Description of a Digital Work-Flow for CBCT-Guided Construction of Micro-Implant Supported Maxillary Skeletal Expander
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient’s Clinical Characteristics
Clinical Assessment of Palatal Morphology
2.2. Digital Work-Flow
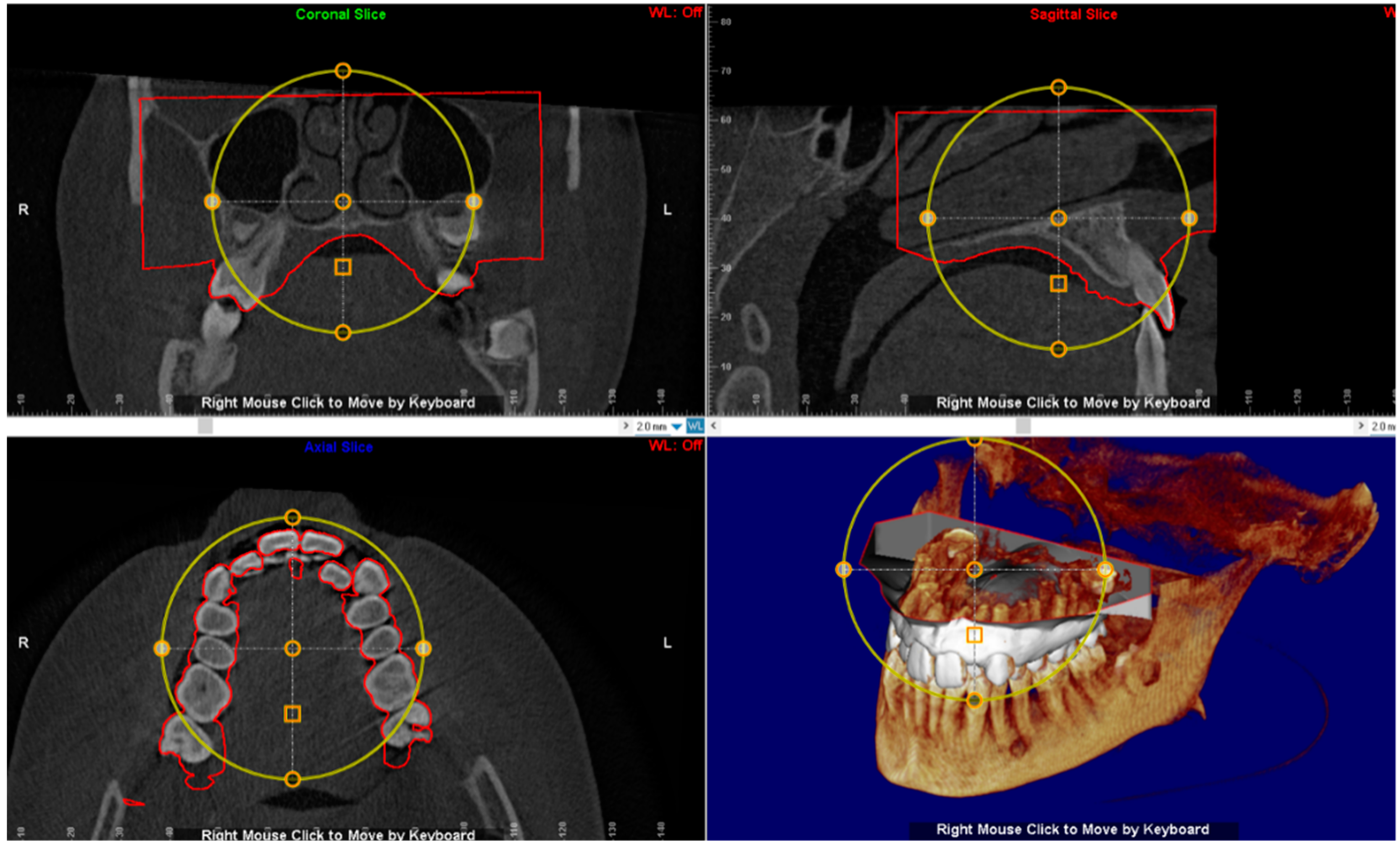
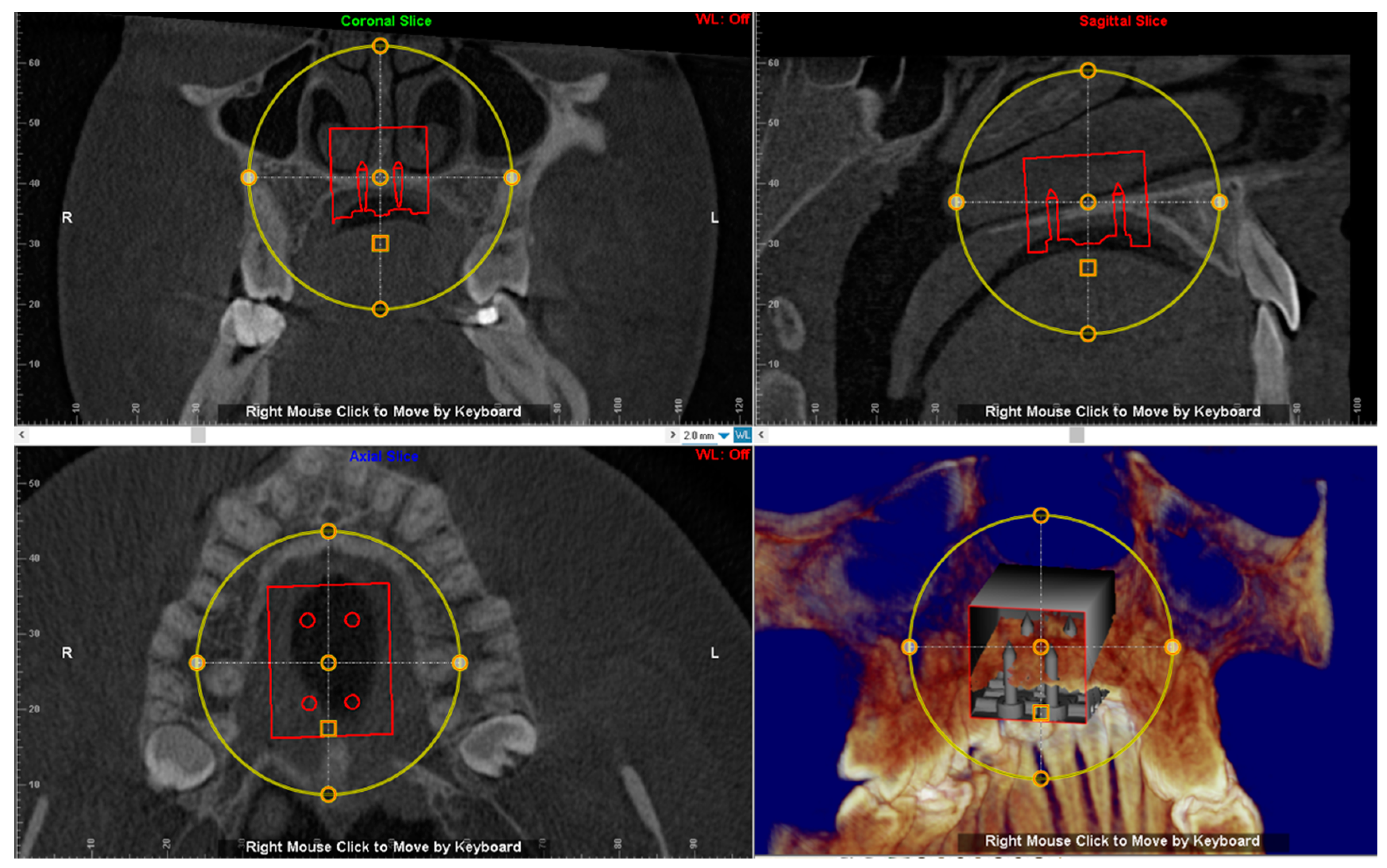
2.3. CBCT Examination
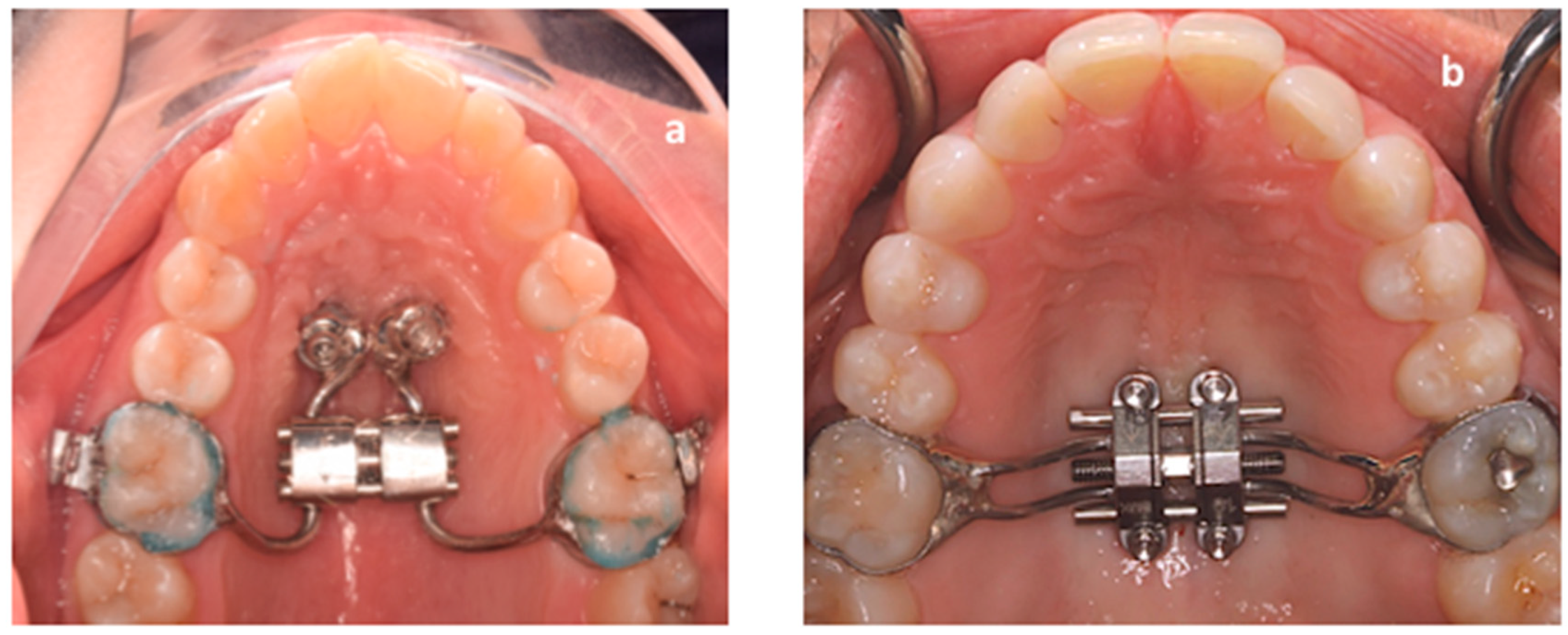
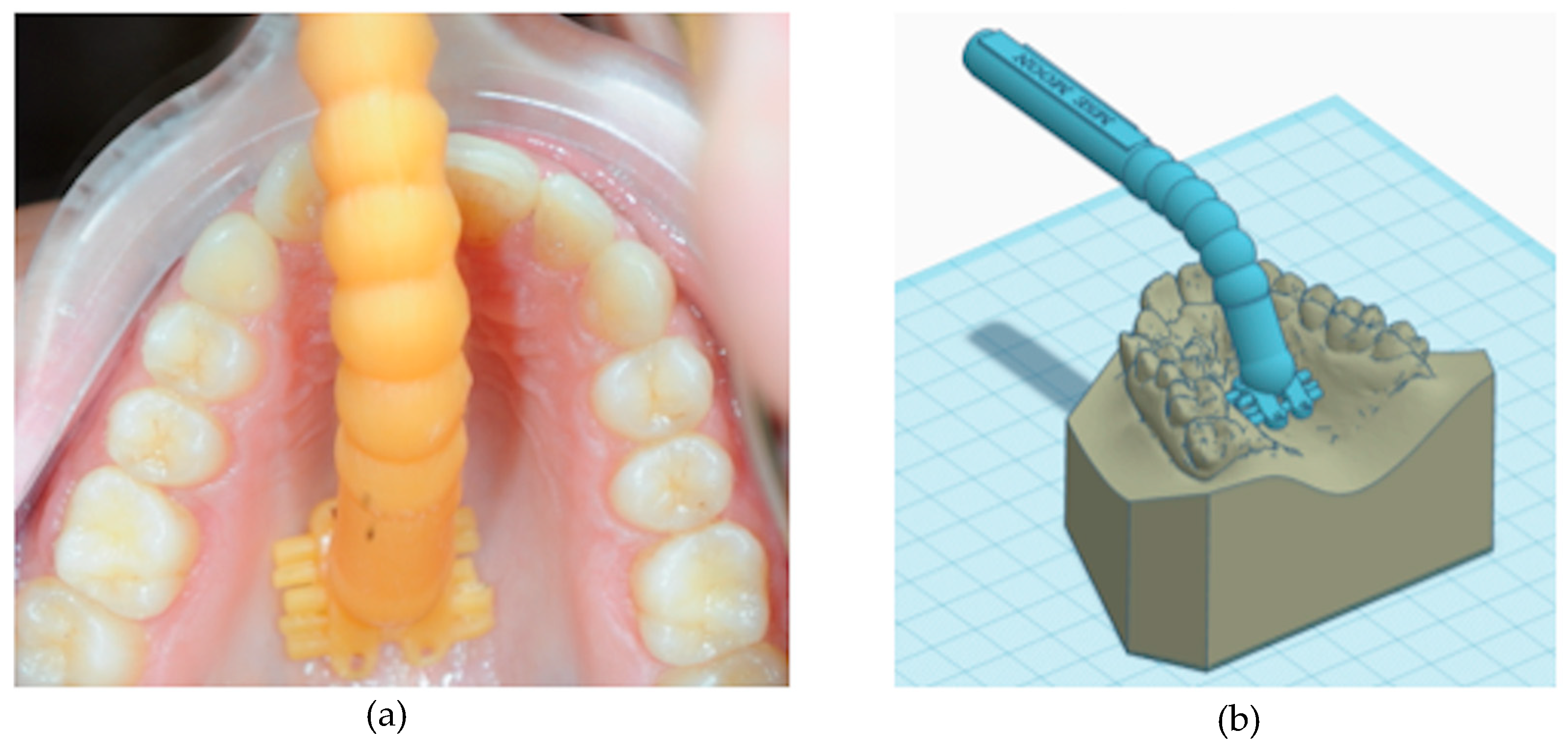
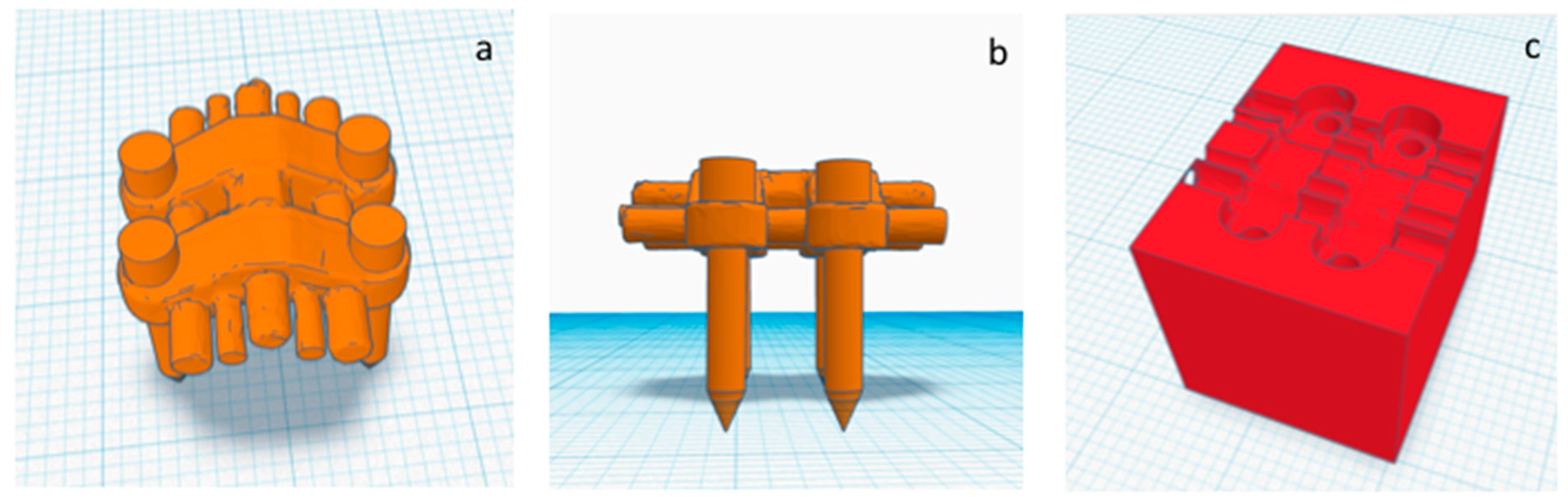
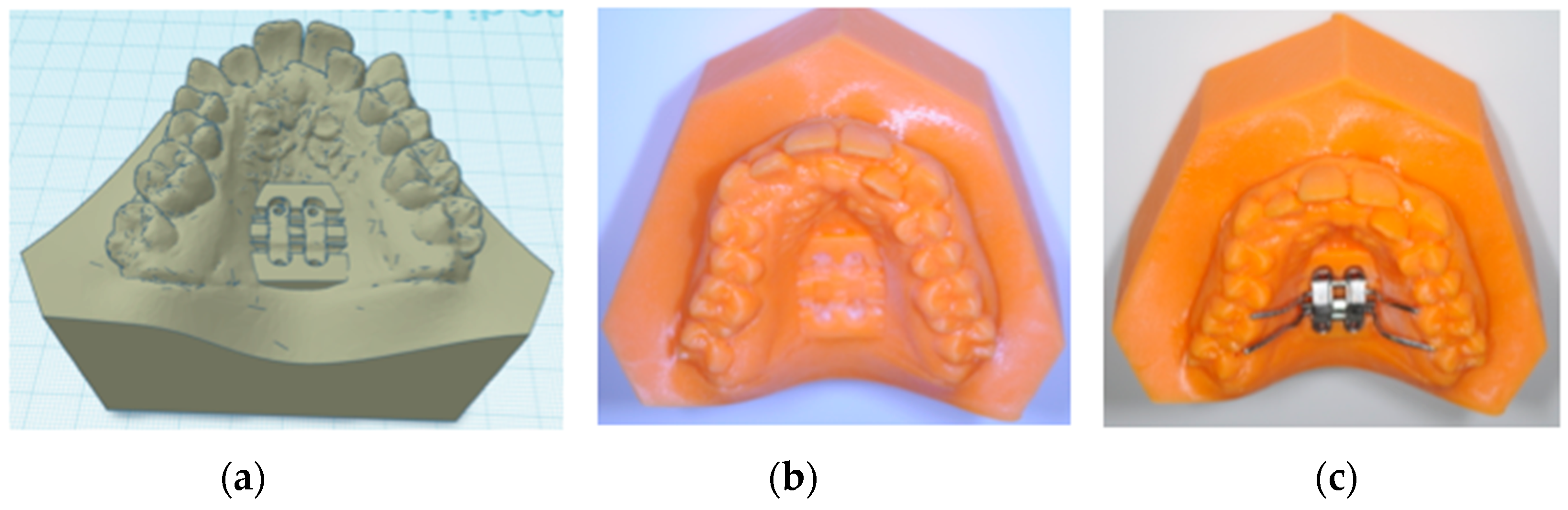
2.4. Construction of Positional Template of the MSE
2.5. Virtual Placement of MSE (Negative Template) and Construction of the Final Lab Template
3. Case Report
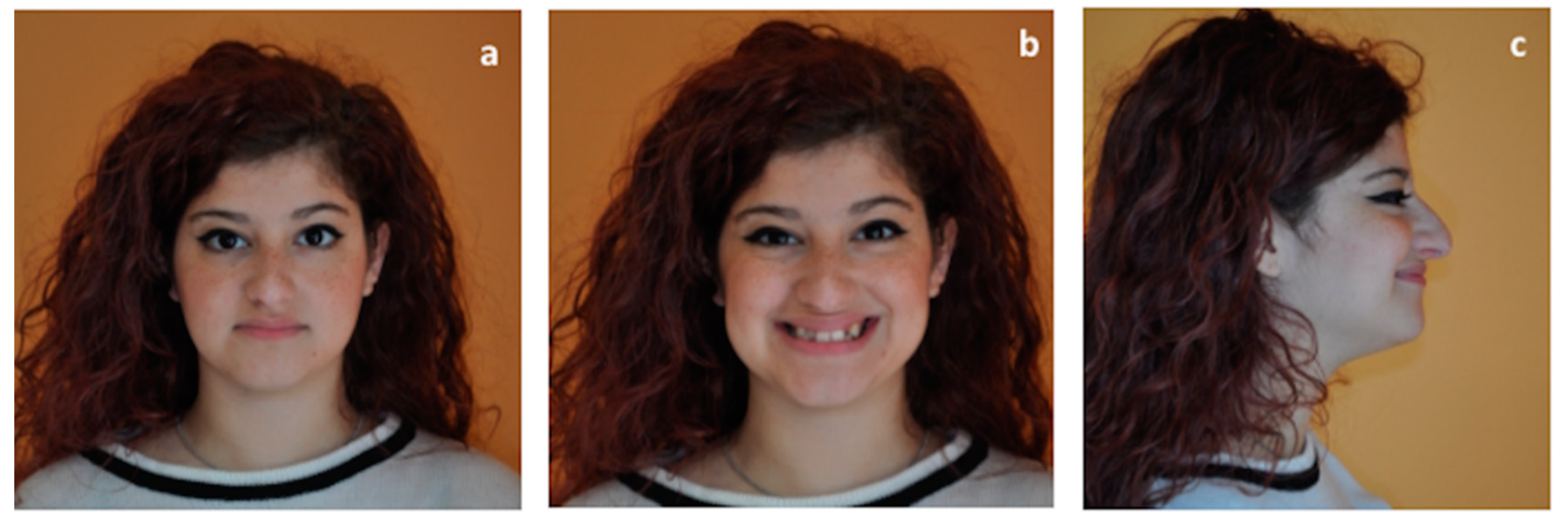
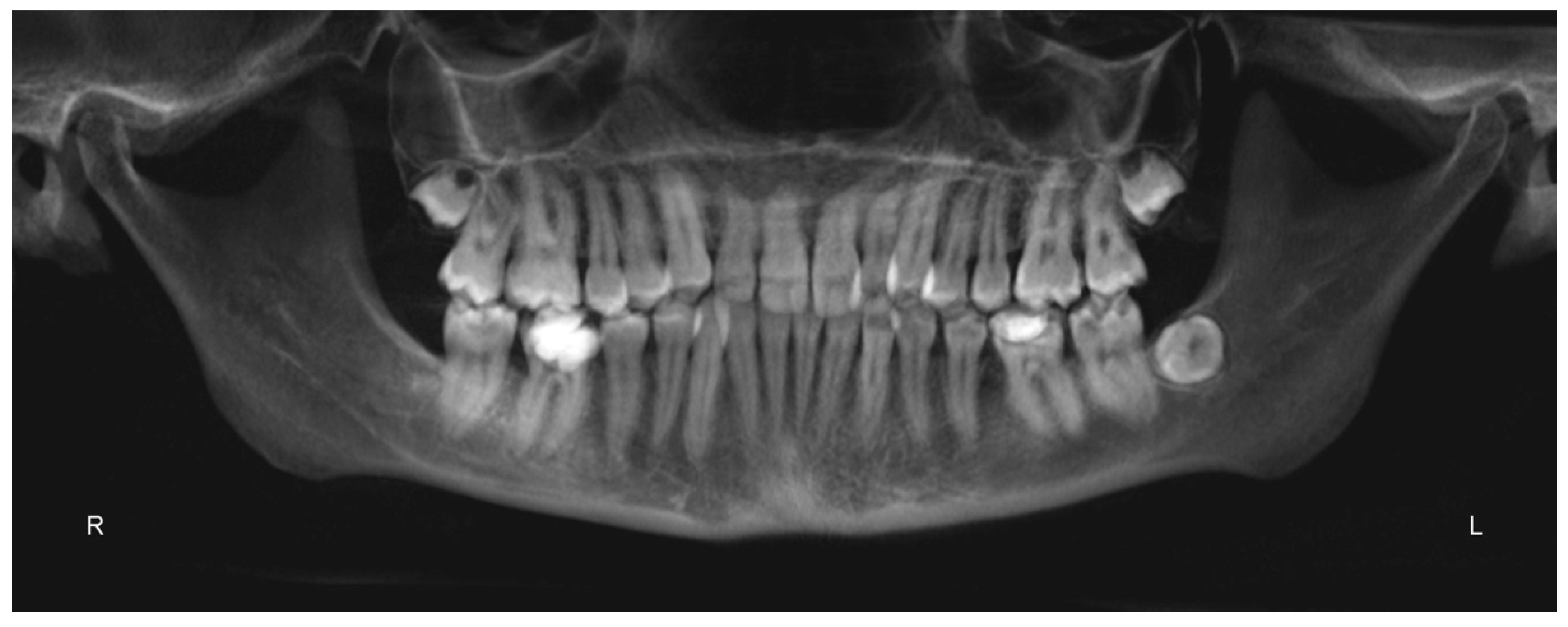
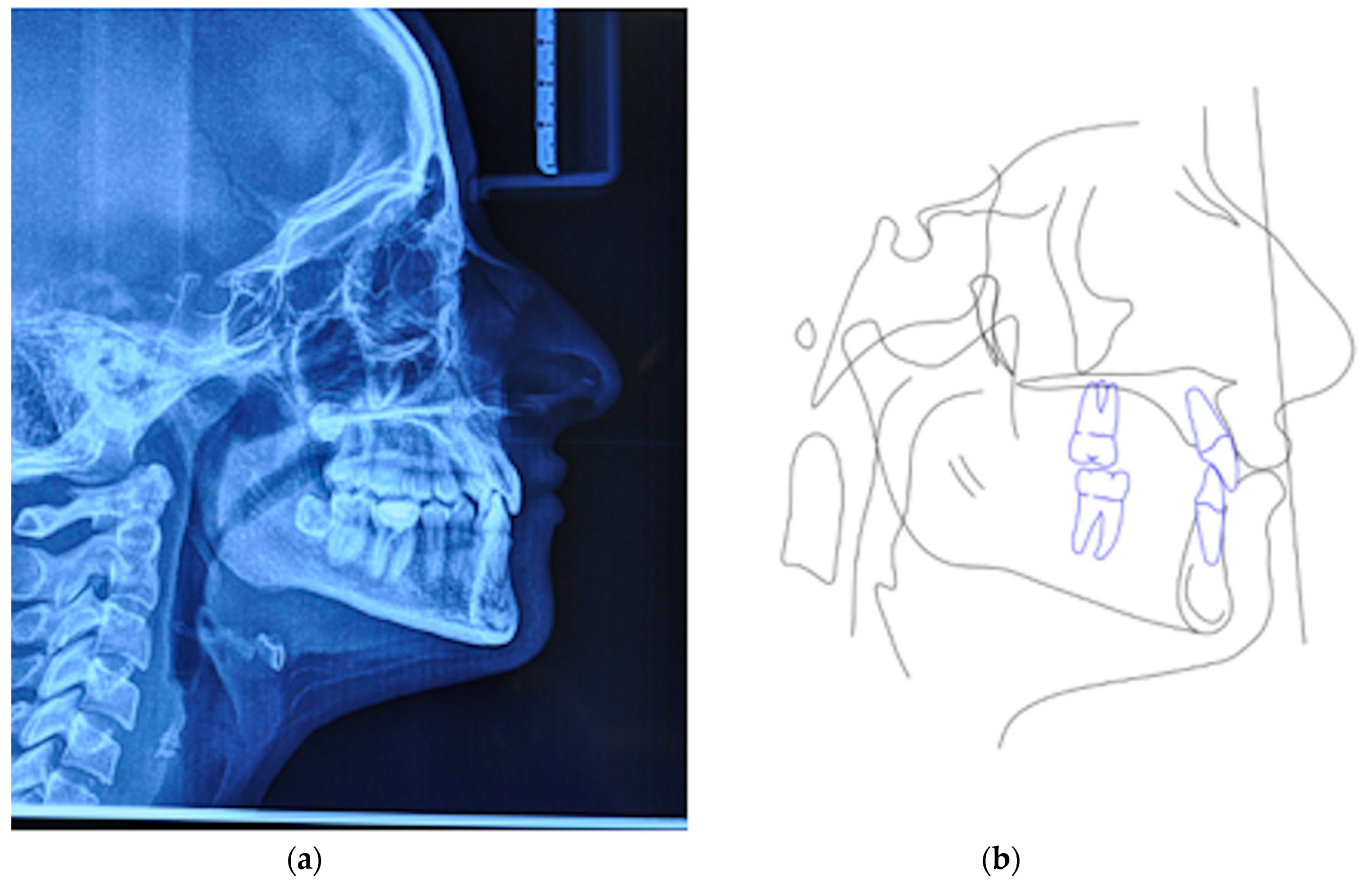
3.1. Diagnosis and Treatment Plan
3.2. Digital Workflow for Planning MSE Device
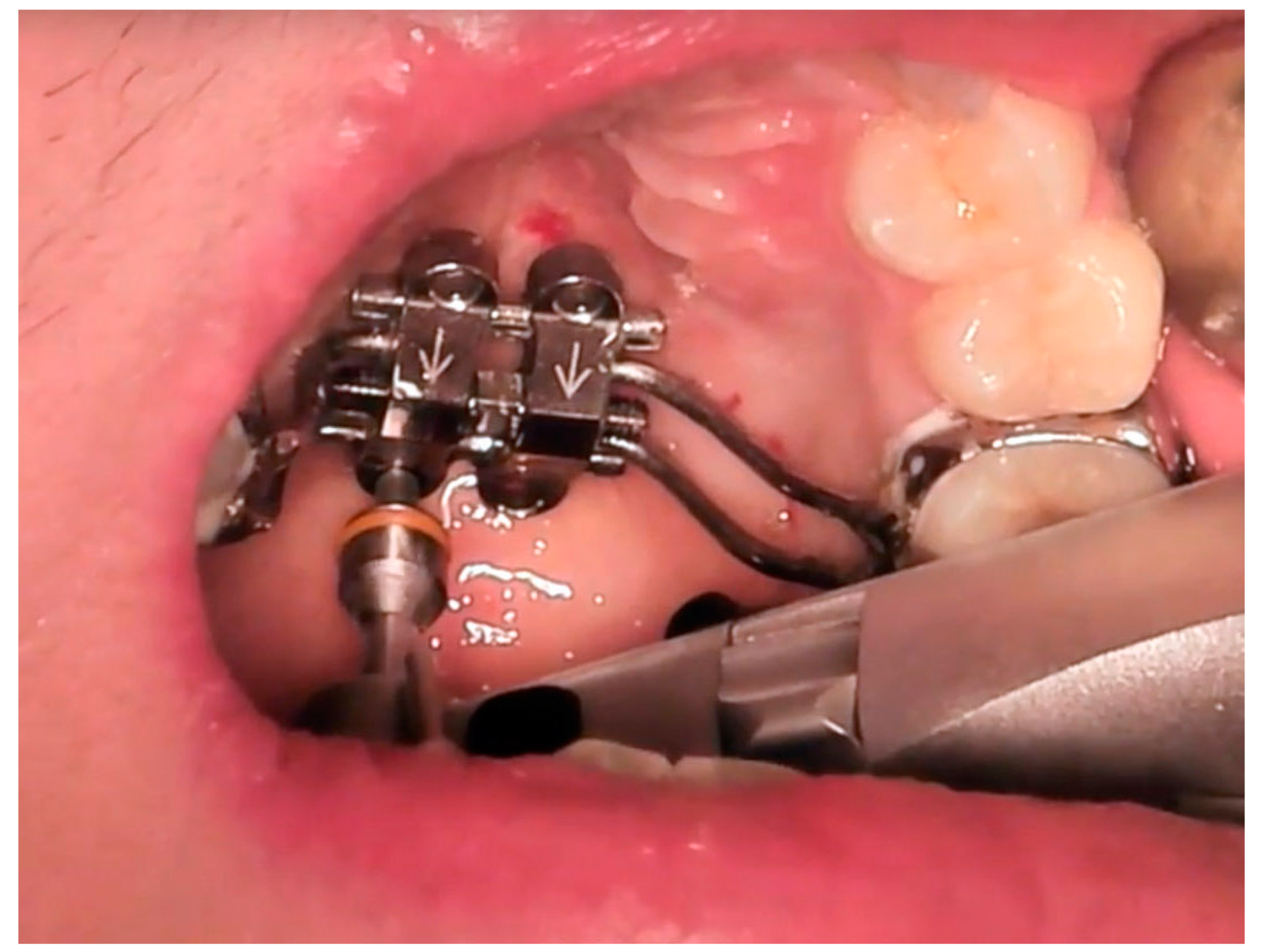
3.3. MSE and Miniscrews Insertion
3.4. Treatment Progress
4. Discussion
- (1)
- predictable placement of the MSE appliance, according to the patient’s anatomical characteristics
- (2)
- the construction of a negative positional template of the MSE that allows lab technicians to construct the device in a reliable and accurate position, according to the virtual project planned by the orthodontist.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lo Giudice, A.; Barbato, E.; Cosentino, L.; Ferraro, C.M.; Leonardi, R. Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur. J. Orthod. 2018, 40, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Bucci, R.; D’Anto, V.; Rongo, R.; Valletta, R.; Martina, R.; Michelotti, A. Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and meta-analyses. J. Oral. Rehabil. 2016, 43, 543–564. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Long, H.; Ye, N.; Xue, J.; Yang, X.; Liao, L.; Lai, W. The effectiveness of non-surgical maxillary expansion: A meta-analysis. Eur. J. Orthod. 2014, 36, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Fastuca, R.; Portelli, M.; Militi, A.; Bellocchio, M.; Spinuzza, P.; Briguglio, F.; Caprioglio, A.; Nucera, R. Effects of rapid vs slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur. J. Paediatr. Dent. 2017, 18, 299–304. [Google Scholar]
- Garib, D.G.; Henriques, J.F.; Janson, G.; de Freitas, M.R.; Fernandes, A.Y. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 749–758. [Google Scholar] [CrossRef]
- Sun, Z.; Hueni, S.; Tee, B.C.; Kim, H. Mechanical strain at alveolar bone and circummaxillary sutures during acute rapid palatal expansion. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e219–e228. [Google Scholar] [CrossRef]
- Baysal, A.; Karadede, I.; Hekimoglu, S.; Ucar, F.; Ozer, T.; Veli, I. Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2012, 82, 488–494. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Galletti, C.; Gay-Escoda, C.; Leonardi, R. CBCT assessment of radicular volume loss after rapid maxillary expansion: A systematic review. J. Clin. Exp. Dent. 2018, 10, e484–e494. [Google Scholar] [CrossRef]
- Park, J.J.; Park, Y.C.; Lee, K.J.; Cha, J.Y.; Tahk, J.H.; Choi, Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J. Orthod. 2017, 47, 77–86. [Google Scholar] [CrossRef]
- Kavand, G.; Lagravère, M.; Kula, K.; Stewart, K.; Ghoneima, A. Retrospective CBCT analysis of airway volume changes after bone-borne vs tooth-borne rapid maxillary expansion. Angle Orthod. 2019, 89, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.W.; Kim, M.J.; Ahn, H.W.; Kim, S.J.; Kim, S.H.; Chung, K.R.; Nelson, G. Molar inclination and surrounding alveolar bone change relative to the design of bone-borne maxillary expanders: A CBCT study. Angle Orthod. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Ahn, H.W.; Kim, S.J.; Moon, S.C.; Kim, S.H.; Nelson, G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015, 85, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Holm, M.; Jost-Brinkmann, P.G.; Mah, J.; Bumann, A. Bone thickness of the anterior palate for orthodontic miniscrews. Angle Orthod. 2016, 86, 826–831. [Google Scholar] [CrossRef]
- Krusi, M.; Eliades, T.; Papageorgiou, S.N. Are there benefits from using bone-borne maxillary expansion instead of tooth-borne maxillary expansion? A systematic review with meta-analysis. Prog. Orthod. 2019, 20, 9. [Google Scholar] [CrossRef]
- Celenk-Koca, T.; Erdinc, A.E.; Hazar, S.; Harris, L.; English, J.D.; Akyalcin, S. Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: A prospective randomized clinical trial. Angle Orthod. 2018, 88, 702–709. [Google Scholar] [CrossRef]
- Gracco, A.; Lombardo, L.; Cozzani, M.; Siciliani, G. Quantitative cone-beam computed tomography evaluation of palatal bone thickness for orthodontic miniscrew placement. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 361–369. [Google Scholar] [CrossRef]
- Winsauer, H.; Vlachojannis, C.; Bumann, A.; Vlachojannis, J.; Chrubasik, S. Paramedian vertical palatal bone height for mini-implant insertion: A systematic review. Eur. J. Orthod. 2014, 36, 541–549. [Google Scholar] [CrossRef]
- Ludwig, B.; Glasl, B.; Bowman, S.J.; Wilmes, B.; Kinzinger, G.S.; Lisson, J.A. Anatomical guidelines for miniscrew insertion: Palatal sites. J. Clin. Orthod. 2011, 45, 433–441. [Google Scholar]
- Maequezan, M.; Nojima, L.I.; Ayres de Freitas, A.O.; Baratieri, C.; Junior, M.A.; Nojima, M. Tomographic mapping of the hard palate and overlying mucosa. Braz. Oral Res. 2012, 26, 36–42. [Google Scholar] [CrossRef]
- Nucera, R.; Lo Giudice, A.; Bellocchio, A.M.; Spinuzza, P.; Caprioglio, A.; Perillo, L.; Matarese, G.; Cordasco, G. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. Angle Orthod. 2017, 87, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Kitai, N.; Yasuda, Y.; Takada, K. A stent fabricated on a selectively colored stereo lithographic model for placement of orthodontic miniimplants. Int. J. Adult Orthod. Orthognath. Surg. 2002, 17, 264–266. [Google Scholar]
- Cantarella, D.; Savio, G.; Grigolato, L.; Zanata, P.; Berveglieri, C.; Lo Giudice, A.; Isola, G.; Del Fabbro, M.; Moon, W. A new methodology for the digital planning of micro-implant-supported maxillary skeletal expansion. Med. Devices Evid. Res. 2020, 13, 93–106. [Google Scholar] [CrossRef]
- Brunetto, D.P.; Sant’Anna, E.F.; Machado, A.W.; Moon, W. Non-surgical treatment of transverse deficiency in adults using Microimplant-assisted Rapid Palatal Expansion (MARPE). Dent. Press J. Orthod. 2017, 22, 110–125. [Google Scholar] [CrossRef] [PubMed]
- Loubele, M.; Bogaerts, R.; Van Dijck, E.; Pauwels, R.; Vanheusden, S.; Suetens, P.; Marchal, G.; Sanderink, G.; Jacobs, R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur. J. Radiol. 2009, 71, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Lo Giudice, A.; Bellocchio, M.; Spinuzza, P.; Caprioglio, A.; Cordasco, G. Diagnostic concordance between skeletal cephalometrics, radiograph-based soft-tissue cephalometrics, and photograph-based soft-tissue cephalometrics. Eur. J. Orthod. 2017, 39, 352–357. [Google Scholar] [CrossRef]
- Cordasco, G.; Portelli, M.; Militi, A.; Nucera, R.; Lo Giudice, A.; Gatto, E.; Lucchese, A. Low-dose protocol of the spiral CT in orthodontics: Comparative evaluation of entrance skin dose with traditional X-ray techniques. Prog. Orthod. 2013, 14, 24. [Google Scholar] [CrossRef]
- Caccianiga, G.; Lo Giudice, A.; Paiusco, A.; Portelli, M.; Militi, A.; Baldoni, M.; Nucera, R. Maxillary Orthodontic Expansion Assisted by Unilateral Alveolar Corticotomy and Low-Level Laser Therapy: A Novel Approach for Correction of a Posterior Unilateral Cross-Bite in Adults. J. Lasers Med. Sci. 2019, 10, 225–229. [Google Scholar] [CrossRef]
- Isola, G.; Anastasi, GP.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef]
- Isola, G.; Perillo, L.; Migliorati, M.; Matarese, M.; Dalessandri, D.; Grassia, V.; Alibrandi, A.; Matarese, G. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur. J. Orthod. 2019, 41, 117–124. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Rustico, L.; Caprioglio, A.; Migliorati, M.; Nucera, R. Evaluation of condylar cortical bone thickness in patient groups with different vertical facial dimensions using cone-beam computed tomography. Odontology 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of vitamin d in patients with periodontal and cardiovascular disease: A cross-sectional study. J. Periodontal Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 concentrations in individuals with periodontitis. Sci. Rep. 2020, 10, 1652. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Moon, W.; Previdente, L.H.; Suzuki, S.S.; Garcez, A.S.; Consolaro, A. Miniscrew-assisted rapid palatal expander (MARPE): The quest for pure orthopedic movement. Dent. Press J. Orthod. 2016, 21, 17–23. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of Salivary and Serum Malondialdehyde and Lipid Profile of Patients with Periodontitis and Coronary Heart Disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Giudice, A.L.; Polizzi, A.; Alibrandi, A.; Patini, R.; Ferlito, S. Periodontitis and Tooth Loss Have Negative Systemic Impact on Circulating Progenitor Cell Levels: A Clinical Study. Genes (Basel). 2019, 10, E1022. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Alibrandi, A.; Dalessandri, D.; Migliorati, M.; Pedullà, E.; Rapisarda, E. Comparison of Effectiveness of Etoricoxib and Diclofenac on Pain and Perioperative Sequelae After Surgical Avulsion of Mandibular Third Molars: A Randomized, Controlled, Clinical Trial. Clin. J. Pain. 2019, 35, 908–915. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Muraglie, S.; Leonardi, R.; Lo Giudice, A. Assessment of Vitamin C and Antioxidant Profiles in Saliva and Serum in Patients with Periodontitis and Ischemic Heart Disease. Nutrients. 2019, 11, E2956. [Google Scholar] [CrossRef]
- Bourassa, C.; Hosei, Y.K.; Pollmann, S.I.; Galil, K.; Bohay, R.N.; Holdsworth, D.W.; Tassi, A. In-vitro comparison of different palatal sites for orthodontic miniscrew insertion: Effect of bone quality and quantity on primary stability. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 809–819. [Google Scholar] [CrossRef]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Giudice, A.; Quinzi, V.; Ronsivalle, V.; Martina, S.; Bennici, O.; Isola, G. Description of a Digital Work-Flow for CBCT-Guided Construction of Micro-Implant Supported Maxillary Skeletal Expander. Materials 2020, 13, 1815. https://doi.org/10.3390/ma13081815
Lo Giudice A, Quinzi V, Ronsivalle V, Martina S, Bennici O, Isola G. Description of a Digital Work-Flow for CBCT-Guided Construction of Micro-Implant Supported Maxillary Skeletal Expander. Materials. 2020; 13(8):1815. https://doi.org/10.3390/ma13081815
Chicago/Turabian StyleLo Giudice, Antonino, Vincenzo Quinzi, Vincenzo Ronsivalle, Stefano Martina, Orazio Bennici, and Gaetano Isola. 2020. "Description of a Digital Work-Flow for CBCT-Guided Construction of Micro-Implant Supported Maxillary Skeletal Expander" Materials 13, no. 8: 1815. https://doi.org/10.3390/ma13081815
APA StyleLo Giudice, A., Quinzi, V., Ronsivalle, V., Martina, S., Bennici, O., & Isola, G. (2020). Description of a Digital Work-Flow for CBCT-Guided Construction of Micro-Implant Supported Maxillary Skeletal Expander. Materials, 13(8), 1815. https://doi.org/10.3390/ma13081815







