K.; Edelhoff, D.; Liebermann, A. Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin. Oral Investig. 2019, 24, 277–284. [Google Scholar] [CrossRef]
- Jain, G.; Palekar, U.; Awinashe, V.; Mishra, S.K.; Kawadkar, A.; Rahangdale, T. The Effect of Different Chemical Surface Treatments of Denture Teeth on Shear Bond Strength: A Comparative Study. J. Clin. Diagn. Res. 2014, 8, ZC15-8. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Kanazawa, M.; Iwaki, M.; Jokanovic, A.; Minakuchi, S. Effects of offset values for artificial teeth positions in CAD/CAM complete denture. Comput. Biol. Med. 2014, 52, 1–7. [Google Scholar] [CrossRef]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef]
- Patil, S.B.; Naveen, B.H.; Patil, N.P. Bonding acrylic teeth to acrylic resin denture bases: A review. Gerodontology 2006, 23, 131–139. [Google Scholar] [CrossRef]
- Marra, J.; Paleari, A.G.; Pero, A.; de Souza, R.F.; Barbosa, D.B.; Compagnoni, M.A. Effect of methyl methacrylate monomer on bond strength of denture base resin to acrylic teeth. Int. J. Adhes. Adhes. 2009, 29, 391–395. [Google Scholar] [CrossRef]
- Spratley, M. An investigation of the adhesion of acrylic resin teeth to dentures. J. Prosthet. Dent. 1987, 58, 389–392. [Google Scholar] [CrossRef]
- Cunningham, J.; Benington, I. A survey of the pre-bonding preparation of denture teeth and the efficiency of dewaxing methods. J. Dent. 1997, 25, 125–128. [Google Scholar] [CrossRef]
- Barbosa, D.B.; Monteiro, D.R.; Barão, V.A.R.; Pero, A.C.; Compagnoni, M.A. Effect of monomer treatment and polymerisation methods on the bond strength of resin teeth to denture base material. Gerodontology 2009, 26, 225–231. [Google Scholar] [CrossRef]
- Kurt, M.; Saraç, Y.Ş.; Ural, Ç.; Saraç, D. Effect of pre-processing methods on bond strength between acrylic resin teeth and acrylic denture base resin. Gerodontology 2012, 29, e357–e362. [Google Scholar] [CrossRef]
- Akin, H.; Kirmali, O.; Tugut, F.; Coskun, M.E. Effects of Different Surface Treatments on the Bond Strength of Acrylic Denture Teeth to Polymethylmethacrylate Denture Base Material. Photomed. Laser Surg. 2014, 32, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.-H.; Chung, C.Y.; Chan, D.C.N. Effect of pre-processing surface treatments of acrylic teeth on bonding to the denture base. J. Oral Rehabil. 2008, 35, 268–275. [Google Scholar] [CrossRef]
- Nishigawa, G.; Maruo, Y.; Oka, M.; Okamoto, M.; Minagi, S.; Irie, M.; Suzuki, K. Effect of Plasma Treatment on Adhesion of Self-curing Repair Resin to Acrylic Denture Base. Dent. Mater. J. 2004, 23, 545–549. [Google Scholar] [CrossRef]
- Zhang, H.; Fang, J.; Hu, Z.; Ma, J.; Han, Y.; Bian, J. Effect of oxygen plasma treatment on the bonding of a soft liner to an acrylic resin denture material. Dent. Mater. J. 2010, 29, 398–402. [Google Scholar] [CrossRef][Green Version]
- Zuckerman, G.R. A reliable method for securing anterior denture teeth in denture bases. J. Prosthet. Dent. 2003, 89, 603–607. [Google Scholar] [CrossRef]
- Meng, G.K.; Chung, K.-H.; Fletcher-Stark, M.L.; Zhang, H. Effect of surface treatments and cyclic loading on the bond strength of acrylic resin denture teeth with autopolymerized repair acrylic resin. J. Prosthet. Dent. 2010, 103, 245–252. [Google Scholar] [CrossRef]
- Akin, H.; Tugut, F.; Guney, U.; Akar, T. Shear Bond Strength of Denture Teeth to Two Chemically Different Denture Base Resins after Various Surface Treatments. J. Prosthodont. 2013, 23, 152–156. [Google Scholar] [CrossRef]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef]
- De Abreu, C.W.; Filho, G.D.; Kojima, A.N.; Jóias, R.M.; Mesquita, A.M.M. Evaluation of crosshead speed influence on shear bond strength test. Braz. Dent. Sci. 2014, 17, 50. [Google Scholar] [CrossRef]
- Mahadevan, V.; Krishnan, M.; Krishnan, C.S.; Azhagarasan, N.; Sampathkumar, J.; Ramasubramanian, H. Influence of Surface Modifications of Acrylic Resin Teeth on Shear Bond Strength with Denture Base Resin-An Invitro Study. J. Clin. Diagn. Res. 2015, 9, ZC16–ZC21. [Google Scholar] [CrossRef] [PubMed]
- Aljudy, H.J. Effect of Plasma Treatment of Acrylic Denture Teeth and Thermocycling on the Bonding Strength to Heat Cured Acrylic Denture Base Material. J. Baghdad Coll. Dent. 2013, 25, 6–11. [Google Scholar] [CrossRef]



| Subgroup | Group A (Resin Tooth) Ra | Group B (PMMA Base) Ra | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| none | 2.17 | 0.05 | 1.46 | 0.17 |
| MMA | 2.09 | 0.08 | 1.55 | 0.18 |
| sandblasted | 2.31 | 0.3 | 1.96 | 0.3 |
| oxygen plasma | 2.1 | 0.08 | 1.6 | 0.17 |
| nitrogen plasma | 2.13 | 0.06 | 2.01 | 0.17 |
| Subgroup Surface Treatment | Group A | Group B | ||||
|---|---|---|---|---|---|---|
| SBS (MPa) | ||||||
| Mean | SD | Sign. | Mean | SD | Sign. * | |
| none | 11.59 | 3.49 | AD | 15.04 | 2.05 | A |
| MMA | 16.62 | 1.52 | B | 14.46 | 1.59 | A |
| sandblasted | 13.33 | 1.99 | CD | 14.44 | 1.07 | A |
| oxygen plasma | 15.53 | 3.04 | BC | 12.14 | 3.92 | A |
| nitrogen plasma | 9.12 | 1.69 | A | 4.93 | 3.28 | B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klaiber, D.; Spintzyk, S.; Geis-Gerstorfer, J.; Klink, A.; Unkovskiy, A.; Huettig, F. Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow. Materials 2021, 14, 3822. https://doi.org/10.3390/ma14143822
Klaiber D, Spintzyk S, Geis-Gerstorfer J, Klink A, Unkovskiy A, Huettig F. Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow. Materials. 2021; 14(14):3822. https://doi.org/10.3390/ma14143822
Chicago/Turabian StyleKlaiber, Dominik, Sebastian Spintzyk, Juergen Geis-Gerstorfer, Andrea Klink, Alexey Unkovskiy, and Fabian Huettig. 2021. "Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow" Materials 14, no. 14: 3822. https://doi.org/10.3390/ma14143822
APA StyleKlaiber, D., Spintzyk, S., Geis-Gerstorfer, J., Klink, A., Unkovskiy, A., & Huettig, F. (2021). Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow. Materials, 14(14), 3822. https://doi.org/10.3390/ma14143822








