Biological Reactions to Metal Particles and Ions in the Synovial Layer of Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Metal Particle/Ion Generation
2.2. Elimination of Endotoxin
2.3. Animals and Intraarticular Injection
2.4. Immunohistochemistry
2.5. Statistics
3. Results
3.1. Characterization of Metal Particles and Ions
3.2. Results of the Left Knee Joints
3.2.1. Expression of TNF-α, IL-1β and IL-6
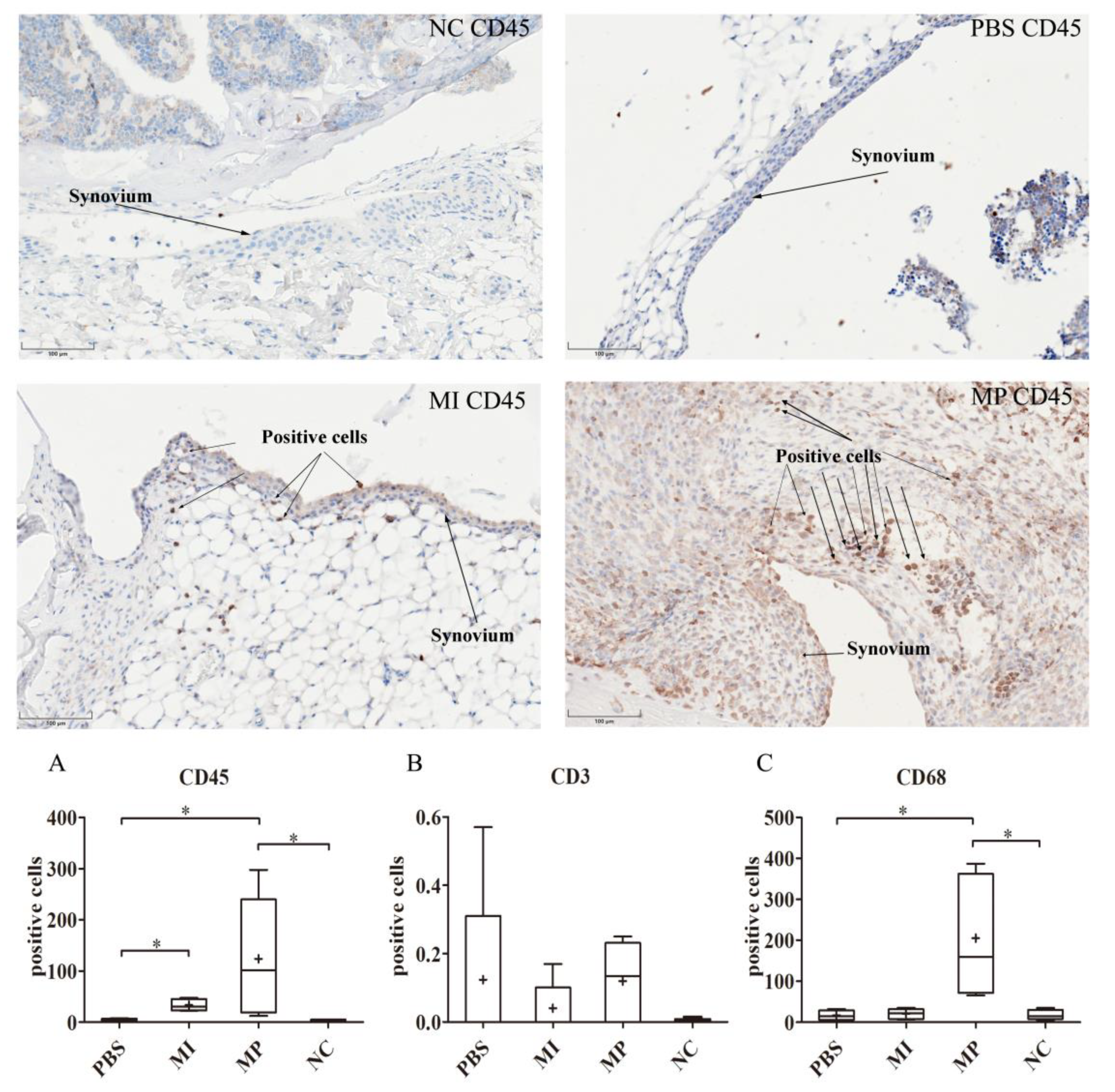
3.2.2. Expression of CD68, CD3 and CD45
3.3. Results of the Right Knee Joints
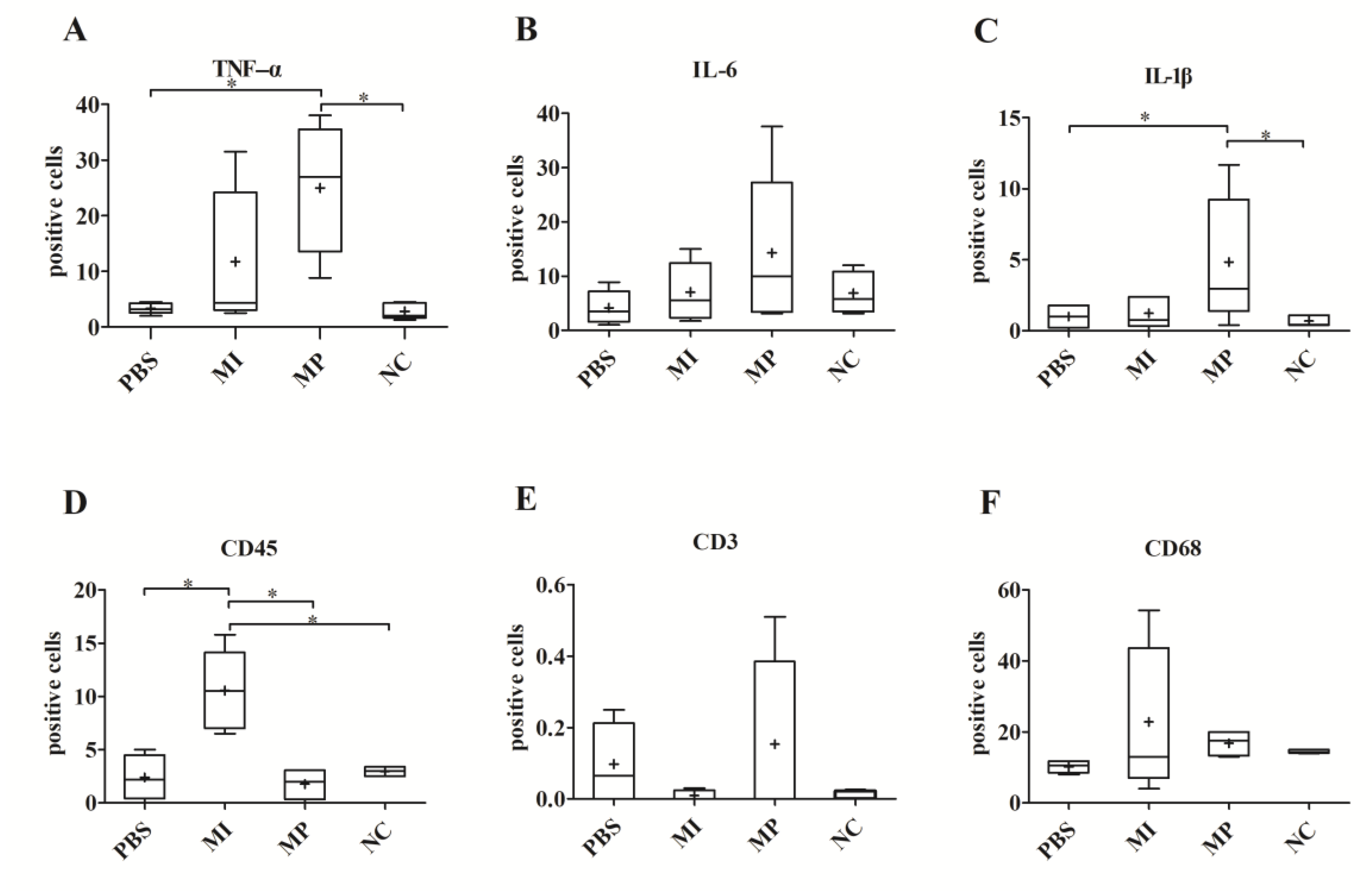
3.3.1. Expression of TNF-α, IL-1β and IL-6
3.3.2. Expression of CD68, CD3 and CD45
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Eliaz, N. Corrosion of Metallic Biomaterials: A Review. Materials 2019, 12, 407. [Google Scholar] [CrossRef] [Green Version]
- Catelas, I.; Bobyn, J.D.; Medley, J.B.; Krygier, J.J.; Zukor, D.J.; Huk, O.L. Size, shape, and composition of wear particles from metal-metal hip simulator testing: Effects of alloy and number of loading cycles. J. Biomed. Mater. Res. A 2003, 67, 312–327. [Google Scholar] [CrossRef]
- Merola, M.; Affatato, S. Materials for Hip Prostheses: A Review of Wear and Loading Considerations. Materials 2019, 12, 495. [Google Scholar] [CrossRef] [Green Version]
- Grieco, P.W.; Pascal, S.; Newman, J.M.; Shah, N.V.; Stroud, S.G.; Sheth, N.P.; Maheshwari, A.V. New alternate bearing surfaces in total hip arthroplasty: A review of the current literature. J. Clin. Orthop. Trauma 2018, 9, 7–16. [Google Scholar] [CrossRef]
- Xu, J.; Yang, J.; Nyga, A.; Ehteramyan, M.; Moraga, A.; Wu, Y.; Zeng, L.; Knight, M.M.; Shelton, J.C. Cobalt (II) ions and nanoparticles induce macrophage retention by ROS-mediated down-regulation of RhoA expression. Acta Biomater. 2018, 72, 434–446. [Google Scholar] [CrossRef]
- Sidaginamale, R.P.; Joyce, T.J.; Bowsher, J.G.; Lord, J.K.; Avery, P.J.; Natu, S.; Nargol, A.V.; Langton, D.J. The clinical implications of metal debris release from the taper junctions and bearing surfaces of metal-on-metal hip arthroplasty: Joint fluid and blood metal ion concentrations. Bone Jt. J. 2016, 98, 925–933. [Google Scholar] [CrossRef]
- Kretzer, J.P.; Mueller, U.; Streit, M.R.; Kiefer, H.; Sonntag, R.; Streicher, R.M.; Reinders, J. Ion release in ceramic bearings for total hip replacement: Results from an in vitro and an in vivo study. Int. Orthop. 2018, 42, 65–70. [Google Scholar] [CrossRef]
- Utzschneider, S.; Paulus, A.; Datz, J.C.; Schroeder, C.; Sievers, B.; Wegener, B.; Jansson, V. Influence of design and bearing material on polyethylene wear particle generation in total knee replacement. Acta Biomater. 2009, 5, 2495–2502. [Google Scholar] [CrossRef]
- Pourzal, R.; Catelas, I.; Theissmann, R.; Kaddick, C.; Fischer, A. Characterization of Wear Particles Generated from CoCrMo Alloy under Sliding Wear Conditions. Wear 2011, 271, 1658–1666. [Google Scholar] [CrossRef] [Green Version]
- Sansone, V.; Pagani, D.; Melato, M. The effects on bone cells of metal ions released from orthopaedic implants. A review. Clin. Cases Miner. Bone Metab. 2013, 10, 34–40. [Google Scholar] [CrossRef]
- Yu, F.Y.; Xie, C.Q.; Sun, J.T.; Peng, W.; Huang, X.W. Overexpressed miR-145 inhibits osteoclastogenesis in RANKL-induced bone marrow-derived macrophages and ovariectomized mice by regulation of Smad3. Life Sci. 2018, 202, 11–20. [Google Scholar] [CrossRef]
- Gallo, J.; Vaculova, J.; Goodman, S.B.; Konttinen, Y.T.; Thyssen, J.P. Contributions of human tissue analysis to understanding the mechanisms of loosening and osteolysis in total hip replacement. Acta Biomater. 2014, 10, 2354–2366. [Google Scholar] [CrossRef] [Green Version]
- Pajarinen, J.; Jamsen, E.; Konttinen, Y.T.; Goodman, S.B. Innate immune reactions in septic and aseptic osteolysis around hip implants. J. Long Term Eff. Med. Implants 2014, 24, 283–296. [Google Scholar] [CrossRef] [Green Version]
- Campbell, P.; Ebramzadeh, E.; Nelson, S.; Takamura, K.; De Smet, K.; Amstutz, H.C. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin. Orthop. Relat. Res. 2010, 468, 2321–2327. [Google Scholar] [CrossRef] [Green Version]
- Mao, X.; Tay, G.H.; Godbolt, D.B.; Crawford, R.W. Pseudotumor in a well-fixed metal-on-polyethylene uncemented hip arthroplasty. J. Arthroplast. 2012, 27, 493.e13. [Google Scholar] [CrossRef]
- Goodman, S.B. Wear particles, periprosthetic osteolysis and the immune system. Biomaterials 2007, 28, 5044–5048. [Google Scholar] [CrossRef] [Green Version]
- Granchi, D.; Savarino, L.M.; Ciapetti, G.; Baldini, N. Biological effects of metal degradation in hip arthroplasties. Crit. Rev. Toxicol. 2018, 48, 170–193. [Google Scholar] [CrossRef]
- Granchi, D.; Savarino, L.; Ciapetti, G.; Cenni, E.; Rotini, R.; Mieti, M.; Baldini, N.; Giunti, A. Immunological changes in patients with primary osteoarthritis of the hip after total joint replacement. J. Bone Jt. Surg. Br. 2003, 85, 758–764. [Google Scholar] [CrossRef]
- Konttinen, Y.T.; Pajarinen, J. Adverse reactions to metal-on-metal implants. Nat. Rev. Rheumatol. 2013, 9, 5–6. [Google Scholar] [CrossRef]
- Gallo, J.; Goodman, S.B.; Konttinen, Y.T.; Wimmer, M.A.; Holinka, M. Osteolysis around total knee arthroplasty: A review of pathogenetic mechanisms. Acta Biomater. 2013, 9, 8046–8058. [Google Scholar] [CrossRef] [Green Version]
- Abu-Amer, Y.; Darwech, I.; Clohisy, J.C. Aseptic loosening of total joint replacements: Mechanisms underlying osteolysis and potential therapies. Arthritis. Res. Ther. 2007, 9 (Suppl. 1), S6. [Google Scholar] [CrossRef] [Green Version]
- De Smet, K.; De Haan, R.; Calistri, A.; Campbell, P.A.; Ebramzadeh, E.; Pattyn, C.; Gill, H.S. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J. Bone Jt. Surg. Am. 2008, 90 (Suppl. 4), 202–208. [Google Scholar] [CrossRef] [Green Version]
- Posada, O.M.; Tate, R.J.; Grant, M.H. Toxicity of cobalt-chromium nanoparticles released from a resurfacing hip implant and cobalt ions on primary human lymphocytes in vitro. J. Appl. Toxicol. 2015, 35, 614–622. [Google Scholar] [CrossRef] [Green Version]
- Lin, T.H.; Tamaki, Y.; Pajarinen, J.; Waters, H.A.; Woo, D.K.; Yao, Z.; Goodman, S.B. Chronic inflammation in biomaterial-induced periprosthetic osteolysis: NF-kappaB as a therapeutic target. Acta Biomater. 2014, 10, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Tchilian, E.Z.; Beverley, P.C. CD45 in memory and disease. Arch. Immunol. Ther. Exp. 2002, 50, 85–93. [Google Scholar]
- Hermiston, M.L.; Xu, Z.; Weiss, A. CD45: A critical regulator of signaling thresholds in immune cells. Annu. Rev. Immunol. 2003, 21, 107–137. [Google Scholar] [CrossRef]
- Martin-Romero, C.; Santos-Alvarez, J.; Goberna, R.; Sanchez-Margalet, V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell. Immunol. 2000, 199, 15–24. [Google Scholar] [CrossRef]
- Xu, W.; Holzhuter, G.; Sorg, H.; Wolter, D.; Lenz, S.; Gerber, T.; Vollmar, B. Early matrix change of a nanostructured bone grafting substitute in the rat. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 91, 692–699. [Google Scholar] [CrossRef]
- Ramprasad, M.P.; Terpstra, V.; Kondratenko, N.; Quehenberger, O.; Steinberg, D. Cell surface expression of mouse macrosialin and human CD68 and their role as macrophage receptors for oxidized low density lipoprotein. Proc. Natl. Acad. Sci. USA 1996, 93, 14833–14838. [Google Scholar] [CrossRef] [Green Version]
- Reinders, J.; Sonntag, R.; Vot, L.; Gibney, C.; Nowack, M.; Kretzer, J.P. Wear testing of moderate activities of daily living using in vivo measured knee joint loading. PLoS ONE 2015, 10, e0123155. [Google Scholar] [CrossRef] [Green Version]
- Schroder, C.; Reinders, J.; Zietz, C.; Utzschneider, S.; Bader, R.; Kretzer, J.P. Characterization of polyethylene wear particle: The impact of methodology. Acta Biomater. 2013, 9, 9485–9491. [Google Scholar] [CrossRef]
- Jonitz-Heincke, A.; Tillmann, J.; Klinder, A.; Krueger, S.; Kretzer, J.P.; Hol, P.J.; Paulus, A.C.; Bader, R. The Impact of Metal Ion Exposure on the Cellular Behavior of Human Osteoblasts and PBMCs: In Vitro Analyses of Osteolytic Processes. Materials 2017, 10, 734. [Google Scholar] [CrossRef] [Green Version]
- Holt, G.; Murnaghan, C.; Reilly, J.; Meek, R.M. The biology of aseptic osteolysis. Clin. Orthop. Relat. Res. 2007, 460, 240–252. [Google Scholar] [CrossRef]
- Al Saffar, N.; Revell, P.A. Interleukin-1 production by activated macrophages surrounding loosened orthopaedic implants: A potential role in osteolysis. Br. J. Rheumatol. 1994, 33, 309–316. [Google Scholar] [CrossRef]
- Utzschneider, S.; Becker, F.; Grupp, T.M.; Sievers, B.; Paulus, A.; Gottschalk, O.; Jansson, V. Inflammatory response against different carbon fiber-reinforced PEEK wear particles compared with UHMWPE in vivo. Acta Biomater. 2010, 6, 4296–4304. [Google Scholar] [CrossRef]
- Smith, A.J.; Dieppe, P.; Vernon, K.; Porter, M.; Blom, A.W. Failure rates of stemmed metal-on-metal hip replacements: Analysis of data from the National Joint Registry of England and Wales. Lancet 2012, 379, 1199–1204. [Google Scholar] [CrossRef]
- Lorber, V.; Paulus, A.C.; Buschmann, A.; Schmitt, B.; Grupp, T.M.; Jansson, V.; Utzschneider, S. Elevated cytokine expression of different PEEK wear particles compared to UHMWPE in vivo. J. Mater. Sci. Mater. Med. 2014, 25, 141–149. [Google Scholar] [CrossRef]
- Paulus, A.C.; Frenzel, J.; Ficklscherer, A.; Rossbach, B.P.; Melcher, C.; Jansson, V.; Utzschneider, S. Polyethylene wear particles induce TLR 2 upregulation in the synovial layer of mice. J. Mater. Sci. Mater. Med. 2014, 25, 507–513. [Google Scholar] [CrossRef]
- Utzschneider, S.; Lorber, V.; Dedic, M.; Paulus, A.C.; Schroder, C.; Gottschalk, O.; Schmitt-Sody, M.; Jansson, V. Biological activity and migration of wear particles in the knee joint: An in vivo comparison of six different polyethylene materials. J. Mater. Sci. Mater. Med. 2014, 25, 1599–1612. [Google Scholar] [CrossRef]
- Klinder, A.; Seyfarth, A.; Hansmann, D.; Bader, R.; Jonitz-Heincke, A. Inflammatory Response of Human Peripheral Blood Mononuclear Cells and Osteoblasts Incubated With Metallic and Ceramic Submicron Particles. Front. Immunol. 2018, 9, 831. [Google Scholar] [CrossRef] [Green Version]
- Kraft, C.N.; Diedrich, O.; Burian, B.; Schmitt, O.; Wimmer, M.A. Microvascular response of striated muscle to metal debris. A comparative in vivo study with titanium and stainless steel. J. Bone Jt. Surg. Br. 2003, 85, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Anabtawi, M.; Beck, P.; Lemons, J. Biocompatibility testing of simulated total joint arthoplasty articulation debris. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 84, 478–485. [Google Scholar] [CrossRef]
- Tchilian, E.Z.; Beverley, P.C. Altered CD45 expression and disease. Trends Immunol. 2006, 27, 146–153. [Google Scholar] [CrossRef]
- Bijukumar, D.R.; Segu, A.; Souza, J.C.; Li, X.; Barba, M.; Mercuri, L.G.; Jacobs, J.J.; Mathew, M.T. Systemic and local toxicity of metal debris released from hip prostheses: A review of experimental approaches. Nanomedicine 2018, 14, 951–963. [Google Scholar] [CrossRef]
- Delgado-Ruiz, R.; Romanos, G. Potential Causes of Titanium Particle and Ion Release in Implant Dentistry: A Systematic Review. Int. J. Mol. Sci. 2018, 19, 3585. [Google Scholar] [CrossRef] [Green Version]
- Haeri, M.; Wllert, T.; Langford, G.M.; Gilbert, J.L. Electrochemical control of cell death by reduction-induced intrinsic apoptosis and oxidation-induced necrosis on CoCrMo alloy in vitro. Biomaterials 2012, 33, 6295–6304. [Google Scholar] [CrossRef]
- Chamaon, K.; Schonfeld, P.; Awiszus, F.; Bertrand, J.; Lohmann, C.H. Ionic cobalt but not metal particles induces ROS generation in immune cells in vitro. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 1246–1253. [Google Scholar] [CrossRef]
- Hallab, N.J.; Jacobs, J.J. Biologic effects of implant debris. Bull. NYU Hosp. Jt. Dis. 2009, 67, 182–188. [Google Scholar]
- Caicedo, M.S.; Pennekamp, P.H.; McAllister, K.; Jacobs, J.J.; Hallab, N.J. Soluble ions more than particulate cobalt-alloy implant debris induce monocyte costimulatory molecule expression and release of proinflammatory cytokines critical to metal-induced lymphocyte reactivity. J. Biomed. Mater. Res. A 2010, 93, 1312–1321. [Google Scholar] [CrossRef]
- Caicedo, M.S.; Desai, R.; McAllister, K.; Reddy, A.; Jacobs, J.J.; Hallab, N.J. Soluble and particulate Co-Cr-Mo alloy implant metals activate the inflammasome danger signaling pathway in human macrophages: A novel mechanism for implant debris reactivity. J. Orthop. Res. 2009, 27, 847–854. [Google Scholar] [CrossRef]
- Pandit, H.; Vlychou, M.; Whitwell, D.; Crook, D.; Luqmani, R.; Ostlere, S.; Murray, D.W.; Athanasou, N.A. Necrotic granulomatous pseudotumours in bilateral resurfacing hip arthoplasties: Evidence for a type IV immune response. Virchows Arch. Int. J. Pathol. 2008, 453, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Dapunt, U.; Giese, T.; Prior, B.; Gaida, M.M.; Hansch, G.M. Infectious versus non-infectious loosening of implants: Activation of T lymphocytes differentiates between the two entities. Int. Orthop. 2014, 38, 1291–1296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warrington, R.; Watson, W.; Kim, H.L.; Antonetti, F.R. An introduction to immunology and immunopathology. Allergy Asthma Clin. Immunol. 2011, 7 (Suppl. 1), S1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burkandt, A.; Katzer, A.; Thaler, K.; Von Baehr, V.; Friedrich, R.E.; Ruther, W.; Amling, M.; Zustin, J. Proliferation of the synovial lining cell layer in suggested metal hypersensitivity. In Vivo 2011, 25, 679–686. [Google Scholar]
- Urban, R.M.; Tomlinson, M.J.; Hall, D.J.; Jacobs, J.J. Accumulation in liver and spleen of metal particles generated at nonbearing surfaces in hip arthroplasty. J. Arthroplast. 2004, 19 (Suppl. 3), 94–101. [Google Scholar] [CrossRef]
- Dinarello, C.A. Blocking IL-1 in systemic inflammation. J. Exp. Med. 2005, 201, 1355–1359. [Google Scholar] [CrossRef]
- Ma, T.; Huang, Z.; Ren, P.G.; McCally, R.; Lindsey, D.; Smith, R.L.; Goodman, S.B. An in vivo murine model of continuous intramedullary infusion of polyethylene particles. Biomaterials 2008, 29, 3738–3742. [Google Scholar] [CrossRef] [Green Version]

| Material | ECD | Aspect Ratio | Roundness |
|---|---|---|---|
| CoCr29Mo6 alloy | 61.25 ± 18.47nm | 1.69 ± 0.66 | 0.64 ± 0.16 |
| Content in | Co | Cr | Mo | Ni |
|---|---|---|---|---|
| stock solution | 12.0 ± 2.4 mg/L | 3.9 ± 0.6 mg/L | 0.9 ± 0.1 mg/L | 1.3 ± 0.6 mg/L |
| experimental solution | 120 ± 24 µg/L | 39 ± 5.7 µg/L | 8.8 ± 1.1 µg/L | 12.8 ± 6.0 µg/L |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, X.; Dirmeier, S.C.; Haßelt, S.; Baur-Melnyk, A.; Kretzer, J.P.; Bader, R.; Utzschneider, S.; Paulus, A.C. Biological Reactions to Metal Particles and Ions in the Synovial Layer of Mice. Materials 2020, 13, 1044. https://doi.org/10.3390/ma13051044
Cheng X, Dirmeier SC, Haßelt S, Baur-Melnyk A, Kretzer JP, Bader R, Utzschneider S, Paulus AC. Biological Reactions to Metal Particles and Ions in the Synovial Layer of Mice. Materials. 2020; 13(5):1044. https://doi.org/10.3390/ma13051044
Chicago/Turabian StyleCheng, Xiangyun, Sabine C. Dirmeier, Sandra Haßelt, Andrea Baur-Melnyk, Jan Philippe Kretzer, Rainer Bader, Sandra Utzschneider, and Alexander C. Paulus. 2020. "Biological Reactions to Metal Particles and Ions in the Synovial Layer of Mice" Materials 13, no. 5: 1044. https://doi.org/10.3390/ma13051044
APA StyleCheng, X., Dirmeier, S. C., Haßelt, S., Baur-Melnyk, A., Kretzer, J. P., Bader, R., Utzschneider, S., & Paulus, A. C. (2020). Biological Reactions to Metal Particles and Ions in the Synovial Layer of Mice. Materials, 13(5), 1044. https://doi.org/10.3390/ma13051044





