Marginal Leakage of Endodontic Temporary Restorative Materials around Access Cavities Prepared with Pre-Endodontic Composite Build-Up: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre-Endodontic Composite Build-Up
2.2. Intracanal Irrigation
2.3. Temporary Restoration
- Hydraulic temporary restorative material (Caviton EX, GC, Tokyo, Japan): an appropriate amount of material was collected with a dental plastic filling instrument, pressed into the access cavity, and hardened with a wet cotton ball.
- Temporary stopping material (Temporary Stopping, GC, Tokyo, Japan): a temporary stopping material was inserted into a stopping carrier (YDM, Tokyo, Japan). The carrier was heated with a gas burner, and the softened temporary stopping material was inserted into the access cavity and pressure-welded with a dental plastic filling instrument.
- Zinc oxide eugenol cement (Neodyne-α, Neo Dental Chemical Products, Tokyo, Japan): powder and liquid was mixed using a mixing pad and a stainless steel spatula under the recommended powder-to-liquid ratio, and filled into the access cavity using a C-R syringe Mark II (Centrix, Shelton, CT, USA). A polyester matrix strip (GC, Tokyo, Japan) was placed on the top and finger pressure was applied.
- Glass-ionomer cement (Shofu Base Cement [White], Shofu, Kyoto, Japan): powder and liquid was mixed using a mixing pad and a stainless plastic spatula under the recommended powder-to-liquid ratio, and filled into the access cavity using a C-R syringe. A polyester matrix strip was placed on top and finger pressure was applied. After initial curing, protective varnish (GC Fuji Varnish, GC, Tokyo, Japan) was applied to the surface of the applied cement.
- Light-cured resin-based temporary filling material (Evadyne Plus, Neo Dental Chemical Products, Tokyo, Japan): a dedicated tip was attached to a syringe, and the material was inserted directly into the access cavity. After a polyester matrix strip was placed, finger pressure was applied to the filled material, and the coronal surface was light-cured using an LED light-curing unit (Demi Plus, Kerr, Orange, CA, USA). Light-curing was applied for 20 s from each of the two lateral areas for a total of 60 s.
- Self-cured resin-based temporary filling material (Nishika Plast Seal Quick, Japan Dental Pharmaceutical Manufacturing, Shimonoseki, Japan): a mixture of powder and liquid was placed in the access cavity using a brush-on-technique. A polyester matrix strip was applied with finger pressure until completion of the hardening.
2.4. Thermocycling and Dye Penetration
2.5. Measurement of Linear Dye Penetration
3. Results
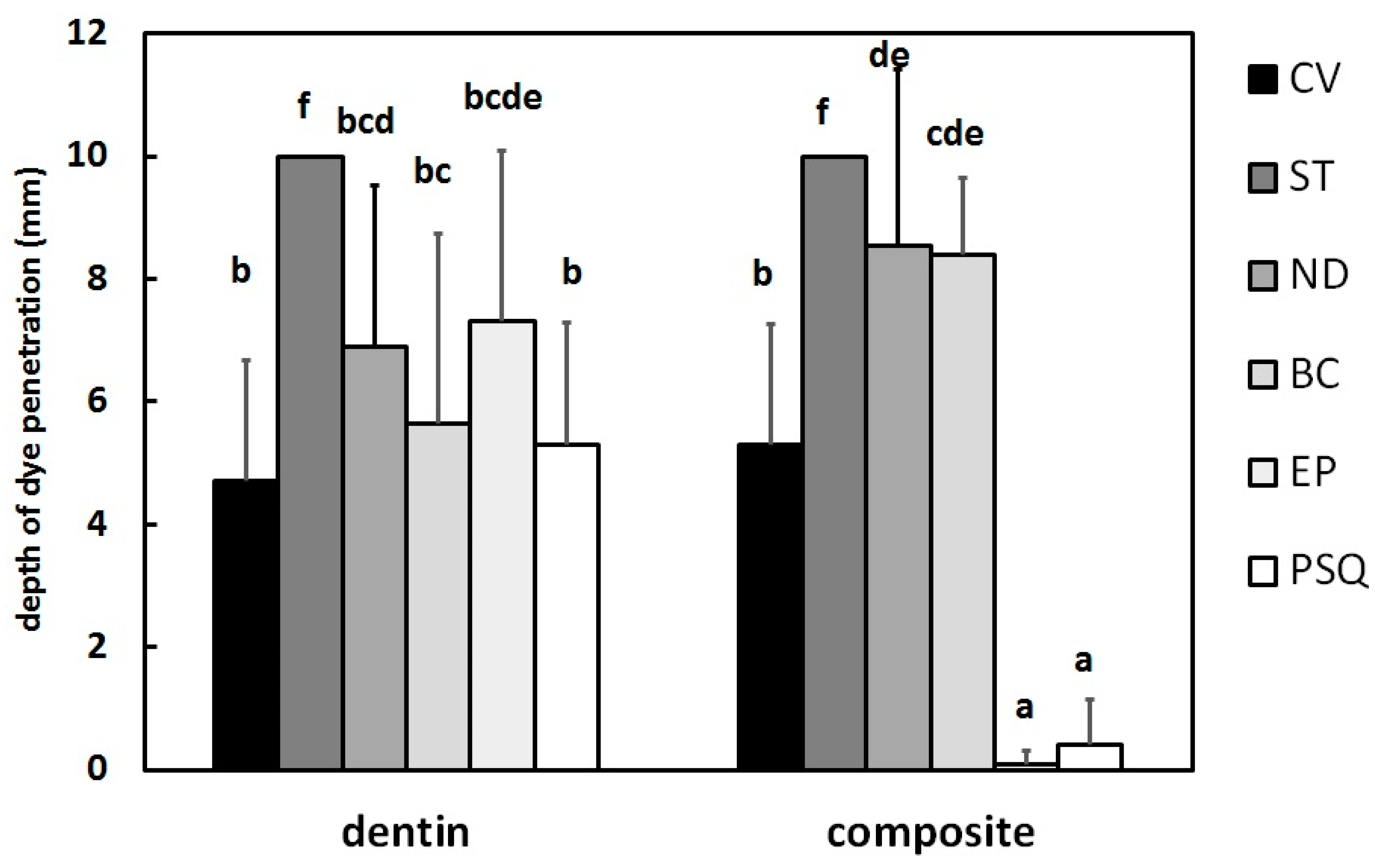
3.1. Dentin Side
3.2. Composite Side
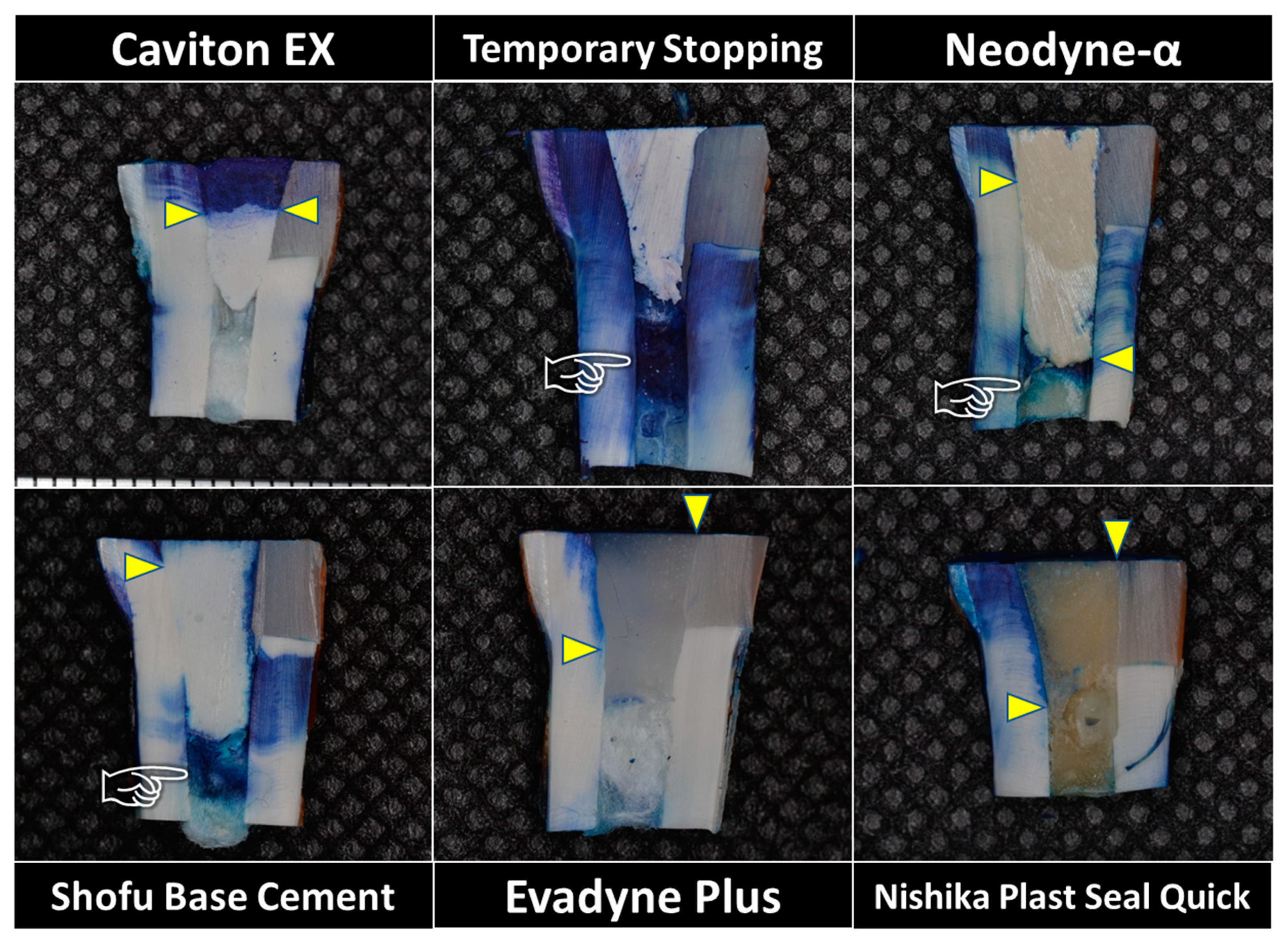
3.3. Observation of Dye Penetration
4. Discussion
5. Conclusions
- For dentinal margins, hydraulic temporary restorative material (Caviton EX), zinc oxide eugenol cement (Neodyne-α), glass-ionomer cement (Shofu Base Cement), and resin-based temporary restorative materials (Nishika Plast Seal Quick and Evadyne Plus) had similarly effective sealing ability. However, the sealing effect of Temporary Stopping was significantly lower than the other tested materials.
- For the margins of pre-endodontic resin composite build-up, two resin-based temporary restorative materials (Nishika Plast Seal Quick and Evadyne Plus) showed excellent sealing properties. Caviton EX had a moderate sealing effect to both types of cavity wall. The sealing effect of zinc oxide eugenol cement (Neodyne-α) and glass-ionomer cement (Shofu Base Cement) was lower than Caviton EX.
Author Contributions
Funding
Conflicts of Interest
References
- Swanson, K.; Madison, S. An evaluation of coronal microleakage in endodontically treated teeth. Part 1. Time periods. J. Endod. 1987, 13, 56–59. [Google Scholar] [CrossRef]
- Sivakumar, J.S.; Suresh Kumar, B.N.; Shyamala, P.V. Role of provisional restorations in endodontic therapy. J. Pharm. Bioall. Sci. 2013, 5 (Suppl. S1), S120–S124. [Google Scholar] [CrossRef]
- Križnar, I.; Seme, K.; Fidler, A. Bacterial microleakage of temporary filling materials used for endodontic access cavity sealing. J. Dent. Sci. 2016, 11, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Zmener, O.; Bebegas, G.; Pameijer, C.H. Coronal microleakage of three temporary restorative materials: An in vitro study. J. Endod. 2004, 30, 582–584. [Google Scholar] [CrossRef] [PubMed]
- Üçtaşh, M.B.; Tinaz, A.C. Microleakage of different types of temporary restorative materials used in endodontics. J. Oral Sci. 2000, 42, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Çiftçi, A.; Vardarlı, D.A.; Sönmez, I.Ş. Coronal microleakage of four endodontic temporary restorative materials: An in vitro study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, e67–e70. [Google Scholar] [CrossRef]
- Prabhakar, A.R.; Rani, N.S.; Naik, S.V. Comparative evaluation of sealing ability, absorption, and solubility of three temporary restorative materials: An in vitro study. Int. J. Clin. Pediatr. Dent. 2017, 10, 136–141. [Google Scholar] [CrossRef]
- Srivastava, P.K.; Nagpal, A.; Setya, G.; Kumar, S.; Chaudary, A.; Dhanker, K. Assessment of coronal leakage of temporary restorations in root canal treated teeth: An in vitro study. J. Contemp. Dent. Pract. 2017, 18, 126–130. [Google Scholar] [CrossRef]
- Shahi, S.; Samiei, S.; Rahimi, S.; Nezami, H. In vitro comparison of dye penetration through four temporary restorative materials. Iran. Endod. J. 2010, 5, 59–63. [Google Scholar]
- Suehara, M.; Suzuki, S.; Nakagawa, K. Evaluation of wear and subsequent dye penetration of endodontic temporary restorative materials. Dent. Mater. J. 2006, 25, 199–204. [Google Scholar] [CrossRef][Green Version]
- Kim, S.-Y.; Ahn, J.-S.; Yi, Y.-A.; Lee, Y.; Hwang, J.-Y.; Seo, D.-G. Quantitative microleakage analysis of endodontic temporary filling materials using a glucose penetration model. Acta Odontol. Scand. 2015, 73, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Yang, S.D.; Hwang, Y.F.; Chueh, L.H.; Chung, K.H. Microleakage of endodontic temporary restorative materials. J. Endod. 1993, 19, 516–520. [Google Scholar] [CrossRef]
- Kshirsagar, S.; Aggarwal, S.; Mukhtar, A.; Gupta, P.; Rai, V.; Chawla, M. Pre endodontic build-up of a grossly destructed tooth: A case report. Int. J. Sci. Stud. 2015, 2, 225–229. [Google Scholar] [CrossRef]
- Heydrich, R.W. Pre-endodontic treatment restorations. A modification of the ‘donut’ technique. J. Am. Dent. Assoc. 2005, 136, 641–642. [Google Scholar] [CrossRef] [PubMed]
- Pai, S.-F.; Yang, S.-F.; Sue, W.-L.; Chueh, L.-H.; Rivera, E.M. Microleakage between endodontic temporary restorative materials placed at different times. J. Endod. 1999, 25, 453–456. [Google Scholar] [CrossRef]
- Hargreaves, K.H.; Cohen, S. Pathways of the Pulp, 10th ed.; Mosby: St Louis, MO, USA, 2010; p. 109. [Google Scholar]
- Anderson, R.W.; Powell, B.J.; Pashley, D.H. Microleakage of temporary restorations in complex endodontic access preparations. J. Endod. 1989, 15, 526–529. [Google Scholar] [CrossRef]
- Nakashima, K.; Terata, R.; Yoshinaka, S.; Kubota, M. Marginal sealing ability of resinous temporary materials—Effect of thermal stress on marginal sealing ability. Jpn. J. Conserv. Dent. 1997, 40, 1000–1003. [Google Scholar]
- Noguiera, A.P.; McDonald, N.J. A comparative in vitro coronal microleakage study of new endodontic restorative materials. J. Endod. 1990, 16, 523–527. [Google Scholar] [CrossRef]
- Marosky, J.E.; Patterson, S.S.; Swartz, M. Marginal leakage of temporary restorative materials used between endodontic appointments assessed by calcium 45—An in vitro study. J. Endod. 1977, 3, 110–113. [Google Scholar] [CrossRef]
- Ono, K.; Matsumoto, K. The physical properties of a new sealing cement. Int. Endod. J. 1992, 25, 130–133. [Google Scholar] [CrossRef]
- Widerman, F.H.; Eames, W.B.; Serene, T.P. The physical and biologic properties of Cavit. J. Am. Dent. Assoc. 1971, 82, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Grossman, L.I. A study of temporary fillings as hermetic sealing agents. J. Dent. Res. 1939, 18, 67–71. [Google Scholar] [CrossRef]
- Blaney, T.D.; Peters, D.D.; Setterstrom, J.; Bernier, W.E. Marginal sealing quality of IRM and Cavit as assessed by microbial penetration. J. Endod. 1981, 7, 453–457. [Google Scholar] [CrossRef]
- Friedman, S.; Shani, J.; Stabholz, A.; Kaplawi, J. Comparative sealing ability of temporary filling materials evaluated by leakage of radiosodium. Int. Endod. J. 1986, 19, 187–193. [Google Scholar] [CrossRef]
- Furusawa, M.; Okutomi, T.; Kohno, T.; Shibuya, Y.; Yamaguchi, S.; Ito, A.; Asai, Y. Additional studies of sealing properties of various hydraulic temporary sealing materials in vitro. Shikwa Gakuho 1993, 93, 867–882. [Google Scholar]
- Gilles, J.A.; Fuget, E.F.; Stone, R.C. Dimensional stability of temporary restoratives. Oral Surg. Oral Med. Oral Pathol. 1975, 40, 796–800. [Google Scholar] [CrossRef]
- Lohbauer, U. Dental glass ionomer cements as permanent filling materials?—Properties, limitations and future trends. Materials 2010, 3, 76–96. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A review of glass-ionomer cements for clinical dentistry. J. Funct. Biomater. 2016, 7, 16. [Google Scholar] [CrossRef]
- Tamura, Y.; Takahashi, F.; Sumino, N.; Kawamoto, R.; Tsujimoto, A.; Yamaji, A.; Tsubota, K.; Kurokawa, H.; Miyazaki, M. A study on marginal sealing of an experimental temporary restorative material containing S-PRG filler. Jpn. J. Conserv. Dent. 2013, 56, 193–199. [Google Scholar] [CrossRef]
- Webber, R.; del Rio, C.E.; Brandy, J.M.; Segall, R.O. Sealing quality of a temporary filling material. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1978, 46, 123–130. [Google Scholar] [CrossRef]
- Turner, J.E.; Anderson, R.W.; Pashley, D.H.; Pantera, E.A., Jr. Microleakage of temporary endodontic materials in teeth restored with amalgam. J. Endod. 1990, 16, 1–4. [Google Scholar] [CrossRef]
- Camps, J.; Pashley, D. Reliability of the dye penetration studies. J. Endod. 2003, 29, 592–594. [Google Scholar] [CrossRef] [PubMed]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kameyama, A.; Saito, A.; Haruyama, A.; Komada, T.; Sugiyama, S.; Takahashi, T.; Muramatsu, T. Marginal Leakage of Endodontic Temporary Restorative Materials around Access Cavities Prepared with Pre-Endodontic Composite Build-Up: An In Vitro Study. Materials 2020, 13, 1700. https://doi.org/10.3390/ma13071700
Kameyama A, Saito A, Haruyama A, Komada T, Sugiyama S, Takahashi T, Muramatsu T. Marginal Leakage of Endodontic Temporary Restorative Materials around Access Cavities Prepared with Pre-Endodontic Composite Build-Up: An In Vitro Study. Materials. 2020; 13(7):1700. https://doi.org/10.3390/ma13071700
Chicago/Turabian StyleKameyama, Atsushi, Aoi Saito, Akiko Haruyama, Tomoaki Komada, Setsuko Sugiyama, Toshiyuki Takahashi, and Takashi Muramatsu. 2020. "Marginal Leakage of Endodontic Temporary Restorative Materials around Access Cavities Prepared with Pre-Endodontic Composite Build-Up: An In Vitro Study" Materials 13, no. 7: 1700. https://doi.org/10.3390/ma13071700
APA StyleKameyama, A., Saito, A., Haruyama, A., Komada, T., Sugiyama, S., Takahashi, T., & Muramatsu, T. (2020). Marginal Leakage of Endodontic Temporary Restorative Materials around Access Cavities Prepared with Pre-Endodontic Composite Build-Up: An In Vitro Study. Materials, 13(7), 1700. https://doi.org/10.3390/ma13071700





