Mechanical, Histological, and Scanning Electron Microscopy Study of the Effect of Mixed-Acid and Heat Treatment on Additive-Manufactured Titanium Plates on Bonding to the Bone Surface
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Method
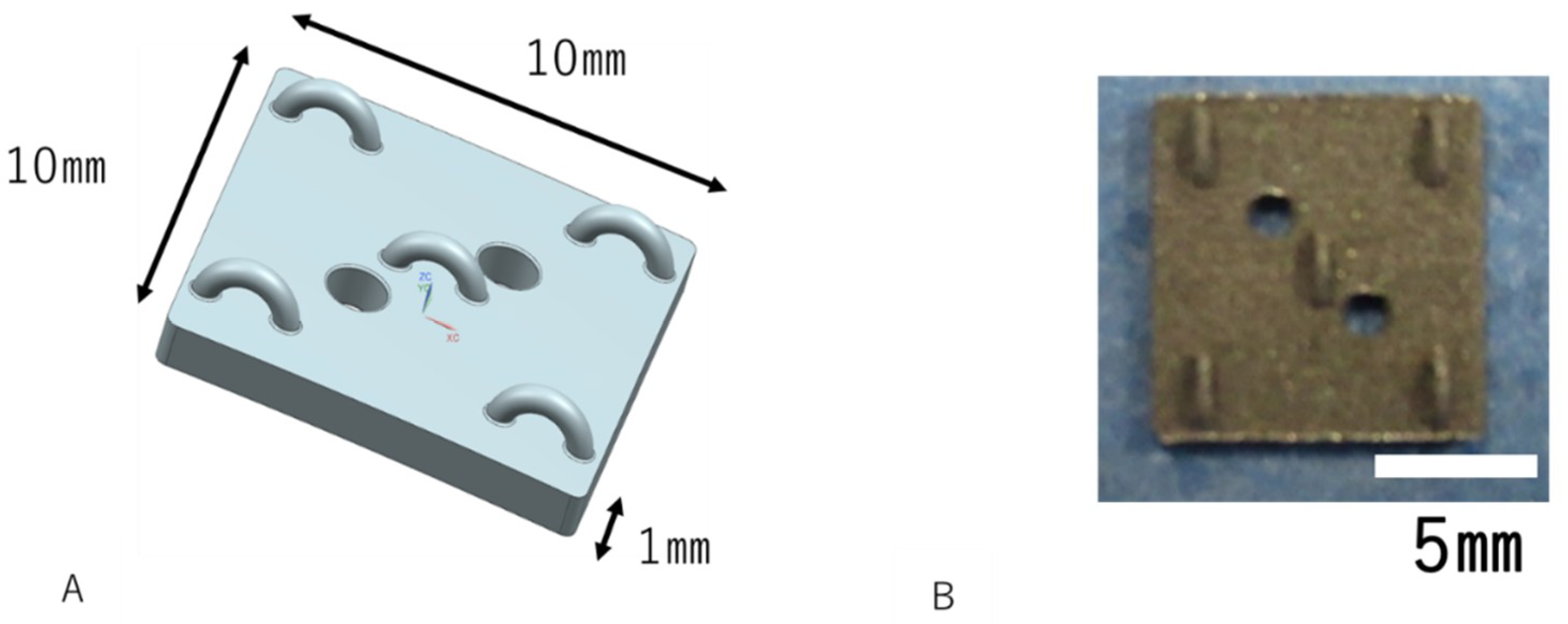
2.2. Design of the AM Ti Plate
2.3. Mixed-Acid and Heat Treatment
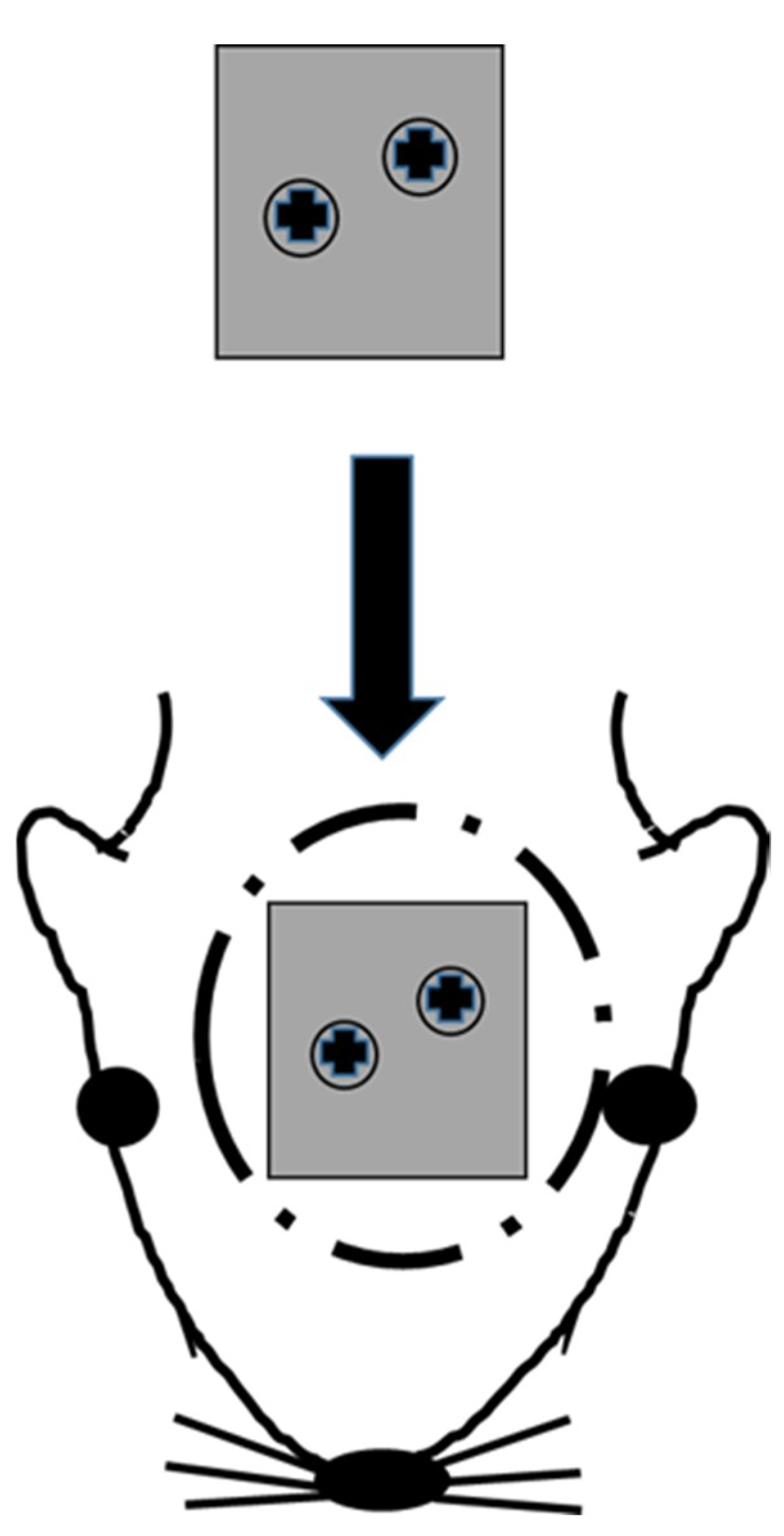
2.4. Implantation Technique
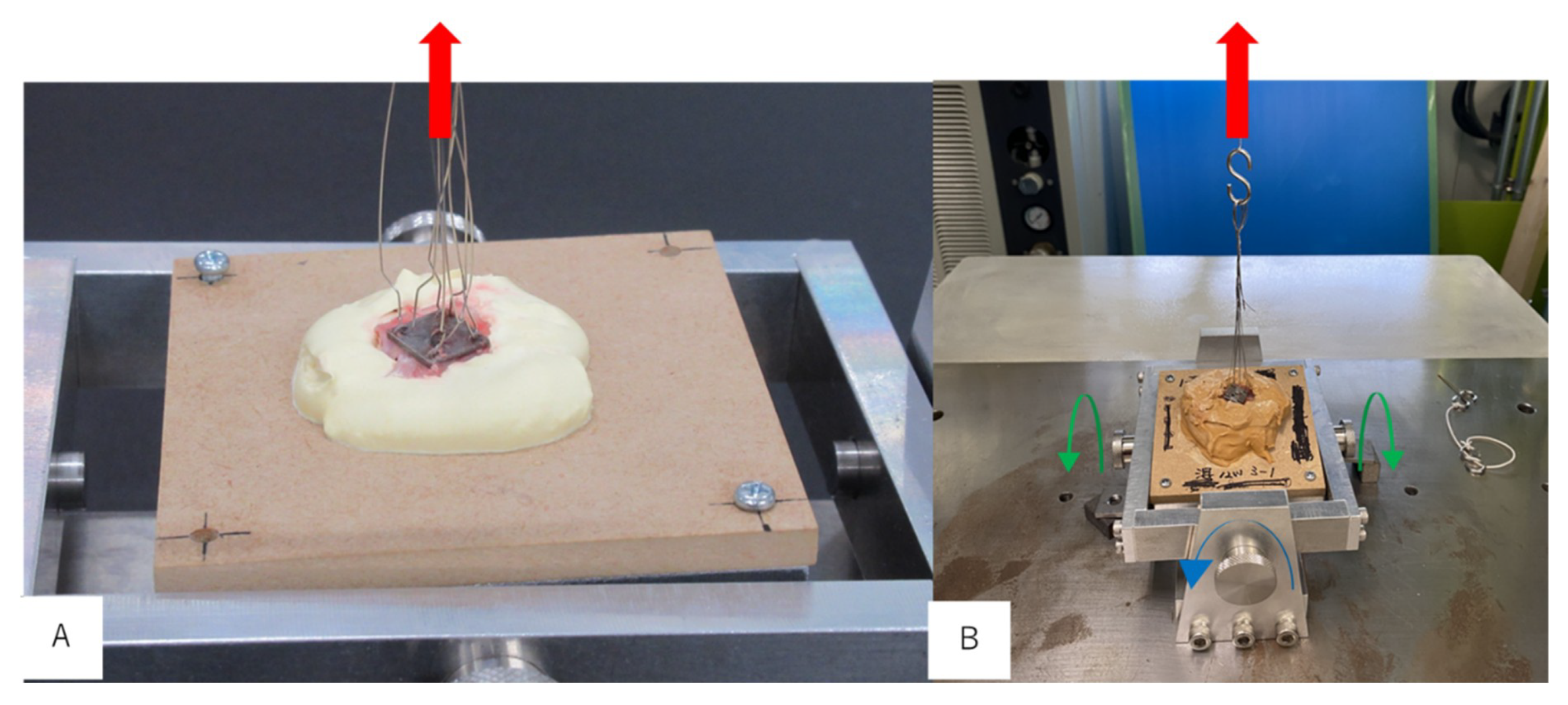
2.5. Evaluation of Bone Bonding
2.6. Scanning Electron Microscope Observation
2.7. Histological Observation
2.8. Statistical Analysis
3. Results
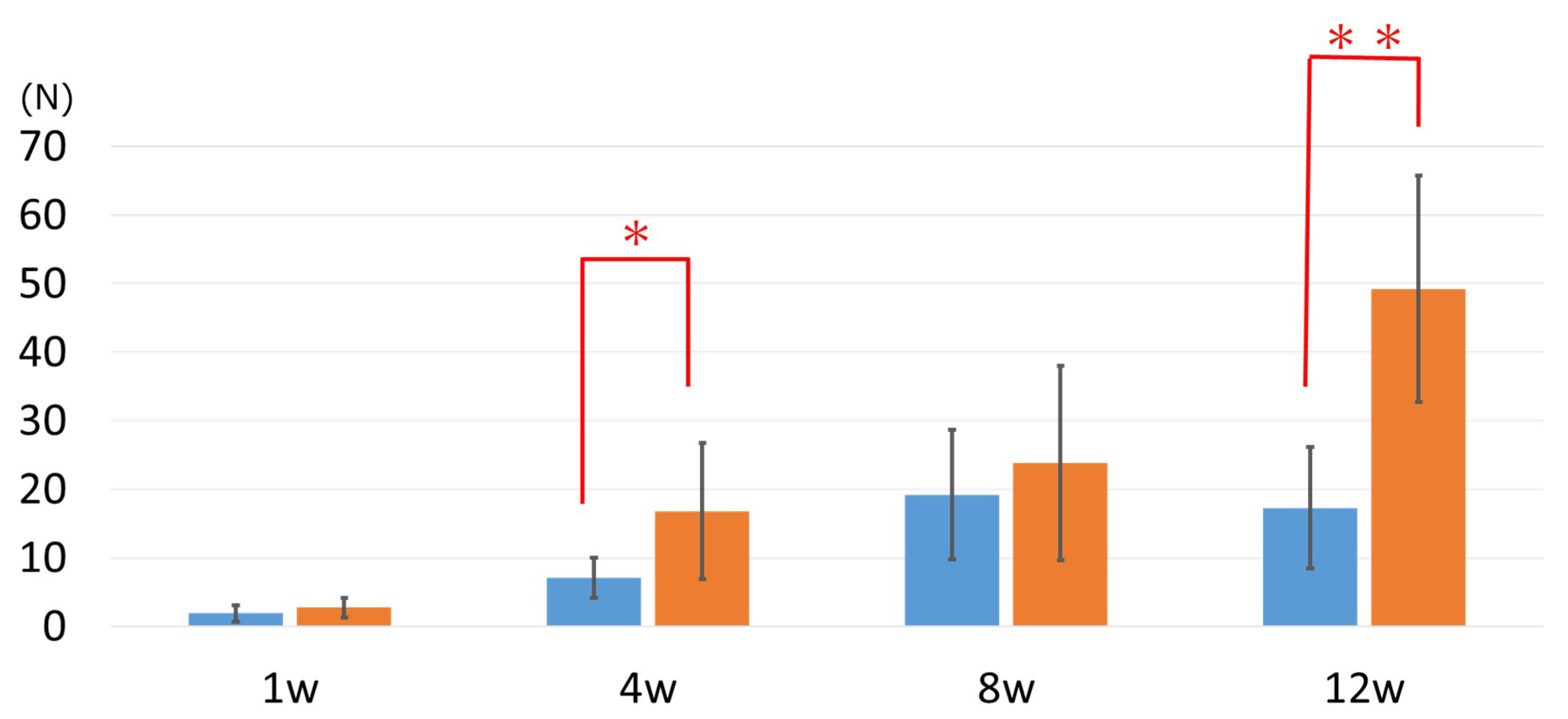
3.1. Evaluation of Bone Bonding
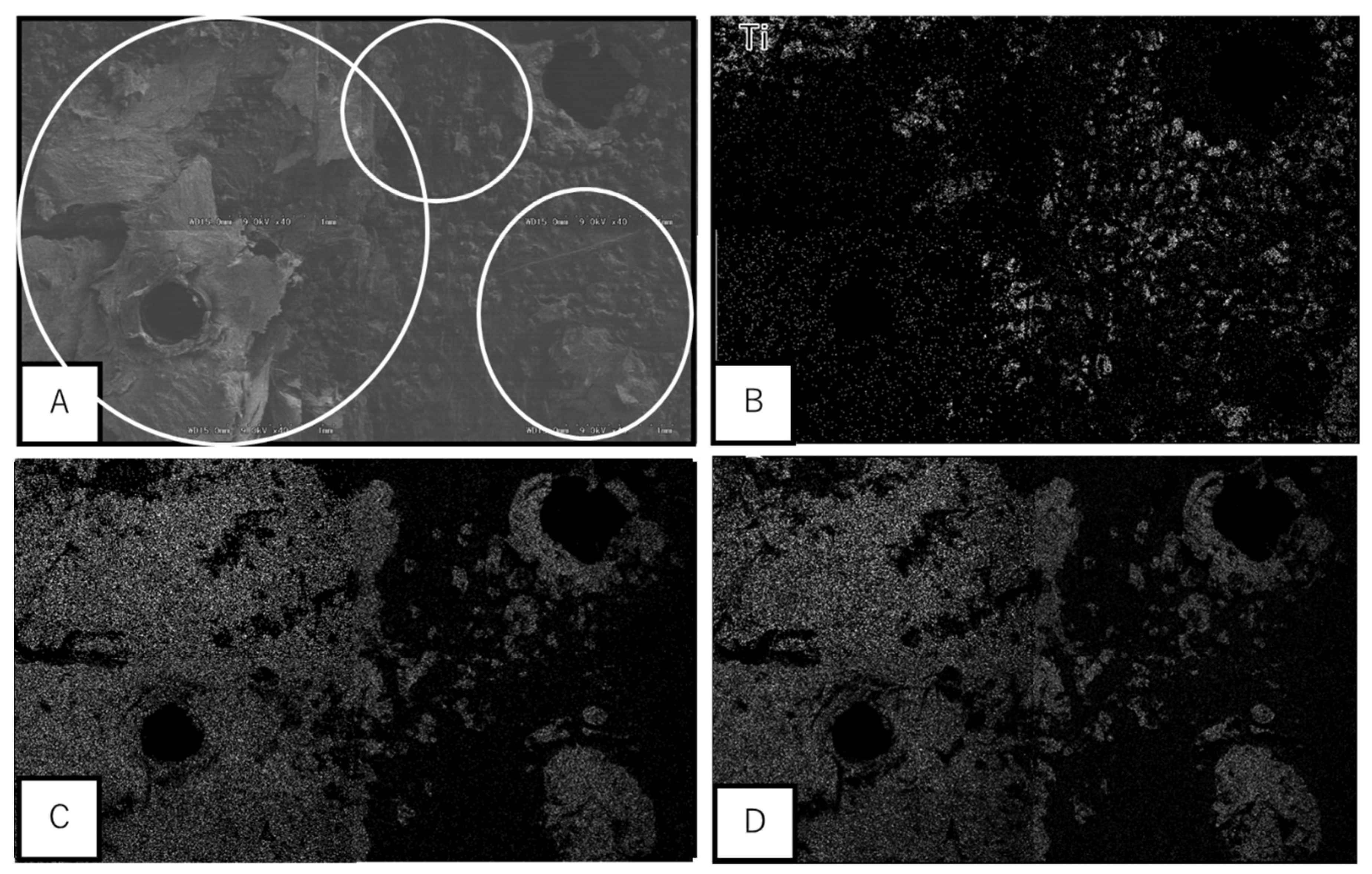
3.2. Scanning Electron Microscopic Observation
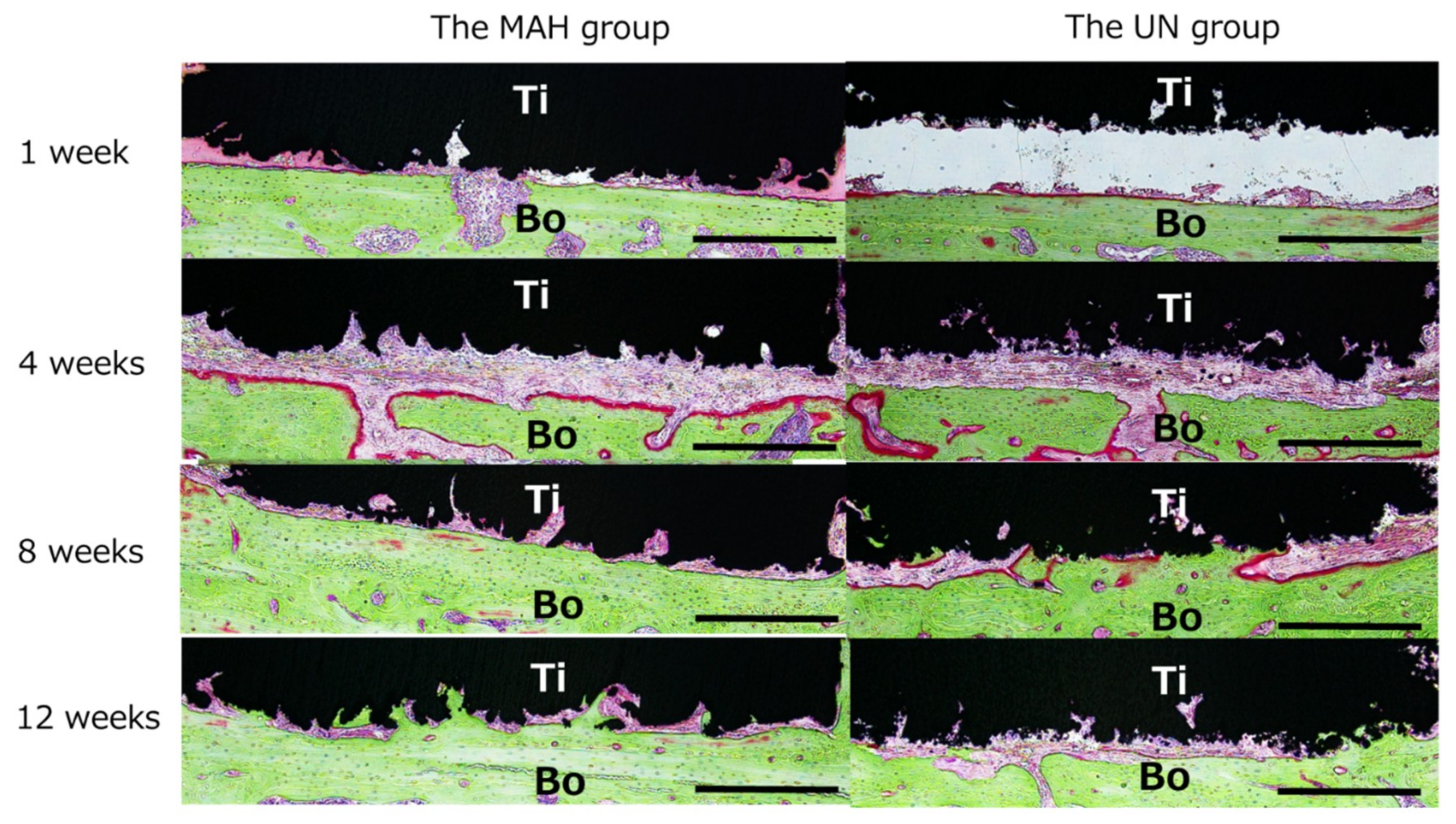
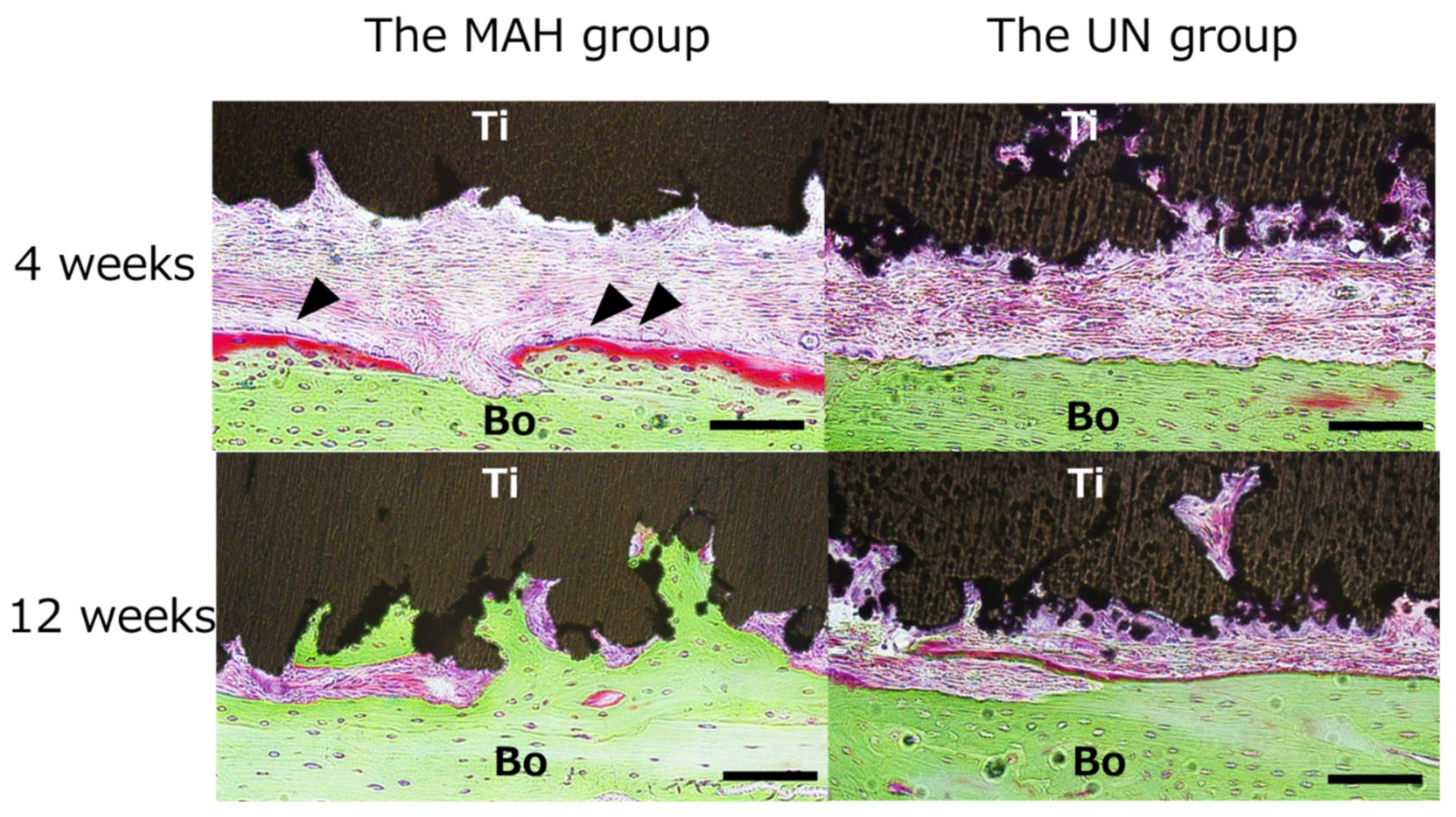
3.3. Histological Observation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Adekeye, E.O. Reconstruction of mandibular defects by autogenous bone grafts: A review of 37 cases. J. Oral Surg. 1978, 36, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Fibula free flap: A new method of mandible reconstruction. Plast. Reconstr. Surg. 1989, 84, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Cobetto, G.A.; McClary, S.A.; Zallen, R.D. Treatment of mandibular fractures with malleable titanium mesh plates: A Review of 120 cases. J. Oral Maxillofac. Surg. 1983, 41, 597–600. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Technical Considerations for AM Medical Devices; US Food and Drug Administration: Concord, MD, USA, 2017.
- Okazaki, Y. Development trend of custom-made orthopedic implant. J. Artif Organs. 2012, 15, 20–25. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Guidance on Evaluation of Customized Orthopedic Devices for Osteosynthesis; PFSB/ELD/OMDE(Yakushokuki)Notification 1215 No.1 of the Director of Medical Devices and Regenerative Medicine Evaluation Division; Pharmaceutical Safety and Environmental Bureau: Tokyo, Japan, 2011.
- Wang, Y.; Huang, S.; Fang, Y.; Huang, S.; Cheng, H.; Chen, C.; Wang, P.; Lin, C. Anatomical thin titanium mesh plate structural optimization for zygomatic-maxillary complex fracture under fatigue testing. Biomed. Res. Int. 2018, 1, 1–7. [Google Scholar] [CrossRef]
- Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Clarissa, P.; Frank, K.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of dental implant surface modifications on osseointegration. Biomed. Res. Int. 2016, 2, 1–16. [Google Scholar] [CrossRef]
- Nuri, T.; Ueda, K.; Iwanaga, H.; Otsuki, Y.; Nakajima, Y.; Ueno, T.; Kawata, R. Microsurgical mandibular reconstruction using a resin surgical guide combined with a metal reconstructive plate. Microsurgery 2019, 39, 696–703. [Google Scholar] [CrossRef]
- Nakajima, Y.; Ueno, T.; Kato-Kogoe, N.; Yamamoto, K.; Fukui, N.; Suwa, Y.; Kimura, Y.; Ito, Y.; Takahashi, Y.; Kasuya, S.; et al. Study on suitability of grafted bone following mandibular reconstruction evaluated according to masticatory performance scores using half-portion gummy jelly. J. Hard Tissue Biol. 2016, 25, 427–430. [Google Scholar] [CrossRef][Green Version]
- Bozic, K.; Kurtz, S.; Lau, E.; Ong, K.; Vail, T.; Berry, D. The epidemiology of revision total hip arthroplasty in the united states. J. Bone Joint Surg. Am. 2009, 91, 128–133. [Google Scholar] [CrossRef]
- Delanois, R.; Mistry, J.; Gwam, C.; Mohamed, N.; Choksi, U.; Mont, M. Current epidemiology of revision total knee arthroplasty in the United States. J. Arthroplasty 2017, 32, 2663–2668. [Google Scholar] [CrossRef]
- Wong, K.C.; Kumta, S.M. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin. Orthop. Relat. Res. 2013, 471, 762–773. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, F.; Calignano, F.; Aversa, A.; Marchese, G.; Lombardi, M.; Biamino, S.; Ugues, D.; Manfredi, D. Additive manufacturing of titanium alloys in the biomedical field: Processes, properties and applications. J. Appl. Biomater. Funct. Mater. 2018, 16, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Avila, J.D.; Bose, S.; Bandyopadhyay, A. Additive manufacturing of titanium and titanium alloys for biomedical applications. In Titanium in Medical and Dental Applications; Woodhead Publishing: Sawston, UK, 2018; pp. 325–343. [Google Scholar] [CrossRef]
- Inoue, K.; Nakajima, Y.; Omori, M.; Suwa, Y.; Kato-Kogoe, N.; Yamamoto, K.; Kitagaki, H.; Mori, S.; Nakano, H.; Ueno, T. Reconstruction of the alveolar bone using bone augmentation with selective laser melting titanium mesh sheet: A report of 2 cases. Implant. Dent. 2018, 27, 602–607. [Google Scholar] [CrossRef]
- Bartolomeu, F.; Dourado, N.; Pereira, F.; Alves, N.; Miranda, G.; Silva, F.S. Additive manufactured porous biomaterials targeting orthopedic implants: A suitable combination of mechanical, physical and topological properties. Mater. Sci. Eng, C Mater. Biol. Appl. 2020, 107, 110342. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Luo, C.; Zhang, C.; Zhang, G.; Qiu, W.; Zhang, Z. Design and fabrication of the custom-made titanium condyle by selective laser melting technology. Zhonghua Kou Qiang Yi Xue Za Zhi 2014, 49, 625–630. [Google Scholar]
- Kokubo, T.; Yamaguchi, S. Simulated body fluid and the novel bioactive materials derived from it. J. Biomed. Mater. Res. A 2019, 107, 968–977. [Google Scholar] [CrossRef]
- Kawai, T.; Takemoto, M.; Fujibayashi, S.; Neo, M.; Akiyama, H.; Yamaguchi, S.; Pattanayak, D.; Matsushita, T.; Nakamura, T.; Kokubo, T. Bone-bonding properties of Ti metal subjected to acid and heat treatments. J. Mater. Sci. Mater. Med. 2012, 23, 2981–2992. [Google Scholar] [CrossRef][Green Version]
- Otawa, N.; Sumida, T.; Kitagaki, H.; Sasaki, K.; Fujibayashi, S.; Takemoto, M.; Nakamura, T.; Yamada, T.; Mori, Y.; Matsushita, T. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Modeling accuracy of titanium products constructed with selective laser melting. J. Craniomaxillofac. Surg. 2015, 43, 1289–1295. [Google Scholar] [CrossRef]
- Sumida, T.; Otawa, N.; Kamata, Y.; Kamakura, S.; Matsushita, T.; Kitagaki, H.; Mori, S.; Sasaki, K.; Fujibayashi, S.; Takemoto, M.; et al. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Clinical application and the comparison with conventional titanium mesh. J. Craniomaxillofac. Surg. 2015, 43, 2183–2188. [Google Scholar] [CrossRef]
- Villanueva, A.R.; Mehr, L.A. Modifications of the Goldner and Gomori one-step trichrome stains for plastic-embedded thin sections of bone. Am. J. Med. Technol. 1977, 43, 36–38. [Google Scholar]
- Kawai, T.; Takemoto, M.; Fujibayashi, S.; Akiyama, H.; Yamaguchi, S.; Pattanayak, D.; Doi, K.; Matsushita, T.; Nakamura, T.; Kokubo, T.; et al. Osteoconduction of porous Ti metal enhanced by acid and heat treatments. J. Mater. Sci Mater. Med. 2013, 24, 1707–1715. [Google Scholar] [CrossRef]
- Okazaki, Y.; Gotoh, E.; Mori, J. Strength-durability correlation of osteosynthesis devices made by 3D layer manufacturing. Materials 2019, 12, 436. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, Y.; Ishino, A. Microstuructures and mechanical properties of laser-sintered commercially pure Ti and Ti-6Al-4V alloy for dental applications. Materials 2020, 13, 609. [Google Scholar] [CrossRef] [PubMed]
- Gokuldoss, P.K.; Kolla, S.; Eckert, J. Additive manufacturing processes: Selective laser melting, electron beam melting and binder jetting-selection guidelines. Materials 2017, 19, 672. [Google Scholar] [CrossRef]
- Chengyang, D.; Jinwu, K.; Tao, F.; Yunlong, F.; Xiang, W.; Pengyue, W. Study on the selective laser melting of CuSn10 powder. Materials 2018, 11, 614. [Google Scholar] [CrossRef]
- Tsukanaka, M.; Yamamoto, K.; Fujibayashi, S.; Pattanayak, D.; Matsushita, T.; Kokubo, T.; Matsuda, S.; Akiyama, H. Evaluation of bioactivity of alkali- and heat-treated titanium using fluorescent mouse osteoblasts. J. Bone Miner. Metab. 2014, 32, 660–670. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Yamaguchi, S.; Matsushita, T.; Mori, S.; Kitagaki, H.; Yoshimura, H.; Sano, K.; Sunano, A.; Nakkajima, Y.; Nakano, H.; et al. Histologic evaluation of bone regeneration using titanium mesh prepared by selective laser melting technique. J. Hard Tissue Biol. 2017, 26, 257–260. [Google Scholar] [CrossRef][Green Version]
- Yamamoto, K.; Yamaguchi, S.; Matsushita, T.; Mori, S.; Hirata, A.; Kato-Kogoe, N.; Nakano, H.; Nakajima, Y.; Nishitani, Y.; Nagatsuka, H.; et al. Osteogenic capacity of mixed-acid and heat treated titanium mesh prepared by a selective laser melting technique. RSC Adv. 2018, 8, 26069–26077. [Google Scholar] [CrossRef]
- Takahashi, Y.; Kanou, M.; Ito, Y.; Ohmori, M.; Yamamoto, K.; Kimura, Y.; Kato-Kogoe, N.; Nakajima, Y.; Fujita, Y.; Ariyoshi, Y.; et al. Histological evaluation of alveolar bone ridge for dental implant placement using a nondecalcified frozen section technique. J. Hard Tissue Biol. 2017, 26, 61–66. [Google Scholar] [CrossRef]
- Kokubo, T.; Pattanayak, D.; Yamaguchi, S.; Takadama, H.; Matsushita, T.; Kawai, T.; Takemoto, M.; Fujibayashi, S.; Nakamura, T. Positively charged bioactive Ti metal prepared by simple chemical and heat treatments. J. R. Soc. Interface 2010, 7, S503–S513. [Google Scholar] [CrossRef]
- Kokubo, T.; Kushitani, H.; Sakka, S.; Kisugi, T.; Yamamoto, T. Solutions able to reproduce in vivo surface structure changes in bioactive glass-ceramic A-W. J. Biomed. Mater. Res. 1990, 24, 721–734. [Google Scholar] [CrossRef] [PubMed]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Takemoto, M.; Fujibayashi, S.; Akiyama, H.; Tanaka, M.; Yamaguchi, S.; Pattanayak, D.; Doi, K.; Matsushita, T.; Nakamura, T.; et al. Osteoinduction on Acid and Heat Treated Porous Ti Metal Samples in Canie Muscle. PLoS ONE 2014, 9, e88366. [Google Scholar] [CrossRef] [PubMed]
- Shibahara, T.; Noma, H.; Furuya, Y.; Takaki, R. Fracture of mandibular reconstruction plates used after tumor resection. J. Oral Maxillofac. Surg. 2002, 60, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Almansoori, A.A.; Choung, H.W.; Kim, B.; Park, J.Y.; Kim, S.M.; Lee, J.H. Fracture of Standard Titanium Mandibular Reconstruction Plates and Preliminary Study of Three-Dimensional Printed Reconstruction Plates. J. Oral Maxillofac. Surg. 2020, 78, 153–166. [Google Scholar] [CrossRef]
- Komisar, A.; Warman, S.; Danziger, E. A critical analysis of immediate and delayed mandibular reconstruction using A-O plates. Arch. Otolaryngol. Head Neck Surg. 1989, 115, 830–833. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imagawa, N.; Inoue, K.; Matsumoto, K.; Ochi, A.; Omori, M.; Yamamoto, K.; Nakajima, Y.; Kato-Kogoe, N.; Nakano, H.; Matsushita, T.; et al. Mechanical, Histological, and Scanning Electron Microscopy Study of the Effect of Mixed-Acid and Heat Treatment on Additive-Manufactured Titanium Plates on Bonding to the Bone Surface. Materials 2020, 13, 5104. https://doi.org/10.3390/ma13225104
Imagawa N, Inoue K, Matsumoto K, Ochi A, Omori M, Yamamoto K, Nakajima Y, Kato-Kogoe N, Nakano H, Matsushita T, et al. Mechanical, Histological, and Scanning Electron Microscopy Study of the Effect of Mixed-Acid and Heat Treatment on Additive-Manufactured Titanium Plates on Bonding to the Bone Surface. Materials. 2020; 13(22):5104. https://doi.org/10.3390/ma13225104
Chicago/Turabian StyleImagawa, Naoko, Kazuya Inoue, Keisuke Matsumoto, Ayako Ochi, Michi Omori, Kayoko Yamamoto, Yoichiro Nakajima, Nahoko Kato-Kogoe, Hiroyuki Nakano, Tomiharu Matsushita, and et al. 2020. "Mechanical, Histological, and Scanning Electron Microscopy Study of the Effect of Mixed-Acid and Heat Treatment on Additive-Manufactured Titanium Plates on Bonding to the Bone Surface" Materials 13, no. 22: 5104. https://doi.org/10.3390/ma13225104
APA StyleImagawa, N., Inoue, K., Matsumoto, K., Ochi, A., Omori, M., Yamamoto, K., Nakajima, Y., Kato-Kogoe, N., Nakano, H., Matsushita, T., Yamaguchi, S., Thi Minh Le, P., Maruyama, S., & Ueno, T. (2020). Mechanical, Histological, and Scanning Electron Microscopy Study of the Effect of Mixed-Acid and Heat Treatment on Additive-Manufactured Titanium Plates on Bonding to the Bone Surface. Materials, 13(22), 5104. https://doi.org/10.3390/ma13225104




