Polymer Hernia Repair Materials: Adapting to Patient Needs and Surgical Techniques
Abstract
:1. Introduction
2. Classic Polymer Biomaterials and Hernia Repair
2.1. Structural Modifications to the Classic Polymer Biomaterials
2.2. Modifications to Improve Host Tissue Incorporation
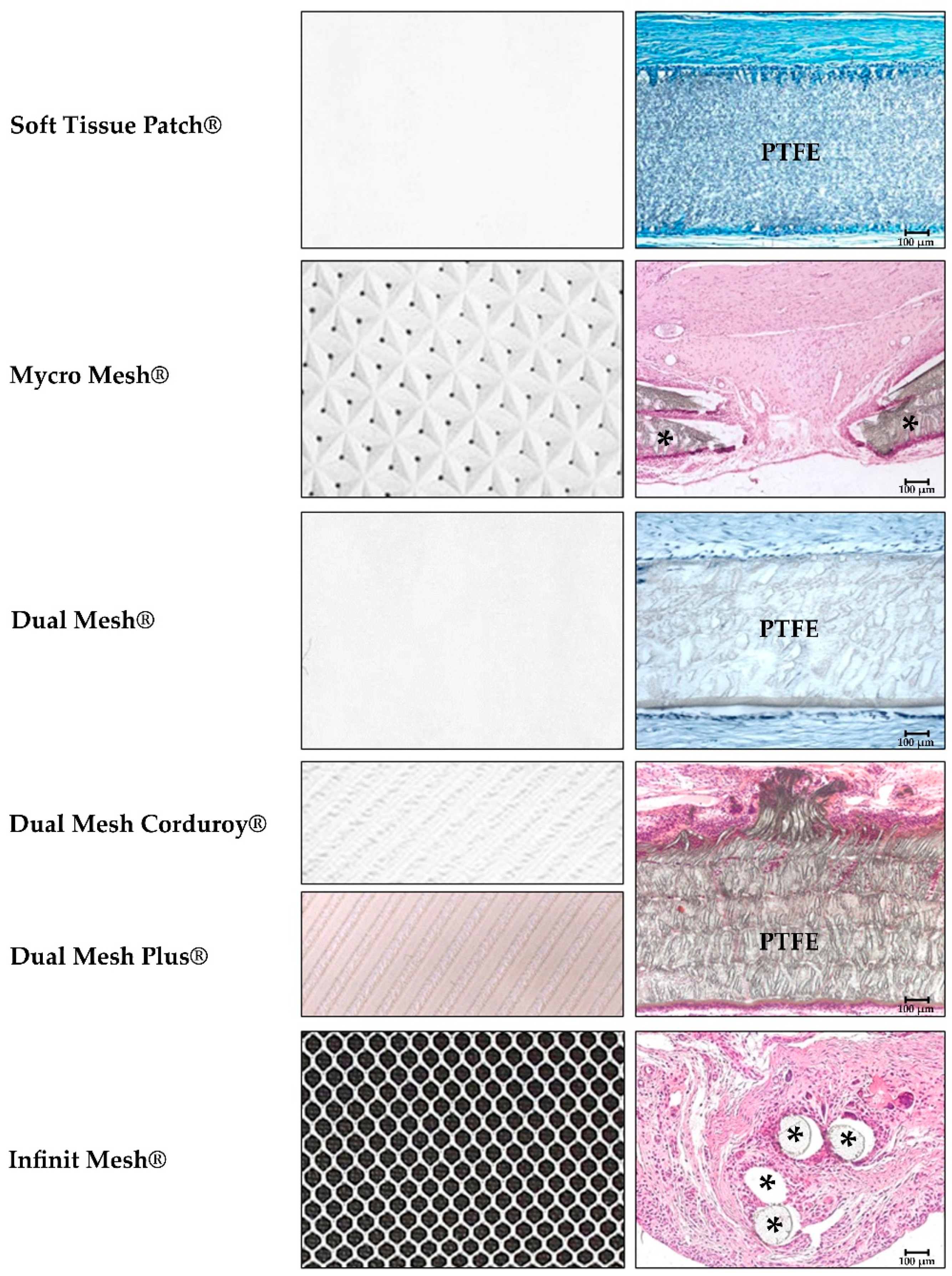
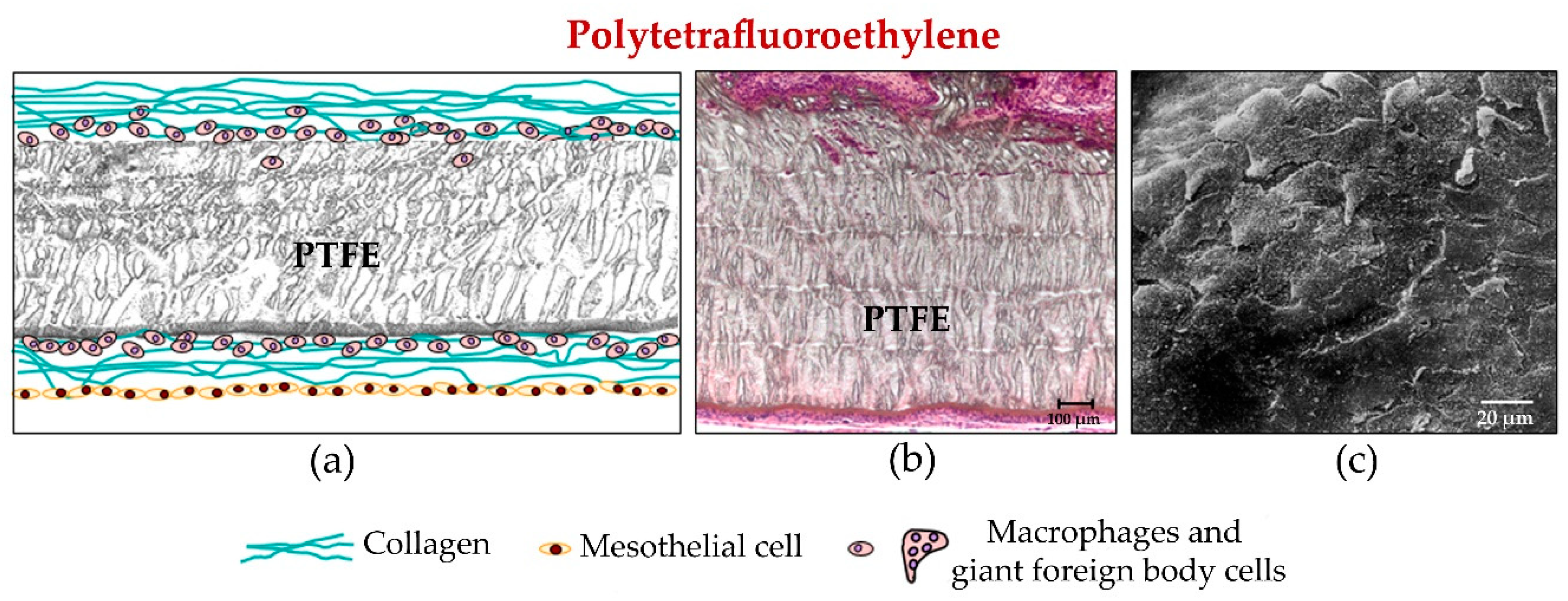
2.2.1. Expanded Polytetrafluoroethylene
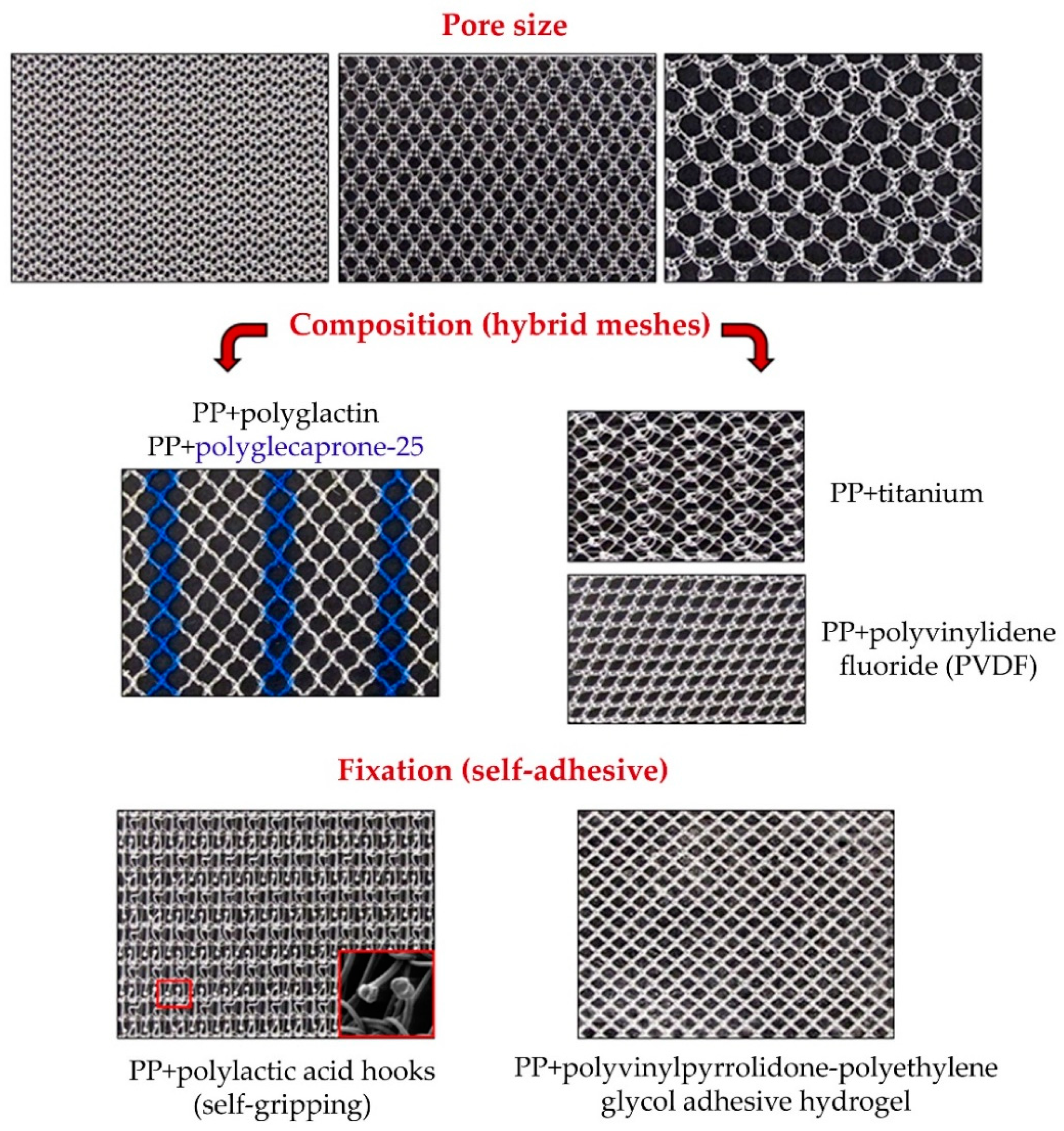
2.2.2. Polypropylene
2.3. Modifications Designed to Improve Adhesion to the Host: Self-Gripping Meshes
2.4. Reticular Polyvinylidenfluoride (PVDF) Materials
2.5. Condensed Polytetrafluoroethylene (cPTFE)
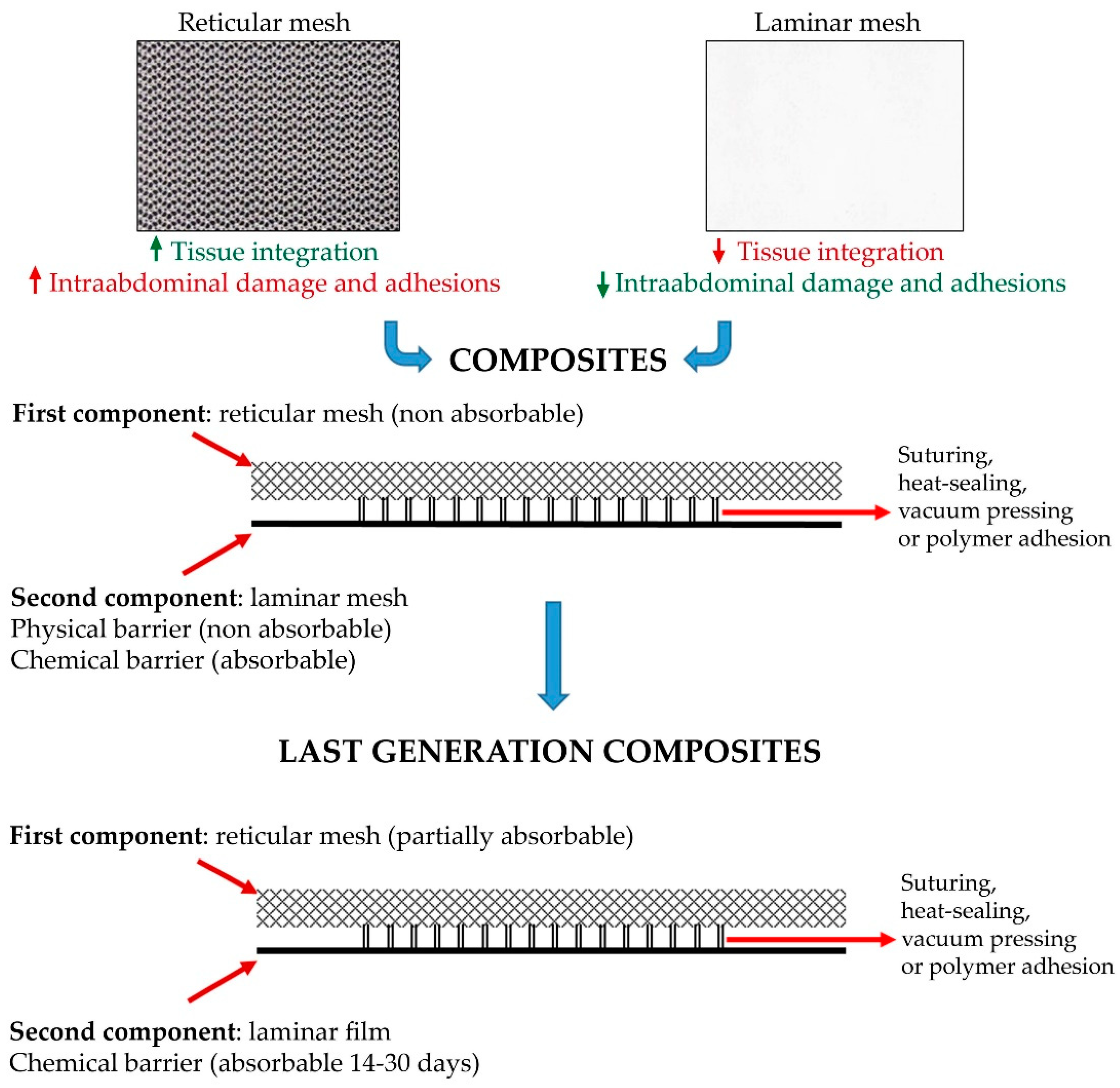
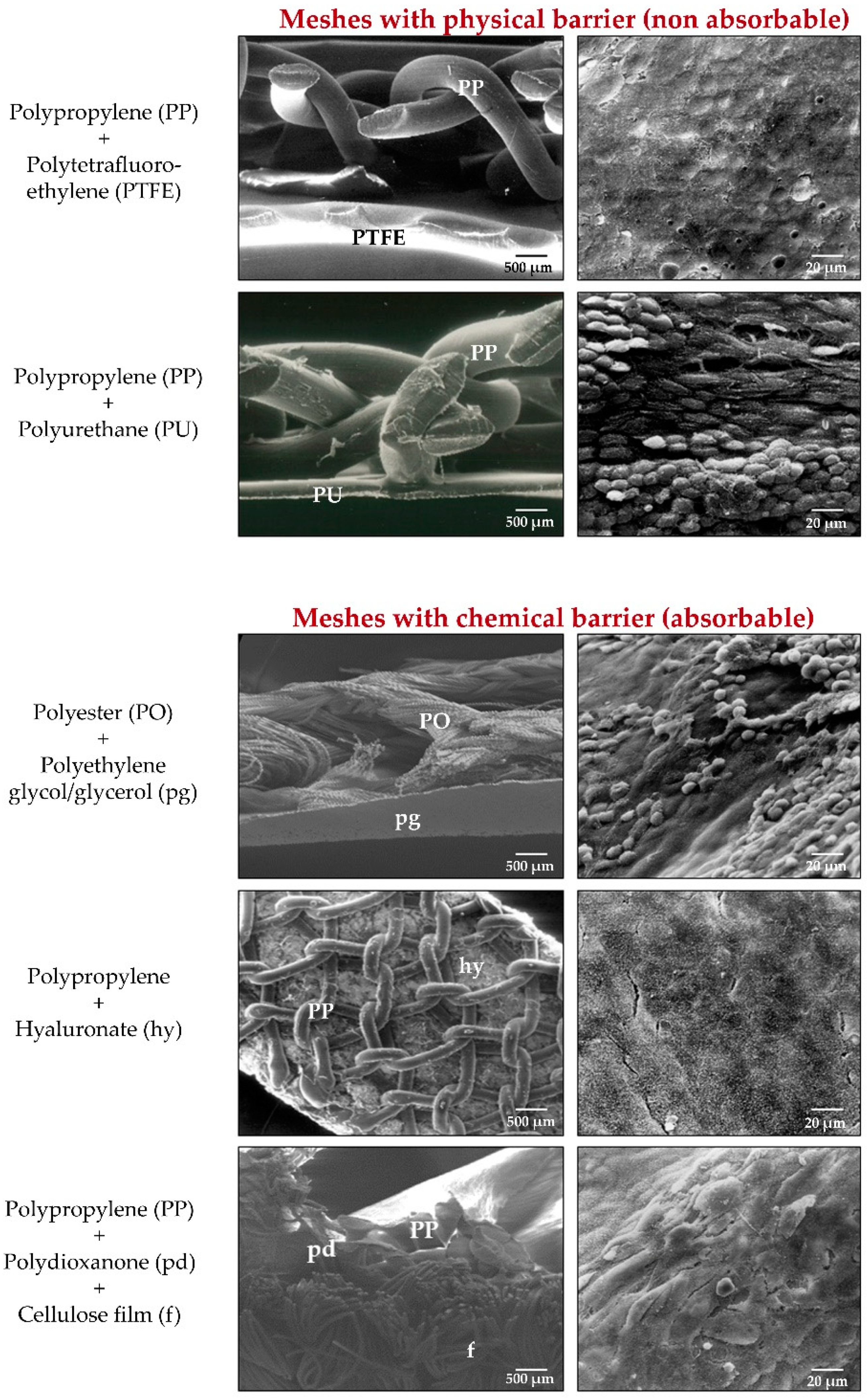
3. Composite Materials
3.1. Classic Composite Materials
3.2. Structural Modifications to Classic Composite Materials
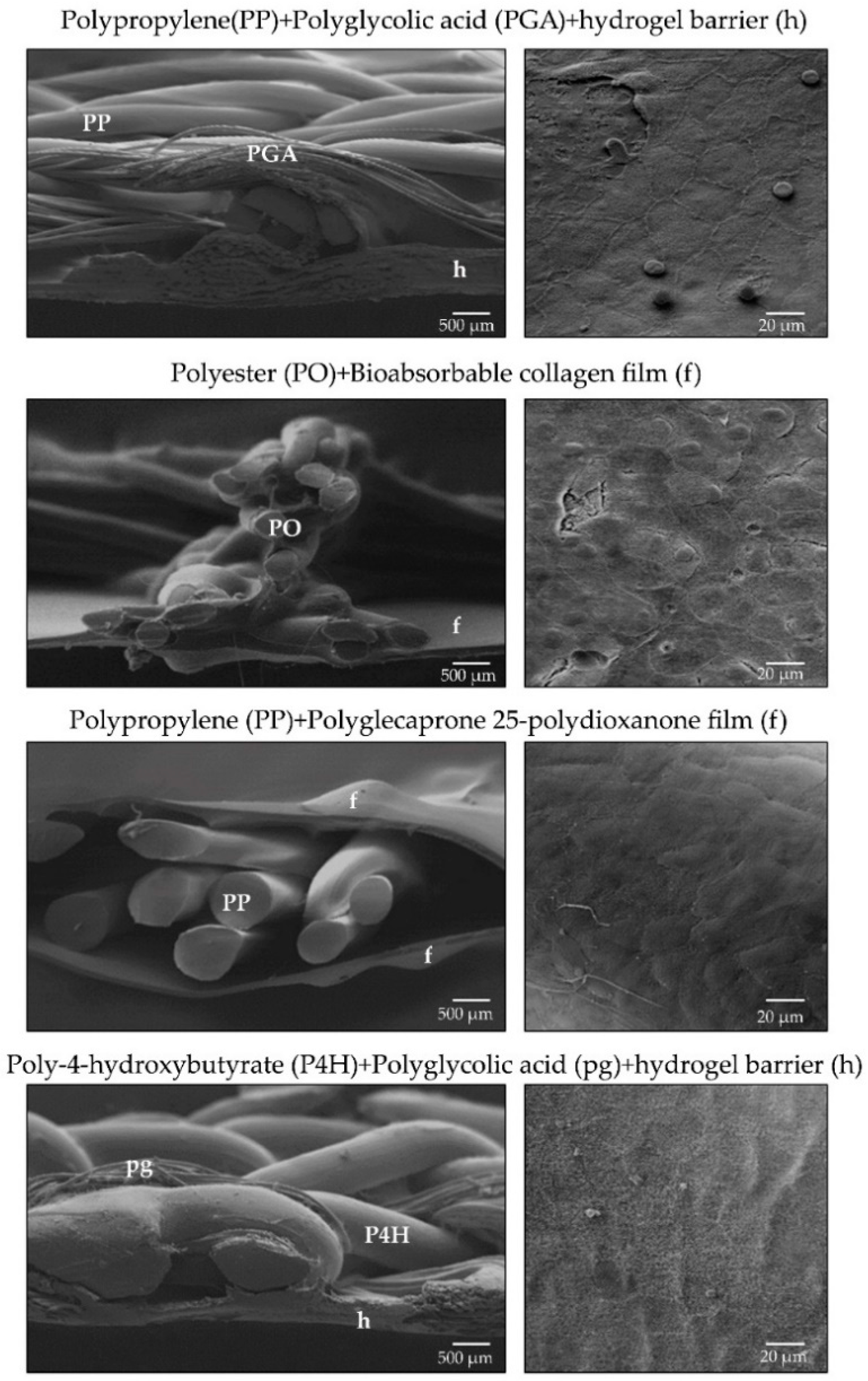
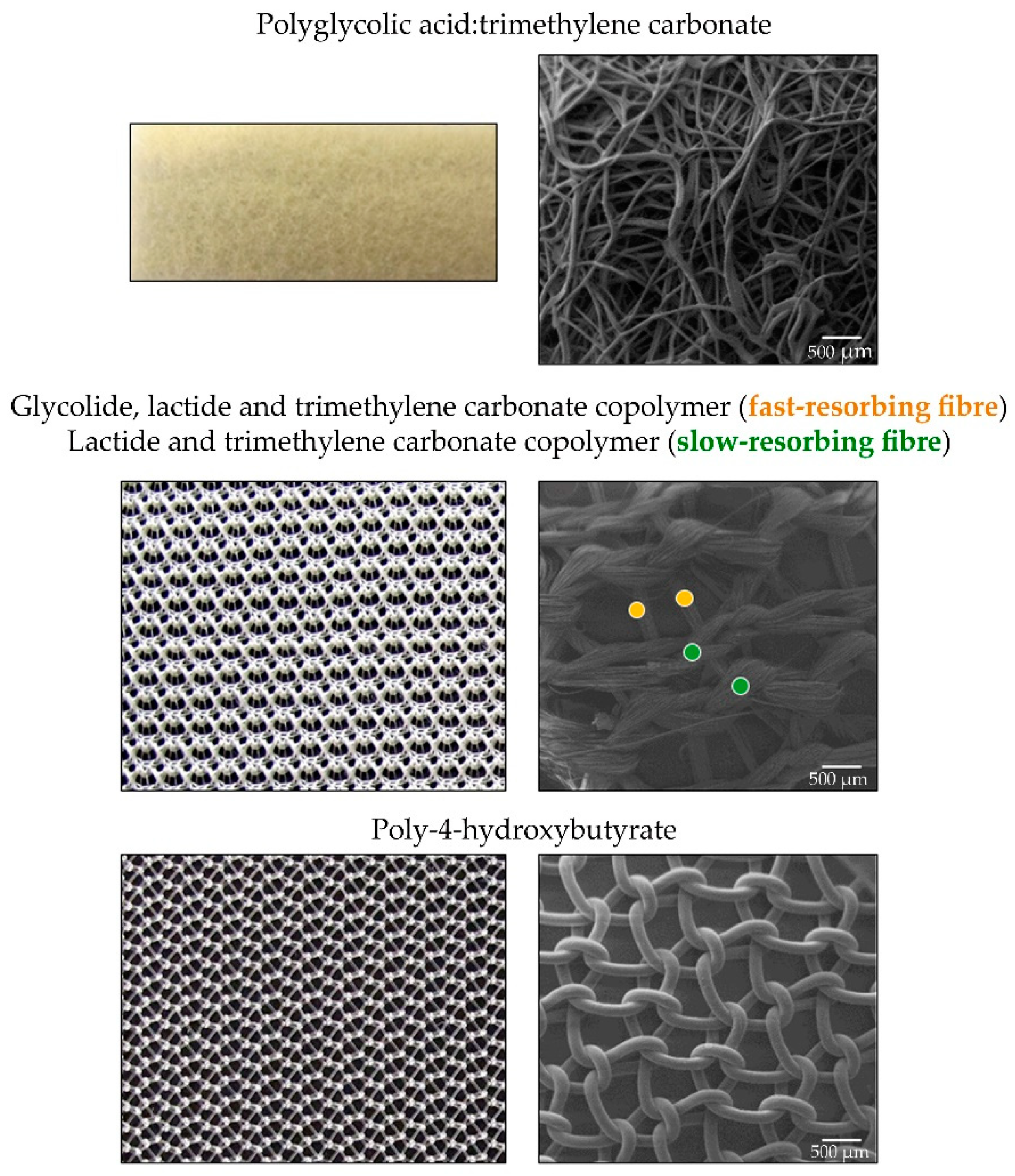
4. Last-Generation Polymer Materials
5. Prosthetic Structure and Placement in Host Tissue: Adapting to Surgical Techniques
6. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ratner, B.D.; Hoffman, A.S. Biomaterials Science: An Introduction to Materials in Medicine, 3rd ed.; Academic Press: San Diego, CA, USA, 2012. [Google Scholar]
- Kingsnorth, A.; LeBlanc, K. Hernias: Inguinal and incisional. Lancet 2003, 362, 1561–1571. [Google Scholar] [CrossRef]
- Luijendijk, R.W.; Hop, W.C.; van del Tol, M.P.; de Lange, D.C.; Braaksma, M.M.; Ijzermans, J.N.; Boelhouwer, R.U.; de Vriers, B.C.; Salu, M.K.; Wereldsma, J.C.; et al. A comparison of suture repair with mesh repair for incisional hernia. N. Engl. J. Med. 2000, 343, 392–398. [Google Scholar] [CrossRef]
- Langer, C.; Liersch, T.; Kley, C.; Flosman, M.; Süss, M.; Siemer, A. Twenty-five years of experience in incisional hernia surgery. A comparative retrospective study of 432 incisional hernia repairs. Der Chir. Z. Fur Alle Geb. Der Oper. Medizen 2003, 74, 638–645. [Google Scholar]
- Yang, F. Radical tumor excision and immediate abdominal wall reconstruction in patients with aggressive neoplasm com-promised full thickness lower abdominal wall. Am. J. Surg. 2013, 205, 15–21. [Google Scholar] [CrossRef]
- Schumpelick, V.; Klinge, U. Prosthetic implants for hernia repair. BJS 2003, 90, 1457–1458. [Google Scholar] [CrossRef] [PubMed]
- Rösch, R.; Junge, K.; Schachtrupp, A.; Klinge, U.; Klosterhalfen, B.; Schumpelick, V. Mesh implants in hernia repair. Eur. Surg. Res. 2003, 35, 161–166. [Google Scholar] [CrossRef]
- Klinge, U. Mesh for hernia repair. BJS 2008, 95, 539–540. [Google Scholar] [CrossRef] [PubMed]
- The HerniaSurge Group. International guidelines for groin hernia management. Hernia 2018, 22, 1–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lichtenstein, I.L.; Shulman, A.G. Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int. Surg. 1986, 71, 1–4. [Google Scholar]
- Sanders, D.L.; Kingsnorth, A.N. From ancient to contemporary times: A concise history of incisional hernia repair. Hernia 2011, 16, 1–7. [Google Scholar] [CrossRef]
- Usher, F.C.; Cogan, J.E.; Lowry, T.I. A new technique for the repair of inguinal and incisional hernias. Arch. Surg. 1960, 81, 847–854. [Google Scholar] [CrossRef]
- Wolstenholme, J.T. Use of commercial Dacron fabric in the repair of inguinal hernias and abdominal wall defects. Arch. Surg. 1956, 73, 1004–1008. [Google Scholar] [CrossRef]
- Stoppa, R.E.; Petit, J.; Henry, X. Unsutured Dacron prothesis in groin hernias. Int. Surg. 1975, 60, 411–412. [Google Scholar]
- Wantz, G.E. Incisional hernioplasty with Mersilene. Surg. Gynecol. Obstet. 1991, 172, 129–137. [Google Scholar] [PubMed]
- Usher, F.C.; Hill, J.R.; Ochsner, J.L. Hernia repair with Marlex mesh. A comparison of techniques. Surgery 1959, 46, 718–724. [Google Scholar]
- Usher, F.C. A new technique for repairing large abdominal wall defects. Arch. Surg. 1961, 82, 870–877. [Google Scholar] [CrossRef]
- Usher, F.C. Knitted Marlex mesh. An improved Marlex prosthesis for repairing hernias and other tissues defects. Arch. Surg. 1961, 82, 771–773. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, E.; Blaisdell, F.; Hall, A.D. Use of knitted Marlex mesh in the repair of ventral hernias. Am. J. Surg. 1965, 110, 897–902. [Google Scholar] [CrossRef]
- Walker, P.M.; Langer, B. Marlex mesh for repair of abdominal wall defects. Can. J. Surg. 1976, 19, 211–215. [Google Scholar] [PubMed]
- Elliot, M.P.; Juler, G.L. Comparison of Marlex mesh and microporous Teflon sheets when used for hernia repair in the experimental animal. Am. J. Surg. 1979, 137, 342–345. [Google Scholar] [CrossRef]
- Cameron, A.E.P.; Taylor, D.E.M. Carbon-fibre versus Marlex mesh in the repair of experimental abdominal wall defects in rats. BJS 1985, 72, 648–650. [Google Scholar] [CrossRef]
- Murphy, J.L.; Freeman, J.B.; Dionne, P.G. Comparison of Marlex and Goretex to repair abdominal wall defects in the rat. Can. J. Surg. 1989, 32, 244–247. [Google Scholar]
- Lichtenstein, I.L.; Shulman, A.G.; Amid, P.K.; Montllor, M.M. The tension-free hernioplasty. Am. J. Surg. 1989, 157, 188–193. [Google Scholar] [CrossRef]
- Molloy, R.G.; Moran, K.T.; Waldron, R.P.; Brady, M.P.; Kirwan, W.O. Massive incisional hernia: Abdominal wall replacement with Marlex ™ mesh. BJS 1991, 78, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Matapurkar, B.G.; Gupta, A.K.; Agarwal, A.K. A new technique of “Marlex-Peritoneal Sandwich” in the repair of large incisional hernias. World J. Surg. 1991, 15, 768–770. [Google Scholar] [CrossRef] [PubMed]
- Liakakos, T.; Karanikas, I.; Panagiotidis, H.; Dendrinos, S. Use of Marlex mesh in the repair of recurrent incisional hernia. BJS 2005, 81, 248–249. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.H. A teflon weave for replacing tissue defects. Surg. Gynecol. Obstet. 1957, 104, 584–590. [Google Scholar] [PubMed]
- Gibson, L.D.; Stafford, C.E. Synthetic mesh repair of abdominal wall defects: Follow up and reappraisal. Am. Surg. 1964, 30, 481–486. [Google Scholar] [PubMed]
- Oshige, S. Fabrication of Porous Polytetrafluoroethylene. Japanese Patent No. 42-13560 (67/13560), August 1967. [Google Scholar]
- Gore, R.W. Process for producing porous products. U.S. Patent 3953566 (W.L. Gore and Assoc.), 27 April 1976. [Google Scholar]
- Sher, W.; Pollack, D.A.; Paulides, C.; Matsumoto, T. Repair of abdominal wall defects: Gore-Tex vs. Marlex graft. Am. Surg. 1980, 46, 618–623. [Google Scholar] [PubMed]
- Lamb, J.P.; Vitale, T.; Kaminski, D.L. Comparative evaluation of synthetic meshes used for abdominal wall replacement. Surgery 1983, 93, 643–648. [Google Scholar]
- Hamer-Hodges, D.W.; Scott, N.B. Surgeon’s workshop. Replacement of an abdominal wall defect using expanded PTFE sheet (Gore-tex). J. R. Coll. Surg. Edinb. 1985, 30, 65–67. [Google Scholar] [PubMed]
- Brown, G.L.; Richardson, J.D.; Malangoni, M.A.; Tobin, G.R.; Ackerman, D.; Polk, H.C. Comparison of Prosthetic Materials for Abdominal Wall Reconstruction in the Presence of Contamination and Infection. Ann. Surg. 1985, 201, 705–711. [Google Scholar] [CrossRef]
- Pairolero, P.C.; Arnold, P.G. Thoracic Wall Defects: Surgical Management of 205 Consecutive Patients. Mayo Clin. Proc. 1986, 61, 557–563. [Google Scholar] [CrossRef]
- Bauer, J.J.; Salky, B.A.; Gelernt, I.M.; Kreel, I. Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PFTE). Ann. Surg. 1987, 206, 765–769. [Google Scholar] [CrossRef] [PubMed]
- van der Lei, B.; Bleichrodt, R.P.; Simmermacher, R.K.J.; van Schilfgaarde, R. Expanded polytetrafluoroethylene patch for the repair of large abdominal wall defects. BJS 1989, 76, 803–805. [Google Scholar] [CrossRef]
- Law, N.W.; Ellis, H. Preliminary results for the repair of difficult recurrent inguinal hernias using expanded PTFE patch. Acta Chir. Scand. 1990, 156, 609–612. [Google Scholar] [PubMed]
- Law, N.W.; Ellis, H. A comparison of polypropylene mesh and expanded polytetrafluoroethylene patch for the repair of contaminated abdominal wall defects—An experimental study. Surgery 1991, 109, 652–655. [Google Scholar] [PubMed]
- DeBord, J.R.; Wyffels, P.L.; Marshall, S.; Miller, G.; Marshall, W.H. Repair of large ventral incisional hernias with expanded polytetrafluoroethylene prosthetic patches. Postgrad. Gen. Surg. 1992, 4, 156–160. [Google Scholar]
- Berliner, S.D. Clinical experience with an inlay expanded polytetrafluoroethylene soft tissue patch as an adjunct in inguinal hernia repair. Surg. Gynecol. Obstet. 1993, 176, 323–326. [Google Scholar]
- Bellón, J.M.; Contreras, L.A.; Sabater, C.; Buján, J. Pathologic and clinical aspects of repair of large incisional hernias after implant of a polytetrafluoroethylene prosthesis. World J. Surg. 1997, 21, 402–407. [Google Scholar] [CrossRef]
- Bellón, J.M.; Buján, J.; Contreras, L.A.; Carrera-San Martin, A.; Jurado, F. Comparison of a new type of polytetrafluoroethylene patch (Mycro Mesh) and polypropylene prosthesis (Marlex) for repair of abdominal wall defects. J. Am. Coll. Surg. 1996, 183, 11–18. [Google Scholar] [PubMed]
- Bellón, J.M.; Contreras, L.A.; Buján, J.; Martín, A.C.-S. Experimental assay of a Dual Mesh® polytetrafluoroethylene prosthesis (non-porous on one side) in the repair of abdominal wall defects. Biomaterials 1996, 17, 2367–2372. [Google Scholar] [CrossRef]
- Harrell, A.G.; Novitsky, Y.W.; Kercher, K.W.; Foster, M.; Burns, J.M.; Kuwada, T.S.; Heniford, B.T. In vitro infectability of prosthetic mesh by methicillin-resistant Staphylococcus aureus. Hernia 2006, 10, 120–124. [Google Scholar] [CrossRef]
- Melman, L.; Jenkins, E.D.; Hamilton, N.A.; Bender, L.C.; Brodt, M.D.; Deeken, C.R.; Greco, S.C.; Frisella, M.M.; Matthews, B.D. Histologic and biomechanical evaluation of a novel macroporous polytetrafluoroethylene knit mesh compared to light-weight and heavyweight polypropylene mesh in a porcine model of ventral hernia repair. Hernia 2011, 15, 423–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacob, D.A.; Schug-Pass, C.; Sommerer, F.; Tannapfel, A.; Lippert, H.; Köckerling, F. Comparison of a lightweight polypro-pylene mesh (Optilene® LP) and a large-pore knitted PTFE mesh (Gore® Infinit® mesh)-biocompatibility in a standardized en-doscopic extraperitoneal hernia model. Langenbecks Arch. Surg. 2012, 397, 283–289. [Google Scholar] [CrossRef]
- Bellón, J.M.; Jurado, F.; García-Honduvilla, N.; López, R.; Martín, A.C.-S.; Buján, J. The structure of a biomaterial rather than its chemical composition modulates the repair process at the peritoneal level. Am. J. Surg. 2002, 184, 154–159. [Google Scholar] [CrossRef]
- Klinge, U.; Klosterhalfen, B.; Birkenhauer, V.; Junge, K.; Conze, J.; Schumpelick, V. Impact of polymer pore size on the interface scar formation in a rat model. J. Surg. Res. 2002, 103, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Weyhe, D.; Schmitz, I.; Belyaev, O.; Grabs, R.; Müller, K.-M.; Uhl, W.; Zumtobel, V. Experimental comparison of monofile light and heavy polypropylene meshes: Less weight does not mean less biological response. World J. Surg. 2006, 30, 1586–1591. [Google Scholar] [CrossRef]
- Cobb, W.S.; Kercher, K.W.; Heniford, B.T. The argument for lightweight polypropylene mesh in hernia repair. Surg. Innov. 2005, 12, 63–69. [Google Scholar] [CrossRef]
- Cobb, W.S.; Burns, J.M.; Peindl, R.D.; Carbonell, A.M.; Matthews, B.D.; Kercher, K.W.; Heniford, B.T. Textile analysis of heavy weight, mid-weight, and light weight polypropylene mesh in a porcine ventral hernia model. J. Surg. Res. 2006, 136, 1–7. [Google Scholar] [CrossRef]
- Earle, D.B.; Mark, L.A. Prosthetic material in inguinal hernia repair: How do I choose? Surg. Clin. N. Am. 2008, 88, 179–201. [Google Scholar] [CrossRef] [PubMed]
- Weyhe, D.; Belyaev, O.; Muller, C.; Meurer, K.; Bauer, K.-H.; Papapostolou, G.; Uhl, W. Improving outcomes in hernia repair by the use of light meshes—A comparison of different implant constructions based on a critical appraisal of the literature. World J. Surg. 2006, 31, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Klosterhalfen, B.; Junge, K.; Klinge, U. The lightweight and large porous mesh concept for hernia repair. Expert Rev. Med. Devices 2005, 2, 103–117. [Google Scholar] [CrossRef] [PubMed]
- Junge, K.; Rosch, R.; Krones, C.J.; Klinge, U.; Mertens, P.R.; Lynen, P.; Shumpelick, V.; Klosterhalfen, B. Influence of poly-glecaprone 25 supplementation on the biocompatibility of a polypropylene mesh for hernia repair. Hernia 2005, 9, 212–217. [Google Scholar] [CrossRef]
- Köckerling, F.; Schug-Pass, C. What do we know about titanized polypropylene meshes? An evidence-based review of the literature. Hernia 2013, 18, 445–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellón, J.M.; Buján, J.; Contreras, L.A.; Carrera-San Martín, A.; Hernando, A.; Jurado, F. Improvement of the tissue integration of a new modified polytetrafluoroethylene prosthesis: MycroMesh. Biomaterials 1996, 17, 1265–1271. [Google Scholar] [CrossRef]
- Simmermacher, R.K.; van der Lei, B.; Schakenraad, J.M.; Bleichrodt, R.P. Improved tissue ingrowth and anchorage of expanded polytetrafluoroethylene by perforation: An experimental study in the rat. Biomaterials 1991, 12, 22–24. [Google Scholar] [CrossRef]
- Bellón, J.M.; Buján, J.; Contreras, L.; Hernando, A.; Jurado, F. Similarity in behavior of polytetrafluoroethylene (ePTFE) prostheses implanted into different interfaces. J. Biomed. Mat. Res. 1996, 31, 1–9. [Google Scholar] [CrossRef]
- Pascual, G.; Hernández, B.; Peña, E.; Sotomayor, S.; Calvo, B.; Bellón, J.M. Regeneración tisular de la pared abdominal después del implante de una nueva malla quirúrgica macroporosa compuesta por politetrafluoroetileno no expandido. Rev. His-panoam. Hernia 2015, 3, 17–25. [Google Scholar] [CrossRef] [Green Version]
- Hernández-Gascón, B.; Peña, E.; Melero, H.; Pascual, G.; Doblaré, M.; Ginebra, M.P.; Bellón, J.M.; Calvo, B. Mechanical be-haviour of synthetic meshes: Finite element simulation of the herniated abdominal wall. Acta Biomater. 2011, 7, 3905–3913. [Google Scholar] [CrossRef]
- Bellón, J.M.; Buján, J.; Contreras, L.; Hernando, A. Interface formed between visceral peritoneum and experimental polypropylene or polytetrafluoroethylene abdominal wall implants. J. Mat. Sci. Mat. Med. 1996, 7, 331–336. [Google Scholar] [CrossRef]
- Bellón, J.M.; Contreras, L.A.; Pascual, G.; Buján, J. Neoperitoneal formation after implantation of various biomaterials for the repair of abdominal wall defects in rabbits. Eur. J. Surg. 1999, 165, 145–150. [Google Scholar]
- LeBlanc, K.A.; Booth, W.V. Repair of primary and secondary inguinal hernias using an expanded polytetrafluoroethylene patch. Contemp. Surg. 1992, 41, 29–35. [Google Scholar]
- LeBlanc, K.A.; Booth, W.V. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: Preliminary findings. Surg. Laparosc. Endosc. Percutaneous Tech. 1993, 3, 39–41. [Google Scholar]
- Koehler, R.H.; Begos, D.; Berger, D.; Carey, S.; LeBlanc, K.; Park, A.; Ramshaw, B.; Smoot, R.; Voeller, G. Minimal adhesions to ePTFE mesh after laparoscopic ventral incisional hernia repair: Preoperative findings in 65 cases. JSLS J. Soc. Laparoendosc. Surg. 2003, 7, 335–340. [Google Scholar]
- Klinge, U.; Klosterhalfen, B.; Conze, J.; Limberg, W.; Obolenski, B.; Öttinger, A.P.; Schumpelick, V. Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur. J. Surg. 2003, 164, 951–960. [Google Scholar] [CrossRef]
- Klinge, U.; Junge, K.; Stumpf, M.; Öttinger, A.P.; Klosterhalfen, B. Functional and morphological evaluation of a low-weight, monofilament polypropylene mesh for hernia repair. J. Biomed. Mater. Res. 2002, 63, 129–136. [Google Scholar] [CrossRef]
- Bellón, J.M.; Rodríguez, M.; García-Honduvilla, N.; Pascual, G.; Buján, J. Partially absorbable meshes for hernia repair offer advantages over nonabsorbable meshes. Am. J. Surg. 2007, 194, 68–74. [Google Scholar] [CrossRef]
- Greca, F.H.; de Paula, J.B.; Biondo-Simoes, M.L.; da Costa, F.D.; da Silva, A.P.; Time, S.; Mansur, A. The influence of differing pore sizes on the biocompatibility of two polypropylene meshes in the repair of abdominal defects: Experimental study in dogs. Hernia 2001, 5, 59–64. [Google Scholar]
- Pascual, G.; Rodríguez, M.; Gómez-Gil, V.; García-Honduvilla, N.; Buján, J.; Bellón, J.M. Early tissue incorporation and collagen deposition in lightweight polypropylene meshes: Bioassay in an experimental model of ventral hernia. Surgery 2008, 144, 427–435. [Google Scholar] [CrossRef]
- Pascual, G.; Hernández-Gascón, B.; Rodríguez, M.; Sotomayor, S.; Peña, E.; Calvo, B.; Bellón, J.M. The long-term behavior of lightweight and heavyweight meshes used to repair abdominal wall defects is determined by the host tissue repair process provoked by the mesh. Surgery 2012, 152, 886–895. [Google Scholar] [CrossRef]
- Bellón, J.; Buján, J.; Contreras, L.; Hernando, A. Integration of biomaterials implanted into abdominal wall: Process of scar formation and macrophage response. Biomaterials 1995, 16, 381–387. [Google Scholar] [CrossRef]
- Bellón, J.M.; García-Honduvilla, N.; López, R.; Corrales, C.; Jurado, F.; Buján, J. In vitro mesothelialization of prosthetic material designed for the repair of abdominal wall defects. J. Mat. Sci. Mat. Med. 2003, 14, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Junge, K.; Rosch, R.; Klinge, U.; Saklak, M.; Klosterhalfen, B.; Peiper, C.; Schumpelick, V. Titanium coating of a polypropylene mesh for hernia repair: Effect of biocompatibility. Hernia 2005, 9, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Scheidbach, H.; Tannapfel, A.; Schmidt, U.; Lippert, H.; Köckerling, F. Influence of Titanium Coating on the Biocompatibility of a Heavyweight Polypropylene Mesh. Eur. Surg. Res. 2004, 36, 313–317. [Google Scholar] [CrossRef]
- Schug-Pass, C.; Tamme, C.; Tannapfel, A.; Kökerling, F. A lightweight polypropylene mesh (TiMesh) for laparoscopic intraperitoneal repair of abdominal wall hernias. Surg. Endosc. 2006, 20, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Koch, A.; Bringman, S.; Myrelid, P.; Smeds, S.; Kald, A. Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. BJS 2008, 95, 1226–1231. [Google Scholar] [CrossRef]
- Moreno-Egea, A.; Carrillo-Alcaraz, A.; Soria-Aledo, V. Randomized clinical trial of laparoscopic hernia repair comparing titanium-coated lightweight mesh and medium-weight composite mesh. Surg. Endosc. 2012, 27, 231–239. [Google Scholar] [CrossRef]
- Chastan, P. Tension-free open hernia repair using an innovative self-gripping semi-resorbable mesh. Hernia 2008, 13, 137–142. [Google Scholar] [CrossRef]
- Champault, G.; Polliand, C.; Dufour, F.; Ziol, M.; Behr, L. A “self adhering” prosthesis for hernia repair: Experimental study. Hernia 2008, 13, 49–52. [Google Scholar] [CrossRef]
- Ben Yehuda, A.; Nyska, A.; Szold, A. Mesh fixation using novel bio-adhesive coating compared to tack fixation for IPOM hernia repair: In vivo evaluation in a porcine model. Surg. Endosc. 2019, 33, 2364–2375. [Google Scholar] [CrossRef]
- Muysoms, F.E.; Norik, B.; Kyke-Lienhase, I.; Berrevoet, F. Mesh fixation alternatives in laparoscopic ventral hernia repair. Surg. Technol. Int. 2012, 22, 125–132. [Google Scholar]
- Hollinsky, C.; Kolbe, T.; Walter, I.; Joachim, A.; Sandberg, S.; Koch, T.; Rülicke, T. Comparison of a new self-gripping mesh with other fixation methods for laparoscopic hernia repair in a rat model. J. Am. Coll. Surg. 2009, 208, 1107–1114. [Google Scholar] [CrossRef]
- Champault, G.; Torcivia, A.; Paolino, L.; Chaddad, W.; Lacaine, F.; Barrat, C. A self-adhering mesh for inguinal hernia repair: Preliminary results of a prospective multicenter study. Hernia 2011, 15, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Sanders, D.L.; Nienhuijs, S.; Ziprin, P.; Miserez, M.; Gingell-Littlejohn, M.; Smeds, S. Randomized clinical trial comparing self-gripping mesh with suture fixation of lightweight polypropylene mesh in open inguinal hernia repair. BJS 2014, 101, 1373–1382. [Google Scholar] [CrossRef]
- Gruber-Blum, S.; Riepl, N.; Brand, J.; Keibl, C.; Redl, H.; Fortelny, R.H.; Petter-Puchner, A.H. A comparison of Progrip® and Adhesix® self-adhering hernia meshes in an onlay model in the rat. Hernia 2014, 18, 761–769. [Google Scholar] [CrossRef]
- Tabbara, M.; Genser, L.; Bossi, M.; Barat, M.; Polliand, C.; Carandina, S.; Barrat, C. Inguinal hernia repair using self-adhering sutureless mesh: Adhesix™: A 3-year follow-up with low chronic pain and recurrence rate. Am. Surg. 2016, 82, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Molegraaf, M.; Kaufmann, R.; Lange, J. Comparison of self-gripping mesh and sutured mesh in open inguinal hernia repair: A meta-analysis of long-term results. Surgery 2018, 163, 351–360. [Google Scholar] [CrossRef]
- Thölix, A.-M.; Kössi, J.; Remes, V.; Scheinin, T.; Harju, J. Lower incidence of postoperative pain after open inguinal hernia surgery with the usage of synthetic glue-coated mesh (adhesix®). Am. Surg. 2018, 84, 1932–1937. [Google Scholar] [CrossRef]
- Urban, E.; King, M.W.; Guidoin, R.; Laroche, G.; Marois, Y.; Martin, L.; Cardou, A.; Douville, Y. Why make monofilament sutures out of polyvinylidene fluoride? Asaio J. 1994, 40, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Mary, C.; Marois, Y.; King, M.; Laroche, G.; Douville, Y.; Martin, L.; Guidoin, R. Comparison of the in vivo behaviour of polyvinylidene fluoride and polypropylene sutures in vascular surgery. Asaio J. 1998, 44, 199–206. [Google Scholar] [CrossRef]
- Junge, K.; Binnebösel, M.; Rosch, R.; Jansen, M.; Kammer, D.; Otto, J.; Schumpelick, V.; Klinge, U. Adhesion formation of a polyvinylidenfluoride/polypropylene mesh for intra-abdominal placement in a rodent animal model. Surg. Endosc. 2008, 23, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Klinge, U.; Klosterhalfen, B.; Öttinger, A.P.; Junge, K.; Schumpelick, V. PVDF as a new polymer for the construction of surgical meshes. Biomaterials 2002, 23, 3487–3493. [Google Scholar] [CrossRef]
- Conze, J.; Junge, K.; Weiss, C.; Anurov, M.; Öttinger, A.P.; Klinge, U.; Schumpelick, V. New polymer for intra-abdominal meshes-PVDF copolymer. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2008, 87, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Fortelny, R.H.; Petter-Puchner, A.H.; Glaser, K.S.; Offner, F.; Benesch, T.; Rohr, M. Adverse effects of polyvinylidene fluoride-coated polypropylene mesh used for laparoscopic intraperitoneal onlay repair of incisional hernia. Br. J. Surg. 2010, 97, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- Jamry, A.; Jalynski, M.; Piskorz, L.; Brocki, M. Assessment of adhesion formation after laparoscopic intraperitoneal implantation of Dynamesh IPOM mesh. Arch. Med. Sci. 2013, 3, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Tandon, A.; Shahzad, K.; Pathak, S.; Oommen, C.M.; Nunes, Q.M.; Smart, N. Parietex composite mesh versus DynaMesh–IPOM for laparoscopic incisional and ventral hernia repair: A retrospective cohort study. Ann. R. Coll. Surg. Engl. 2016, 98, 568–573. [Google Scholar] [CrossRef] [Green Version]
- D’Amore, L.; Ceci, F.; Mattia, S.; Fabbi, M.; Negro, P.; Gossetti, F. Adhesion prevention in ventral hernia repair: An experi-mental study comparing three lightweight porous meshes recommended for intraperitoneal use. Hernia 2017, 21, 115–123. [Google Scholar] [CrossRef]
- Gómez-Gil, V.; Rodríguez, M.; García-Moreno Nisa, F.; Pérez-Köhler, B.; Pascual, G. Evaluation of synthetic reticular hybrid meshes designed for intraperitoneal abdominal wall repair: Preclinical and in vitro behavior. PLoS ONE 2019, 14, e0213005. [Google Scholar] [CrossRef]
- Domen, A.; Stabel, C.; Jawad, R.; Duchateau, N.; Franzen, E.; Vanclooster, P.; De Gheldere, C. Postoperative ileus after laparoscopic primary and incisional abdominal hernia repair with intraperitoneal mesh (DynaMesh®-IPOM versus Parietex™ Composite): A single institution experience. Langenbecks Arch. Surg. 2021, 406, 209–218. [Google Scholar] [CrossRef]
- Voskerician, G.; Gingras, P.H.; Anderson, J.M. Macroporous condensed poly(tetrafluoroethylene). I. In vivo inflammatory response and healing characteristics . J. Biomed. Mat. Res. 2006, 76A, 234–242. [Google Scholar] [CrossRef]
- Voskerician, G.; Rodriguez, A.; Gingras, P.H. Macroporous condensed poly(tetra fluoro-ethylene). II. In vivo effect on adhesion formation and tissue integration . J. Biomed. Mater. Res. Part. A 2007, 82, 426–435. [Google Scholar] [CrossRef]
- Raptis, D.A.; Vichova, B.; Breza, J.; Skipworth, J.; Barker, S. A comparison of woven versus nonwoven polypropylene (PP) and expanded versus condensed polytetrafluoroethylene (PTFE) on their intraperitoneal incorporation and adhesion for-mation. J. Surg. Res. 2011, 169, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Cheesborough, J.E.; Liu, J.; Hsu, D.; Dumanian, G.A. Prospective repair of ventral hernia working group type 3 and 4 abdominal wall defects with condensed polytetrafluoroethylene (MotifMESH) mesh. Am. J. Surg. 2016, 211, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schein, M.; Wittmann, D.H.; Aprahamian, C.C.; Condon, R.E. The abdominal compartment syndrome: The physiological and clinical consequences of elevated intra-abdominal pressure. J. Am. Coll. Surg 1995, 180, 745–753. [Google Scholar] [PubMed]
- Bellón, J.M.; Buján, J.; Contreras, L.; Jurado, F. Use of nonporous polytetrafluoroethylene prosthesis in combination with polypropylene prosthetic abdominal wall implants in prevention of peritoneal adhesions. J. Biomed. Mat. Res. 1997, 38, 197–202. [Google Scholar] [CrossRef]
- Walker, A.P.; Henderson, J.; Condon, R.E. Double-Layer Prostheses for repair of abdominal wall defects in a rabbit model. J. Surg. Res. 1993, 55, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Amid, P.K.; Shulman, A.G.; Lichtenstein, I.L.; Sostrin, S.; Young, J.; Hakakha, M. Experimental evaluation of a new compo-site mesh with the selective property of incorporation to the abdominal wall without adhering to the intestines. J. Biomed. Mat. Res. 1994, 28, 373–375. [Google Scholar] [CrossRef] [PubMed]
- Bendavid, R. Composite mesh (polypropylene ePTFE) in the intraperitoneal position. A report of 30 cases. Hernia 1997, 1, 5–8. [Google Scholar] [CrossRef]
- Naim, J.O.; Pulley, D.; Scanlan, K.; Hinshaw, J.R.; Lanzafame, R.J. Reduction of postoperative adhesions to marlex mesh using experimental adhesion barriers in rats. J. Laparoendosc. Surg. 1993, 3, 187–190. [Google Scholar] [CrossRef]
- Soler, M.; Verhaeghe, P.; Essomba, A.; Sevestre, H.; Stoppa, R. Le traitment des éventrations post-operatoires par prothèse composée (polyester-polyglactine 910). Etude clinique et expérimentale. Ann. Chir. 1993, 47, 598–608. [Google Scholar] [PubMed]
- Alponat, A.; Lakshminarasappa, S.T.; Rajnakova, A.; Moochhala, S.; Goh, P.M.Y.; Chan, S.T.F. Effects of physical barriers in prevention of adhesions: An incisional hernia model in rabbits. J. Surg. Res. 1997, 68, 126–132. [Google Scholar] [CrossRef]
- Arnold, P.B.; Green, C.W.; Foresman, P.A.; Rodeheaver, G.T. Evaluation of resorbable barriers for preventing surgical adhesions. Fertil. Steril. 2000, 73, 157–161. [Google Scholar] [CrossRef]
- Greenawalt, K.E.; Butler, T.J.; Rowe, E.A.; Finneral, A.C.; Garlick, D.S.; Burns, J.W. Evaluation of sepramesh biosurgical composite in a rabbit hernia repair model. J. Surg. Res. 2000, 94, 92–98. [Google Scholar] [CrossRef]
- Baptista, M.L.; Bonsack, M.E.; Delaney, J.P. Seprafilm reduces adhesions to polypropylene mesh. Surgery 2000, 128, 86–92. [Google Scholar] [CrossRef] [PubMed]
- van’t Riet, M.; de Vos van Steenwijk, P.J.; Bonthuis, F.; Marquet, R.L.; Steyerberg, E.W.; Jeekel, J.; Bonjer, H.J. Prevention of adhesion to prosthetic mesh: Comparison of different barriers, using incisional hernia model. Ann. Surg. 2003, 237, 123–128. [Google Scholar] [CrossRef]
- Bellón, J.M.; Serrano, N.; Rodríguez, M.; García-Honduvilla, N.; Pascual, G.; Buján, J. Composite prostheses used to repair abdominal wall defects: Physical or chemical adhesion barriers? J. Biomed. Mater. Res. Part. B Appl. Biomater. 2005, 74, 718–724. [Google Scholar] [CrossRef]
- Judge, T.W.; Parker, D.M.; Dinsmore, R.C. Abdominal wall hernia repair: A comparison of sepramesh and parietex composite mesh in a rabbit hernia model. J. Am. Coll. Surg. 2007, 204, 276–281. [Google Scholar] [CrossRef]
- Bellón, J.M.; Rodríguez, M.; García-Honduvilla, N.; Pascual, G.; Gil, V.G.; Buján, J. Peritoneal effects of prosthetic meshes used to repair abdominal wall defects: Monitoring adhesions by sequential laparoscopy. J. Laparoendosc. Adv. Surg. Tech. 2007, 17, 160–166. [Google Scholar] [CrossRef]
- Rodríguez, M.; Pascual, G.; Sotomayor, S.; Pérez-Köhler, B.; Cifuentes, A.; Bellón, J.M. Chemical adhesion barriers: Do they affect the intraperitoneal behavior of a composite mesh? J. Investig. Surg. 2011, 24, 115–122. [Google Scholar] [CrossRef]
- Deeken, C.R.; Abdo, M.S.; Frisella, M.M.; Matthews, B.D. Physicomechanical evaluation of absorbable and nonabsorbable barrier composite meshes for laparoscopic ventral hernia repair. Surg. Endosc. 2010, 25, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- Deeken, C.R.; Faucher, K.M.; Matthews, B.D. A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg. Endosc. 2011, 26, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Deeken, C.R.; Matthews, B.D. Comparison of contracture, adhesion, tissue ingrowth, and histologic response characteristics of permanent and absorbable barrier meshes in a porcine model of laparoscopic ventral hernia repair. Hernia 2011, 16, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Bellón, J.M.; García-Honduvilla, N.; Serrano, N.; Rodríguez, M.; Pascual, G.; Buján, J. Composites prosthesis for the repair of abdominal wall defects: Effect of the structure of the adhesion barrier component. Hernia 2005, 9, 338–343. [Google Scholar] [CrossRef]
- Bellón, J.M.; Jurado, F.; García-Moreno, F.; Corrales, C.; Carrera-San Martín, A.; Buján, J. Healing process induced by three composite prostheses in the repair of abdominal Wall defects. J. Biomed. Mat. Res. Appl. Biomater. 2002, 63, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Bellón, J.M.; García-Honduvilla, N.; Carnicer, E.; Serrano, N.; Rodríguez, M.; Buján, J. Temporary closure of the abdomen using a new composite prosthesis (PL-PU99). Am. J. Surg. 2004, 188, 314–320. [Google Scholar] [CrossRef]
- Novitsky, Y.W.; Harrell, A.G.; Cristiano, J.A.; Paton, B.L.; Norton, H.J.; Peindl, R.D.; Kercher, K.W.; Heniford, B.T. Comparative evaluation of adhesion formation, strength of ingrowth, and textile properties of prosthetic meshes after long-term in-traabdominal implantation in a rabbit. J. Surg. Res. 2007, 140, 6–11. [Google Scholar] [CrossRef]
- Schug-Pass, C.; Sommerer, F.; Tannapfel, A.; Lippert, H.; Köckerling, F. The use of composite meshes in laparoscopic repair of abdominal wall hernias: Are there differences in biocompatibility? Experimental results obtained in a laparoscopic porcine model. Surg. Endosc. 2009, 23, 487–495. [Google Scholar] [CrossRef]
- Schreinemacher, M.H.F.; Emans, P.J.; Gijbels, M.J.J.; Greve, J.M.; Beets, G.L.; Bouvy, N.D. Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. BJS 2009, 96, 305–313. [Google Scholar] [CrossRef]
- Pierce, R.A.; Perrone, J.M.; Nimeri, A.; Sexton, J.A.; Walcutt, J.; Frisella, M.M.; Matthews, B.D. 120-Day Comparative analysis of adhesion grade and quantity, mesh contraction, and tissue response to a novel omega-3 fatty acid bioabsorbable barrier macroporous mesh after intraperitoneal placement. Surg. Innov. 2008, 16, 46–54. [Google Scholar] [CrossRef]
- Chubbak, J.A.; Sigh, R.S.; Sill, C.; Dick, L.S. Small bowel obstruction resulting from mesh plug migration after open inguinal hernia repair. Surgery 2000, 127, 475–476. [Google Scholar] [CrossRef]
- Savioz, D.; Ludwig, C.; Leissing, C.; Bolle, J.F.; Bühler, L.; Morel, P. Repeated macroscopic haematuria caused by intravesical migration of a preperitoneal prosthesis. Eur. J. Surg 1997, 163, 631–632. [Google Scholar]
- Ott, V.; Groebli, Y.; Schneider, R. Late intestinal fistula formation after incisional hernia using intraperitoneal mesh. Hernia 2004, 9, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Moussi, A.; Daldoul, S.; Bourguiba, B.; Othmani, D.; Zaouche, A. Gas gangrene of the abdominal wall due to late-onset enteric fistula after polyester mesh repair of an incisional hernia. Hernia 2012, 16, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Arnaud, J.P.; Hennekinne-Muccis, S.; Pessaux, P.; Tuech, J.J.; Aube, C. Ultrasound detection of visceral adhesion after intra-peritoneal ventral hernia treatment: A comparative study of protected versus unprotected meshes. Hernia 2003, 7, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Lermite, E.; Pessaux, P.; Tuech, J.J.; Aubé, C.; Arnaud, J.P. Visceral adhesion after intraperitoneal ventral hernia treatment: Monocentric study comparative of protected versus unprotected meshes. Ann. Chir. 2004, 129, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Balique, J.G.; Benchetrit, S.; Bouillot, J.L.; Flament, J.B.; Gouillat, C.; Jarsaillon, P.; Mantion, G.; Arnaud, J.P.; Magne, E.; Brunetti, F. Intraperitoneal treatment of incisional and umbilical hernias using an innovative composite mesh: Four-year results of a prospective multicenter clinical trial. Hernia 2004, 9, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Egea, A.; Bustos, J.A.C.; Girela, E.; Aguayo-Albasini, J.L. Long-term results of laparoscopic repair of incisional hernias using an intraperitoneal composite mesh. Surg. Endosc. 2009, 24, 359–365. [Google Scholar] [CrossRef]
- Chelala, E.; Debardemaeker, Y.; Éliás, B.; Charara, F.; Dessily, M.; Allé, J.-L. Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: Adhesion and recurrence analysis. Hernia 2010, 14, 123–129. [Google Scholar] [CrossRef]
- Pascual, G.; Sotomayor, S.; Rodríguez, M.; Bayon, Y.; Bellón, J.M. Behaviour of a new composite mesh for the repair of full-thickness abdominal wall defects in a rabbit model. PLoS ONE 2013, 8, e80647. [Google Scholar] [CrossRef] [Green Version]
- Deeken, C.R.; Brent, D. Characterization of the mechanical strength, resorption properties, and histologic characteristics of a fully absorbable material (Poly-4-hydroxybutyrate-PHASIX mesh) in a porcine model of hernia repair. ISRN Surg. 2013, 2013, 1–12. [Google Scholar] [CrossRef]
- Scott, J.R.; Deeken, C.R.; Martindale, R.G.; Rosen, M.J. Evaluation of a fully absorbable poly-4-hydroxibutyrate/absorbable barrier composite mesh in a porcine model of ventral hernia repair. Surg. Endosc. 2016, 30, 3691–3701. [Google Scholar] [CrossRef] [Green Version]
- Pascual, G.; Benito-Martínez, S.; Rodríguez, M.; Pérez-Köhler, B.; García-Moreno, F.; Bellón, J.M. Behaviour at the peritoneal interface of next-generation prosthetic materials for hernia repair. Surg. Endosc. 2021, 1–12. [Google Scholar] [CrossRef]
- Bittner, J.G.; El-Hayek, K.; Strong, A.T.; La Pinska, M.P.; Yoo, J.S.; Pauli, E.C.; Kroh, M. First human use of hybrid synthetic/biologic mesh in ventral hernia repair: A multicenter trial. Surg Endosc. 2018, 32, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- GORE BIO-A Product Brochure. Available online: http://www.goremedical.com/resources/dam/assets/AQ3037-EN2.pdf (accessed on 12 February 2011).
- Pascual, G.; Sotomayor, S.; Rodríguez, M.; Pérez-Köhler, B.; Bellón, J.M. Repair of abdominal wall defects with biodegradable laminar prostheses: Polymeric or biological? PLoS ONE 2012, 7, e52628. [Google Scholar] [CrossRef] [Green Version]
- Symeonidis, D.; Efthimiou, M.; Koukoulis, G.; Athanasiou, E.; Mamaloudis, I.; Tzovaras, G. Open inguinal hernia repair with the use of polyglycolic acid/trimethylene carbonate absorbable mesh: A critical update of the long-term results. Hernia 2012, 17, 85–87. [Google Scholar] [CrossRef]
- TIGR (R) Matrix Long-Term Resorbable Mesh. Novus World. Available online: http://novusscientific.com/us/products/tigr-matrix (accessed on 23 August 2018).
- Hjort, H.; Mathisen, T.; Alves, A.; Clermont, G.; Boutrand, J.P. Three-year results from a preclinical implantation study of a long-term resorbable surgical mesh with time-dependent mechanical characteristics. Hernia 2011, 16, 191–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruiz-Jasbon, F.; Norrby, J.; Ivarsson, M.L.; Bjork, S. Inguinal hernia repair using a synthetic long-term resorbable mesh: Results from a 3-year prospective safety and performance study. Hernia 2014, 18, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Bard, D. Phaxis TM Mesh Fully Resorbable Scaffold for Hernia Repair. Available online: https://www.bd.com/assets/documents/pdh/initial/Phasix-Brochure-with-LX.pdf (accessed on 23 March 2021).
- Martin, D.P.; Williams, S.F. Medical applications of poly-4-hydroxybutirate: A strong flexible absorbable biomaterial. Bioch. Eng. J. 2003, 16, 97–105. [Google Scholar] [CrossRef]
- Williams, S.F.; Rizk, S.; Martin, D.P. Poly-4-hydroxybutyrate (P4HB): A new generation of resorbable medical devices for tissue repair and regeneration. Biomed. Eng. Biomed. Tech. 2013, 58, 439–452. [Google Scholar] [CrossRef]
- Miserez, M.; Jairam, A.P.; Boersema, G.S.; Bayon, Y.; Jeekel, J.; Lange, J.F. Resorbable synthetic meshes for abdominal wall defects in preclinical setting: A literature review. J. Surg. Res. 2019, 237, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Pascual, G.; Rodríguez, M.; Pérez-Köhler, B.; Benito-Martínez, S.; Calvo, B.; García-Moreno, F.; Bellón, J.M. Long-term comparative evaluation of two types of absorbable meshes in partial abdominal wall defects: An experimental study in rabbits. Hernia 2020, 24, 1159–1173. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.P.; Badhwar, A.; Shah, D.V.; Rizk, S.; Eldridge, S.N.; Gagne, D.H.; Ganatra, A.; Darois, R.E.; Williams, S.F.; Tai, H.-C.; et al. Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J. Surg. Res. 2013, 184, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Plymale, M.A.; Davenport, D.L.; Dugan, A.; Zachem, A.; Roth, J.S. Ventral hernia repair with poly-4-hydroxybutyrate mesh. Surg. Endosc. 2018, 32, 1689–1694. [Google Scholar] [CrossRef]
- Roth, J.S.; Anthone, G.J.; Selzer, D.J.; Poulose, B.K.; Bittner, J.G.; Hope, W.H.; Dunn, R.M.; Martindale, R.G.; Goldblatt, M.I.; Earle, D.B.; et al. Prospective evaluation of poly-4-hydroxybutyrate mesh in CDC class I/high-risk ventral and incisional hernia repair: 18 month follow-up. Surg. Endosc. 2018, 32, 1929–1936. [Google Scholar] [CrossRef]

| Type of Mesh | Modifications | Advantages | Limitations | References | |
|---|---|---|---|---|---|
| Polyester (PO) | Standard mesh (Dacron®, Mersilene®) | Good and lasting mechanical strength | Adhesion formation Foreign body reaction | [13,14,15] | |
| Polypropylene (PP) | Standard mesh (Marlex®, Prolene®, Surgipro®) | Low recurrence rates Flexible and easily inserted Good mechanical resistance | High adhesion formation Disorganized neoperitoneum | [16,17,18,19,20,21,22,23,24,25,26,27,64,65,75] | |
| Structural modifications | Increased pore size Smaller knots Fine filaments Lower density (ParieteneTM, Optilene®) | Improved integration and compliance Reduction of foreign material Reduction of inflammation and fibrosis Reduction of bridging effect | Adhesion formation | [50,51,52,53,54,55,56,69,70,72,73,74] | |
| Introduction of a second component | Absorbable filaments (Vypro®, Ultrapro®) | Reduced foreign material | Adhesion formation | [57,71] | |
| Inert filaments: PVDF (Dynamesh®) | Diminished inflammatory response Resistance to degradation | Controversial results among experiments Adhesion formation | [93,94,95,96,97,98,99,100,101,102,103] | ||
| Mesh coating: titanium (TiMESH®) | Improved biocompatibility Diminished foreign body reaction | [58,77,78,79,80,81,102] | |||
| Self-gripping | PLA hooks (Progrip®) Adhesive (LifemeshTM, Adhesix®) | Results comparable to sutured meses (Progrip®) Avoidance of the trauma caused by sutures or tacks | Mesh dislocated (onlay procedures) | [88,89,90,91,92] | |
| Polytetrafluoroethylene (PTFE) | Expanded PTFE, laminar structure | Standard material (Soft Tissue Patch®) | Good biological tolerance Low incidence of adhesions Adequate neoperitoneum | Deficient tissue incorporation Reduced mechanical strength (vs. PP) Encapsulation Scarce angiogenesis | [30,31,32,33,34,35,36,37,38,39,40,41,42,43,59,64,65,66,67,68,75] |
| Introduction of evenly spaced large pores (Mycro Mesh®) | More rapid tissue incorporation | Not mentioned | [44,60] | ||
| Non-porous side and standard microporous surface (DualMesh®) | Adhesion prevention Good tissue ingrowth at microporous/rougher surface | Poor tissue integration at nonporous surface | [45,46,75] | ||
| Rougher surface (Dual Mesh Corduroy®) | |||||
| Pretreatment with antibacterial agent (Dual Mesh Plus®) | Reduced adherence of bacteria | Not mentioned | [46] | ||
| PTFE, reticular structure (Infinit Mesh®) | Improved tissue incorporation Improved mechanical strength (vs. PTFE) | Adhesion formation High elastic modulus | [47,48,49,62] | ||
| Condensed PTFE (MotifMESH®) | Reduced adhesion formation Minimal bacterial adherence | Adhesions on raised edges | [104,105,106,107] | ||
| Type of Mesh | Modifications | Advantages | Limitations | References | |
|---|---|---|---|---|---|
| Classic composite materials | Tissue integrating component | Reticular non absorbable mesh (PP, PO) | Good host tissue ingrowth Good mechanical strength Adequate behaviour at the peritoneal interface Reduced inflammatory reaction | Foreign material in the recipient | [108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142] |
| Visceral component | Physical barrier (non absorbable): PTFE (Composix®) PU (PL-PU99®) | ||||
| Chemical barrier (absorbable): PEG (Parietex CompositeTM) hy (SeprameshTM) pd + cellulose (ProceedTM) | |||||
| Last generation composites | Tissue integrating component | Partially or totally absorbable mesh: PP+PGA (Ventraligth TM ST) P4H (Phasix TM ST) Non absorbable mesh: PO (SymbotexTM) PP (PhysiomeshTM) | Same as classic composites Reduced foreign material in the recipient | Not mentioned | [143,144,145,146,147] |
| Visceral component | Chemical barrier (absorbable): pd hydrogel (VentraligthTM) Collagen+chitosan (SymbotexTM) Polyglecaprone 25 (PhysiomeshTM) PGA hydrogel (Phasix TM ST) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez, M.; Gómez-Gil, V.; Pérez-Köhler, B.; Pascual, G.; Bellón, J.M. Polymer Hernia Repair Materials: Adapting to Patient Needs and Surgical Techniques. Materials 2021, 14, 2790. https://doi.org/10.3390/ma14112790
Rodríguez M, Gómez-Gil V, Pérez-Köhler B, Pascual G, Bellón JM. Polymer Hernia Repair Materials: Adapting to Patient Needs and Surgical Techniques. Materials. 2021; 14(11):2790. https://doi.org/10.3390/ma14112790
Chicago/Turabian StyleRodríguez, Marta, Verónica Gómez-Gil, Bárbara Pérez-Köhler, Gemma Pascual, and Juan Manuel Bellón. 2021. "Polymer Hernia Repair Materials: Adapting to Patient Needs and Surgical Techniques" Materials 14, no. 11: 2790. https://doi.org/10.3390/ma14112790
APA StyleRodríguez, M., Gómez-Gil, V., Pérez-Köhler, B., Pascual, G., & Bellón, J. M. (2021). Polymer Hernia Repair Materials: Adapting to Patient Needs and Surgical Techniques. Materials, 14(11), 2790. https://doi.org/10.3390/ma14112790








