Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method
Abstract
1. Introduction
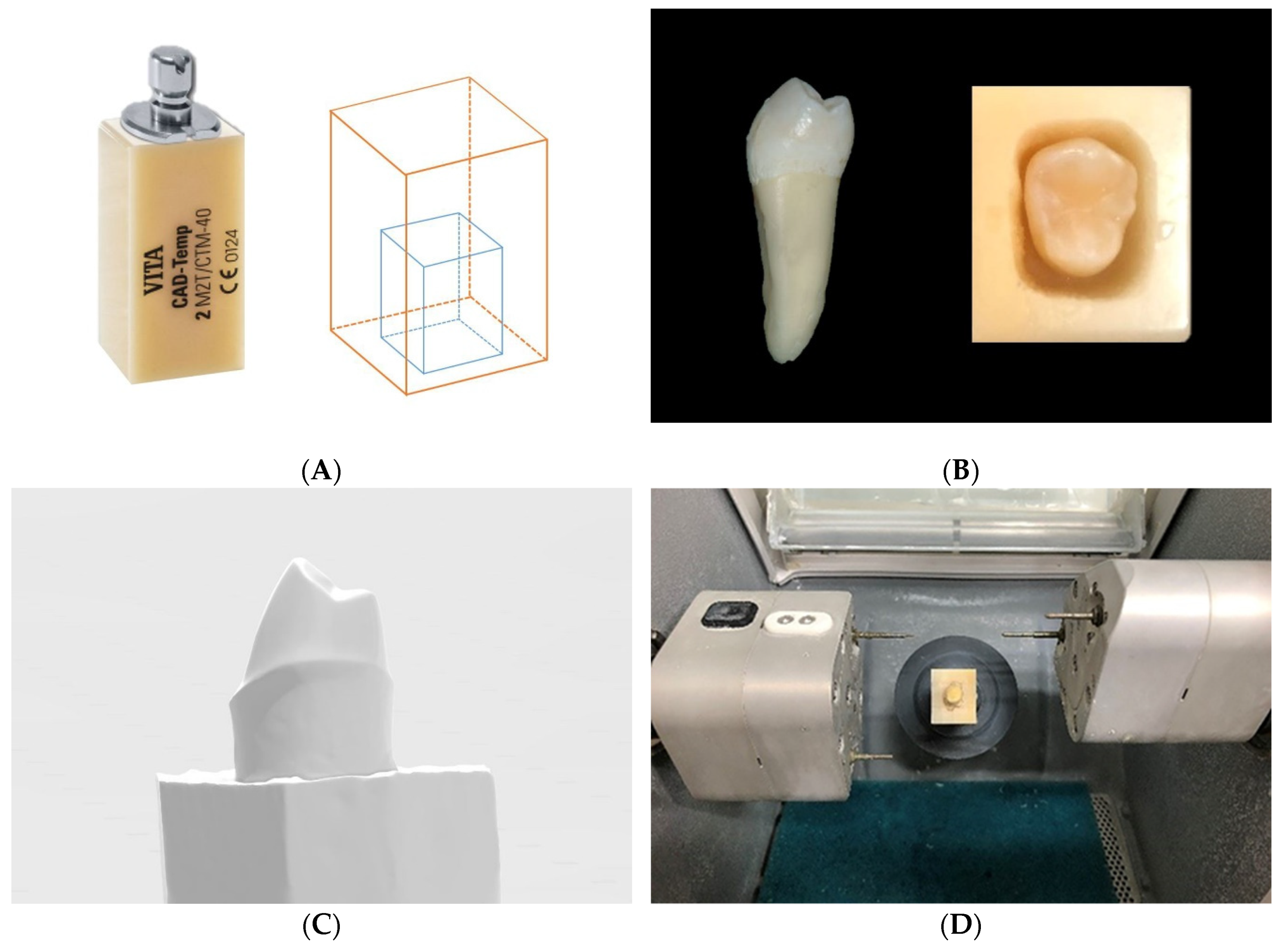
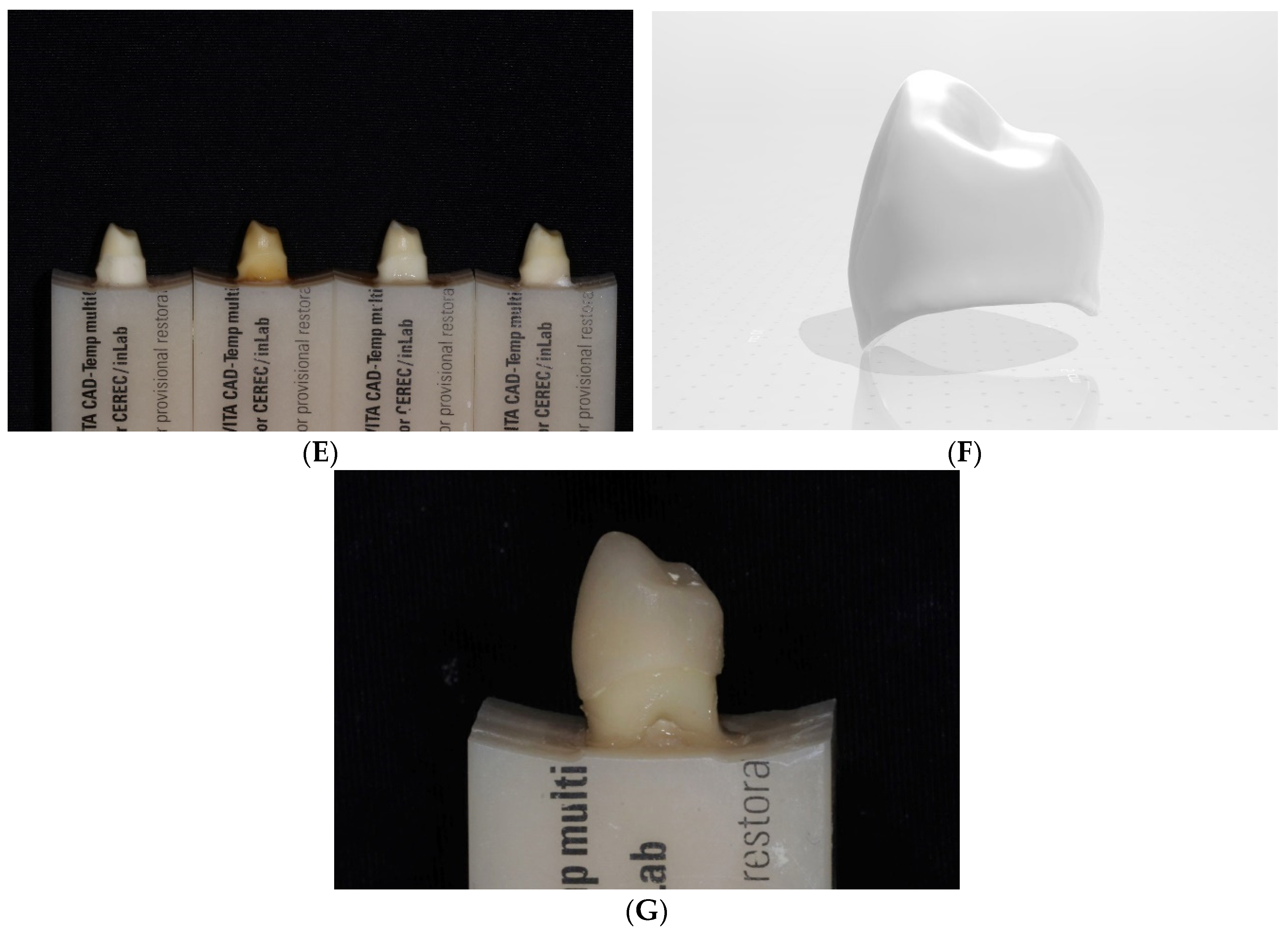
2. Material and Methods
3. Statistical Analysis
4. Results
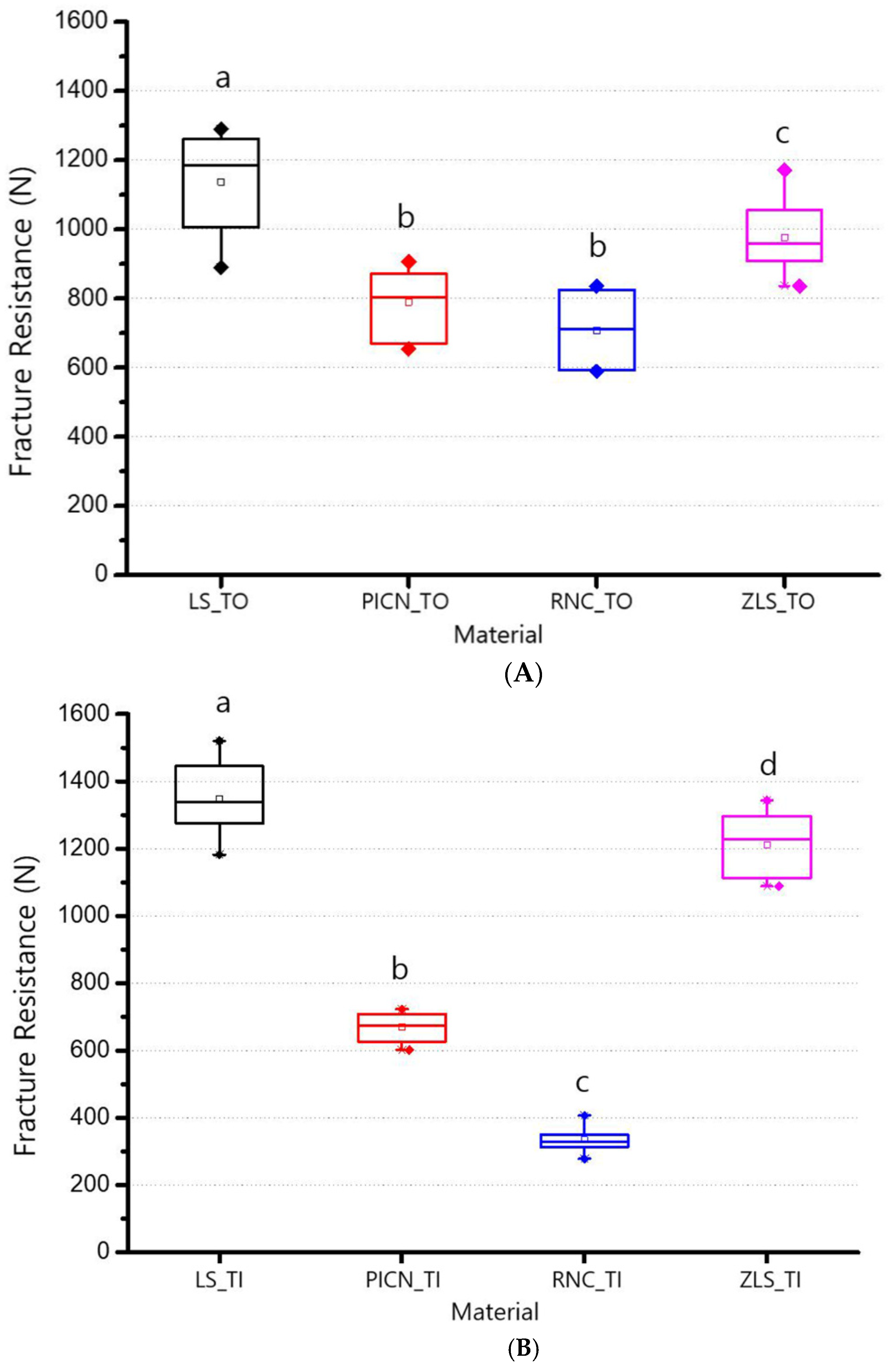
4.1. Analyses of Fracture Resistance
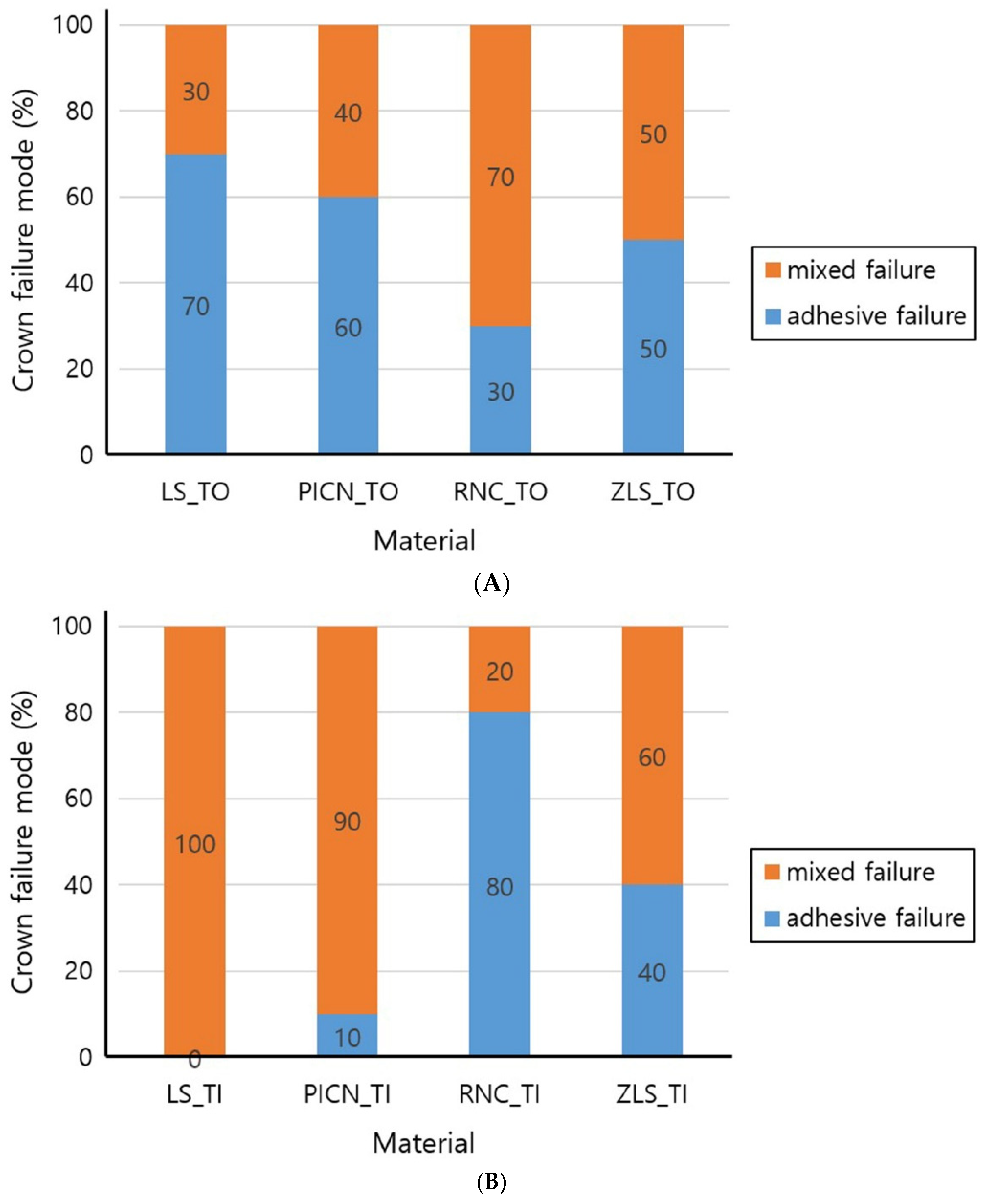
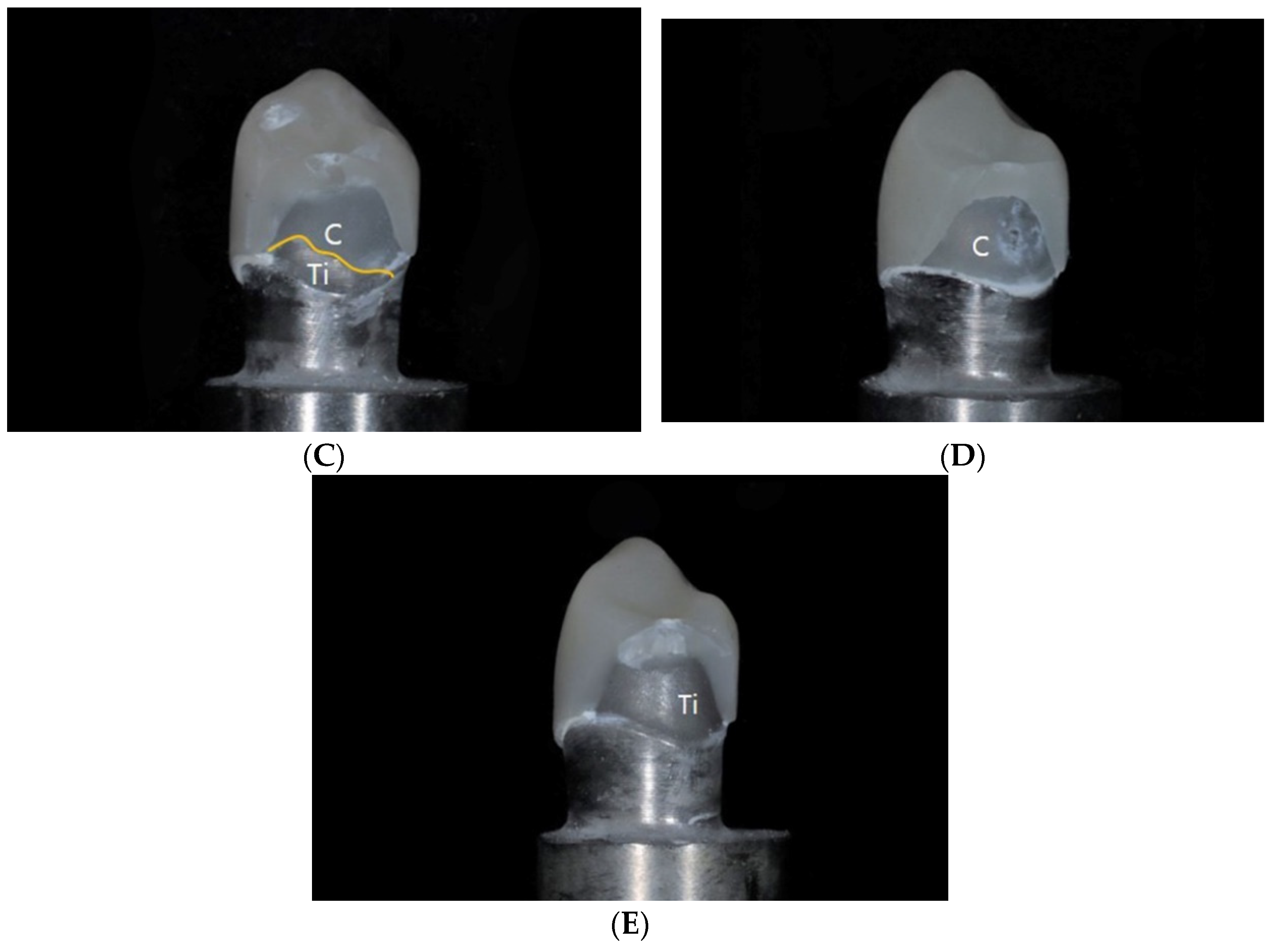
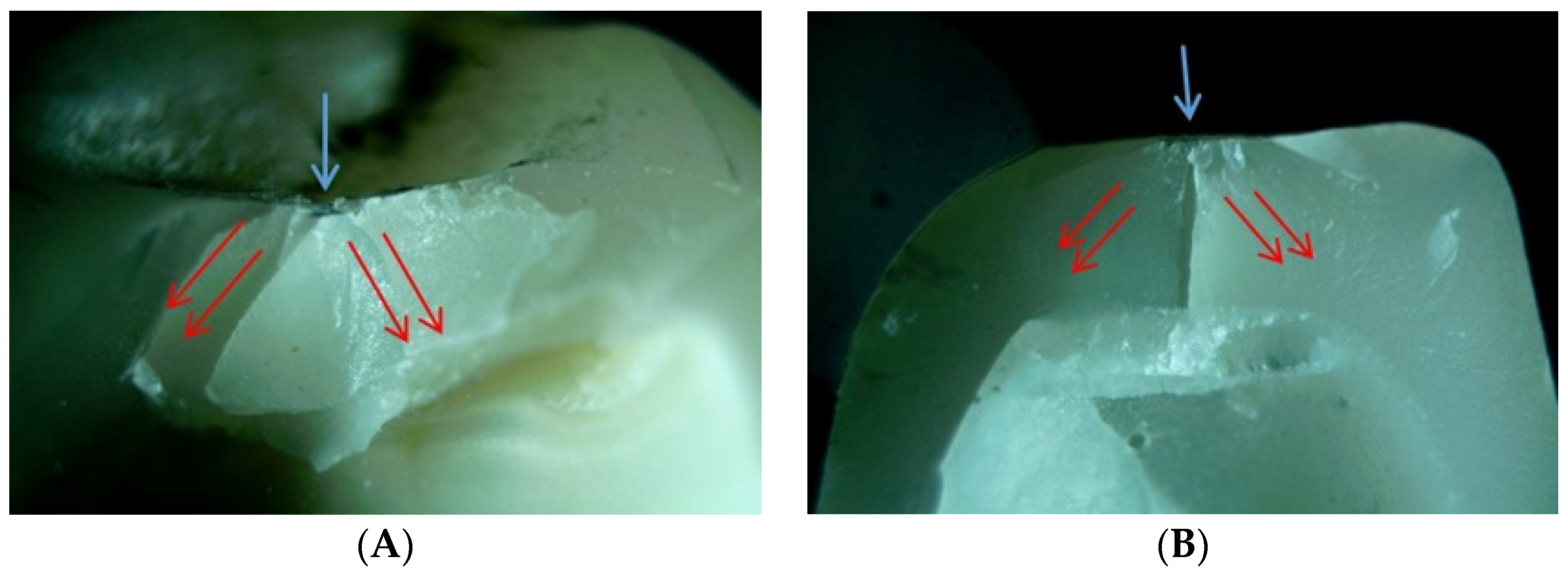
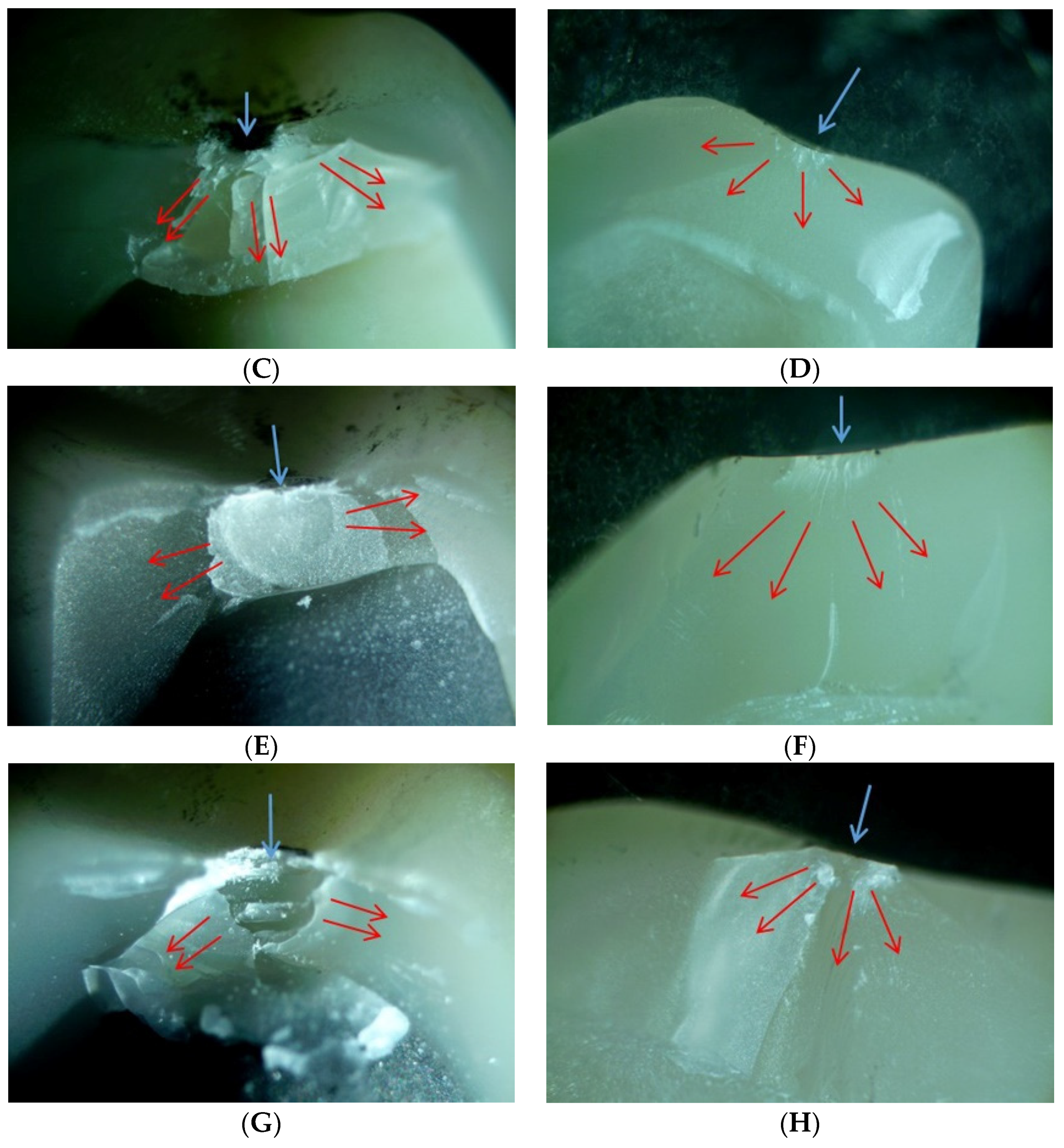
4.2. Fracture Failure Mode
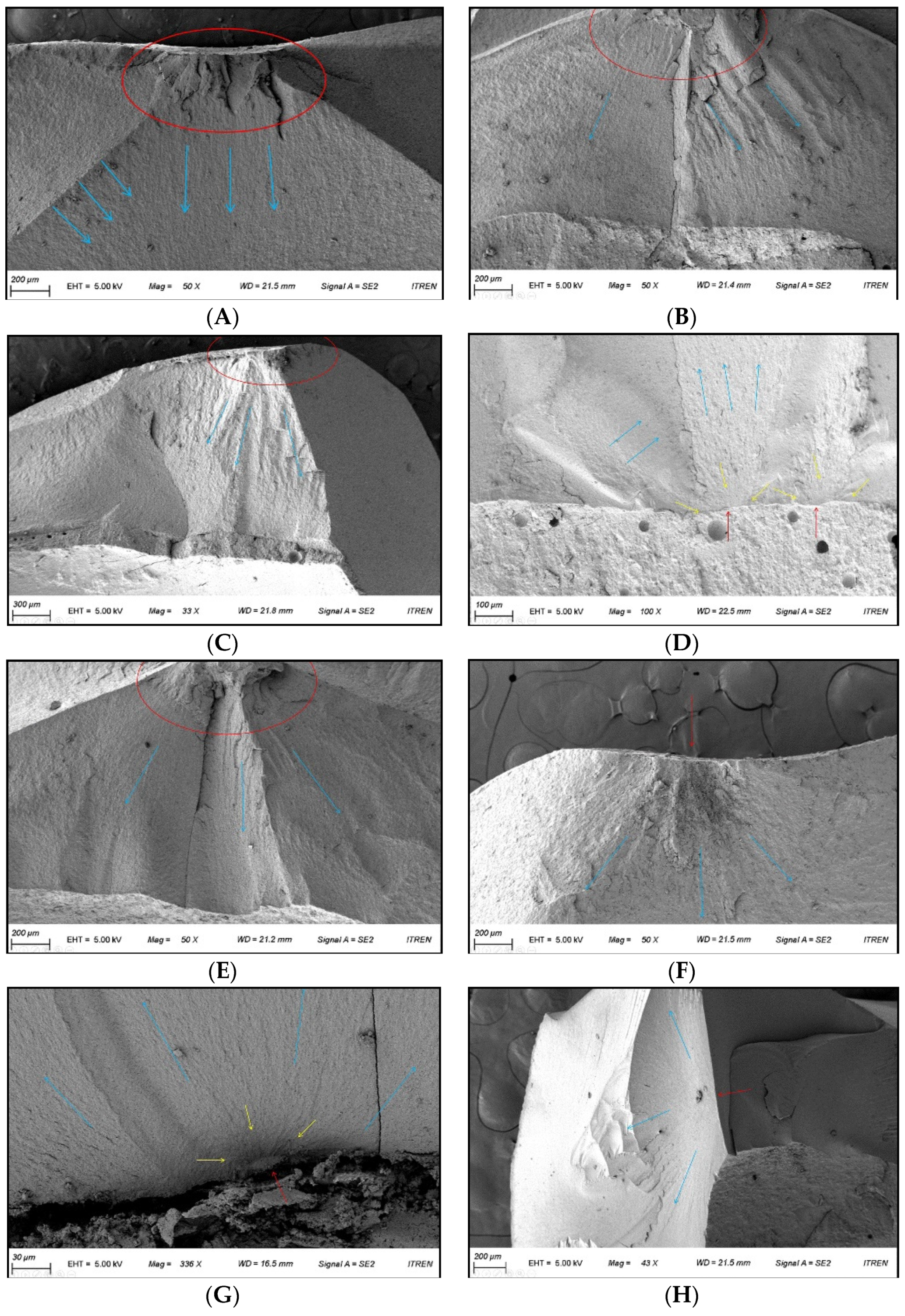
4.3. Fractography Analysis
5. Discussion
6. Conclusions
- For the fracture resistances of the restorations, there are statistically significant correlations between the types of chairside CAD/CAM materials and the types of abutments.
- Lithium disilicate and zirconia-reinforced lithium silicate restorations exhibited statistically significant high fracture resistances, indicating their suitability as restorative materials for natural teeth or implant abutments.
- The chairside CAD/CAM restorations showed different fracture failure modes based on the types of materials and abutments.
- The fracture of the chairside CAD/CAM restorations initiated at the groove where the ball indenter toughed and propagated toward the axial wall. There were no distinct differences based on the types of materials and abutments.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef]
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef]
- Sriram, S.; Shankari, V.; Chacko, Y. Computer aided designing/computer aided manufacturing in dentistry (CAD/CAM)–A Review. Int. J. Curr. Res. 2018, 10, 20–24. [Google Scholar]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Estevan, L.; Millan-Martínez, D.; Fons-Font, A.; Agustín-Panadero, R.; Román-Rodríguez, J.L. Methodology in specimen fabrication for in vitro dental studies: Standardization of extracted tooth preparation. J. Clin. Exp. Dent. 2017, 9, e897–e900. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in dentistry. Dent. Clin. 2011, 55, 559–570. [Google Scholar] [CrossRef]
- Miyazaki, T.; Hotta, Y.; Kunii, J.; Kuriyama, S.; Tamaki, Y. A review of dental CAD/CAM: Current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009, 28, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Çehreli, M.C.; Kökat, A.M.; Akça, K. CAD/CAM Zirconia vs. slip-cast glass-infiltrated Alumina/Zirconia all-ceramic crowns: 2-year results of a randomized controlled clinical trial. J. Appl. Oral Sci. 2009, 17, 49–55. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, Y.S. Microtensile bond strength and micromorphologic analysis of surface-treated resin nanoceramics. J. Adv. Prosthodont. 2016, 8, 275–284. [Google Scholar] [CrossRef]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V.J. Does artificial aging affect mechanical properties of CAD/CAM composite materials. J. Prosthodont. Res. 2017, 62, 65–74. [Google Scholar] [CrossRef]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [Google Scholar] [CrossRef] [PubMed]
- Belli, R.; Wendler, M.; de Ligny, D.; Cicconi, M.R.; Petschelt, A.; Peterlik, H.; Lohbauer, U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017, 33, 84–98. [Google Scholar] [CrossRef]
- Wendler, M.; BellI, R.; Petschelt, A.; Mevec, D.; Harrer, W.; Lube, T.; Danzer, R.; Lohbauer, U. Chairside CAD/CAM materials. Part 2: Flexural strength testing. Dent. Mater. 2017, 33, 99–109. [Google Scholar] [CrossRef]
- Øilo, M.; Hardang, A.D.; Ulsund, A.H.; Gjerdet, N.R. Fractographic features of glass-ceramic and zirconia-based dental restorations fractured during clinical function. Eur. J. Oral Sci. 2014, 122, 238–244. [Google Scholar] [CrossRef]
- Kasem, A.T.; Sakrana, A.A.; Ellayeh, M.; Özcan, M. Evaluation of zirconia and zirconia-reinforced glassceramic systems fabricated for minimal invasive preparations using a novel standardization method. J. Esthet. Restor. Dent. 2020, 32, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Preis, V.; Hahnel, S.; Behr, M.; Bein, L.; Rosentritt, M. In-vitro fatigue and fracture testing of CAD/CAM-materials in implant-supported molar crowns. Dent. Mater. 2017, 33, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Dogan, D.O.; Gorler, O.; Mutaf, B.; Ozcan, M.; Eyuboglu, G.B.; Ulgey, M. Fracture resistance of molar crowns fabricated with monolithic all-ceramic CAD/CAM materials cemented on titanium abutments: An in vitro study. J. Prosthet. Dent. 2017, 26, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Atsü, S.S.; Aksan, M.E.; Bulut, A.C. Fracture Resistance of Titanium, Zirconia, and Ceramic-Reinforced Polyetheretherketone Implant Abutments Supporting CAD/CAM Monolithic Lithium Disilicate Ceramic Crowns After Aging. Int. J. Oral Maxillofac. Implants 2019, 34, 622–630. [Google Scholar] [CrossRef]
- Mahmood, D.J.; Linderoth, E.H.; Vult Von Steyern, P. The influence of support properties and complexity on fracture strength and fracture mode of all-ceramic fixed dental prostheses. Acta Odontol. Scand. 2011, 69, 229–237. [Google Scholar] [CrossRef]
- Almehmadi, N.; Kutkut, A.; Al-Sabbagh, M. What is the Best Available Luting Agent for Implant Prosthesis? Dent. Clin. N. Am. 2019, 63, 531–545. [Google Scholar] [CrossRef]
- Garg, P.; Gupta, G.; Prithviraj, D.R.; Pujari, M. Retentiveness of various luting agents used with implant-supported prostheses: A preliminary in vitro study. Int. J. Prosthodont. 2013, 26, 82–84. [Google Scholar] [CrossRef]
- Radcliffe, C.E.; Potouridou, L.; Qureshi, R.; Habahbeh, N.; Qualtrough, A.; Worthington, H.; Druker, D.B. Antimicrobial activity of varying concentrations of sodium hypochlorite on the endodontic microorganisms Actinomyces israelii, A. naeslundii, Candida albicans and Enterococcus faecalis. Int. Endod. J. 2004, 37, 438–446. [Google Scholar] [CrossRef]
- Yi, Y.; Heo, S.J.; Koak, J.Y.; Kim, S.K. Comparison of CAD/CAM abutment and prefabricated abutment in Morse taper internal type implant after cyclic loading: Axial displacement, removal torque, and tensile removal force. J. Adv. Prosthodont. 2019, 11, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.R.; Ansari, A.S.; Bajunaid, S.O.; Alshahrani, A.; Javed, M.Q. Evaluation of Film Thickness of Crown Disclosing Agents and Their Comparison with Cement Film Thickness after Final Cementation. Eur. J. Dent. 2020, 14, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Andrade, J.P.; Stona, D.; Bittencourt, H.R.; Borges, G.A.; Burnett, L.H.; Spohr, A.M. Effect of different computer-aided design/computer-aided manufacturing (CAD/CAM) materials and thicknesses on the fracture resistance of occlusal veneers. Oper. Dent. 2018, 43, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Al-Akhali, M.; Chaar, M.S.; Elsayed, A.; Samran, A.; Kern, M. Fracture resistance of ceramic and polymer-based occlusal veneer restorations. J. Mech. Behav. Biomed. Mater. 2017, 74, 245–250. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Lohbauer, U.; Della Bona, A.; Vichi, A.; Tholey, M.J.; Kelly, J.R.; van Noort, R.; Cesar, P.F. ADM guidance—ceramics: Guidance to the use of fractography in failure analysis of brittle materials. Dent. Mater. 2017, 33, 599–620. [Google Scholar] [CrossRef]
- Quinn, G.D. Fractography of Ceramics and Glasses, 2nd ed.; National Institute of Standards and Technology: Washington, DC, USA, 2016; pp. 165–208.
- Quinn, J.B.; Quinn, G.D. Material properties and fractography of an indirect dental resin composite. Dent. Mater. 2010, 26, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Scherrer, S.S.; Quinn, G.D.; Quinn, J.B. Fractographic failure analysis of a Procera AllCeram crown using stereo and scanning electron microscopy. Dent. Mater. 2008, 24, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Hamza, T.A.; Sherif, R.M. Fracture resistance of monolithic glass-ceramics versus bilayered zirconia-based restorations. J. Prosthet. Dent. 2019, 28, e259–e264. [Google Scholar] [CrossRef]
- Jalalian, E.; Atashkar, B.; Rostami, R. The effect of preparation design on the fracture resistance of zirconia crown copings (computer associated design/computer associated machine, CAD/CAM System). J. Dent. 2011, 8, 123–129. [Google Scholar]
- Alammari, M.; Abdelnabi, M.; Swelem, A. Effect of total occlusal convergence on fit and fracture resistance of zirconia-reinforced lithium silicate crowns. Clin. Cosmet. Investig. Dent. 2019, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Román-Rodríguez, J.L.; Millan-Martínez, D.; Fons-Font, A.; Agustín-Panadero, R.; Fernández-Estevan, L. Traction test of temporary dental cements. J. Clin. Exp. Dent. 2017, 9, e564–e568. [Google Scholar] [CrossRef][Green Version]
- Schlenz, M.A.; Schmidt, A.; Rehmann, P.; Niem, T.; Wöstmann, B. Microleakage of composite crowns luted on CAD/CAM-milled human molars: A new method for standardized in vitro tests. Clin. Oral Investig. 2019, 23, 511–517. [Google Scholar] [CrossRef]
- Duan, Y.; Griggs, J.A. Effect of elasticity on stress distribution in CAD/CAM dental crowns: Glass ceramic vs. polymer–matrix composite. J. Dent. 2015, 43, 742–749. [Google Scholar] [CrossRef]
- Kelly, J.R.; Rungruanganunt, P.; Hunter, B.; Vailati, F. Development of a clinically validated bulk failure test for ceramic crowns. J. Prosthet. Dent. 2010, 104, 228–238. [Google Scholar] [CrossRef]
- Malament, K.A.; Socransky, S.S. Survival of Dicor glass-ceramic dental restorations over 16 years. Part III: Effect of luting agent and tooth or tooth-substitute core structure. J. Prosthet. Dent. 2001, 86, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Hahnel, S.; Engelhardt, F.; Behr, M.; Preis, V. In vitro performance and fracture resistance of CAD/CAM-fabricated implant supported molar crowns. Clin. Oral Investig. 2017, 21, 1213–1219. [Google Scholar] [CrossRef]
- Bencun, M.; Ender, A.; Wiedemeier, D.B.; Mehl, A. Fracture load of CAD/CAM feldspathic crowns influenced by abutment material. Materials 2020, 13, 3407. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, P.; Singh, S.B.; Chakraborty, M. Elastic modulus of biomedical titanium alloys by nano-indentation and ultrasonic techniques—A comparative study. Mater. Sci. Eng. A 2008, 489, 419–425. [Google Scholar] [CrossRef]
- Shembish, F.A.; Tong, H.; Kaizer, M.; Janal, M.N.; Thompson, V.P.; Opdam, N.J.; Zhang, Y. Fatigue resistance of CAD/CAM resin composite molar crowns. Dent. Mater. 2016, 32, 499–509. [Google Scholar] [CrossRef]
- Krejci, I.; Daher, R. Stress distribution difference between Lava Ultimate full crowns and IPS e. max CAD full crowns on a natural tooth and on tooth-shaped implant abutments. Odontology 2017, 105, 254–256. [Google Scholar] [CrossRef]
- Schepke, U.; Lohbauer, U.; Meijer, H.J.; Cune, M.S. Adhesive failure of Lava Ultimate and Lithium Disilicate crowns bonded to zirconia abutments: A prospective within-patient comparison. Int. J. Prosthodont. 2018, 31, 208–210. [Google Scholar] [CrossRef]
- Kumchai, H.; Juntavee, P.; Sun, A.F.; Nathanson, D. Comparing the Repair of Veneered Zirconia Crowns with Ceramic or Composite Resin: An in Vitro Study. Dent. J. 2020, 8, 37. [Google Scholar] [CrossRef]
- Floystrand, F.; Kleven, E.; Oilo, G. A novel miniature bite force recorder and its clinical application. Acta. Odontol. Scand. 1982, 40, 209–214. [Google Scholar] [CrossRef]
- Attia, A.; Kern, M. Fracture strength of all-ceramic crowns luted using two bonding methods. J. Prosthet. Dent. 2004, 91, 247–252. [Google Scholar] [CrossRef]
- Quinn, J.B.; Quinn, G.D.; Kelly, J.R.; Scherrer, S.S. Fractographic analyses of three ceramic whole crown restoration failures. Dent. Mater. 2005, 21, 920–929. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Lee, K.B. Effect of Tooth Types on the Accuracy of Dental 3D Scanners: An In Vitro Study. Materials 2020, 13, 1744. [Google Scholar] [CrossRef] [PubMed]


| Product Name | Code | Manufacturer | Lot No. | Shade | Composition | Groups | |
|---|---|---|---|---|---|---|---|
| Tooth | Titanium | ||||||
| IPS e.max CAD | LS | Ivoclar Vivadent | Y00999, Y26950 | A2-HT | 0.2–2 μm lithium disilicate glass-ceramic | LS_TO | LS_TI |
| Vita Enamic | PICN | Vita Zahnfabrik | 78540, 78880 | 2M2-HT | Polymer-infiltrated feldspathic ceramic-network material (UDMA, TEGDMA) with 86 wt% ceramic | PICN_TO | PICN_TI |
| Cerasmart | RNC | GC dental product | 1910101 | A2-HT | Composite resin material (BisMEPP, UDMA, DMA) with 71 wt% silica and barium glass nanoparticles | RNC_TO | RNC_TI |
| Celtra Duo | ZLS | Dentsply Sirona | 16006746, 16006750 | A2-HT | 10% dissolved zirconia in a silica-based glass matrix. | ZLS_TO | ZLS_TI |
| Group | Mean ± SD (N) | p | |
|---|---|---|---|
| TO | TI | ||
| LS | 1137.33 ± 139.30 a | 1346.60 ± 103.53 a | 0.001 * |
| PICN | 789.73 ± 98.90 b | 670.24 ± 40.80 b | 0.002 * |
| RNC | 707.39 ± 100.74 b | 334.39 ± 36.30 c | <0.001 * |
| ZLS | 976.47 ± 107.37 c | 1211.32 ± 93.70 d | <0.001 * |
| Source | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Corrected Model | 7,804,216.38 a | 7 | 1,114,888.055 | 121.937 | <0.001 * |
| Intercept | 64,323,143.29 | 1 | 64,323,143.29 | 7035.104 | <0.001 * |
| Material | 6,542,454.222 | 3 | 2,180,818.074 | 238.519 | <0.001 * |
| Abutment | 2923.299 | 1 | 2923.299 | 0.320 | 0.574 |
| Material * abutment | 1,258,838.862 | 3 | 419,612.954 | 45.894 | <0.001 * |
| Error | 658,308.150 | 72 | 9143.169 | ||
| Total | 72,785,667.82 | 80 | |||
| Corrected Total | 8,462,524.533 | 79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, M.-S.; Choi, Y.-S.; Lee, H.-H.; Lee, J.-H.; Ahn, J. Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method. Materials 2021, 14, 3115. https://doi.org/10.3390/ma14113115
Hong M-S, Choi Y-S, Lee H-H, Lee J-H, Ahn J. Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method. Materials. 2021; 14(11):3115. https://doi.org/10.3390/ma14113115
Chicago/Turabian StyleHong, Myung-Sik, Yu-Sung Choi, Hae-Hyoung Lee, Jung-Hwan Lee, and Junyong Ahn. 2021. "Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method" Materials 14, no. 11: 3115. https://doi.org/10.3390/ma14113115
APA StyleHong, M.-S., Choi, Y.-S., Lee, H.-H., Lee, J.-H., & Ahn, J. (2021). Comparison of Mechanical Properties of Chairside CAD/CAM Restorations Fabricated Using a Standardization Method. Materials, 14(11), 3115. https://doi.org/10.3390/ma14113115








