Antitumor Efficacy of Focused Ultrasound-MFL Nanoparticles Combination Therapy in Mouse Breast Cancer Xenografts
Abstract
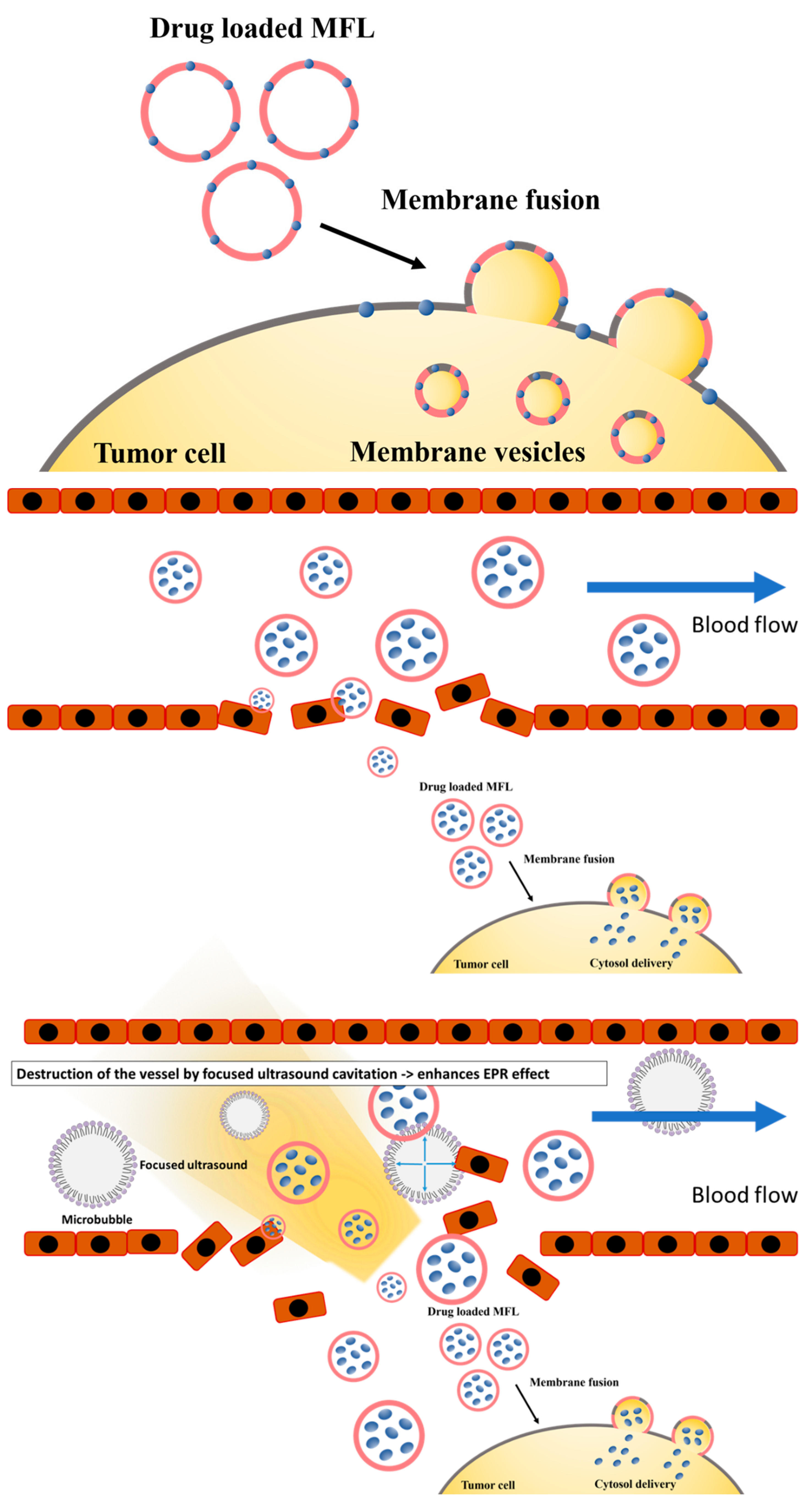
:1. Introduction
2. Materials and Method
2.1. Materials
2.2. Preparation of Docetaxel-Loaded MFLs
2.3. Characterization of MFLs
2.4. Cell Culture
2.5. In Vitro Fluorescence Cellular Imaging
2.6. Cell Viability-Assay
2.7. In Vivo Study
2.8. Focused Ultrasound (FUS) Treatment Parameters
2.9. Statistical Analysis
3. Results and Discussion
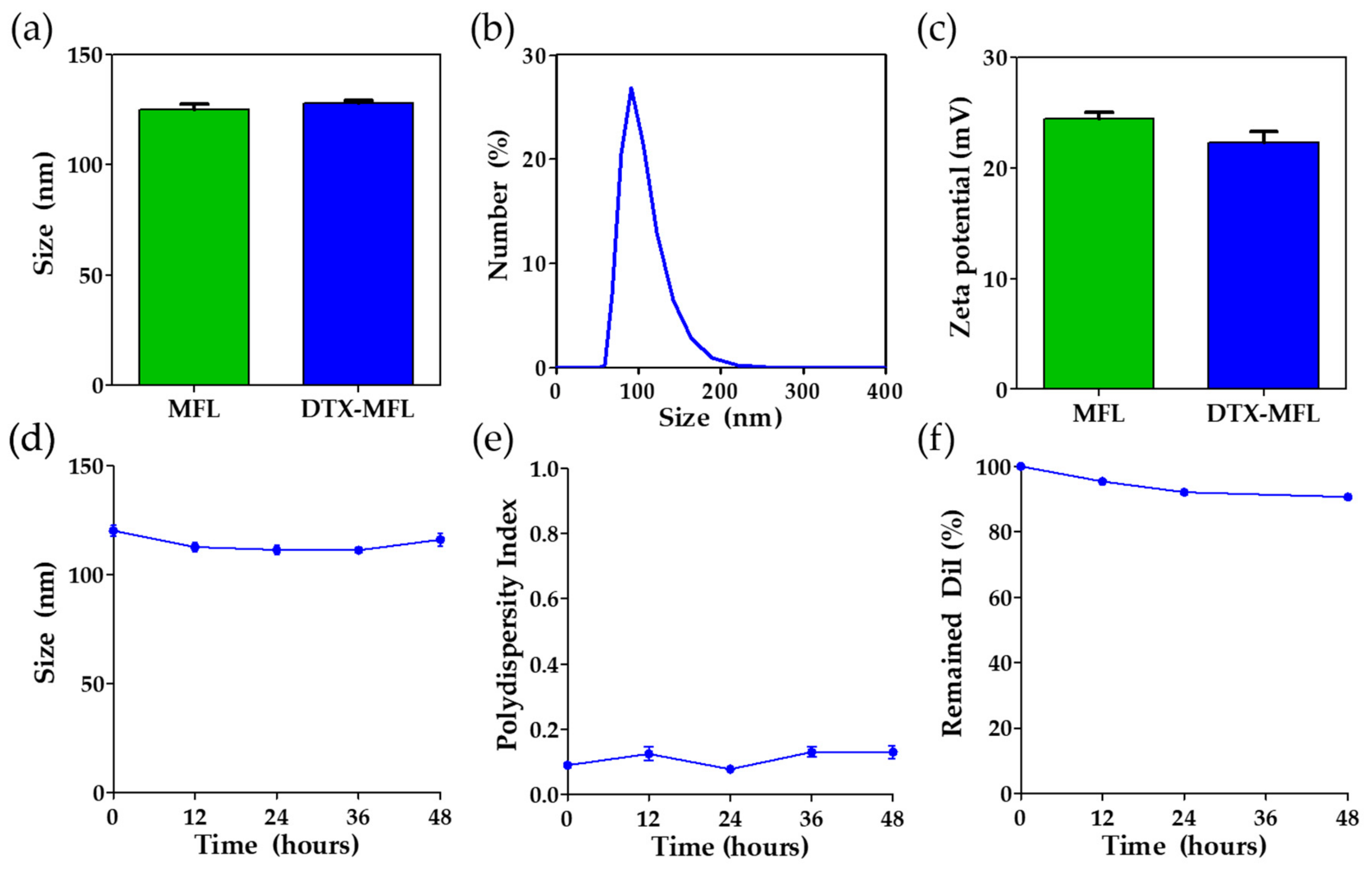
3.1. Characterization of MFLs
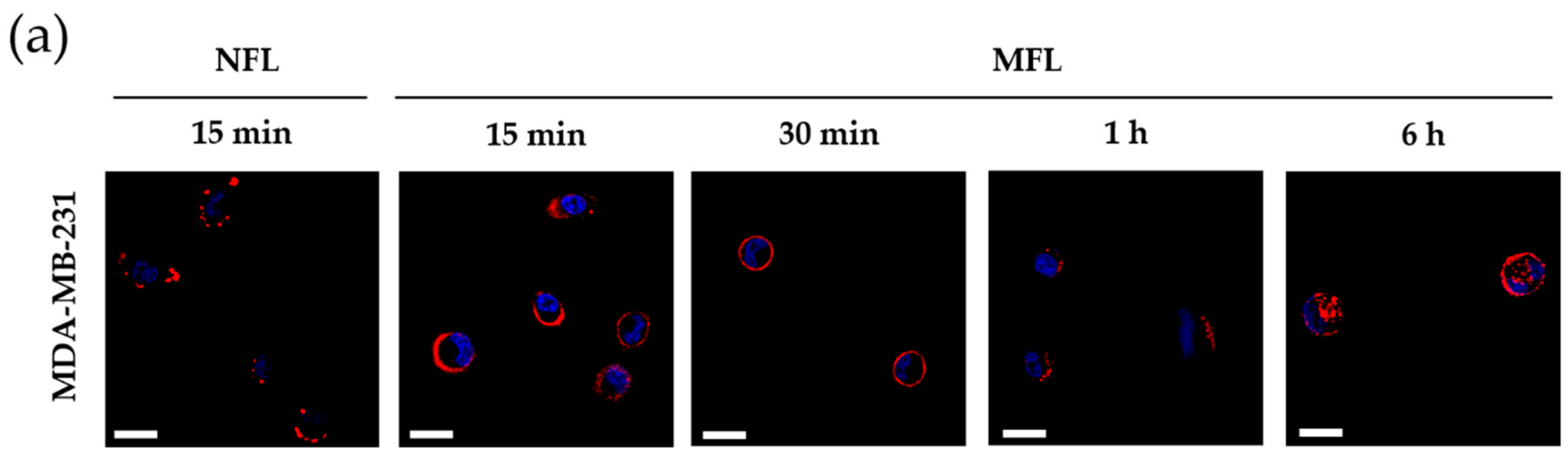
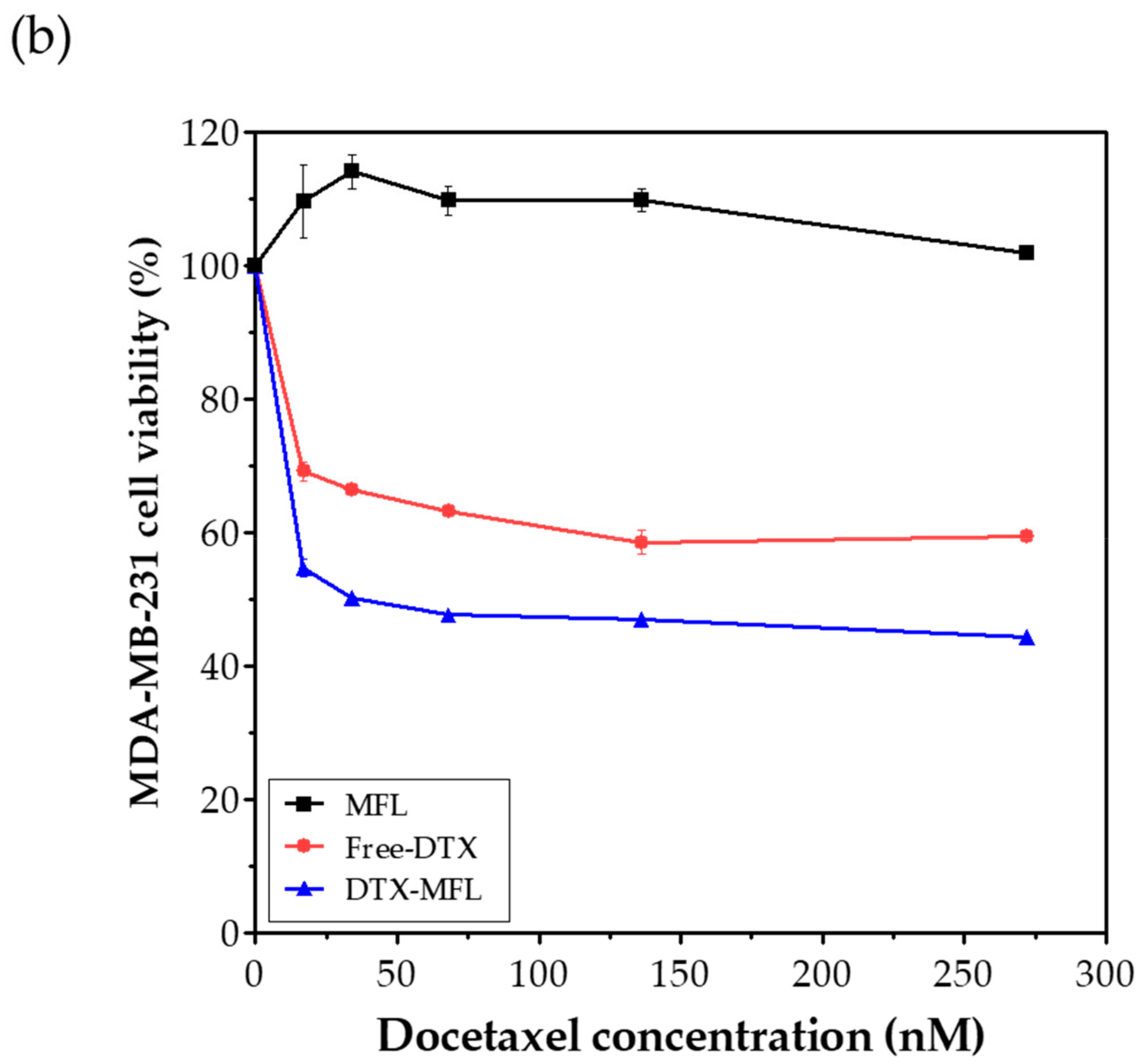
3.2. In Vitro Study
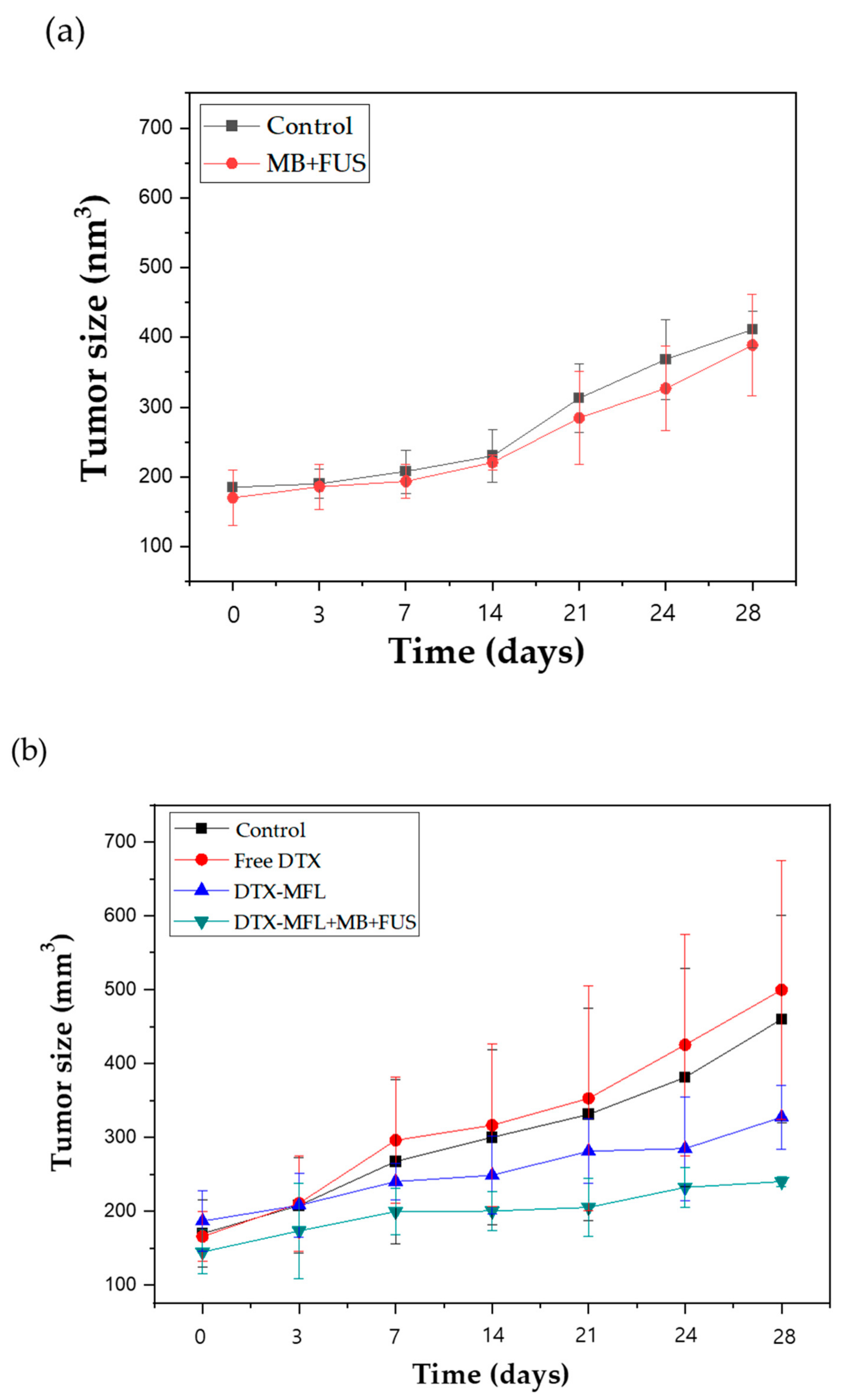
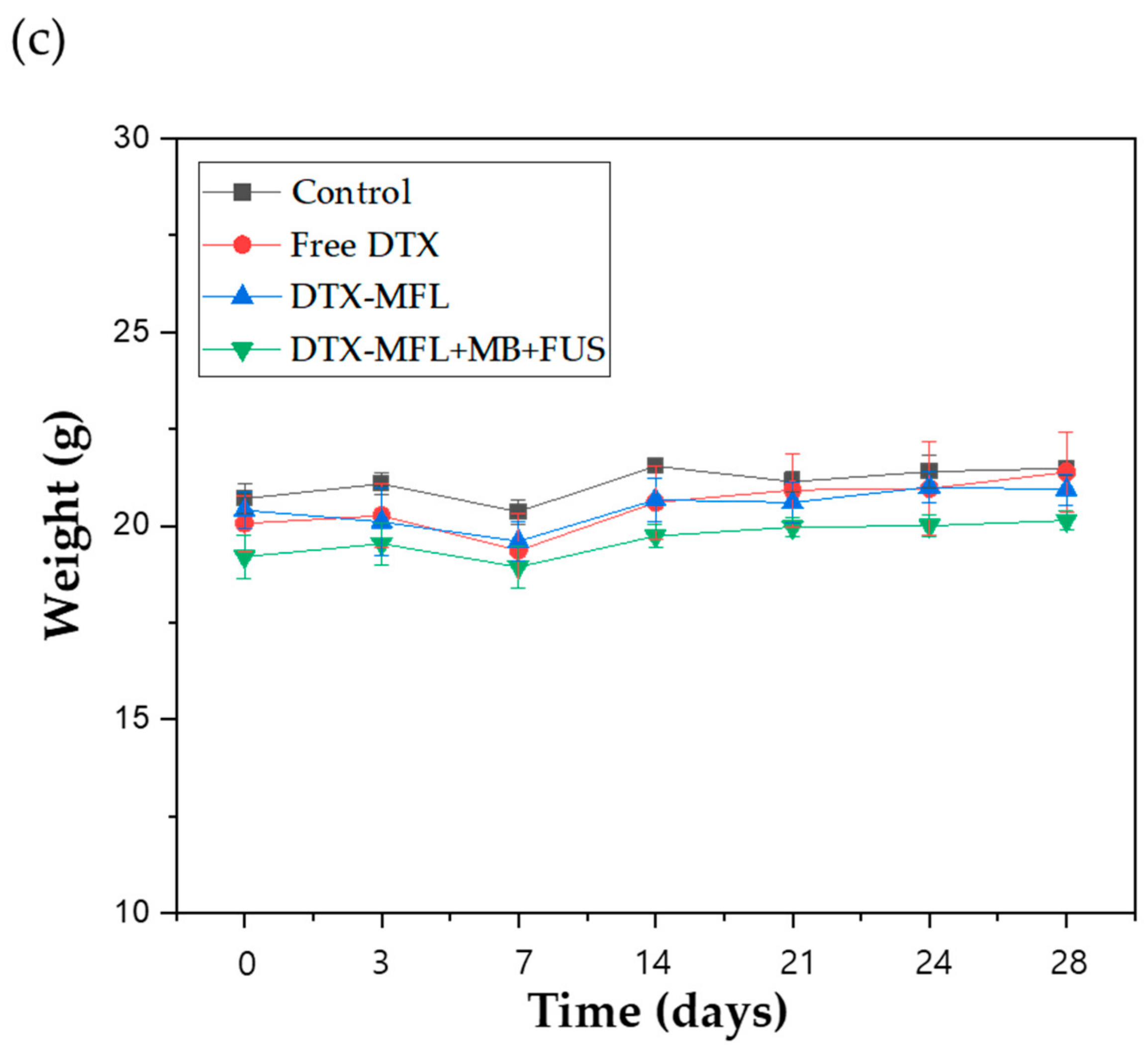
3.3. In Vivo Study
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- DeSantis, C.E.; Ma, J.; Goding Sauer, A.; Newman, L.A.; Jemal, A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J. Clin. 2017, 67, 439–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saika, K.; Sobue, T. Cancer statistics in the world. Gan to Kagaku ryoho. Cancer Chemother. 2013, 40, 2475–2480. [Google Scholar]
- Pruthi, S.; Brandt, K.R.; Degnim, A.C.; Goetz, M.P.; Perez, E.A.; Reynolds, C.A.; Schomberg, P.J.; Dy, G.K.; Ingle, J.N. A multidisciplinary approach to the management of breast cancer, part 1: Prevention and diagnosis. Mayo Clin. Proc. 2007, 82, 999–1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forbes, J.F. The incidence of breast cancer: The global burden, public health considerations. Semin. Oncol. 1997, 24, S20–S35. [Google Scholar]
- Stewart, B.W.; Kleihues, P. World Cancer Report; International Agency for Research on Cancer: Lyon, France, 2003. [Google Scholar]
- Jaiyesimi, I.A.; Buzdar, A.U.; Hortobagyi, G. Inflammatory breast cancer: A review. J. Clin. Oncol. 1992, 10, 1014–1024. [Google Scholar] [CrossRef]
- Woo, J.C.; Yu, T.; Hurd, T.C. Breast cancer in pregnancy: A literature review. Arch. Surg. 2003, 138, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Smith, I.C.; Heys, S.D.; Hutcheon, A.W.; Miller, I.D.; Payne, S.; Gilbert, F.J.; Ah-See, A.K.; Eremin, O.; Walker, L.G.; Sarkar, T.K.; et al. Neoadjuvant chemotherapy in breast cancer: Significantly enhanced response with docetaxel. J. Clin. Oncol. 2002, 20, 1456–1466. [Google Scholar] [CrossRef]
- Cortes, J.E.; Pazdur, R. Docetaxel. J. Clin. Oncol. 1995, 13, 2643–2655. [Google Scholar] [CrossRef]
- Nabholtz, J.M.; Falkson, C.; Campos, D.; Szanto, J.; Martin, M.; Chan, S.; Pienkowski, T.; Zaluski, J.; Pinter, T.; Krzakowski, M. Docetaxel and doxorubicin compared with doxorubicin and cyclophosphamide as first-line chemotherapy for metastatic breast cancer: Results of a randomized, multicenter, phase III trial. J. Clin. Oncol. 2003, 21, 968–975. [Google Scholar] [CrossRef]
- Keam, B.; Im, S.A.; Kim, H.J.; Oh, D.Y.; Kim, J.H.; Lee, S.H.; Chie, E.K.; Han, W.; Kim, D.W.; Moon, W.K. Prognostic impact of clinicopathologic parameters in stage II/III breast cancer treated with neoadjuvant docetaxel and doxorubicin chemotherapy: Paradoxical features of the triple negative breast cancer. BMC Cancer 2007, 7, 203. [Google Scholar] [CrossRef] [Green Version]
- Tsai, S.M.; Lin, C.Y.; Wu, S.H.; Hou, L.A.; Ma, H.; Tsai, L.Y.; Hou, M.F. Side effects after docetaxel treatment in Taiwanese breast cancer patients with CYP3A4, CYP3A5, and ABCB1 gene polymorphisms. Clin. Chim. Acta 2009, 404, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Engels, F.K.; Mathot, R.A.; Verweij, J. Alternative drug formulations of docetaxel: A review. Anticancer Drugs 2007, 18, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Ding, Y.; Zhang, L.; Qian, X.; Jiang, X.; Liu, B. Novel thermosensitive polymeric micelles for docetaxel delivery. J. Biomed. Mater. Res. A 2007, 81, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Zhang, H.; He, W.; Zhao, D.; Song, A. Luan Y Disulfide-linked amphiphilic polymer-docetaxel conjugates assembled redox-sensitive micelles for efficient antitumor drug delivery. Biomacromolecules 2016, 17, 1621–1632. [Google Scholar] [CrossRef] [PubMed]
- Csiszár, A.; Hersch, N.; Dieluweit, S.; Biehl, R.; Merke, R.; Hoffmann, B. Novel fusogenic liposomes for fluorescent cell labeling and membrane modification. Bioconjug. Chem. 2010, 21, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, H.; Goh, U.; Kim, J.; Jeong, M.; Lee, J.; Park, J.H. Cellular engineering with membrane fusogenic liposomes to produce functionalized extracellular vesicles. ACS Appl. Mater. Interfaces 2016, 8, 6790–6795. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.; Jeong, M.; Lee, H.; Goh, U.; Kim, H.; Kim, B.; Park, J.H. Liposome-based engineering of cells to package hydrophobic compounds in membrane vesicles for tumor penetration. Nano Lett. 2015, 15, 2938–2944. [Google Scholar] [CrossRef]
- Kang, J.; Wu, X.; Wang, Z.; Ran, H.; Xu, C.; Wu, J.; Wang, Z.; Zhang, Y. Antitumor effect of docetaxel-loaded lipid microbubbles combined with ultrasound-targeted microbubble activation on VX2 rabbit liver tumors. J. Ultrasound Med. 2010, 29, 61–70. [Google Scholar] [CrossRef]
- Moghimi, S.M.; Hunter, A.C.; Murray, J.C. Long-circulating and target-specific nanoparticles: Theory to practice. Pharmacol. Rev. 2001, 53, 283–318. [Google Scholar]
- Vancraeynest, D.; Havaux, X.; Pouleur, A.C.; Pasquet, A.; Gerber, B.; Beauloye, C.; Rafter, P.; Bertrand, L.; Vanoverschelde, J.L. Myocardial delivery of colloid nanoparticles using ultrasound-targeted microbubble destruction. Eur. Heart. J. 2005, 27, 237–245. [Google Scholar] [CrossRef] [Green Version]
- Zarnitsyn, V.; Rostad, C.A.; Prausnitz, M.R. Modeling transmembrane transport through cell membrane wounds created by acoustic cavitation. Biophys. J. 2008, 95, 4124–4138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lentacker, I.; Geers, B.; Demeester, J.; De Smedt, S.C.; Sanders, N.N. Design and evaluation of doxorubicin-containing microbubbles for ultrasound-triggered doxorubicin delivery: Cytotoxicity and mechanisms involved. Mol. Ther. 2010, 18, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Yin, T.; Wang, P.; Li, J.; Zheng, R.; Zheng, B.; Cheng, D.; Li, R.; Lai, J.; Shuai, X. Ultrasound-sensitive siRNA-loaded nanobubbles formed by hetero-assembly of polymeric micelles and liposomes and their therapeutic effect in gliomas. Biomaterials 2013, 34, 4532–4543. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.; Khokhlova, V.A.; Sapozhnikov, O.A.; Kargl, S.G. Physical mechanisms of the therapeutic effect of ultrasound (a review). Acoust. Phys. 2003, 49, 369–388. [Google Scholar] [CrossRef]
| Full Name | Abbreviation | Lipid Chain | Transition Temperature | Structure |
|---|---|---|---|---|
| 1,2-dimyristoyl-sn-glycerol-3-phosphocholine | DMPC | 14:0 | 24 °C | 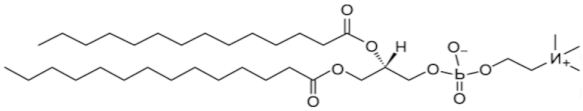 |
| 1,2-dioleoyl-3-trimethlammonium-propane | DOTAP | 18:1 | <5 °C | 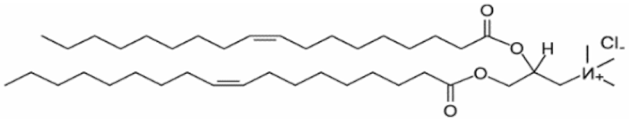 |
| 1,2-distearoyl-sn-glycerol-3-phosphoethanolamine-N-[methoxy(polyethylene glycol)-2000] | DSPE- mPEG(2000) | 18:0 | 12.8 °C | 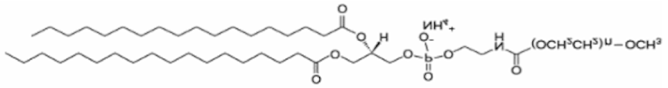 |
| Lipid Composition (Molar Ratio) | |||||
|---|---|---|---|---|---|
| Nanoparticle | DMPC | DOTAP | DSPE- mPEG(2000) | Docetaxel | Drug Loading Efficiency (%) |
| NFL | 80 | 20 | 0 | — | — |
| MFL | 76.15 | 20 | 3.85 | — | — |
| DTX-MFL | 76.15 | 20 | 3.85 | 0.05 | 55.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.; Han, J.; Park, S.Y.; Kim, H.; Park, J.-H.; Lee, H.J. Antitumor Efficacy of Focused Ultrasound-MFL Nanoparticles Combination Therapy in Mouse Breast Cancer Xenografts. Materials 2020, 13, 1099. https://doi.org/10.3390/ma13051099
Kim D, Han J, Park SY, Kim H, Park J-H, Lee HJ. Antitumor Efficacy of Focused Ultrasound-MFL Nanoparticles Combination Therapy in Mouse Breast Cancer Xenografts. Materials. 2020; 13(5):1099. https://doi.org/10.3390/ma13051099
Chicago/Turabian StyleKim, Daehyun, Junhee Han, So Yeon Park, Heegon Kim, Ji-Ho Park, and Hak Jong Lee. 2020. "Antitumor Efficacy of Focused Ultrasound-MFL Nanoparticles Combination Therapy in Mouse Breast Cancer Xenografts" Materials 13, no. 5: 1099. https://doi.org/10.3390/ma13051099
APA StyleKim, D., Han, J., Park, S. Y., Kim, H., Park, J.-H., & Lee, H. J. (2020). Antitumor Efficacy of Focused Ultrasound-MFL Nanoparticles Combination Therapy in Mouse Breast Cancer Xenografts. Materials, 13(5), 1099. https://doi.org/10.3390/ma13051099








