Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures
Abstract
1. Introduction
2. Materials and Test Methods
2.1. Materials
2.2. Method of Thermocycling
2.3. Microhardness Testing
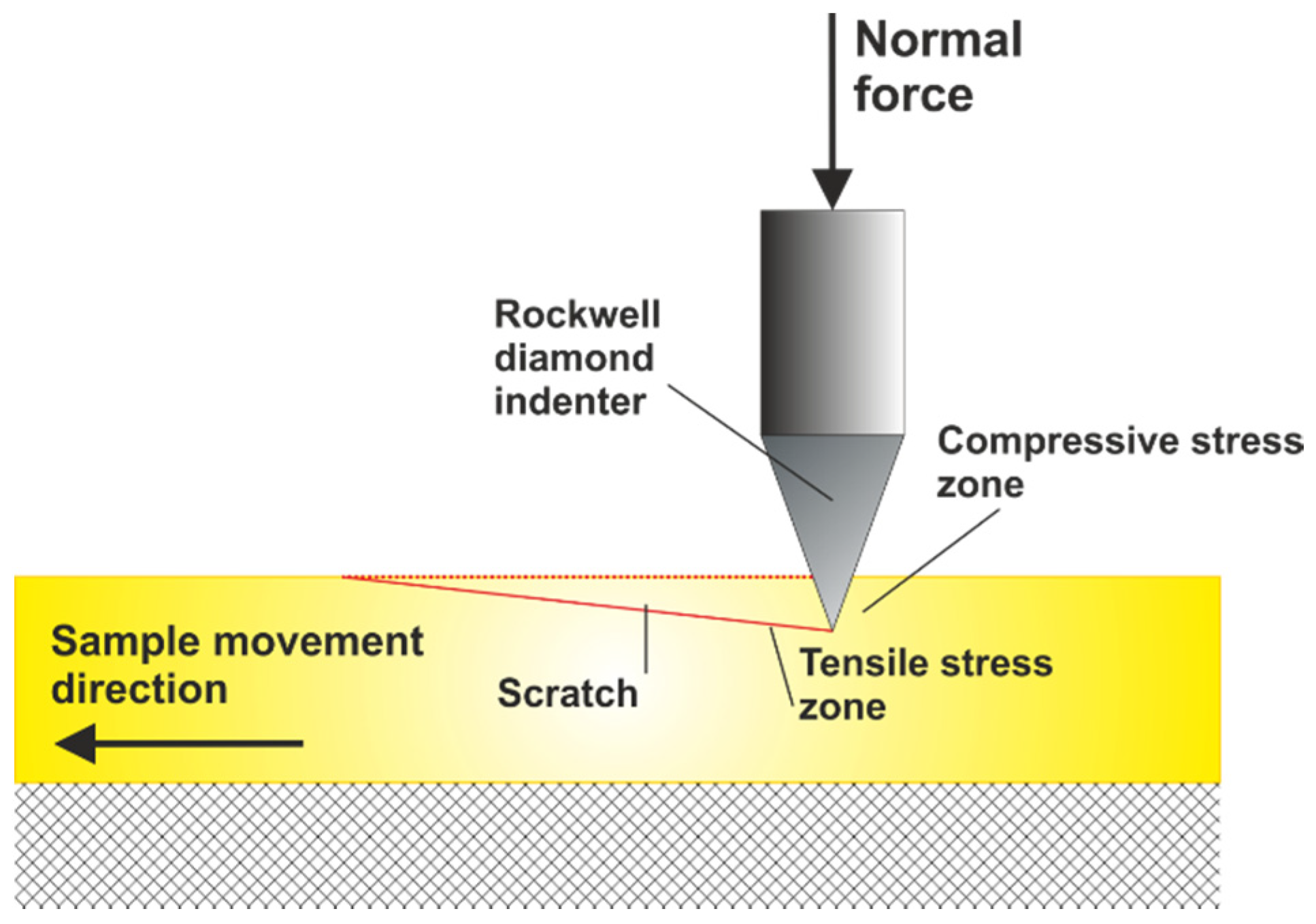
2.4. Microscratch Tests
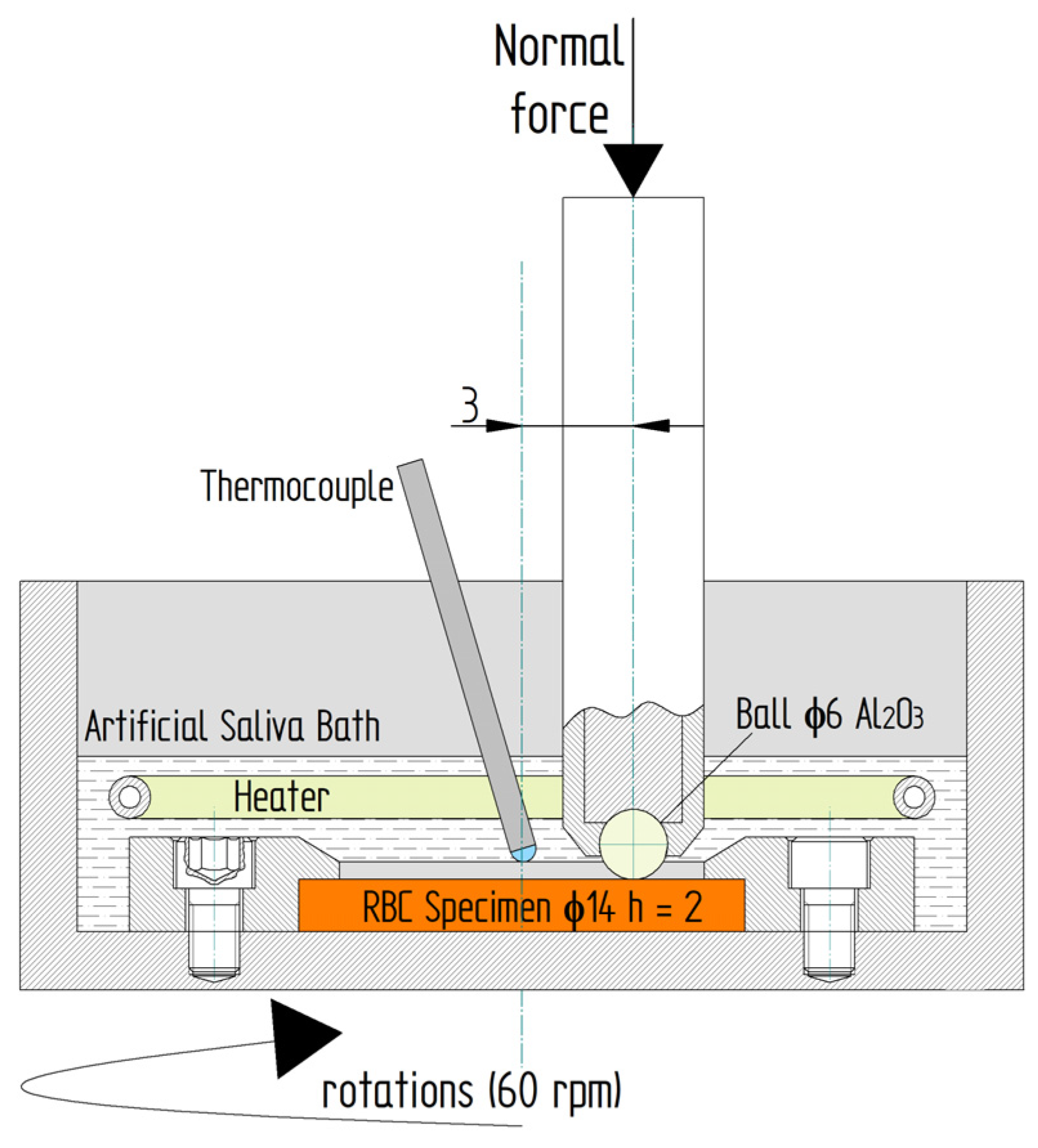
2.5. Wear Sliding Test
3. Results and Discussion
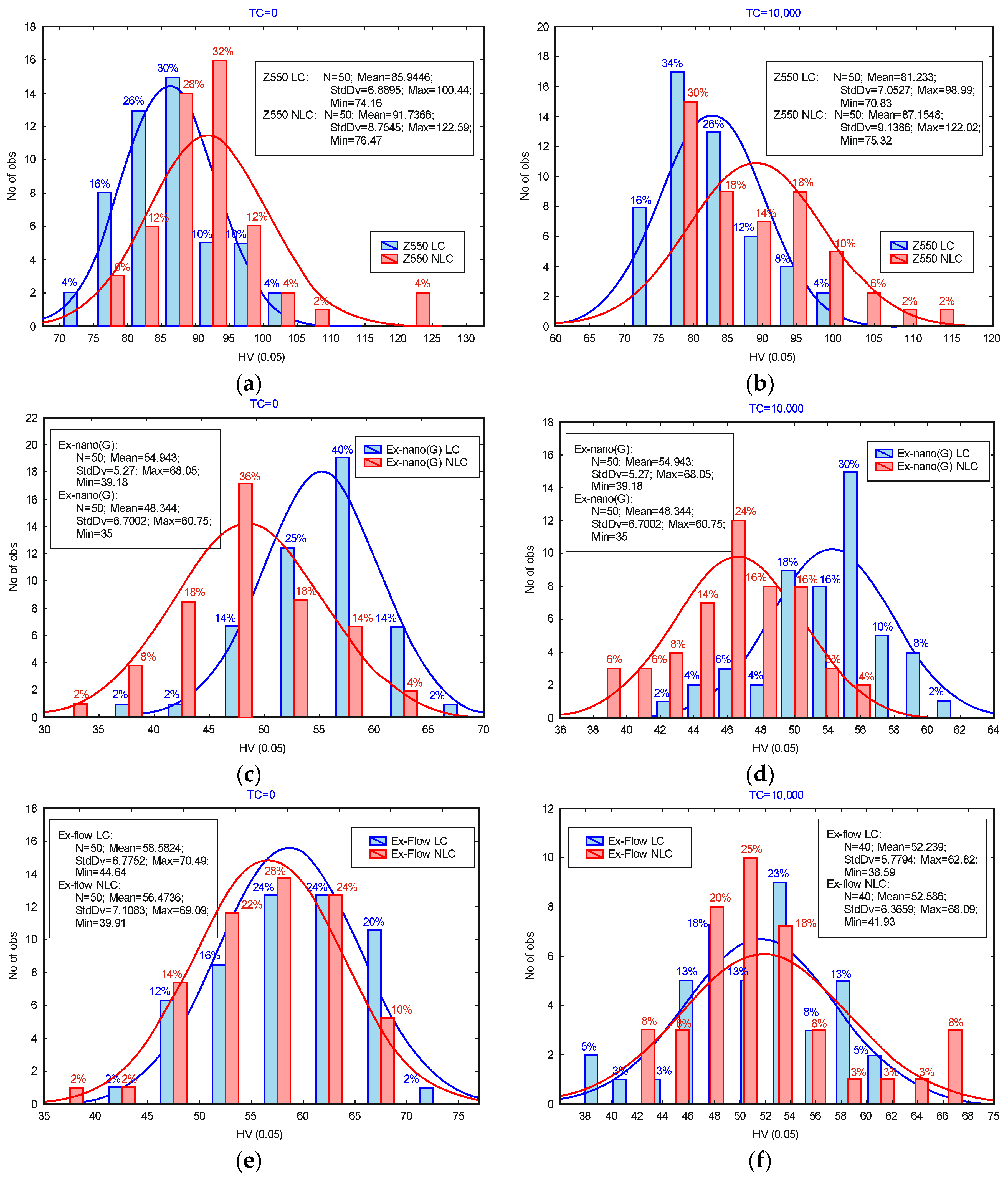
3.1. Microhardness
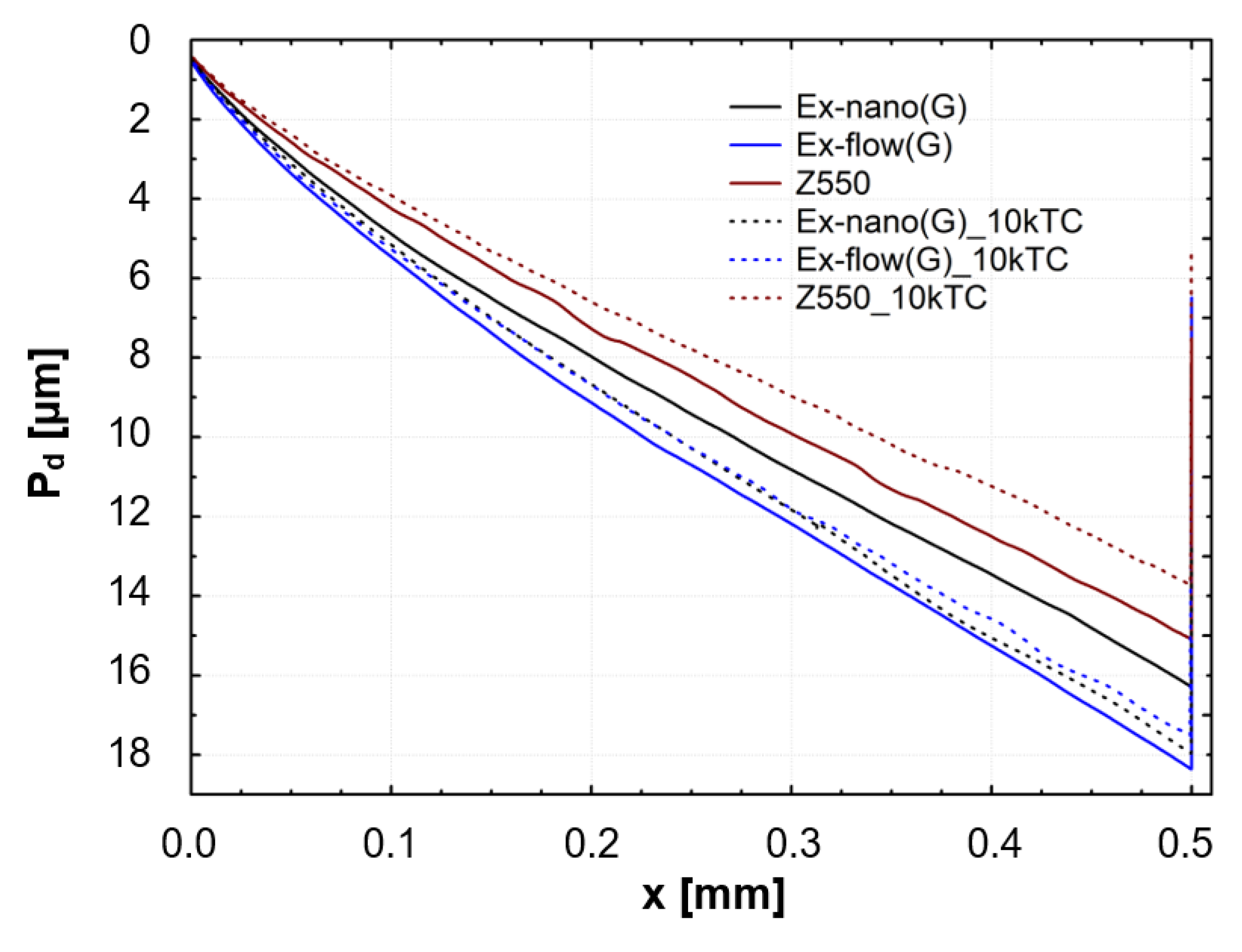
3.2. Scratch Tests
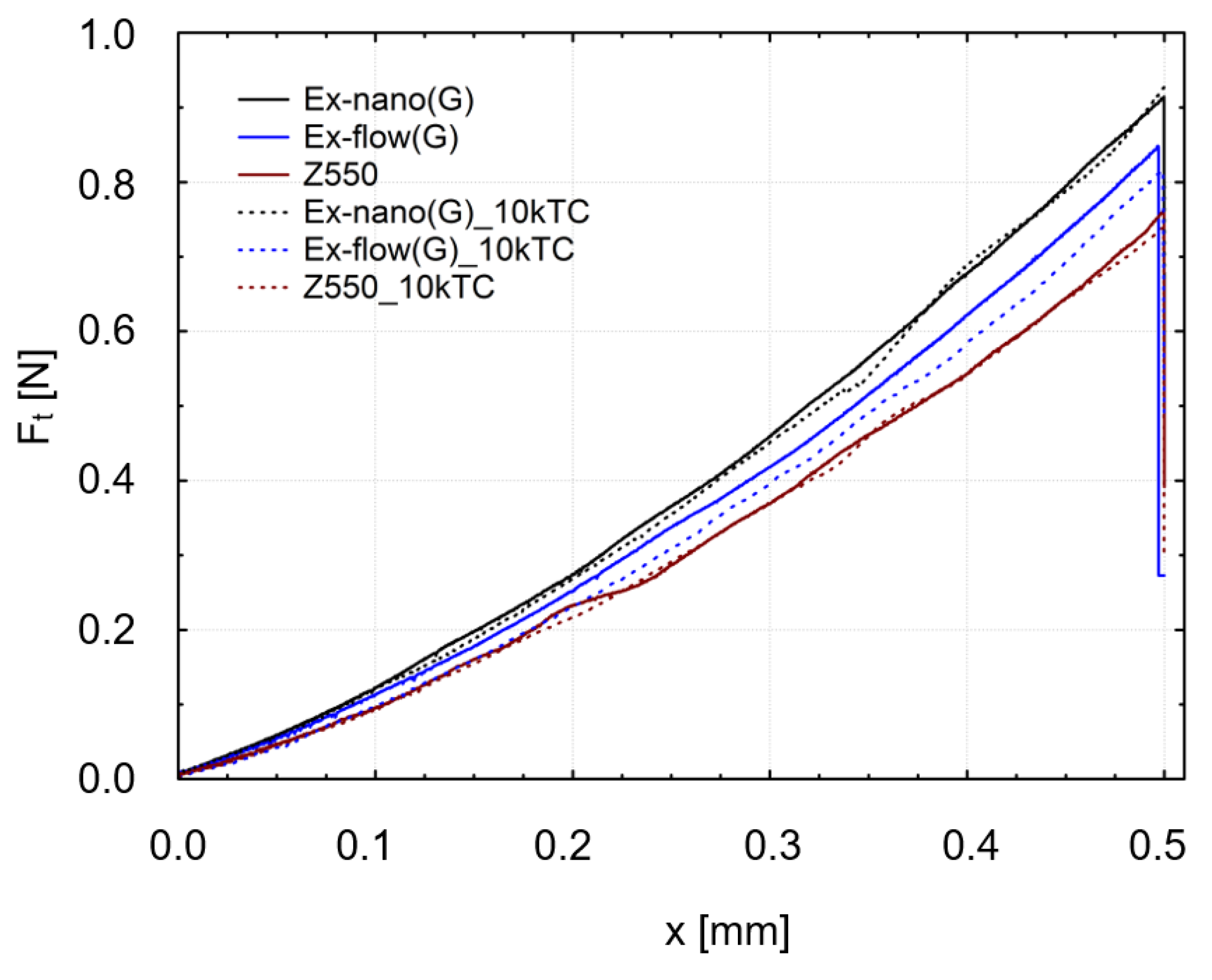
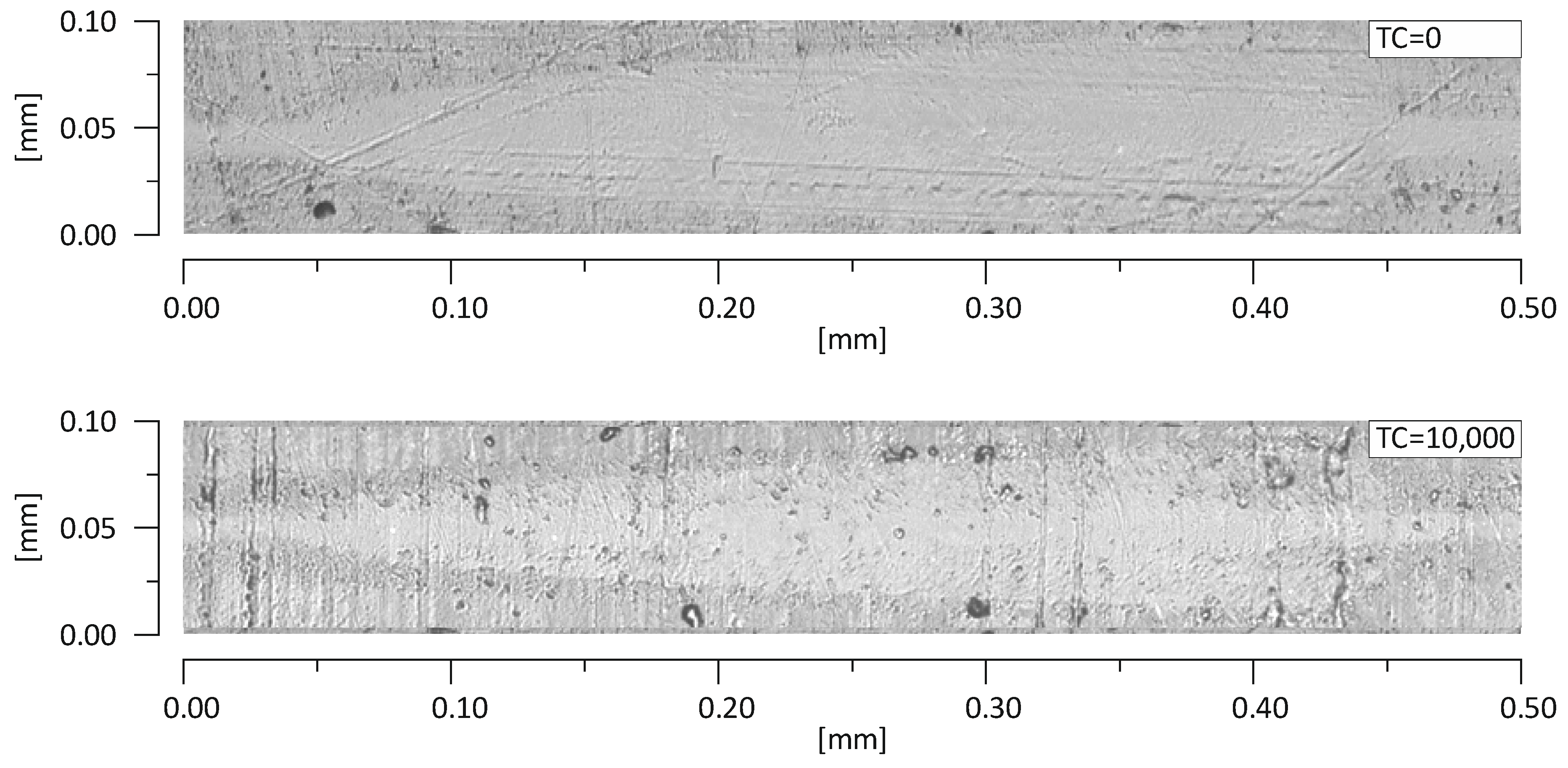
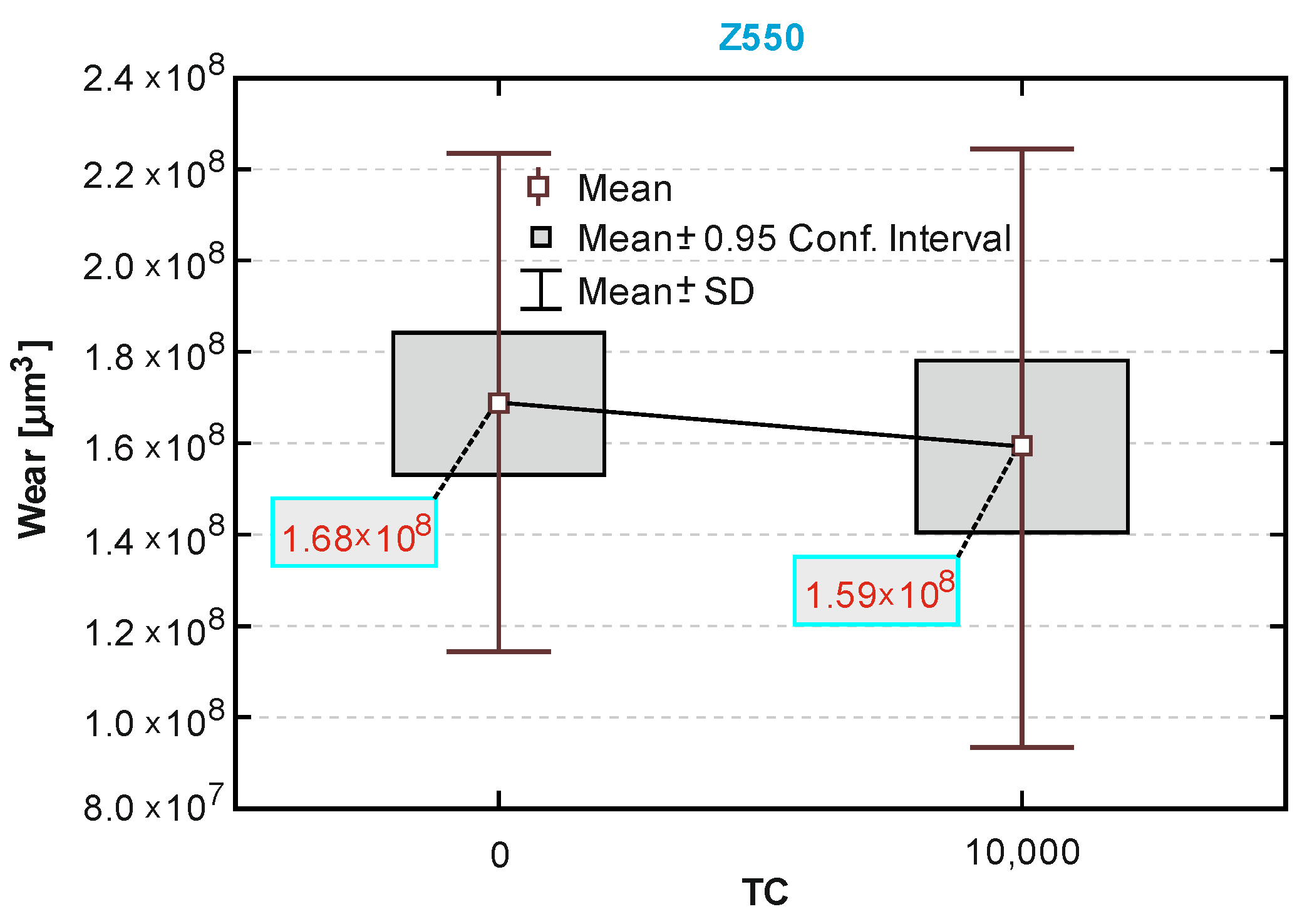
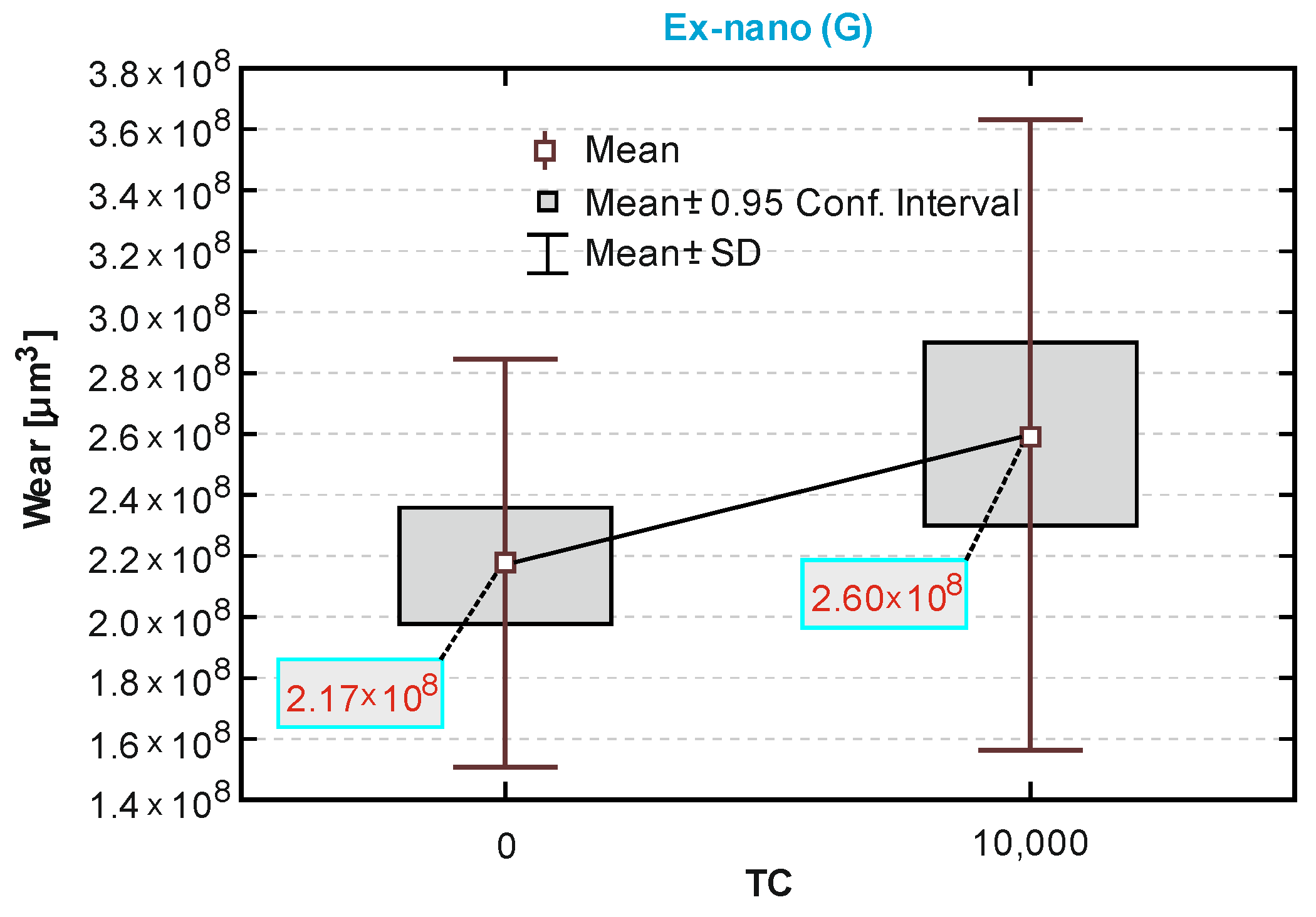
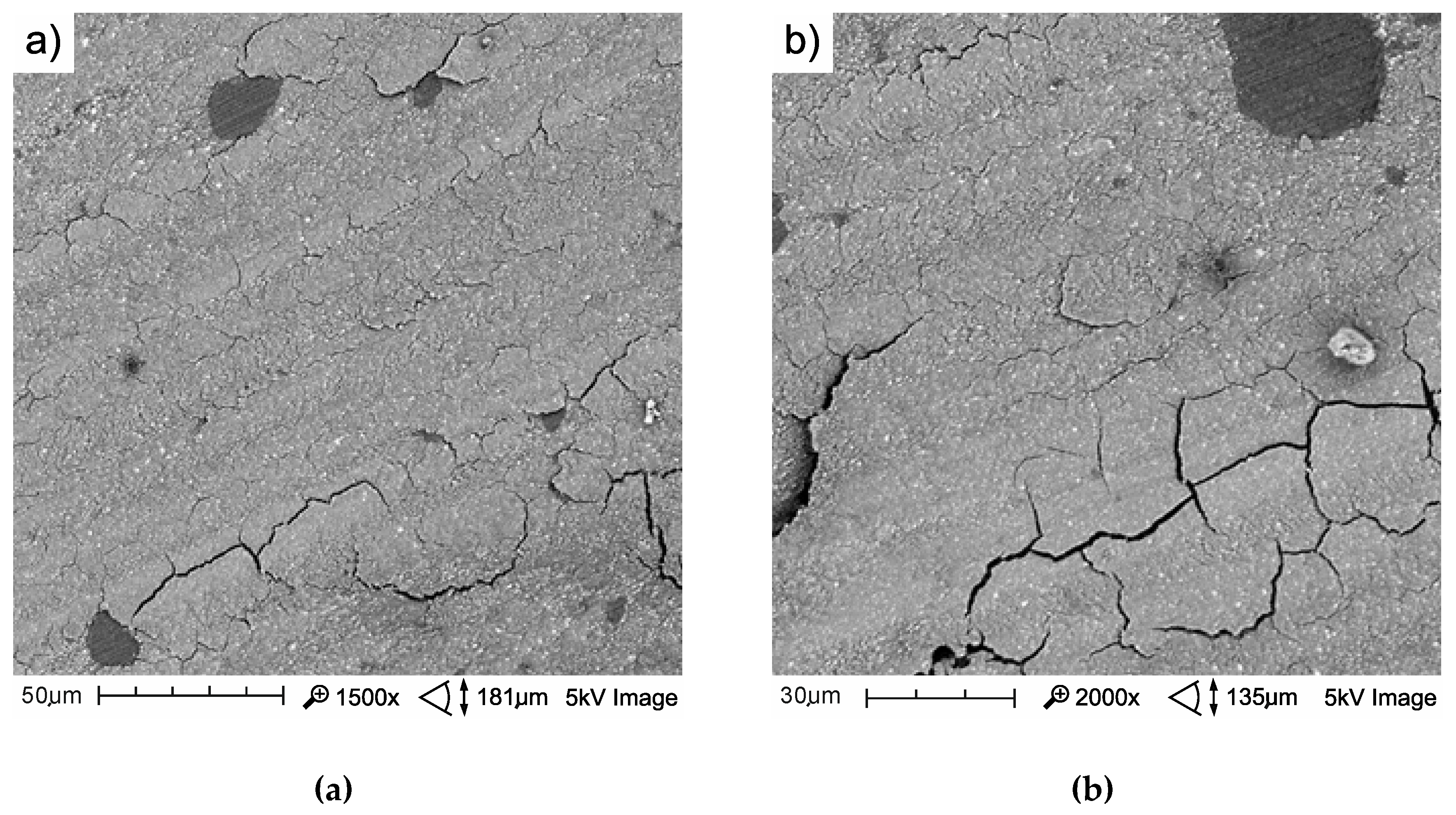
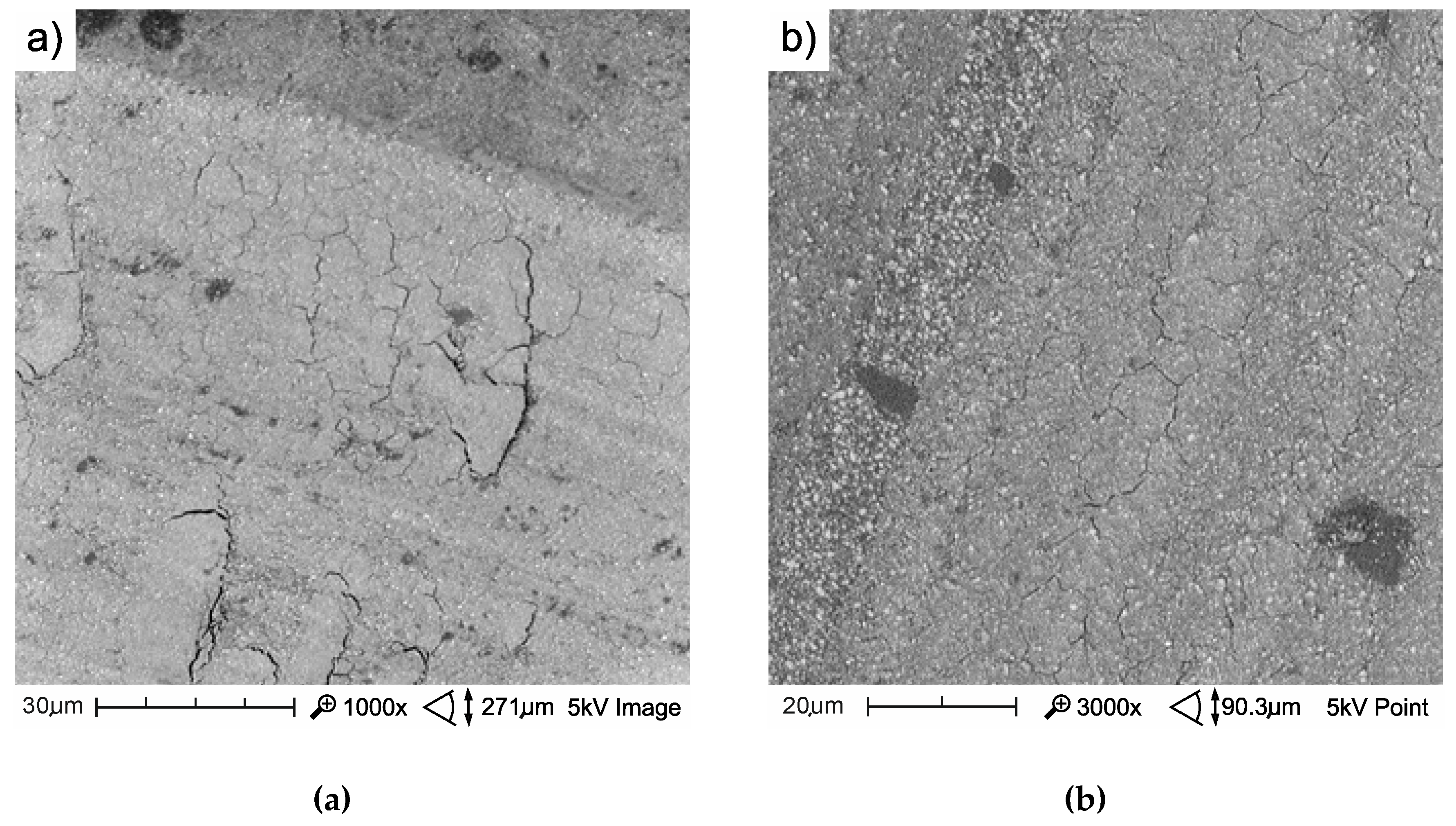
3.3. Sliding Wear
4. Conclusions
- A direct positive correlation was found between thermocycling fatigue and microhardness. Decreases in microhardness were not high after the implementation of 104 thermocycles.
- The dominant mechanism of the wear of experimental composites after thermocycling is the removal of fragments of materials in the form of flakes from the friction surface (spalling). Total wear was a combination of abrasive and fatigue wear, which resulted in flake extraction.
- The results presented in this paper indicated that in the case of the experimental materials, in particular Ex-nano (G), hydrothermal fatigue was synergistic with mechanical fatigue. In addition, thermal cycler loading can lead to reduced resistance to tribological wear.
- The results obtained did not indicate a correlation of Vickers hardness with sliding wear but indicated a correlation between Vickers hardness and scratch resistance.
- The SEM analysis of traces after tribological tests indicated that the nature of wear in both cases is quasi-brittle and is typical of materials with moderate toughness and yield strength and the damage zone has numerous microcrackings.
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Finlay, N.; Hahnel, S.; Dowling, A.H.; Fleming, G.J.P. The in vitro wear behavior of experimental resin-based composites derived from a commercial formulation. Dent. Mat. 2013, 29, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Kruzic, J.J.; Arsecularatne, J.A.; Tanaka, C.B.; Hoffman, M.J.; Cesar, P.F. Recent advances in understanding the fatigue and wear behavior of dental composites and ceramics. J. Mech. Behav. Biomed. Mater. 2018, 88, 504–533. [Google Scholar] [CrossRef] [PubMed]
- Chadda, H.; Satapathy, B.K.; Patnaik, A.; Ray, A.R. Mechanistic interpretations of fracture toughness and correlations to wear behavior of hydroxyapatite and silica/hydroxyapatite filled bis-GMA/TEGDMA micro/hybrid dental restorative composites. Compos. Pt. B-Eng. 2017, 130, 132–146. [Google Scholar] [CrossRef]
- Walczak, A.; Niewczas, A.; Pieniak, D.; Gil, L.; Kozłowski, E.; Kordos, P. Temporary Stability of Compressive Strength of Flow and Universal Type LC PMCCS Materials. Adv. Mater. Sci. 2018, 18, 22–33. [Google Scholar] [CrossRef]
- Antunes, P.V.; Ramahlo, A.; Carrihlo, E.V.P. Mechanical and wear behaviours of nano and microfilled polymeric composite: Effect of filler fraction and size. Mater. Des. 2014, 61, 50–60. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Ferracene, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef]
- Braem, M.; Lambrechts, P.; van Doren, V.; Vanherle, G. In vivo evaluation of four posterior composites: Quantitative wear measurements and clinical behaviour. Dent. Mater. 1986, 2, 106–113. [Google Scholar] [CrossRef]
- Gonçalves, F.; Kawano, Y.; Braga, R.R. Contraction stress related to composite inorganic content. Dent. Mater. 2010, 26, 704–709. [Google Scholar] [CrossRef]
- Kim, K.H.; Ong, J.L.; Okuno, O. The effect of filler loading and morphology on the mechanical properties of contemporary composites. J. Prosthet. Dent. 2002, 87, 642–649. [Google Scholar] [CrossRef]
- Shalaby, W.S.; Salz, U. Polymers for Dental and Orthopedic Applications; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Pieniak, D.; Przystupa, K.; Walczak, A.; Niewczas, A.M.; Krzyzak, A.; Bartnik, G.; Gil, L.; Lonkwic, P. Hydro-Thermal Fatigue of Polymer Matrix Composite Biomaterials. Materials 2019, 12, 3650. [Google Scholar] [CrossRef]
- Leibrock, H.; Degenhart, M.; Behr, M.; Rosentritt, M.; Handel, G. In vitro study on the effect of thermo- and load-cycling on the bond strength of porcelain repair systems. J. Oral Rehabil. 1999, 26, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Zbaren, C.; Stawarczyk, B.; Hammerle, C.H.F. The effect of thermal cycling on metal–ceramic bond strength. J. Dent. 2009, 37, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Arsecularatne, J.A.; Chung, N.R.; Hoffman, M. An in vitro study of the wear behaviour of dental composites. Biosurf. Biotribol. 2016, 2, 102–113. [Google Scholar] [CrossRef]
- Makarian, K.; Santhanam, S.; Wing, Z.N. Thermal shock resistance of refractory composites with Zirconia and Silicon-Carbide inclusions and alumina binder. Ceram. Int. 2018, 44, 12055–12064. [Google Scholar] [CrossRef]
- Freeman, R.; Varanasi, S.; Meyers, I.A.; Symons, A.L. Effect of air abrasion and thermocycling on resin adaptation and shear bond strength to dentin for an etch-and-rinse and selfetch resin adhesive. Dent. Mater. J. 2012, 31, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Drummond, J.L. Degradation, fatigue and failure of resin dental composite materials. J. Dent. Res. 2008, 87, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Rousson, V. Clinical effectiveness of direct class II restorations a meta-analysis. J. Adhes Dent. 2012, 14, 407–431. [Google Scholar]
- Bayne, S.C. Correlation of clinical performance with “in vitro tests” of restorative dental materials that use polymer-based matrices. Dent. Mater. 2012, 28, 52–71. [Google Scholar] [CrossRef]
- Przystupa, K. Reliability assessment method of device under incomplete observation of failure. In Proceedings of the 2018 18th International Conference on Mechatronics-Mechatronika (ME), Brno, Czech Republic, 5–7 December 2018; IEEE: Piscataway, NJ, USA, 2019; pp. 1–6. [Google Scholar]
- Przystupa, K. The methods analysis of hazards and product defects in food processing. Czech J. Food Sci. 2019, 37, 44–50. [Google Scholar] [CrossRef]
- Akin, H.; Ozdemir, A.K. Effect of corrosive environments and thermocycling on the attractive force of four types of dental magnetic attachments. J. Den. Sci. 2013, 8, 184–188. [Google Scholar] [CrossRef]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.R.; D’arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Vasiliu, R.-D.; Porojan, S.D.; Bîrdeanu, M.I.; Porojan, L. Effect of Thermocycling, Surface Treatments and Microstructure on the Optical Properties and Roughness of CAD-CAM and Heat-Pressed Glass Ceramics. Materials 2020, 13, 381. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Kochan, O.; Przystupa, K.; Su, J. Information-measuring System to Study the Thermocouple with Controlled Temperature Field. Meas. Sci. Rev. 2019, 19, 161–169. [Google Scholar] [CrossRef]
- Cavalcanti, A.N.; Mitsui, F.H.O.; Ambrosano, G.M.B.; Marchi, G.M. Influence of adhesive systems and flowable composite lining on bond strength of class II restorations submitted to thermal and mechanical stresses. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2007, 80, 52–58. [Google Scholar] [CrossRef]
- Xu, H.; Eichmiller, F.; Smith, D.; Schumacher, G.; Giuseppetti, A.; Antonucci, J. Effect of thermal cycling of whiskers - reinforced dental resin composites. J. Mater. Sci.-Mater. Med. 2002, 13, 875–883. [Google Scholar] [CrossRef]
- Javaheri, M.; Seifi, S.M.; Aghazadeh Mohandesi, J.; Shafie, F. Compressive fatigue and thermal compressive fatigue of hybrid resin base dental composites. In IFMBE Proceedings, Proceedings of the13th International Conference on Biomedical Engineering, Singapore, 3–6 December 2008; Lim, C.T., Goh, J.C.H., Eds.; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Mair, L.H.; Stolarski, T.A.; Vowles, R.W.; Lloyd, C.H. Wear: Mechanisms, manifestations and measurement. Rep. Workshop J. Dent. 1996, 24, 141–148. [Google Scholar]
- Kawano, F.; Ohguri, T.; Ichikawa, T.; Matsumoto, N. Influence of thermal cycles in water on flexural strength of laboratory-processed composite resin. J. Oral Rehabil. 2001, 28, 703–707. [Google Scholar] [CrossRef]
- Janda, R.; Roulet, J.F.; Latta, M.; Ruttermann, S. Water sorption and solubility of contemporary resin-based filling materials. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2007, 82, 545–551. [Google Scholar] [CrossRef]
- Pieniak, D.; Walczak, A.; Niewczas, A.M.; Przystupa, K. The Effect of Thermocycling on Surface Layer Properties of Light Cured Polymer Matrix Ceramic Composites (PMCCs) Used in Sliding Friction Pair. Materials 2019, 12, 2776. [Google Scholar] [CrossRef]
- Walczak, A.; Pieniak, D.; Niewczas, A.M.; Gil, L. Laboratory studies of the influence of thermal cycling on anti-wear properties of composites used in biotribological friction pairs. Tribologia 2018, 280, 143–149. [Google Scholar] [CrossRef]
- Pieniak, D.; Kordos, P. Analysis of the degree of hydro-thermal fatigue damage of the surface layer of polymer-ceramic composites intended for operation in a biotribological node. Tribologia 2019, 284, 105–115. [Google Scholar] [CrossRef]
- Palaniappan, S.; Peumans, M.; Van Meerbeek, B.; Lambrechts, P. Wear prediction in dental composites. In Woodhead Publishing Series in Biomaterials, Bio-Tribocorrosion in Biomaterials and Medical Implants; Yan, Y., Ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 130–144. [Google Scholar]
- Souza, J.; Bentes, A.; Reis, K.; Gavinha, S.; Buciumeanu, M.; Henriques, B.; Silva, F.S.; Gomes, J.R. Abrasive and sliding wear of resin composites for dental restorations. Tribol. Int. 2016, 102, 154–160. [Google Scholar] [CrossRef]
- Lambrechts, P.; Goovaerts, K.; Bharadwaj, D.; De Munck, J.; Bergmans, L.; Peumans, M.; Van Meerbeek, B. Degradation of tooth structure and restorative materials: A review. Wear 2006, 261, 980–986. [Google Scholar] [CrossRef]
- Heintze, S.D.; Zellweger, G.; Zappini, G. The relationship between physical parameters and wear of dental composites. Wear 2007, 263, 1138–1146. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Li, J.; Li, H.; Foka, A.S.L.; Watts, D.C. Multiple correlations of material parameters of light-cured dental composites. Dent. Mater. 2009, 25, 829–836. [Google Scholar] [CrossRef]
- Mayworm, C.D.; Camargo, S.S., Jr.; Bastian, F.L. Influence of artificial saliva on abrasive wear and microhardness of dental composites filled with nanoparticles. J. Dent. 2008, 36, 703–710. [Google Scholar] [CrossRef]
- Marovic, D.; Panduric, V.; Tarle, Z.; Ristic, M.; Sariri, K.; Demoli, N.; Klaric, E.; Jankovic, B.; Prskalo, K. Degree of conversion and microhardness of dental composite resin materials. J. Mol. Struct. 2013, 1044, 299–302. [Google Scholar] [CrossRef]
- Delfino, C.S.; Youssef, M.N.; Souza, F.B.; Braz, R.; Turbino, M.L. Microhardness of a dental restorative composite resin containing nanoparticles polymerized with argon ion laser. Optik 2012, 123, 263–267. [Google Scholar] [CrossRef]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of Dental Materials guidance-Resin composites: Part I-Mechanical properties. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef]
- Łępicka, M.; Grądzka-Dahlke, M.; Pieniak, D.; Pasierbiewicz, K.; Niewczas, A. Effect of mechanical properties of substrate and coating on wear performance of TiN- or DLC-coated 316LVM stainless steel. Wear 2017, 382–383, 62–70. [Google Scholar] [CrossRef]
- Łępicka, M.; Grądzka-Dahlke, M.; Pieniak, D.; Pasierbiewicz, K.; Kryńska, K.; Niewczas, A. Tribological performance of titanium nitride coatings: A comparative study on TiN-coated stainless steel and titanium alloy. Wear 2019, 422–423, 68–80. [Google Scholar] [CrossRef]
- Łępicka, M.; Ciszewski, A.; Golak, K.; Grądzka-Dahlke, M. A Comparative Study of Friction and Wear Processes of Model Metallic Biomaterials Including Registration of Friction-Induced Temperature Response of a Tribological Pair. Materials 2019, 12, 4163. [Google Scholar] [CrossRef] [PubMed]
- Clelland, N.L.; Agarwala, V.; Knobloch, L.A.; Seghi, R.R. Wear of enamel opposing low-fusing and conventional ceramic restorative materials. J. Prosthodont. 2001, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, S.; Schultz, S.; Trempler, C.; Ach, B.; Handel, G.; Rosentritt, M. Two-body wear of dental restorative materials. J. Mech. Behav. Biomed. Mater. 2011, 4, 237–244. [Google Scholar] [CrossRef]
- Ghazal, M.; Albashaireh, Z.S.; Kern, M. Wear resistance of nanofilled composite resin and feldspathic ceramic artificial teeth. J. Prosthet. Dent. 2008, 100, 441–448. [Google Scholar] [CrossRef]
- Paczkowska, M.; Selech, J.; Piasecki, A. Effect of surface treatment on abrasive wear resistance of seeder coulter flap. Surf. Rev. Lett. 2016, 23, 1650007. [Google Scholar] [CrossRef]
- Borrero-Lopez, O.; Guiberteau, F.; Zhang, Y.; Lawn, B.R. Wear of ceramic-based dental materials. J. Mech. Behav. Biomed. Mater. 2019, 92, 144–151. [Google Scholar] [CrossRef]
- Walczak, M.; Pieniak, D.; Niewczas, A.M. Effect of recasting on the useful properties CoCrMoW alloy. Eksploat. Niezawodn. 2014, 16, 330–336. [Google Scholar]
- Pieniak, D.; Niewczas, A.M.; Walczak, M.; Zamościńska, J. Influence of photopolymerization parameters on the mechanical properties of polymer – ceramic composites applied in the conservative dentistry. Acta Bioeng. Biomech. 2014, 16, 29–35. [Google Scholar]
- Tuncer, S.; Demirci, M.; Tiryaki, M.; Ünlü, N.; Uysal, Ö. The Effect of a modeling resin and thermocycling on the surface hardness, roughness, and color of different resin composites. J. Esthet. Restor. Dent. 2013, 25, 404–419. [Google Scholar] [CrossRef] [PubMed]
- Pieniak, D.; Niewczas, A.M.; Kordos, P. Influence of thermal fatigue and ageing on the microhardness of polymer-ceramic composites for biomedical applications. Eksploat. Niezawodn. 2012, 14, 181–188. [Google Scholar]
- Souza, R.O.A.; Ozcan, M.; Michida, S.M.A.; de Melo, R.M.; Pavanelli, C.A.; Bottino, M.A.; Soares, L.E.S.; Martin, A.A. Conversion degree of indirect resin composites and effect of thermocycling on their physical properties. J. Prosthodon. 2010, 19, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Ayatollahi, M.R.; Yahya, M.Y.; Karimzadeh, A.; Nikkhooyifar, M.; Ayob, A.B. Effects of temperature change and beverage on mechanical and tribological properties of dental restorative composites. Mat. Sci. Eng. C-Mater. 2015, 54, 69–75. [Google Scholar] [CrossRef]
- Mair, L.H. Wear in dentistry—Current terminology. J. Dent. 1992, 20, 140–144. [Google Scholar] [CrossRef]
- Mehl, C.; Scheibner, S.; Ludwig, K.; Kern, M. Wear of composite resin veneering materials and enamel in a chewing simulator. Dent. Mater. 2007, 23, 1382–1389. [Google Scholar] [CrossRef]
- Wang, R.; Bao, S.; Liu, F.; Jiang, X.; Zhang, Q.; Sun, B.; Zhu, M. Wear behavior of light-cured resin composites with bimodal silica nanostructures as fillers. Mater. Sci. Eng. C-Mater. Biol. Appl. 2012, 33, 4759–4766. [Google Scholar] [CrossRef]
- Turssi, C.P.; De Moraes Purquerio, B.; Serra, M.C. Wear of dental resin composites: Insights into underlying processes and assessment methods—A review. J. Biomed. Mater. Res. Part. B 2003, 65, 280–285. [Google Scholar] [CrossRef]
- Pieniak, D.; Walczak, A.; Niewczas, A.M. Comparative study of wear resistance of the composite with microhybrid structure and nanocomposite. Acta Mech. Autom. 2016, 10, 306–309. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin-based composite performance: Are there some things we can’t predict. Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef]
- Friedrich, K. Wear of reinforced polymers by different abrasive counterparts. In Friction and Wear of Polymer Composites; Friedrich, K., Ed.; Elsevier Science Publishers: Amsterdam, The Netherlands, 1986; pp. 258–281. [Google Scholar]
- Zwierzycki, W. Prognozowanie Niezawodności Zużywających Się Elementów Maszyn; ITeE (Biblioteka Problemów Eksploatacji): Poznań-Radom, Poland, 1998; p. 331. (In Polish) [Google Scholar]
- Truong, V.T.; Cock, D.J.; Padmanathan, N. Fatigue crack propagation in posterior dental composites and prediction of clinical wear. J. Appl. Biomater. 1990, 1, 21–30. [Google Scholar] [CrossRef]
- McKinney, J.E.; Wu, W. Relationship between subsurface damage and wear of dental restorative composites. J. Dent. Res. 1982, 61, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Marquis, P.M.; Shortall, A.C. Two-body in vitro wear study of some current dental composites and amalgams. J. Prostht. Dent. 1999, 82, 214–220. [Google Scholar] [CrossRef]
- Wieleba, W. Bezobsługowe Łozyska Ślizgowe z Polimerów Termoplastycznych; OWPWr: Wrocław, Poland, 2013; p. 274. (In Polish) [Google Scholar]
- de Souza, J.A.; Dolavale, L.C.; de Souza Camargo, S.A. Wear mechanisms of dental composite restorative materials by two different in-vitro methods. Mater. Res. 2013, 16, 333–340. [Google Scholar] [CrossRef]
- Pieniak, D.; Niewczas, A. Phenomenological evaluation of fatigue cracking of dental restorations under conditions of cyclic mechanical loads. Acta Bioeng. Biomech. 2012, 14, 9–17. [Google Scholar] [PubMed]





| Parameter | Name of materials | ||
|---|---|---|---|
| Filtek Z550 (abbreviation: Z550) | Ex-nano (G) | Ex-flow (G) | |
| Manufacturer | 3M ESPE (USA) | – | – |
| Composite type | Nanohybrid composite | Nanocomposite | Semiliquid composite |
| Matrix (resin) | BIS-GMA, UDMA, BIS-EMA, PEGDMA, TEGDMA | BIS-GMA, UDMA, TEGDMA | BIS-GMA, UDMA, TEGDMA |
| Filler type | SiO2 (size: 20 nm), ZrO2/SiO2 nanoparticles (size: 5–20 nm) and ZrO2/SiO2 clusters (size: 0.6–1.4 mm) | The inorganic filler particles consist of barium aluminum, bore glass, highly dispersed silicon dioxide, and nanoparticles. | The inorganic filler particles comprise silica, dental glass (strontium aluminum boronsilicate glass), and nanoparticles. |
| Filler content (wt %) | 82% | 82% | 74% |
| Parameter | Characteristic value | Unit |
|---|---|---|
| Radius | 3 | mm |
| Linear speed (rotation speed) | 1.88 (60) | cm/s (rev/min) |
| Load | 5 | N |
| Distance travelled | 300 | m |
| Counterspecimen | Al2O3 ball (diameter: 6 mm) | - |
| Temperature | 37 | °C |
| Medium | artificial saliva | |
| Material | Average Values of the Friction Work (J) | |
|---|---|---|
| After Aging Only (0 TC) | After Thermal Fatigue Cycling (10,000 TCs) | |
| Filtek Z550 | 870.9 | 875.7 |
| Ex-nano(G) | 695.7 | 694.2 |
| Ex-flow(G) | 679.8 | 731.4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieniak, D.; Walczak, A.; Walczak, M.; Przystupa, K.; Niewczas, A.M. Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials 2020, 13, 1255. https://doi.org/10.3390/ma13051255
Pieniak D, Walczak A, Walczak M, Przystupa K, Niewczas AM. Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials. 2020; 13(5):1255. https://doi.org/10.3390/ma13051255
Chicago/Turabian StylePieniak, Daniel, Agata Walczak, Mariusz Walczak, Krzysztof Przystupa, and Agata M. Niewczas. 2020. "Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures" Materials 13, no. 5: 1255. https://doi.org/10.3390/ma13051255
APA StylePieniak, D., Walczak, A., Walczak, M., Przystupa, K., & Niewczas, A. M. (2020). Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials, 13(5), 1255. https://doi.org/10.3390/ma13051255







