Retention Forces of Monolithic CAD/CAM Crowns Adhesively Cemented to Titanium Base Abutments—Effect of Saliva Contamination Followed by Cleaning of the Titanium Bond Surface
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setup
2.2. Contamination
2.3. Fabrication of Specimens
2.4. Thermo-Mechanical Aging
2.5. Bond Failure Analysis
2.6. Pull-off Test
2.7. Scanning Electron Microscope Surface Analysis
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- contamination followed by cleaning can have a negative influence on the bonding properties to titanium and specific cleaning protocols performed better than others;
- regarding retention force, every protocol allowed the restoration of the bonding forces except for the protocol using alcohol.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patel, N. Integrating Three-Dimensional Digital Technologies for Comprehensive Implant Dentistry. J. Am. Dent. Assoc. 2010, 141, 20S–24S. [Google Scholar] [CrossRef]
- Finelle, G.; Sanz-Martín, I.; Knafo, B.; Figué, M.; Popelut, A. Digitalized CAD/CAM protocol for the fabrication of customized sealing socket healing abutments in immediate implants in molar sites. Int J Comput Dent. 2019, 22, 187–204. [Google Scholar]
- Pitta, J.; Hjerppe, J.; Burkhardt, F.; Fehmer, V.; Mojon, P.; Sailer, I. Mechanical stability and technical outcomes of monolithic CAD/CAM fabricated abutment-crowns supported by titanium bases: An in vitro study. Clin. Oral Implant. Res. 2021, 32, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Motel, C.; Kirchner, E.; Adler, W.; Wichmann, M.; Matta, R.E. Impact of Different Scan Bodies and Scan Strategies on the Accuracy of Digital Implant Impressions Assessed with an Intraoral Scanner: An In Vitro Study. J. Prosthodont. 2019, 29, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Kurbad, A. Final restoration of implants with a hybrid ceramic superstructure Die definitive Versorgung von Implantaten mit Suprakonstruktionen aus Hybridkeramik. Int. J. Comput. Dent. 2016, 19, 257–279. [Google Scholar]
- Kern, M.; Wegner, S.M. Bonding to zirconia ceramic: Adhesion methods and their durability. Dent. Mater. 1998, 14, 64–71. [Google Scholar] [CrossRef]
- Ebert, A.; Hedderich, J.; Kern, M. Retention of zirconia ceramic copings bonded to titanium abutments. Int. J. Oral Maxillofac. Implant. 2008, 22, 921–927. [Google Scholar]
- von Maltzahn, N.F.; Holstermann, J.; Kohorst, P. Retention Forces between Titanium and Zirconia Components of Two-Part Implant Abutments with Different Techniques of Surface Modification. Clin. Implant Dent. Relat. Res. 2016, 18, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Pitta, J.; Burkhardt, F.; Mekki, M.; Fehmer, V.; Mojon, P.; Sailer, I. Effect of airborne-particle abrasion of a titanium base abutment on the stability of the bonded interface and retention forces of crowns after artificial aging. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, F.; Sailer, I.; Fehmer, V.; Mojon, P.; Pitta, J. Retention and marginal integrity of CAD/CAM fabricated crowns adhesively cemented to titanium base abutments—Influence of bonding system and restorative material. Int. J. Prosthodont. 2021, 88, 7576. [Google Scholar]
- Matinlinna, J.P.; Lassila, L.V.; Özcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 155–164. [Google Scholar] [PubMed]
- Lung, C.Y.K.; Matinlinna, J.P. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent. Mater. 2012, 28, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J. Adhes. Dent. 2015, 17, 7–26. [Google Scholar] [PubMed]
- Humphrey, S.P.; Williamson, R.T. A review of saliva: Normal composition, flow, and function. J. Prosthet. Dent. 2001, 85, 162–169. [Google Scholar] [CrossRef]
- Ishii, R.; Tsujimoto, A.; Takamizawa, T.; Tsubota, K.; Suzuki, T.; Shimamura, Y.; Miyazaki, M. Influence of surface treatment of contaminated zirconia on surface free energy and resin cement bonding. Dent. Mater. J. 2015, 34, 91–97. [Google Scholar] [CrossRef]
- El-Kalla, I.H.; García-Godoy, F. Saliva contamination and bond strength of single-bottle adhesives to enamel and dentin. Am. J. Dent. 1997, 10, 83–87. [Google Scholar]
- Fritz, U.B.; Finger, W.J.; Stean, H. Salivary contamination during bonding procedures with a one-bottle adhesive system. Quintessence Int. 1998, 29, 567–572. [Google Scholar]
- Raigrodski, A.J. Contemporary materials and technologies for all-ceramic fixed partial dentures: A review of the literature. J. Prosthet. Dent. 2004, 92, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Pitta, J.; Branco, T.C.; Portugal, J. Effect of saliva contamination and artificial aging on different primer/cement systems bonded to zirconia. J. Prosthet. Dent. 2018, 119, 833–839. [Google Scholar] [CrossRef]
- Quaas, A.; Yang, B.; Kern, M. Panavia F 2.0 bonding to contaminated zirconia ceramic after different cleaning procedures. Dent. Mater. 2007, 23, 506–512. [Google Scholar] [CrossRef]
- Angkasith, P.; Burgess, J.O.; Bottino, M.C.; Lawson, N.C. Cleaning Methods for Zirconia Following Salivary Contamination. J. Prosthodont. 2016, 25, 375–379. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Savabi, O.; Savabi, G.; Razavi, M. Effect of cleaning methods on retentive values of saliva-contaminated im-plant-supported zirconia copings. Clin. Oral Implants Res. 2018, 29, 530–536. [Google Scholar] [CrossRef]
- Thompson, J.Y.; Stoner, B.R.; Piascik, J.R.; Smith, R. Adhesion/cementation to zirconia and other non-silicate ceramics: Where are we now? Dent. Mater. 2011, 27, 71–82. [Google Scholar] [CrossRef]
- Phark, J.H.; Duarte, S., Jr.; Kahn, H.; Blatz, M.B.; Sadan, A. Influence of contamination and cleaning on bond strength to modified zirconia. Dent. Mater. 2009, 25, 1541–1550. [Google Scholar] [CrossRef]
- Taira, Y.; Matsumura, H.; Yoshida, K.; Tanaka, T.; Atsuta, M. Adhesive bonding of titanium with a methacrylate?phosphate primer and self-curing adhesive resins. J. Oral Rehabil. 1995, 22, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Taira, Y.; Yanagida, H.; Matsumura, H.; Yoshida, K.; Atsuta, M.; Suzuki, S. Adhesive bonding of titanium with a thione-phosphate dual functional primer and self-curing luting agents. Eur. J. Oral Sci. 2000, 108, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Nijhuis, H.; Valandro, L.F. Effect of Various Surface Conditioning Methods on the Adhesion of Dual-cure Resin Cement with MDP Functional Monomer to Zirconia after Thermal Aging. Dent. Mater. J. 2008, 27, 99–104. [Google Scholar] [CrossRef]
- Yang, B.; Lange-Jansen, H.; Scharnberg, M.; Wolfart, S.; Ludwig, K.; Adelung, R.; Kern, M. Influence of saliva contamination on zirconia ceramic bonding. Dent. Mater. 2008, 24, 508–513. [Google Scholar] [CrossRef]
- Klosa, K.; Wolfart, S.; Lehmann, F.; Wenz, H.-J.; Kern, M. The effect of storage conditions, contamination modes and cleaning procedures on the resin bond strength to lithium disilicate ceramic. J. Adhes. Dent. 2009, 11, 127–135. [Google Scholar] [PubMed]
- Doungsri, J.; Arksornnukit, M. (Eds) Effect of Cleaning Solutions on Shear Bond Strength of Resin Cement to Saliva Contaminated Lithium Disilicate Ceramic. In Proceedings of the International Graduate Research Conference, Chiang Mai, Thailand, 20 December 2013. [Google Scholar]
- Mehl, C.; Harder, S.; Shahriari, A.; Steiner, M.; Kern, M. Influence of abutment height and thermocycling on retrievability of cemented implant-supported crowns. Int. J. Oral Maxillofac. Implant. 2012, 27, 1106–1115. [Google Scholar]
- Pitta, J.; Bijelic-Donova, J.; Burkhardt, F.; Fehmer, V.; Närhi, T.; Sailer, I. Temporary Implant-Supported Single Crowns Using Tita-nium Base Abutments: An In Vitro Study on Bonding Stability and Pull-out Forces. Int. J. Prosthodont. 2020, 33, 546–552. [Google Scholar] [CrossRef]
- Kern, M.; Strub, J.R.; Lü, X.-Y. Wear of composite resin veneering materials in a dual-axis chewing simulator. J. Oral Rehabil. 1999, 26, 372–378. [Google Scholar] [CrossRef]
- Attia, A.; Kern, M. Effect of cleaning methods after reduced-pressure air abrasion on bonding to zirconia ceramic. J. Adhes. Dent. 2011, 13. [Google Scholar] [CrossRef]
- de Melo Costa, D.; de Oliveira Lopes, L.K.; Hu, H.; Tipple, A.F.; Vickery, K. Alcohol fixation of bacteria to surgical instruments increases cleaning difficulty and may contribute to sterilization inefficacy. Am. J. Infect. Control. 2017, 45, e81–e86. [Google Scholar] [CrossRef]
- Kim, D.-H.; Son, J.-S.; Jeong, S.-H.; Kim, Y.-K.; Kim, K.-H.; Kwon, T.-Y. Efficacy of various cleaning solutions on saliva-contaminated zirconia for improved resin bonding. J. Adv. Prosthodont. 2015, 7, 85–92. [Google Scholar] [CrossRef]
- Aboush, Y.E. Removing saliva contamination from porcelain veneers before bonding. J. Prosthet. Dent. 1998, 80, 649–653. [Google Scholar] [CrossRef]
- Aladağ, A.; Elter, B.; Çömlekoğlu, E.; Kanat, B.; Sonugelen, M.; Kesercioğlu, A.; Özcan, M. Effect of Different Cleaning Regimens on the Adhesion of Resin to Saliva-Contaminated Ceramics. J. Prosthodont. 2014, 24, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E. High-resolution scanning electron microscopy of immunogold-labelled cells by the use of thin plasma coating of osmium. J. Microsc. 2002, 208, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Covani, U.; Marconcini, S.; Crespi, R.; Barone, A. Bacterial Plaque Colonization around Dental Implant Surfaces. Implant. Dent. 2006, 15, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Gibson, H.; Taylor, J.H.; Hall, K.E.; Holah, J.T. Effectiveness of cleaning techniques used in the food industry in terms of the removal of bacterial biofilms. J. Appl. Microbiol. 1999, 87, 41–48. [Google Scholar] [CrossRef]
- Güers, P.; Wille, S.; Strunskus, T.; Polonskyi, O.; Kern, M. Durability of resin bonding to zirconia ceramic after contamination and the use of various cleaning methods. Dent. Mater. 2019, 35, 1388–1396. [Google Scholar] [CrossRef] [PubMed]

| Groups | Pre-Treatment | Contamination | Cleaning Protocol | |
|---|---|---|---|---|
| Water | H2O | 50 µm aluminum oxide by 2.0 bar of air pressure for 10 s/ ultrasonic alcohol bath for 5 min/dried with oil-free air | inserted in human saliva (5 min) | water-spray (1 min) |
| Alcohol | ALC | ultrasonic alcohol bath (5 min) | ||
| Suspension of zirconium particles | SZP | alkaline suspension of zirconium oxide particles (20 s) | ||
| Airborne-particle abrasion | APA | reapplied standardized airborne-particle abrasion | ||
| Control | CTR | Not applied | ||
| Group | Bonding Failure | Retention Force | Click at Debonding | ||||
|---|---|---|---|---|---|---|---|
| No Failure | Micro- Movement | Macro- Movement | Loss of Retention | Mean (± SD) | Median (IQR) | ||
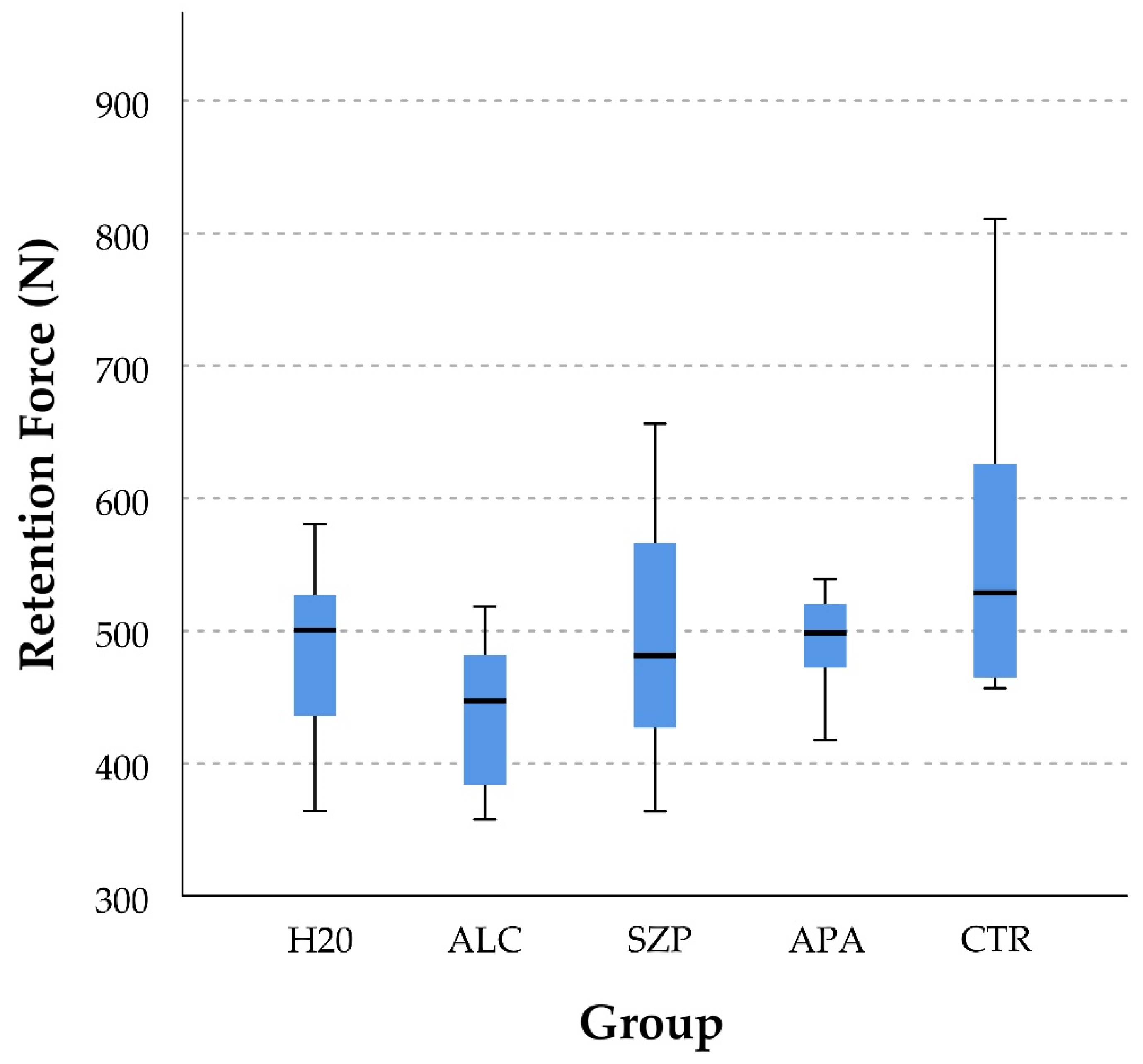
| H2O | 0 | 12 | 0 | 0 | 487 N (± 18.1) | 501 N (101) ab | 0.08 (8%) |
| ALC | 0 | 12 | 0 | 0 | 439 N (± 16.1) | 447 N (107) b | 0.00 (0%) |
| SZP | 6 | 6 | 0 | 0 | 501 N (± 26.4) | 481 N (157) ab | 0.67 (67%) |
| APA | 1 | 11 | 0 | 0 | 493 N (± 10.2) | 498 N (59) ab | 0.00 (0%) |
| CTR | 9 | 3 | 0 | 0 | 562 N (± 33.1) | 529 N (187) a | 0.67 (67%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burkhardt, F.; Pitta, J.; Fehmer, V.; Mojon, P.; Sailer, I. Retention Forces of Monolithic CAD/CAM Crowns Adhesively Cemented to Titanium Base Abutments—Effect of Saliva Contamination Followed by Cleaning of the Titanium Bond Surface. Materials 2021, 14, 3375. https://doi.org/10.3390/ma14123375
Burkhardt F, Pitta J, Fehmer V, Mojon P, Sailer I. Retention Forces of Monolithic CAD/CAM Crowns Adhesively Cemented to Titanium Base Abutments—Effect of Saliva Contamination Followed by Cleaning of the Titanium Bond Surface. Materials. 2021; 14(12):3375. https://doi.org/10.3390/ma14123375
Chicago/Turabian StyleBurkhardt, Felix, João Pitta, Vincent Fehmer, Philippe Mojon, and Irena Sailer. 2021. "Retention Forces of Monolithic CAD/CAM Crowns Adhesively Cemented to Titanium Base Abutments—Effect of Saliva Contamination Followed by Cleaning of the Titanium Bond Surface" Materials 14, no. 12: 3375. https://doi.org/10.3390/ma14123375
APA StyleBurkhardt, F., Pitta, J., Fehmer, V., Mojon, P., & Sailer, I. (2021). Retention Forces of Monolithic CAD/CAM Crowns Adhesively Cemented to Titanium Base Abutments—Effect of Saliva Contamination Followed by Cleaning of the Titanium Bond Surface. Materials, 14(12), 3375. https://doi.org/10.3390/ma14123375






