Abstract
Vascularization in bone tissues is essential for the distribution of nutrients and oxygen, as well as the removal of waste products. Fabrication of tissue-engineered bone constructs with functional vascular networks has great potential for biomimicking nature bone tissue in vitro and enhancing bone regeneration in vivo. Over the past decades, many approaches have been applied to fabricate biomimetic vascularized tissue-engineered bone constructs. However, traditional tissue-engineered methods based on seeding cells into scaffolds are unable to control the spatial architecture and the encapsulated cell distribution precisely, which posed a significant challenge in constructing complex vascularized bone tissues with precise biomimetic properties. In recent years, as a pioneering technology, three-dimensional (3D) bioprinting technology has been applied to fabricate multiscale, biomimetic, multi-cellular tissues with a highly complex tissue microenvironment through layer-by-layer printing. This review discussed the application of 3D bioprinting technology in the vascularized tissue-engineered bone fabrication, where the current status and unique challenges were critically reviewed. Furthermore, the mechanisms of vascular formation, the process of 3D bioprinting, and the current development of bioink properties were also discussed.
1. Introduction
Treatment of large bone defects resulting from cancer, trauma, infection, congenital malformation, or surgical resection is a challenge for clinical doctors [1]. Currently, the autologous bone grafts are the gold treatment standard for large bone defects [2]. However, the amount of autologous bone grafts is limited, and complications at the harvesting site, such as pain, infection, or bleeding, could result in additional donor-site morbidity [3]. Bone grafts fabricated by the tissue-engineered methods are rapidly becoming promising alternatives [4]. However, oxygen and metabolic needs are not met when the thickness of the tissue-engineered bone constructs exceeds 150–200 µm, resulting in lacking tissue integration with host tissue and core ischemia of tissue-engineered bone grafts [5,6]. Furthermore, insufficient vascularization of tissue-engineered bone often results in poor bone regeneration [7]. Therefore, during the fabrication of tissue-engineered bone constructs, it is vital to construct functional vascular networks, which could supply the exchange of nutrition, oxygen, and waste products between bone grafts and host [8].
Bone, being a dynamic tissue, is not only a complex heterogeneous tissue with intricate hierarchical architecture but also a highly ordered and vascularized tissue with vascular networks, which is connected to the blood system by transverse channels [9,10,11]. Traditional tissue-engineered methods based on seeding cells into the scaffold could not precisely control the inner structure, cell distribution, and exocellular microenvironment to meet the biomechanical functions and metabolic requirement of bone tissue [12]. In addition, traditional tissue engineering methods cannot fabricate the biomimetic tissue-engineered constructs with realistic cell microenvironment, which leads to over-simplified tissue-engineered constructs [13,14]. Therefore, the limitations of traditional tissue engineering technologies to recreate similarities and complexes from native bone tissues restrict their further applications [15]. Nanomaterials with bone-mimicking characteristics can construct proper cell microenvironments to enhance bone regeneration [16]. However, there are several challenges of nanomaterials, such as failure to temporospatial administration of growth factors and cells, as well as lack of integrative networks of new bone tissues and blood vessels [17].
Three-dimension (3D) printing technology, initially introduced in 1986, has been widely used to fabricate objects with complex geometries and architecture [18]. Recently, 3D bioprinting technology has emerged as a promising alternative to fabricate 3D functional tissue constructs with geometrically defined structures, which are designed to replace or regenerate the damaged tissues or organs, such as liver, bone, skin, liver, cartilage, nerve, and heart [19]. Three-dimensional (3D) bioprinting is the use of a combination of 3D printing, tissue engineering, developmental biology, and regenerative medicine to construct biomimetic tissues. Particularly, compared to conventional scaffold-based approaches, 3D bioprinting technology could precisely control complex 3D architecture, multiple compositions, and spatial distributions [13]. Both 3D printing and 3D bioprinting could utilize the layer-by-layer manner to fabricate 3D anatomically shaped constructs from a computer-aided design (CAD) model. However, 3D bioprinting technologies involve the utilization of cell-laden bioinks and other bioactive molecules to fabricate biomimetic tissue constructs during the printing process, while 3D printing technologies do not involve the utilization of cells or other bioactive molecules [13,20]. In addition, 3D bioprinting technology can guide tissue formation for patient-specific therapy by precise spatiotemporal control on the distribution of cells, growth factors, small molecules, drugs, miRNA, and other bioactive substances [21,22]. Therefore, we conducted this review using EMBASE, PubMed, Medline, and Web of Science for studies on the application of 3D bioprinting technology in the vascularized tissue-engineered bone fabrication. This review discussed the current status and unique challenges. Furthermore, the mechanisms of vascular formation, the process of 3D bioprinting, and the current development of bioink properties were also discussed.
2. Mechanisms of Vascular Formation
New blood vessels are formed by two main fundamental processes, angiogenesis and vasculogenesis [23]. Vasculogenesis is known as differentiation of endothelial progenitor cells (EPCs) or angioblastic progenitor cells into endothelial cells (ECs) and the formation of a primitive vascular network [24]. During the process of early embryo development, primitive capillary networks form through recruitment and differentiation of angioblastic progenitor cells [25]. In adults, vasculogenesis was often observed in the repair process of various damaged tissues and pathological states such as atherosclerosis, ischemia, and tumor [26]. Angiogenesis is known as the growth process of new capillaries from pre-existing blood vessels. Furthermore, the process of angiogenesis is tightly regulated by related biological factors [27]. When the initial vascular network forms into more complex vascular networks, vasculogenesis is followed by angiogenesis. Angiogenesis plays a vital role during the process of tissue regeneration. Angiogenesis disorders are implicated in the pathogenesis of a variety of diseases, including vascular retinopathy, rheumatoid arthritis, and tumor [28]. After the process of angiogenesis, the vascular network expands and bridges with other capillary networks, which is also called splitting angiogenesis. In the process of vessel maturation, smooth muscle cells and differentiated pericytes stabilize vascular structures and suppress the growth of ECs [26]. The process of vasculogenesis and angiogenesis is shown in Figure 1a.
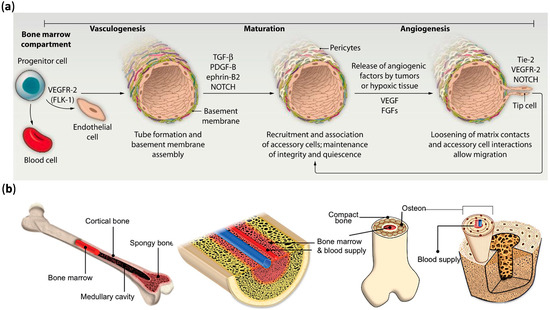
Figure 1.
(a) The process of vasculogenesis and angiogenesis; (b) the schematic illustration of complex bone tissue with vascular structure. Reprinted with permission from References [29,30].
Bones are highly vascularized and receive around 10%–15% of resting cardiac output [31]. The microvasculature of bone tissue is consisted of three types of vessels, namely capillaries, arterioles, and venules [32]. The schematic illustration of complex bone tissue with vascular structure is shown in Figure 1b. Vasculature networks play an important role in the process of bone tissue formation. As a coordinated process, bone tissue regeneration involve the connection between bone cells and blood vessels [33]. The two general ways of bone tissue formation, intramembranous and endochondral ossification, are also regulated by the bone vasculature [34]. During the process of endochondral ossification, mesenchymal progenitor cells aggregate into dense clusters and differentiate into chondrocytes. The nonproliferative chondrocytes in the cartilage template secrete proangiogenic factors, which stimulate blood vessels to invade and, along with osteoclasts and osteoprogenitors, to form the primary ossification center [35]. As the vasculature expands, the cartilage is replaced with bone tissue, resulting in the growth of longitudinal bone [36]. Unlike endochondral ossification, intramembranous ossification is the development process of bone tissue from fibrous membranes. Microcapillary network growth extends into the mesenchymal region of periosteum, resulting in the differentiation of mesenchymal cells into osteoprogenitors and osteoblasts [37]. Currently, two strategies are used to construct the vascular network in engineered bone, including creating a major vessel with ECs and the formation of microcapillaries through self-assembly and biological processes [38,39]. Ideally, intramembranous and endochondral ossification should be combined to fabricate tissue-engineered bone with multiscale vasculatures.
3. 3D Bioprinting
3.1. The Procedure of 3D Bioprinting
As an emerging multidisciplinary subject, 3D bioprinting consists of 3D printing technology, tissue engineering, developmental biology, regenerative medicine [32]. More specifically, 3D bioprinting technology is an additive manufacturing process of tissue-like structures by utilization of 3D printing-like techniques to combine biomaterials, cells, and growth factors [40]. The 3D bioprinting technology utilizes the layer-by-layer manner to deposit biomaterials, also known as bioinks, to fabricate tissue-like structures in tissue engineering fields [41]. Three-dimensional (3D) bioprinting technology can offer precise control on complex 3D architecture, spatial distributions, multiple compositions [42]. The first step of 3D bioprinting is to image the tomographic properties and functions of the target tissue by magnetic resonance imaging (MRI), computed tomography scanning (CT scan), and ultrasound imaging techniques (UI) [43]. The second step is to design and reconstruct precisely 3D functional tissues by a computer-aided design (CAD) model [44]. The next step is the tissue designs, which includes material selection and cell selection. Biomaterials, also known as bioinks, mimic the structure, shape, architecture, and function properties of the extracellular matrix of target tissues [45]. Additionally, bioinks play an essential role in supporting the adhesion, proliferation, and function of encapsulated cells [46]. Following cells suspended in bioinks, the cell-laden bioinks are then utilized to fabricate 3D biomimetic tissue constructs with geometrically defined structures by a bioprinter [47]. The last step of bioprinting procedure is the maturation phase of the engineered tissues or organs. The perfusion bioreactors containing nutrient transport and physiological stimuli mimic the environment and stimuli of natural tissue and promote the maturation of the engineered tissues [18]. During this maturation phase, the printed structures aggregate to form bigger continuous structures and place them precisely in the appropriate position [13]. Additionally, a 3D bioprinting tissue can be printed in situ, in which case the human body acts as the bioreactor. Figure 2 shows the general step-wise procedure for bioprinting 3D tissues.
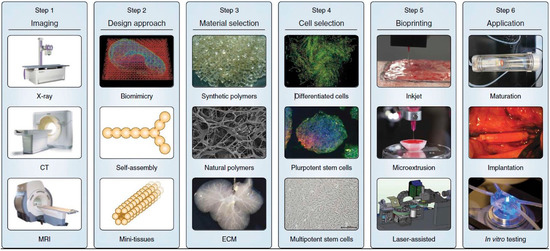
Figure 2.
The general step-wise procedure for bioprinting 3D tissues. Reprinted with permission from Reference [12].
3.2. 3D Bioprinting Methods in Fabrication of Vascular Networks
Briefly, according to their working mechanism, the typical procedures of 3D bioprinting technologies can be broadly classified into laser-assisted bioprinting, inkjet bioprinting, and extrusion-based bioprinting [48]. The simplified procedures of different kinds of 3D bioprinting are shown in Figure 3. Each of these approaches has been summarized in Table 1.
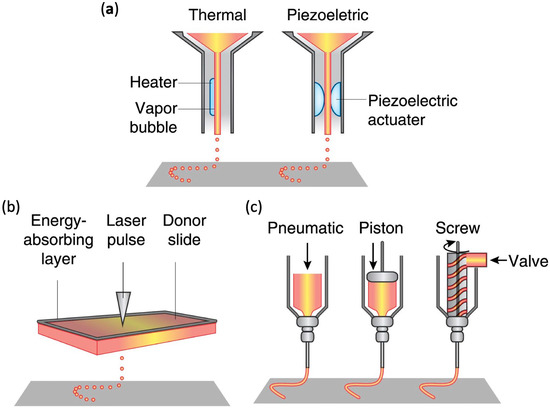
Figure 3.
The simplified procedure of different kinds of 3D bioprinting. (a) Inkjet bioprinting; (b) laser-assisted bioprinting; (c) extrusion-based bioprinting. Reprinted with permission from Reference [12].

Table 1.
Comparison of different kinds of 3D bioprinting.
3.2.1. Inkjet Bioprinting
Inkjet bioprinting is a rapid and large-scale fabrication technique that has been adapted from the inkjet printing technology to print living cells by desktop inkjet printers [76] (Figure 3a). Currently, many studies utilize inkjet bioprinting to construct various engineered tissues with different kinds of living cells [77,78,79]. In addition, inkjet bioprinting can rapidly fabricate tissue-like structures with intricate hierarchical architectures by the utilization of the controlled dropwise deposition of cell-laden bioinks [79]. As a non-contact printing technique, inkjet bioprinting could precisely deposit droplets of cell-laden bioinks in the z-axis onto the surface of culture dish or hydrogel substrates [80]. According to the droplet actuation mechanism, the inkjet bioprinting could be further classified into thermal inkjet printing and piezoelectric inkjet printing [81]. Thermal inkjet printing dispensed the bioink droplet by a thermal actuator with a voltage pulse to locally heat the bioink. In the process of piezoelectric inkjet bioprinting, the piezoelectric actuator can be activated by variations in the electric impulse and amplitude and used to control the stress to which the bioink is exposed [54]. As a nozzle-based technique, inkjet bioprinting had advantaged of high printing speed, affordability, high resolution [5]. However, the inkjet bioprinting is limited by the fact that only low-viscosity bioinks can be used for bioprinting; an additional crosslinking step in the process of inkjet bioprinting is needed to improve the structural stability of 3D tissue constructs [82].
Currently, several studies utilize inkjet bioprinting to create customized tissue-engineered with vascular networks. Xu et al. successfully used the 3D inkjet bioprinting system to fabricate 3D complex tissue-engineered constructs with fibroblast-based tubes [83]. Lee et al. fabricated a perfused vascular channel within thick collagen scaffold by inkjet bioprinting. Fully covered by ECs, the functional vascular channel can not only support the viability of tissue up to 5mm in the distance under the physiological flow condition but also presents a barrier for both plasma protein and dextran molecule [84]. Besides, Lee et al. connected the multi-scale capillary network to the large perfused vascular channels through a natural maturation process [85]. In another study, thermal inkjet bioprinting was used to fabricated constructs with microvasculature by depositing bioink consisting of human microvascular endothelial cells and fibrin [5].
3.2.2. Laser-Assisted Bioprinting
Laser-assisted bioprinting precisely deposit cell-laden bioinks in a 3D spatial arrangement by an energy source of laser radiation, which is highly monochromatic, focused, and coherent [86]. The laser-bioprinting setup mainly consists of a laser source, a receiving substrate, and a ribbon coated with cell-laden bioinks [87] (Figure 3b). During the procedure of laser-assisted bioprinting, the ribbon is illuminated by a focused laser beam. As a consequence, cell-laden bioinks evaporate and reach onto the surface of receiving substrate, which supports the adhesion and proliferation of cells [88]. The lasers used in the laser-assisted bioprinting are mainly nanosecond lasers with UV [89]. The procedure of laser-assisted bioprinting is contactless, resulting in high post-printing cell viabilities. Additionally, laser-assisted bioprinting can not only print various living cells but also peptides and DNA [90]. Currently, few studies apply laser-assisted bioprinting technology to fabricate 3D vascularized tissue-engineered constructs. Wu et al. utilized laser-assisted bioprinting technology to construct a branch/stem structure of umbilical vein smooth muscle cells and umbilical vein endothelial cells (HUVECs) [91]. However, the branch/stem structure fabricated by laser-assisted bioprinting is a very simplified structure and could not mimic the structure of human vascular networks. Gruene et al. [92] utilized human adipose-derived stem cells (hASCs) to fabricate the 3D tissue grafts by the laser-assisted bioprinting technology. In addition, they also demonstrated that the procedure of laser-assisted bioprinting did not affected the proliferation ability and differentiation behavior of the hASCs. In another study, ECs were bioprinted by laser-assisted bioprinting technology onto a collagen hydrogel scaffold previously seeded with mesenchymal stem cells (MSCs) to fabricate a microvascular network [93]. Kérourédan et al. utilized laser-assisted bioprinting to bioprint ECs in situ into mouse calvarial bone defects prefilled with collagen scaffold containing MSCs and vascular endothelial growth factor (VEGF) [94]. The results demonstrated that in vivo laser-assisted bioprinting is a valuable approach to introduce in situ prevascularization with a defined architecture and enhance bone tissue regeneration.
3.2.3. Extrusion-Based Bioprinting
Among these bioprinting technologies, extrusion-based bioprinting is a widely used approach of the material-dispensing technique used for bioprinting [95]. Extrusion-based bioprinting utilizes extrusion of the bioinks through a microscale nozzle to fabricate tissue-engineered constructs onto a stationary substrate [96] (Figure 3c). The extrusion is controlled using pneumatic pressure or mechanical compressions. After the layer-by-layer application, extrusion-based bioprinting fabricates 3D patterns and constructs [97]. Advantages of extrusion-based bioprinting are the direct incorporation of cells, processing at room temperature, and homogenous distribution of cells. Additionally, extrusion-based bioprinting has been utilized in the printing of cells and tissues with defined retention of activity [98]. Furthermore, tissue spheroids can also be loaded in pipettes of extrusion-based bioprinting to fabricate artificial tissues and organs [99]. In contrast to laser-assisted bioprinting limited by scalability and inkjet bioprinting limited by low viscosity, extrusion-based bioprinting can fabricate large, scalable tissue-engineered constructs with a wide range of viscosities. Due to its ease of control, cost-effectiveness, and the availability of shear-thinning bioinks, extrusion-based bioprinting is widely used [100]. However, the extrusion-based bioprinting is limited by the fact that the printing speed is relatively low [101].
Extrusion-based bioprinting technology has be proven a great promise in fabricating vascularized constructs with multiple cell types by the incorporation of several extrusion nozzles [102]. Tan et al. utilized the multi-nozzle extrusion-based technique to print vertically alginate-based tubular structures with varying viscosity [103]. The results demonstrated the feasibility of extrusion-based bioprinting to fabricate large diameter vascularized constructs. Extrusion-based bioprinting combined with microfluidic techniques can construct sophisticated 3D architectures in complex, heterogeneous constructs. Zhang et al. utilized chitosan and alginate hydrogels as bioinks to fabricate a printable vessel-like microfluidic channels by extrusion-based bioprinting [104]. Dolati et al. printed an alginate vascular conduit by a coaxial bioprinting process. In addition, the mechanical properties of the vascular conduit were enhanced by multi-walled carbon nanotubes [105]. Researchers also utilized this combined bioprinting technique to integrate micro-engineered vasculature and cellular layers within the deposited extracellular matrix of target tissues [106]. Gao et al. also used a coaxial nozzle to print vessel-like hollow filaments [98]. Colosi et al. utilized this combined bioprinting technique to fabricate the tissue-engineered constructs with human umbilical vein endothelial cell–lined vasculature by depositing different bioinks using a blend of alginate and gelatin methacrylate (GelMA) [107].
3.3. Bioinks
In the field of bioprinting, bioinks is another important part [100]. The bioink is either a solution or a hydrogel of biomaterials encapsulating the desired cells and used for fabricating tissue-engineered constructs. The bioinks provide stable 3D architecture to affect the development and maturation of tissue [54] and mimic the tissue niche in situ. Therefore, bioink design plays a crucial role in the process of 3D bioprinting. Currently, various natural and synthetic biomaterials with different physical and chemical properties have been formulated and utilized as bioinks [108]. The 3D architecture of bioinks affects the phenotype of encapsulated cells, resulting in the activation of various cellular signaling pathways and the expression of various related genes [109]. Additionally, 3D bioprinting technology can combine two or more bioinks of distinct materials to construct hybrid scaffolds. Therefore, the development of bioinks still needs significant research to achieve better cell regulation function. An ideal bioink should possess a range of properties as follow: (i) good printability withstanding forces applied during the printing process; (ii) biocompatibility mimicking the natural microenvironment of the target tissues; (iii) structural stability and biodegradation; (iv) mechanical properties; (v) suitability for chemical modifications to meet tissue-specific needs. Furthermore, standardized bioink formulations are also required in bioprinting to be applied in different kinds of tissue.
According to the different source, bioinks used in 3D bioprinting can be basically divided into two types of hydrogels: nature-derived and synthetic bioinks [50,110]. Bioinks from various sources exhibit different biological characteristics during the process of 3D bioprinting [111,112,113]. Nature-derived bioinks have been widely used to fabricate the tissue-engineering constructs, which could support the attachment and proliferation of bioprinted cells [75]. Most of the nature-derived bioinks are derived from the natural extracellular matrix of different tissue. Compared to synthetic bioinks, nature-derived bioinks more closely resemble the native tissue and provide a better cell microenvironment. In addition, nature-derived bioinks can provide tissue-specific nutrients for cells. Nature-derived bioinks commonly used in the 3D bioprinting include silk, chitosan, decellularized extracellular matrix, hyaluronic acid, fibrin, collagen, gelatin, hydroxyapatite, and alginate [50]. In contrast to nature-derived bioinks, synthetic bioinks are fabricated by the process of chemical synthesis. They are more controllable than nature-derived bioinks in terms of chemical and mechanical properties, such as alignment, porosity, tensile strength, and elastic modulus. Synthetic bioinks commonly used in 3D bioprinting include polyethylene glycol (PEG), polycaprolactone (PCL), pluronic acid [114,115]. The characteristics of various bioinks commonly used in the bioprinting are shown in Table 2.

Table 2.
Summary of various bioinks.
Among these various bioinks, gelatin methacrylate (GelMA) is the most widely used bioink to fabricate the vascular network in engineered constructs [125,126]. Compared to ionically crosslinked alginate, GelMA can form a chemically stable hydrogel scaffolds when exposed to ultraviolet [127]. GelMA is a photopolymerizable hydrogel and contains many natural cell binding-motifs which promote cell adhesion and cell migration within the GelMA matrix [128]. The hydration and biomechanical properties of GelMA can be regulated by changing the gel concentration and methacrylation degree. In addition, osteogenic cells could be encapsulated into GelMA with microchannels lined with ECs to fabricate vascularized tissue-engineered bone tissues [129,130]. GelMA can also be combined with other biomaterials to form hybrid bioinks for the fabrication of vascularization. Jia et al. fabricated perfused vascular structures by a 3D bioprinting technique based on cell-laden bioinks consisting of sodium alginate and GelMA [63]. The blended bioink was crosslinked by calcium ions [63].
3.4. Cells Used in Bioprinting
The choice of various cell types is another key element for 3D bioprinting. The cells and biomaterials interact with each other. Additionally, to mimic the function of target tissue on a macro scale, the cells used in bioprinting must have the ability to proliferate and mimic the physiological state of cells in vivo and in vitro [131]. Currently, various types of mammalian cells, such as osteogenic, as well as angiogenic cells, have been successfully used to fabricate vascularized tissue-engineered constructs [44]. To date, among many various osteogenic cells, MSCs are the most likely used cells in 3D bioprinting for the fabrication of tissue-engineered bone, owing to their differentiation potential and self-renewing capability [19,132,133]. MSCs are widely found in cord blood, umbilical cord, adipose tissue, and bone marrow [134]. Induced pluripotent stem cells (iPSCs) were first found in 2007 and were generated directly from a somatic cell [135]. IPSCs have the advantages of expandability, easy accessibility, and ability to differentiate into other cell types [136]. Moreover, MSCs were recently derived from iPSCs, which could overcome the inadequate source of autologous MSCs and cell aging [137]. Moreover, MSCs are highly sensitive to the microenvironment of bioinks, including chemical, physical, and biological cues. Therefore, the function of encapsulated stem cells can be regulated by changing the environment of bioinks [138]. Phillippi et al. engineered stem cell microenvironments by 3D bioprinting technology. Through this approach, the researchers engineered cell fate toward the osteogenic lineage [71]. During the procedure of bioprinting, cells could be arranged as individually or dispersed or encapsulated in the hydrogel precursor. Additionally, cells could be utilized to construct cell aggregates or microcarriers into bioinks [139].
Cell Viability
Currently, there are many kinds of cells used in the bioprinting process to fabricate tissue-engineered bone constructs, such as MSCs and ECs [21,125]. There is still a challenge in maintaining the viability of the cells encapsulated inside the bioinks The post-printing cell viability in bioinks of laser-assisted bioprinting, inkjet bioprinting, and extrusion-based bioprinting is shown in Table 2. Currently, most studies found the 3D bioprinted cells had high post-printing cell viability after a few hours or days [13,95]. However, there are few long-term studies focusing on cell viability after bioprinting. In addition, print pressure and print speed directly affect cell viability [22]. Shear and thermal stress during the bioprinting process also affect cell viability [86]. In addition, if used too frequently, piezoelectric technology could damage cell membrane, resulting in cell death [76]. Although the bioinks can protect the cells from being damaged by the potentially high shear stress during the bioprinting process, different kinds of bioinks exhibit differences in maintenance of the viability of cells. In addition, some kinds monomers and photo-initiators, used in the process of crosslinking, can also affects cell viability.
3.5. Multi-Materials Bioprinting
Bioinks, used in the process of bioprinting, are hydrophilic and high-molecular weight polymers with high water content, which can be cross-linked to form a 3D bioprinted construct [140]. In addition, most kinds of bioinks used in bioprinting are hydrogels, which have a certain drawback of weak mechanical property [141]. Multi-materials bioprinting has been used to improve the biomechanical property and structural integrity of 3D bioprinted constructs [142]. In addition, multi-materials bioprinting can be utilized to fabricate biomimetic and heterogeneous constructs, such as vascularized tissues [142]. The ability to deposit multi-materials materials in 3D bioprinting is consistent with support strategies found in the process of 3D printing. During the bioprinting process, support materials are utilized to enhance the structure integrity and mechanical property of 3D bioprinted constructs. Currently, the approaches of multi-materials bioprinting mainly include multi-head systems, core-shell needle systems, stereolithography, and multi-material microfluidic bioprinting [142,143]. However, how to improve printing resolution and integrate different kinds of materials still need to be solved in the application of multi-materials bioprinting.
4. 3D Bioprinting in the Fabrication of Vascularized Tissue-Engineered Bone
The vasculature in various tissues transports the required oxygen and nutrients and removes waste products. Vascularization plays an essential role in successful engineering of tissue constructs. Constructing vascular networks within 3D tissue-engineered bone constructs is a critical challenge in maintaining the viability of bioprinted cells. Currently, many approaches have been utilized to improve the growth of vascular networks within 3D tissue-engineered bone constructs. Currently, many researchers incorporate growth factors into tissue constructs or encapsulated ECs and tissue spheroids into biomaterials to fabricate complex 3D tissue structures with functionalized vasculature.
4.1. Cell-Based Approaches for Vascular Networks
The processes of vascular growth and remodeling involve ECs which line the interior of blood vessels. Currently, many studies encapsulated ECs and other supporting cell types into bioinks to fabricate vascularized tissue-engineered bone [29]. Cell-based approaches activate related cell signaling pathways by strengthening cell-cell interactions to enhance the formation of vascular networks in tissue-engineered constructs. Coculturing of different kinds of cells can achieve the goal of the prevascularization of tissue-engineered constructs [144]. Kolesky et al. fabricated cell-laden, heterogeneous, and vascularized tissue-engineered constructs by 3D Bioprinting [145]. In their study, the embedded vasculature was filled by Pluronic F127, an aqueous fugitive bioink, which could be easily printed and removed under mild conditions [146] (Figure 4a). The endothelialization of embedded vasculature was conducted by the perfusion and incubation of HUVEC suspensions. Chen et al. fabricated the polydopamine-modified calcium silicate (PDACS)/poly-caprolactone (PCL) constructs with Wharton’s jelly MSCs combined with HUVEC-laden bioink [147]. The in vitro results showed that HUVECs in the bioink expressed higher levels of angiogenic proteins [147] (Figure 4b). In another study, Chiesa et al. constucted an in vitro vascularized bone model capillary-like network, using a gelatin-nanohydroxyapatite 3D bioprinted scaffold combined with MSCs and HUVECs [148].
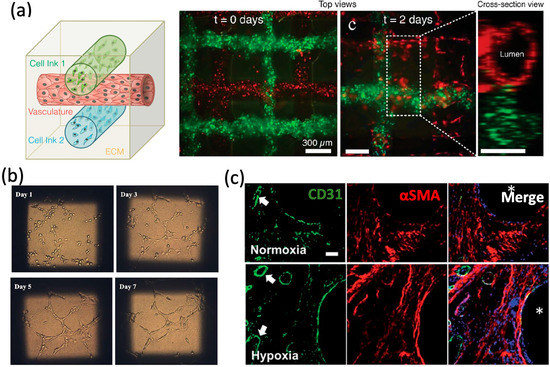
Figure 4.
Cell-based approaches for vascular networks. (a) Schematic view and fluorescence images of an engineered tissue construct cultured for 0 and 2 days, respectively. (b) The tube formation of HUVEC-laden hydrogel/PDACS/PCL scaffold. (c) CD31, aSMA, and nuclei staining for 3D bioprinted constructs. Reprinted with permission from References [133,145,147].
Currently, a lot of promising techniques enhancing vascularization are utilized to combine bioprinting with vascularized bone formation. Some previous studies demonstrated that MSCs with hypoxia pre-treatment could enhance vascularization and osteogenesis in vitro an in vivo [149,150,151]. Kuss et al. [133] fabricated a polycaprolactone/hydroxyapatite (PCL/HAp) and stromal vascular fraction into tissue-engineered bone constructs, which were pre-treated in hypoxic conditions for three weeks. The results showed that short-term hypoxic conditioning could enhance the microvessel formation (Figure 4c). Non-viral gene delivery can facilitate the endogenous expression of desired therapeutic proteins, which can provide a stimulus to cells, resulting in enhanced levels of matrix production and tissue formation [152,153]. Cunniffe et al. [153] bioprinted a non-viral, and MSC-laden gene activated construct. The gene activated bioinks were fabricated by RGD-γ-irradiated alginate and nano-hydroxyapatite (nHA) complexed to plasmid DNA (pDNA) [153]. After implanted subcutaneously in vivo, gene activated MSC-laden constructs could effectively improve mineralization and vascularization.
4.2. Tissue Spheroid-Based Approaches for Vascular Networks
Another approach for the formation of vascular networks involves multiple vascular cell types aggregated as multicellular vascular tissue spheroids [154]. Unlike encapsulated cells which need time to proliferate, spheroids can start with a considerably high density of cells [99]. Spheroids can also mimic the functional and architectural characteristics of target tissue. The spheroidal microcapsules permit intercellular contacts, cell aggregation, and 3D cell growth [155]. Several approaches have been applied to fabricate spheroids for bioprinting purposes, including micromolding, cell sheets, microfluidics, rotating wall vessel techniques, pellet culture, hanging drop, spinner culture, liquid overlay, and external force [99]. Tissue spheroids can fuse and assemble into macrotissues through the process of cell-to-cell adhesion. Norotte et al. [154] successfully utilized multicellular spheroids to construct tubular vascular grafts by 3D bioprinter. The results showed that the closely placed vascular tissue spheroids underwent self-assembly and tissue fusion into a branched vascular tree (Figure 5a). In another study, Tan et al. [156] have successfully utilized 3D bioprinter to robotically place tissue spheroids into the alginate mold to construct toroid-shaped vascular tissue in vitro by the fusion process of tissue spheroids consisting of smooth muscle cells and ECs. In another study, Anada et al. utilized 3D bioprinting to fabricate vascularized bone-mimetic hydrogel constructs, which consist of a central GelMA ring to mimic the bone marrow space and a peripheral GelMA ring to mimic the cortical shell, and [157]. The in vitro results demonstrated the formation of the capillary-like structures originating from the HUVEC spheroids [158] (Figure 5b).
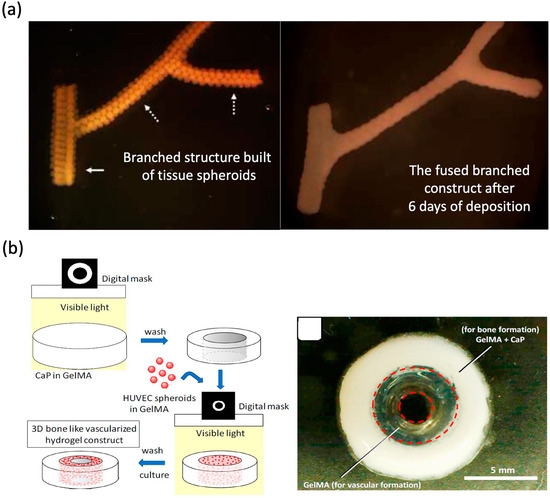
Figure 5.
Tissue spheroid-based approaches for vascular networks. (a) Branched structure built of tissue spheroids and the fused branched construct. (b) Schematic illustration of fabrication process. Reprinted with permission from References [154,157].
4.3. Growth Factor-Based Approaches for Vascular Networks
The process of bone formation involves many influential growth factors, such as angiogenic and osteogenic factors. An alternative strategy is to fabricate the vascular network in tissue-engineered bone tissue by incorporating growth factors into 3D bioprinting constructs. There are many growth factors involved in fabricating vascularized tissue-engineered bone constructs, including vascular platelet-derived growth factor (PDGF), endothelial growth factor (VEGF), fibroblast growth factors (FGFs), epidermal growth factor (EGF), erythropoietin (EPO), transforming growth factor (TGF), hypoxia inducible factor (HIF)-1, BMP-2, and BMP-7 [144,158]. The information of growth factors used to stimulate vasculogenesis is shown in Table 3. Among these growth factors, VEGF has been identified as the most crucial signal protein to stimulate the formation of blood vessels. It is a crucial regulator of physiological vessel formation during embryogenesis [159]. Additionally, VEGF promotes both intramembranous and endochondral ossification by inducing neovascularization [160]. HIF-1 could regulate angiogenesis and vascular remodeling and plays a vital protective role in the pathophysiology of ischemic diseases [161]. EPO plays an important regulatory role in angiogenesis, especially under pathological conditions, and constitutes a crosslink between angiogenesis and hematopoiesis [162]. FGFs, PDGF, and TGF-β could stabilize newly formed blood vessels by recruiting smooth muscle cells. As bone inducers, BMPs induce transcription of numerous osteogenic genes and play a key role in the transformation of mesenchymal cells into bone [163]. Besides, as members of the BMPs, BMP-7 and BMP-2 have been approved for clinical use by the FDA [164]. In addition, stromal-derived factor-1 (SDF-1) is known to act chemotactically on ECs and thereby to enhance the process of angiogenesis [165].

Table 3.
Growth factors used to stimulate vasculogenesis.
Growth factors have a short half-life and are rapidly eliminated, which leads to insufficient amounts [170]. Therefore, a controlled long-term release of growth factors would be helpful in vessel formation in bone tissue constructs [171]. Currently, many growth factor delivery systems have been applied to achieve the goals of sustained release and targeted transport, such as layer-by-layer technology, hydrogel-based delivery and direct adsorption [172,173,174]. Gelatin is a natural product that is used in many kinds of FDA-approved devices. Poldervaart et al. have successfully encapsulated VEGF into gelatin and improved the degree of vascularization [175]. Compared with the single application of growth factors, recent applications also have tried to encapsulate multiple growth factors to improve the osteogenic and angiogenic ability of 3D bioprinting tissue-engineered bone [125,126]. The strongly desired characteristics of advanced bone tissue scaffolds include their ability to regulate the behavior of various cells and to mimic the structure of target tissue. Cui et al. utilized CAD to fabricate a 3D bioprinting bone construct with fluid perfused microvascular structures, and constructed a smart nanoscale release system of dual growth factors (VEGF and BMP-2) [126]. After cultured in co-cultured dynamic fluid systems, the 3D bioprinting scaffolds with dual growth factors and sequential release exhibited excellent bioactivity and vascularized bone forming potential (Figure 6a). In another study, they fabricated a biomimetic vascularized bone construct with regional immobilization of BMP-2 and VEGF [125]. The intrinsic gradient of growth factors within the engineered constructs has been proved to enhance the formation of microcapillaries [39] (Figure 6b). Byambaa et al. [30] utilized 3D bioprinting to fabricate a complex bone-like 3D architectures with vasculogenic and osteogenic niches. Moreover, to promote vascular spreading, chemically conjugated VEGF with gradient concentrations were constructed around bone niches. (Figure 6c).
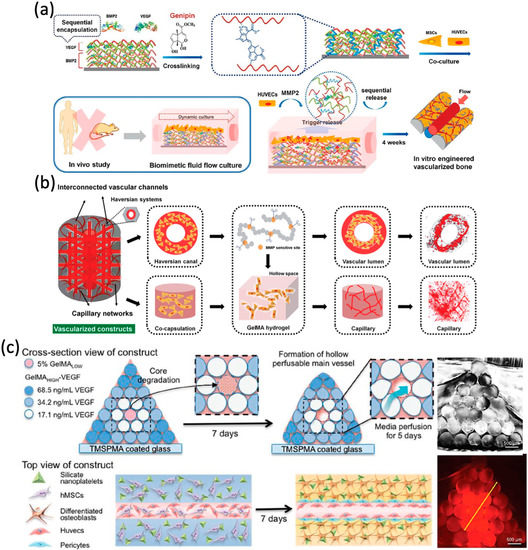
Figure 6.
Growth factor-based approaches for vascular networks. (a) Schematic representation of sequential release of growth factors. (b) Schematic representation of microstructural design of vascularized construct. (c) Illustration of the bioprinting strategy for fabricating complex bone tissue architecture. Reprinted with permission from References [30,125,126].
4.4. Small Moleculers-Based Approaches for Vascular Networks
Distinct from growth factors, small molecules are low molecular weight molecules, such as lipids, metabolites, and drugs [176]. Recently, many kinds of small molecules were synthesized to enhance angiogenesis. Sildenafil, a phosphodiesterase type 5 inhibitor, not only enhances nitric oxide metabolism but has been shown to improve vascular endothelial function [177]. Lithium was also shown to have a concentration-dependent effect on early vascular development in the chick embryo area vasculosa [178]. Delivery of FTY720, a selective agonist for the sphingosine 1-phosphate receptor, has also been proven to enlarge existing arterioles and enhance the formation of new arterioles [166].
Functional peptides are much smaller than full-length growth factors, which are easier to synthesize and cheaper [179]. The functional motif KLT (KLTWQELYQLKYKGI) is a VEGF mimetic peptide and could combined to VEGF receptors and improve the migration, proliferation, and tubulogenesis of ECs [180]. Lu et al. modified hyaluronic acid hydrogels with KLT and demonstrated that the HA-KLT hydrogel could improve the spreading, and proliferation of HUVECs in vitro and promoted angiogenesis in vivo [181]. The glycine-histidine-lysine (GHK) peptide is a fragment of osteonectin, and could promote the secretion of VEGF from MSCs in alginate hydrogels [182]. In addition, Klontzas et al. demonstrated that the oxidized alginate hydrogels modified with GHK significantly improved osteogenic differentiation of encapsulated MSCs in vitro [183]. Even though the use of peptides in bioprinting is actual quite unexplored, they show great potency in the fabrication of vascularized 3D tissue-engineered bone constructs.
5. The Application of 3D Vascularized Models
3D bioprinting technology could precisely control complex 3D architecture and spatial distribution to fabricate 3D vascularized models, which could have great potential for the applications in drug toxicology, drug screening, and potentially disease modeling [20]. Engineered blood vessels can be integrated into 3D biomimetic tissue constructs by 3D bioprinting to mimic the drug administration process in vivo. Massa et al. utilized 3D bioprinting technology to construct a vascularized tissue-engineered model for mimicking physiological drug diffusion and drug toxicity testing [184]. The results demonstrated that the integration of vascularized tissue engineering constructs with bioreactors can helps to fabricate a new, more realistic platform that bridge the gap between in vivo and in vitro drug testing models [184]. Bhise et al. fabricated an organ-on-a-chip platform by combining a 3D bioprinted tissue-engineered construct with a bioreactor [185]. The results demonstrated organ-on-a-chip platform could be a valuable approach for drug toxicity analysis [185]. In addition, Zhou et al. utilized 3D bioprinting technology to constuct a 3D bioprinted tissue-engineered bone construct that facilitates the integration of MSCs, breast cancer (BrCa) cells, and osteoblasts [186]. BrCa cell morphology, migration, and interaction with MSCs and osteoblasts in this system were studied. The results demonstrated that 3D bioprinted tissue-engineered bone construct could be an effective disease model for investigating breast cancer bone invasion and metastasis.
6. Conclusions and Challenges
In recent years, 3D bioprinting has been an emerging and accurate technology to fabricate vascularized tissue-engineered bone constructs layer by layer. Combined with clinical imaging techniques, more complex biomimetic bone structures with multiple types of cells spatially arranged could be bioprinted for clinical transplantation. Although there are several reviews on 3D bioprinting, to our best knowledge, this review is the first review to examine the role of vascularization in bone tissue fabrication during the process of 3D bioprinting. In our review, we recap the current status of 3D bioprinting technology for the fabrication of vascularized tissue-engineered bone. Although successful bioprinting of various vascularized tissue-engineered bone constructs has been reported, several contemporary issues of bioprinting still require focused efforts. Firstly, there is no standard guideline for the overall process of 3D bioprinting technology. Secondly, compared with avascular cartilage tissue with a small number of chondrocytes, the structural complexity of bone tissue increases the difficulty of fabrication. Additionally, different regions of bone tissue in the human body might have different biomechanical properties and microenvironment architectures. Therefore, accurate acquisition of imaging data, computational simulation, and mathematical models might help in designing the structure of target tissue. Thirdly, unlike some tissues that contain only one type of cells, the fabrication of vascularized tissue-engineered bone needs at least two types of cells. Therefore, how to maintain cell viability throughout the process of bioprinting and ensure the exchange of nutrients and bioactive factors between host and tissue-engineered constructs are important. In our opinion, more complex and intelligent bioinks are required to sustain cell bioactivity and mimic the properties of nature tissues. Additionally, long-term cell viability, the intercellular interactions, and cell-to-material interactions after bioprinting should be monitored precisely. Fourthly, bone tissue is a hard tissue, which provides structure and support for the body. In order to fabricate biomimetic tissue-engineered bone constructs, good mechanical properties of scaffolds are necessary. In our opinion, bioinks should be modified to enhance its mechanical strength and the shape fidelity. In addition, when dealing with defects in weight-bearing areas, acellular load bearing implants followed by bioprinting cell-laden bioinks (such as [125]) might be a good solution. Finally, we believe that further developments in 3D bioprinting in the near future will undoubtedly propel the field of bone regeneration to a new height by fabricating biomimetic vascularized tissue-engineered bone constructs.
Author Contributions
Conceptualization, U.R.; investigation and resources, U.R. and F.X.; original draft preparation, F.X.; review and editing, U.R. and Z.X.; supervision and project administration, U.R. and P.M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was financially supported by Foundation of Sino-German center for Research promotion (GZ1219) and Natural Science Foundations of China (No.31870961).
Conflicts of Interest
The authors declare no conflict of interest.
References
- El-Rashidy, A.A.; Roether, J.A.; Harhaus, L.; Kneser, U.; Boccaccini, A.R. Regenerating bone with bioactive glass scaffolds: A review of in vivo studies in bone defect models. Acta Biomater. 2017, 62, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Myeroff, C.; Archdeacon, M. Autogenous bone graft: Donor sites and techniques. J. Bone Joint Surg. 2011, 93, 2227–2236. [Google Scholar] [CrossRef] [PubMed]
- Pape, H.C.; Evans, A.; Kobbe, P. Autologous bone graft: Properties and techniques. J. Orthop. Trauma 2010, 24, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Petite, H.; Viateau, V.; Bensaïd, W.; Meunier, A.; de Pollak, C.; Bourguignon, M.; Oudina, K.; Sedel, L.; Guillemin, G. Tissue-engineered bone regeneration. Nat. Biotechnol. 2000, 18, 959–963. [Google Scholar] [CrossRef]
- Cui, X.; Boland, T. Human microvasculature fabrication using thermal inkjet printing technology. Biomaterials 2009, 30, 6221–6227. [Google Scholar] [CrossRef]
- Zhang, Z.-Y.; Teoh, S.-H.; Chong, M.S.K.; Lee, E.S.M.; Tan, L.-G.; Mattar, C.N.; Fisk, N.M.; Choolani, M.; Chan, J. Neo-vascularization and bone formation mediated by fetal mesenchymal stem cell tissue-engineered bone grafts in critical-size femoral defects. Biomaterials 2010, 31, 608–620. [Google Scholar] [CrossRef]
- Yu, H.; VandeVord, P.J.; Mao, L.; Matthew, H.W.; Wooley, P.H.; Yang, S.-Y. Improved tissue-engineered bone regeneration by endothelial cell mediated vascularization. Biomaterials 2009, 30, 508–517. [Google Scholar] [CrossRef]
- Zhou, J.; Lin, H.; Fang, T.; Li, X.; Dai, W.; Uemura, T.; Dong, J. The repair of large segmental bone defects in the rabbit with vascularized tissue engineered bone. Biomaterials 2010, 31, 1171–1179. [Google Scholar] [CrossRef]
- Zou, D.; Zhang, Z.; He, J.; Zhang, K.; Ye, D.; Han, W.; Zhou, J.; Wang, Y.; Li, Q.; Liu, X.; et al. Blood vessel formation in the tissue-engineered bone with the constitutively active form of HIF-1α mediated BMSCs. Biomaterials 2012, 33, 2097–2108. [Google Scholar] [CrossRef]
- Yu, X.; Tang, X.; Gohil, S.V.; Laurencin, C.T. Biomaterials for Bone Regenerative Engineering. Adv. Healthc. Mater. 2015, 4, 1268–1285. [Google Scholar] [CrossRef]
- Midha, S.; Dalela, M.; Sybil, D.; Patra, P.; Mohanty, S. Advances in three-dimensional bioprinting of bone: Progress and challenges. J. Tissue Eng. Regen. Med. 2019, 13, 925–945. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Vijayavenkataraman, S.; Yan, W.-C.; Lu, W.F.; Wang, C.-H.; Fuh, J.Y.H. 3D bioprinting of tissues and organs for regenerative medicine. Adv. Drug Deliv. Rev. 2018, 132, 296–332. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.S.; Duchamp, M.; Oklu, R.; Ellisen, L.W.; Langer, R.; Khademhosseini, A. Bioprinting the Cancer Microenvironment. ACS Biomater. Sci. Eng. 2016, 2, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Mironov, V.; Reis, N.; Derby, B. Review: Bioprinting: A beginning. Tissue Eng. 2006, 12, 631–634. [Google Scholar] [CrossRef]
- Chieruzzi, M.; Pagano, S.; Moretti, S.; Pinna, R.; Milia, E.; Torre, L.; Eramo, S. Nanomaterials for Tissue Engineering in Dentistry. Nanomaterials 2016, 6, 134. [Google Scholar] [CrossRef]
- Li, Y.; Liu, C. Nanomaterial-based bone regeneration. Nanoscale 2017, 9, 4862–4874. [Google Scholar] [CrossRef]
- Zhang, Y.S.; Oklu, R.; Dokmeci, M.R.; Khademhosseini, A. Three-Dimensional Bioprinting Strategies for Tissue Engineering. Cold Spring Harb. Perspect. Med. 2018, 8, a025718. [Google Scholar] [CrossRef]
- Mandrycky, C.; Wang, Z.; Kim, K.; Kim, D.-H. 3D bioprinting for engineering complex tissues. Biotechnol. Adv. 2016, 34, 422–434. [Google Scholar] [CrossRef]
- Ma, X.; Liu, J.; Zhu, W.; Tang, M.; Lawrence, N.; Yu, C.; Gou, M.; Chen, S. 3D bioprinting of functional tissue models for personalized drug screening and in vitro disease modeling. Adv. Drug Deliv. Rev. 2018, 132, 235–251. [Google Scholar] [CrossRef]
- Cui, H.; Nowicki, M.; Fisher, J.P.; Zhang, L.G. 3D Bioprinting for Organ Regeneration. Adv. Healthc. Mater. 2017, 6, 1601118. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, H. Current Progress in 3D Bioprinting of Tissue Analogs. SLAS TECHNOL. Transl. Life Sci. Innov. 2018, 24, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, P. Mechanisms of angiogenesis and arteriogenesis. Nat. Med. 2000, 6, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Vailhé, B.; Vittet, D.; Feige, J.-J. In Vitro Models of Vasculogenesis and Angiogenesis. Lab. Investig. 2001, 81, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Rouwkema, J.; Rivron, N.C.; van Blitterswijk, C.A. Vascularization in tissue engineering. Trends Biotechnol. 2008, 26, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Rouwkema, J.; Khademhosseini, A. Vascularization and Angiogenesis in Tissue Engineering: Beyond Creating Static Networks. Trends Biotechnol. 2016, 34, 733–745. [Google Scholar] [CrossRef]
- Sun, X.; Altalhi, W.; Nunes, S.S. Vascularization strategies of engineered tissues and their application in cardiac regeneration. Adv. Drug Deliv. Rev. 2016, 96, 183–194. [Google Scholar] [CrossRef]
- Folkman, J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat. Med. 1995, 1, 27–31. [Google Scholar] [CrossRef]
- Bae, H.; Puranik, A.S.; Gauvin, R.; Edalat, F.; Carrillo-Conde, B.; Peppas, N.A.; Khademhosseini, A. Building vascular networks. Sci. Transl. Med. 2012, 4, 160ps123. [Google Scholar] [CrossRef]
- Byambaa, B.; Annabi, N.; Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Jia, W.; Kazemzadeh-Narbat, M.; Shin, S.R.; Tamayol, A.; Khademhosseini, A. Bioprinted Osteogenic and Vasculogenic Patterns for Engineering 3D Bone Tissue. Adv. Healthc. Mater. 2017, 6, 1700015. [Google Scholar] [CrossRef]
- Tomlinson, R.E.; Silva, M.J. Skeletal Blood Flow in Bone Repair and Maintenance. Bone Res. 2013, 1, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Datta, P.; Ayan, B.; Ozbolat, I.T. Bioprinting for vascular and vascularized tissue biofabrication. Acta Biomater. 2017, 51, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Kanczler, J.M.; Oreffo, R.O.C. Osteogenesis and angiogenesis: The potential for engineering bone. Eur. Cells Mater. 2008, 15, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Zhang, P.; Xu, Z.; Chen, H.; Xie, X. GPNMB enhances bone regeneration by promoting angiogenesis and osteogenesis: Potential role for tissue engineering bone. J. Cell. Biochem. 2013, 114, 2729–2737. [Google Scholar] [CrossRef] [PubMed]
- Maes, C.; Kobayashi, T.; Selig, M.K.; Torrekens, S.; Roth, S.I.; Mackem, S.; Carmeliet, G.; Kronenberg, H.M. Osteoblast precursors, but not mature osteoblasts, move into developing and fractured bones along with invading blood vessels. Dev. Cell 2010, 19, 329–344. [Google Scholar] [CrossRef]
- Dirckx, N.; Van Hul, M.; Maes, C. Osteoblast recruitment to sites of bone formation in skeletal development, homeostasis, and regeneration. Birth Defects Res. C Embryo Today Rev. 2013, 99, 170–191. [Google Scholar] [CrossRef]
- Percival, C.J.; Richtsmeier, J.T. Angiogenesis and intramembranous osteogenesis. Dev. Dyn. 2013, 242, 909–922. [Google Scholar] [CrossRef]
- Jain, R.K.; Au, P.; Tam, J.; Duda, D.G.; Fukumura, D. Engineering vascularized tissue. Nat. Biotechnol. 2005, 23, 821–823. [Google Scholar] [CrossRef]
- Discher, D.E.; Mooney, D.J.; Zandstra, P.W. Growth factors, matrices, and forces combine and control stem cells. Science 2009, 324, 1673–1677. [Google Scholar] [CrossRef]
- Kang, H.-W.; Lee, S.J.; Ko, I.K.; Kengla, C.; Yoo, J.J.; Atala, A. A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol. 2016, 34, 312–319. [Google Scholar] [CrossRef]
- Athirasala, A.; Tahayeri, A.; Thrivikraman, G.; França, C.M.; Monteiro, N.; Tran, V.; Ferracane, J.; Bertassoni, L.E. A dentin-derived hydrogel bioink for 3D bioprinting of cell laden scaffolds for regenerative dentistry. Biofabrication 2018, 10, 024101. [Google Scholar] [CrossRef] [PubMed]
- Ostrovidov, S.; Salehi, S.; Costantini, M.; Suthiwanich, K.; Ebrahimi, M.; Sadeghian, R.B.; Fujie, T.; Shi, X.; Cannata, S.; Gargioli, C.; et al. 3D Bioprinting in Skeletal Muscle Tissue Engineering. Small (Weinh. Bergstr. Ger.) 2019, 15, e1805530. [Google Scholar] [CrossRef] [PubMed]
- Sodupe-Ortega, E.; Sanz-Garcia, A.; Pernia-Espinoza, A.; Escobedo-Lucea, C. Accurate Calibration in Multi-Material 3D Bioprinting for Tissue Engineering. Materials 2018, 11, 1402. [Google Scholar] [CrossRef] [PubMed]
- Matai, I.; Kaur, G.; Seyedsalehi, A.; McClinton, A.; Laurencin, C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 2020, 226, 119536. [Google Scholar] [CrossRef] [PubMed]
- Chimene, D.; Peak, C.W.; Gentry, J.L.; Carrow, J.K.; Cross, L.M.; Mondragon, E.; Cardoso, G.B.; Kaunas, R.; Gaharwar, A.K. Nanoengineered Ionic-Covalent Entanglement (NICE) Bioinks for 3D Bioprinting. ACS Appl. Mater. Interfaces 2018, 10, 9957–9968. [Google Scholar] [CrossRef] [PubMed]
- Merceron, T.K.; Burt, M.; Seol, Y.-J.; Kang, H.-W.; Lee, S.J.; Yoo, J.J.; Atala, A. A 3D bioprinted complex structure for engineering the muscle-tendon unit. Biofabrication 2015, 7, 035003. [Google Scholar] [CrossRef]
- Marques, C.F.; Diogo, G.S.; Pina, S.; Oliveira, J.M.; Silva, T.H.; Reis, R.L. Collagen-based bioinks for hard tissue engineering applications: A comprehensive review. J. Mater. Sci. Mater. Med. 2019, 30, 32. [Google Scholar] [CrossRef]
- Sigaux, N.; Pourchet, L.; Breton, P.; Brosset, S.; Louvrier, A.; Marquette, C.A. 3D Bioprinting: Principles, fantasies and prospects. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 128–132. [Google Scholar] [CrossRef]
- Guillemot, F.; Souquet, A.; Catros, S.; Guillotin, B.; Lopez, J.; Faucon, M.; Pippenger, B.; Bareille, R.; Rémy, M.; Bellance, S. High-throughput laser printing of cells and biomaterials for tissue engineering. Acta Biomater. 2010, 6, 2494–2500. [Google Scholar] [CrossRef]
- Panwar, A.; Tan, L.P. Current Status of Bioinks for Micro-Extrusion-Based 3D Bioprinting. Molecules 2016, 21, 685. [Google Scholar] [CrossRef]
- Billiet, T.; Vandenhaute, M.; Schelfhout, J.; Van Vlierberghe, S.; Dubruel, P. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials 2012, 33, 6020–6041. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.; Schilling, A.F.; Hubbell, K.; Yonezawa, T.; Truong, D.; Hong, Y.; Dai, G.; Cui, X. Improved properties of bone and cartilage tissue from 3D inkjet-bioprinted human mesenchymal stem cells by simultaneous deposition and photocrosslinking in PEG-GelMA. Biotechnol. Lett. 2015, 37, 2349–2355. [Google Scholar] [CrossRef] [PubMed]
- Compaan, A.M.; Christensen, K.; Huang, Y. Inkjet bioprinting of 3D silk fibroin cellular constructs using sacrificial alginate. ACS Biomater. Sci. Eng. 2017, 3, 1519–1526. [Google Scholar] [CrossRef]
- Gungor-Ozkerim, P.S.; Inci, I.; Zhang, Y.S.; Khademhosseini, A.; Dokmeci, M.R. Bioinks for 3D bioprinting: An overview. Biomater. Sci. 2018, 6, 915–946. [Google Scholar] [CrossRef] [PubMed]
- Patuzzo, S.; Goracci, G.; Gasperini, L.; Ciliberti, R. 3D bioprinting technology: Scientific aspects and ethical issues. Sci. Eng. Ethics 2018, 24, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Ozbolat, I.T.; Yu, Y. Bioprinting toward organ fabrication: Challenges and future trends. IEEE Trans. Biomed. Eng. 2013, 60, 691–699. [Google Scholar] [CrossRef]
- Pati, F.; Jang, J.; Ha, D.-H.; Kim, S.W.; Rhie, J.-W.; Shim, J.-H.; Kim, D.-H.; Cho, D.-W. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat. Commun. 2014, 5, 1–11. [Google Scholar] [CrossRef]
- Wang, X.; Ao, Q.; Tian, X.; Fan, J.; Wei, Y.; Hou, W.; Tong, H.; Bai, S. 3D bioprinting technologies for hard tissue and organ engineering. Materials 2016, 9, 802. [Google Scholar] [CrossRef]
- Levato, R.; Webb, W.R.; Otto, I.A.; Mensinga, A.; Zhang, Y.; van Rijen, M.; van Weeren, R.; Khan, I.M.; Malda, J. The bio in the ink: Cartilage regeneration with bioprintable hydrogels and articular cartilage-derived progenitor cells. Acta Biomater. 2017, 61, 41–53. [Google Scholar] [CrossRef]
- Mouser, V.H.M.; Abbadessa, A.; Levato, R.; Hennink, W.; Vermonden, T.; Gawlitta, D.; Malda, J. Development of a thermosensitive HAMA-containing bio-ink for the fabrication of composite cartilage repair constructs. Biofabrication 2017, 9, 015026. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, Y.; Akkouch, A.; Dababneh, A.; Dolati, F.; Ozbolat, I.T. In vitro study of directly bioprinted perfusable vasculature conduits. Biomater. Sci. 2015, 3, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Skeldon, G.; Lucendo-Villarin, B.; Shu, W. Three-dimensional bioprinting of stem-cell derived tissues for human regenerative medicine. Philos. Trans. R. Soc. B Biol. Sci. 2018, 373, 20170224. [Google Scholar] [CrossRef] [PubMed]
- Jia, W.; Gungor-Ozkerim, P.S.; Zhang, Y.S.; Yue, K.; Zhu, K.; Liu, W.; Pi, Q.; Byambaa, B.; Dokmeci, M.R.; Shin, S.R. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials 2016, 106, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Yanez, M.; Rincon, J.; Dones, A.; De Maria, C.; Gonzales, R.; Boland, T. In vivo assessment of printed microvasculature in a bilayer skin graft to treat full-thickness wounds. Tissue Eng. Part A 2015, 21, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.N.; Lancaster, K.Z.; Zhen, G.; He, J.; Gupta, M.K.; Kong, Y.L.; Engel, E.A.; Krick, K.D.; Ju, A.; Meng, F. 3D printed anatomical nerve regeneration pathways. Adv. Funct. Mater. 2015, 25, 6205–6217. [Google Scholar] [CrossRef]
- Ng, W.L.; Yeong, W.Y.; Naing, M.W. Polyelectrolyte gelatin-chitosan hydrogel optimized for 3D bioprinting in skin tissue engineering. Int. J. Bioprint. 2016, 2, 53–62. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, X.F.; Gao, G.; Yonezawa, T.; Cui, X. 3D bioprinting and the current applications in tissue engineering. Biotechnol. J. 2017, 12, 1600734. [Google Scholar] [CrossRef]
- Miller, J.S.; Stevens, K.R.; Yang, M.T.; Baker, B.M.; Nguyen, D.-H.T.; Cohen, D.M.; Toro, E.; Chen, A.A.; Galie, P.A.; Yu, X. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat. Mater. 2012, 11, 768–774. [Google Scholar] [CrossRef]
- Xu, T.; Binder, K.W.; Albanna, M.Z.; Dice, D.; Zhao, W.; Yoo, J.J.; Atala, A. Hybrid printing of mechanically and biologically improved constructs for cartilage tissue engineering applications. Biofabrication 2012, 5, 015001. [Google Scholar] [CrossRef]
- Chang, R.; Emami, K.; Wu, H.; Sun, W. Biofabrication of a three-dimensional liver micro-organ as an in vitro drug metabolism model. Biofabrication 2010, 2, 045004. [Google Scholar] [CrossRef]
- Phillippi, J.A.; Miller, E.; Weiss, L.; Huard, J.; Waggoner, A.; Campbell, P. Microenvironments engineered by inkjet bioprinting spatially direct adult stem cells toward muscle-and bone-like subpopulations. Stem Cells 2008, 26, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Skardal, A.; Mack, D.; Kapetanovic, E.; Atala, A.; Jackson, J.D.; Yoo, J.; Soker, S. Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl. Med. 2012, 1, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Koch, L.; Kuhn, S.; Sorg, H.; Gruene, M.; Schlie, S.; Gaebel, R.; Polchow, B.; Reimers, K.; Stoelting, S.; Ma, N. Laser printing of skin cells and human stem cells. Tissue Eng. Part C Methods 2010, 16, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Gaetani, R.; Doevendans, P.A.; Metz, C.H.; Alblas, J.; Messina, E.; Giacomello, A.; Sluijter, J.P. Cardiac tissue engineering using tissue printing technology and human cardiac progenitor cells. Biomaterials 2012, 33, 1782–1790. [Google Scholar] [CrossRef]
- Gaetani, R.; Feyen, D.A.M.; Verhage, V.; Slaats, R.; Messina, E.; Christman, K.L.; Giacomello, A.; Doevendans, P.A.F.M.; Sluijter, J.P.G. Epicardial application of cardiac progenitor cells in a 3D-printed gelatin/hyaluronic acid patch preserves cardiac function after myocardial infarction. Biomaterials 2015, 61, 339–348. [Google Scholar] [CrossRef]
- Li, J.; Chen, M.; Fan, X.; Zhou, H. Recent advances in bioprinting techniques: Approaches, applications and future prospects. J. Transl. Med. 2016, 14, 271. [Google Scholar] [CrossRef]
- Angelopoulos, I.; Allenby, M.C.; Lim, M.; Zamorano, M. Engineering inkjet bioprinting processes toward translational therapies. Biotechnol. Bioeng. 2020, 117, 272–284. [Google Scholar] [CrossRef]
- Alonzo, M.; AnilKumar, S.; Roman, B.; Tasnim, N.; Joddar, B. 3D Bioprinting of cardiac tissue and cardiac stem cell therapy. Transl. Res. 2019, 211, 64–83. [Google Scholar] [CrossRef]
- Solis, L.H.; Ayala, Y.; Portillo, S.; Varela-Ramirez, A.; Aguilera, R.; Boland, T. Thermal inkjet bioprinting triggers the activation of the VEGF pathway in human microvascular endothelial cells in vitro. Biofabrication 2019, 11, 045005. [Google Scholar] [CrossRef]
- Masaeli, E.; Forster, V.; Picaud, S.; Karamali, F.; Nasr-Esfahani, M.H.; Marquette, C. Tissue engineering of retina through high resolution 3-dimensional inkjet bioprinting. Biofabrication 2020, 12, 025006. [Google Scholar] [CrossRef]
- Xu, T.; Jin, J.; Gregory, C.; Hickman, J.J.J.J.; Boland, T. Inkjet printing of viable mammalian cells. Biomaterials 2005, 26, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Dean, D.; Ruggeri, Z.M.; Boland, T. Cell damage evaluation of thermal inkjet printed Chinese hamster ovary cells. Biotechnol. Bioeng. 2010, 106, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Chai, W.; Huang, Y.; Markwald, R.R. Scaffold-free inkjet printing of three-dimensional zigzag cellular tubes. Biotechnol. Bioeng. 2012, 109, 3152–3160. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.K.; Kim, D.Y.; Ngo, H.; Lee, Y.; Seo, L.; Yoo, S.-S.; Vincent, P.A.; Dai, G. Creating perfused functional vascular channels using 3D bio-printing technology. Biomaterials 2014, 35, 8092–8102. [Google Scholar] [CrossRef]
- Lee, V.K.; Lanzi, A.M.; Haygan, N.; Yoo, S.-S.; Vincent, P.A.; Dai, G. Generation of Multi-Scale Vascular Network System within 3D Hydrogel using 3D Bio-Printing Technology. Cell. Mol. Bioeng. 2014, 7, 460–472. [Google Scholar] [CrossRef]
- Jana, S.; Lerman, A. Bioprinting a cardiac valve. Biotechnol. Adv. 2015, 33, 1503–1521. [Google Scholar] [CrossRef]
- Axpe, E.; Oyen, M.L. Applications of Alginate-Based Bioinks in 3D Bioprinting. Int. J. Mol. Sci. 2016, 17, 1976. [Google Scholar] [CrossRef]
- Parak, A.; Pradeep, P.; du Toit, L.C.; Kumar, P.; Choonara, Y.E.; Pillay, V. Functionalizing bioinks for 3D bioprinting applications. Drug Discov. Today 2019, 24, 198–205. [Google Scholar] [CrossRef]
- Guillotin, B.; Souquet, A.; Catros, S.; Duocastella, M.; Pippenger, B.; Bellance, S.; Bareille, R.; Rémy, M.; Bordenave, L.; Amédée, J.; et al. Laser assisted bioprinting of engineered tissue with high cell density and microscale organization. Biomaterials 2010, 31, 7250–7256. [Google Scholar] [CrossRef]
- Keriquel, V.; Guillemot, F.; Arnault, I.; Guillotin, B.; Miraux, S.; Amédée, J.; Fricain, J.-C.; Catros, S. In vivo bioprinting for computer- and robotic-assisted medical intervention: Preliminary study in mice. Biofabrication 2010, 2, 014101. [Google Scholar] [CrossRef]
- Wu, P.; Ringeisen, B. Development of human umbilical vein endothelial cell (HUVEC) and human umbilical vein smooth muscle cell (HUVSMC) branch/stem structures on hydrogel layers via biological laser printing (BioLP). Biofabrication 2010, 2, 014111. [Google Scholar] [CrossRef] [PubMed]
- Gruene, M.; Pflaum, M.; Deiwick, A.; Koch, L.; Schlie, S.; Unger, C.; Wilhelmi, M.; Haverich, A.; Chichkov, B.N. Adipogenic differentiation of laser-printed 3D tissue grafts consisting of human adipose-derived stem cells. Biofabrication 2011, 3, 015005. [Google Scholar] [CrossRef] [PubMed]
- Kérourédan, O.; Bourget, J.M.; Rémy, M.; Crauste-Manciet, S.; Kalisky, J.; Catros, S.; Thébaud, N.B.; Devillard, R. Micropatterning of endothelial cells to create a capillary-like network with defined architecture by laser-assisted bioprinting. J. Mater. Sci. Mater. Med. 2019, 30, 28. [Google Scholar] [CrossRef] [PubMed]
- Kérourédan, O.; Hakobyan, D.; Rémy, M.; Ziane, S.; Dusserre, N.; Fricain, J.-C.; Delmond, S.; Thébaud, N.B.; Devillard, R. In situ prevascularization designed by laser-assisted bioprinting: Effect on bone regeneration. Biofabrication 2019, 11, 045002. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Y. Tissue Engineering Applications of Three-Dimensional Bioprinting. Cell Biochem. Biophys. 2015, 72, 777–782. [Google Scholar] [CrossRef]
- Chang, C.C.; Boland, E.D.; Williams, S.K.; Hoying, J.B. Direct-write bioprinting three-dimensional biohybrid systems for future regenerative therapies. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011, 98, 160–170. [Google Scholar] [CrossRef]
- Nair, K.; Gandhi, M.; Khalil, S.; Yan, K.C.; Marcolongo, M.; Barbee, K.; Sun, W. Characterization of cell viability during bioprinting processes. Biotechnol. J. 2009, 4, 1168–1177. [Google Scholar] [CrossRef]
- Gao, Q.; He, Y.; Fu, J.-Z.; Liu, A.; Ma, L. Coaxial nozzle-assisted 3D bioprinting with built-in microchannels for nutrients delivery. Biomaterials 2015, 61, 203–215. [Google Scholar] [CrossRef]
- Ozbolat, I.T. Scaffold-Based or Scaffold-Free Bioprinting: Competing or Complementing Approaches? J. Nanotechnol. Eng. Med. 2015, 6. [Google Scholar] [CrossRef]
- Miri, A.K.; Khalilpour, A.; Cecen, B.; Maharjan, S.; Shin, S.R.; Khademhosseini, A. Multiscale bioprinting of vascularized models. Biomaterials 2019, 198, 204–216. [Google Scholar] [CrossRef]
- Billiet, T.; Gevaert, E.; De Schryver, T.; Cornelissen, M.; Dubruel, P. The 3D printing of gelatin methacrylamide cell-laden tissue-engineered constructs with high cell viability. Biomaterials 2014, 35, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Marga, F.; Jakab, K.; Khatiwala, C.; Shepherd, B.; Dorfman, S.; Hubbard, B.; Colbert, S.; Gabor, F. Toward engineering functional organ modules by additive manufacturing. Biofabrication 2012, 4, 022001. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.Y.S.; Yeong, W.Y. Concentric bioprinting of alginate-based tubular constructs using multi-nozzle extrusion-based technique. Int. J. Bioprint. 2015, 1, 49–57. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, Y.; Ozbolat, I.T. Direct Bioprinting of Vessel-Like Tubular Microfluidic Channels. J. Nanotechnol. Eng. Med. 2013, 4, 020902. [Google Scholar] [CrossRef]
- Dolati, F.; Yu, Y.; Zhang, Y.; Jesus, A.M.D.; Sander, E.A.; Ozbolat, I.T. In vitroevaluation of carbon-nanotube-reinforced bioprintable vascular conduits. Nanotechnology 2014, 25, 145101. [Google Scholar] [CrossRef]
- Smith, C.M.; Stone, A.L.; Parkhill, R.L.; Stewart, R.L.; Simpkins, M.W.; Kachurin, A.M.; Warren, W.L.; Williams, S.K. Three-dimensional bioassembly tool for generating viable tissue-engineered constructs. Tissue Eng. 2004, 10, 1566–1576. [Google Scholar] [CrossRef]
- Colosi, C.; Shin, S.R.; Manoharan, V.; Massa, S.; Costantini, M.; Barbetta, A.; Dokmeci, M.R.; Dentini, M.; Khademhosseini, A. Microfluidic bioprinting of heterogeneous 3D tissue constructs using low-viscosity bioink. Adv. Mater. 2016, 28, 677–684. [Google Scholar] [CrossRef]
- Groll, J.; Burdick, J.A.; Cho, D.W.; Derby, B.; Gelinsky, M.; Heilshorn, S.C.; Jüngst, T.; Malda, J.; Mironov, V.A.; Nakayama, K.; et al. A definition of bioinks and their distinction from biomaterial inks. Biofabrication 2018, 11, 013001. [Google Scholar] [CrossRef]
- Gopinathan, J.; Noh, I. Recent trends in bioinks for 3D printing. Biomater. Res. 2018, 22, 11. [Google Scholar] [CrossRef]
- Chawla, S.; Midha, S.; Sharma, A.; Ghosh, S. Silk-Based Bioinks for 3D Bioprinting. Adv. Healthc. Mater. 2018, 7, e1701204. [Google Scholar] [CrossRef]
- Das, S.; Pati, F.; Choi, Y.-J.; Rijal, G.; Shim, J.-H.; Kim, S.W.; Ray, A.R.; Cho, D.-W.; Ghosh, S. Bioprintable, cell-laden silk fibroin–gelatin hydrogel supporting multilineage differentiation of stem cells for fabrication of three-dimensional tissue constructs. Acta Biomater. 2015, 11, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.T.; Daly, K.A.; Brennan-Pierce, E.P.; Johnson, S.A.; Carruthers, C.A.; D’Amore, A.; Nagarkar, S.P.; Velankar, S.S.; Badylak, S.F. A hydrogel derived from decellularized dermal extracellular matrix. Biomaterials 2012, 33, 7028–7038. [Google Scholar] [CrossRef] [PubMed]
- Lambricht, L.; De Berdt, P.; Vanacker, J.; Leprince, J.; Diogenes, A.; Goldansaz, H.; Bouzin, C.; Préat, V.; Dupont-Gillain, C.; Des Rieux, A. The type and composition of alginate and hyaluronic-based hydrogels influence the viability of stem cells of the apical papilla. Dent. Mater. 2014, 30, e349–e361. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.; Yonezawa, T.; Hubbell, K.; Dai, G.; Cui, X. Inkjet-bioprinted acrylated peptides and PEG hydrogel with human mesenchymal stem cells promote robust bone and cartilage formation with minimal printhead clogging. Biotechnol. J. 2015, 10, 1568–1577. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Fu, Q.; Yoo, J.; Chen, X.; Chandra, P.; Mo, X.; Song, L.; Atala, A.; Zhao, W. 3D bioprinting of urethra with PCL/PLCL blend and dual autologous cells in fibrin hydrogel: An in vitro evaluation of biomimetic mechanical property and cell growth environment. Acta Biomater. 2017, 50, 154–164. [Google Scholar] [CrossRef]
- Pati, F.; Ha, D.-H.; Jang, J.; Han, H.H.; Rhie, J.-W.; Cho, D.-W. Biomimetic 3D tissue printing for soft tissue regeneration. Biomaterials 2015, 62, 164–175. [Google Scholar] [CrossRef]
- Shanjani, Y.; Pan, C.C.; Elomaa, L.; Yang, Y. A novel bioprinting method and system for forming hybrid tissue engineering constructs. Biofabrication 2015, 7, 045008. [Google Scholar] [CrossRef]
- Jia, J.; Richards, D.J.; Pollard, S.; Tan, Y.; Rodriguez, J.; Visconti, R.P.; Trusk, T.C.; Yost, M.J.; Yao, H.; Markwald, R.R.; et al. Engineering alginate as bioink for bioprinting. Acta Biomater. 2014, 10, 4323–4331. [Google Scholar] [CrossRef]
- Ma, X.; Qu, X.; Zhu, W.; Li, Y.-S.; Yuan, S.; Zhang, H.; Liu, J.; Wang, P.; Lai, C.S.E.; Zanella, F.; et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proc. Natl. Acad. Sci. USA 2016, 113, 2206–2211. [Google Scholar] [CrossRef]
- Yu, J.; Du, K.T.; Fang, Q.; Gu, Y.; Mihardja, S.S.; Sievers, R.E.; Wu, J.C.; Lee, R.J. The use of human mesenchymal stem cells encapsulated in RGD modified alginate microspheres in the repair of myocardial infarction in the rat. Biomaterials 2010, 31, 7012–7020. [Google Scholar] [CrossRef]
- Kundu, J.; Shim, J.-H.; Jang, J.; Kim, S.-W.; Cho, D.-W. An additive manufacturing-based PCL-alginate-chondrocyte bioprinted scaffold for cartilage tissue engineering. J. Tissue Eng. Regen. Med. 2015, 9, 1286–1297. [Google Scholar] [CrossRef] [PubMed]
- Duarte Campos, D.F.; Blaeser, A.; Korsten, A.; Neuss, S.; Jäkel, J.; Vogt, M.; Fischer, H. The stiffness and structure of three-dimensional printed hydrogels direct the differentiation of mesenchymal stromal cells toward adipogenic and osteogenic lineages. Tissue Eng. Part A 2015, 21, 740–756. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Stevens, L.; Thompson, B.C.; Gilmore, K.J.; Gorkin, R., 3rd; Stewart, E.M.; in het Panhuis, M.; Romero-Ortega, M.; Wallace, G.G. 3D printing of layered brain-like structures using peptide modified gellan gum substrates. Biomaterials 2015, 67, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-S.; Hong, J.M.; Jung, J.W.; Shim, J.-H.; Oh, J.-H.; Cho, D.-W. 3D printing of composite tissue with complex shape applied to ear regeneration. Biofabrication 2014, 6, 024103. [Google Scholar] [CrossRef]
- Cui, H.; Zhu, W.; Nowicki, M.; Zhou, X.; Khademhosseini, A.; Zhang, L.G. Hierarchical Fabrication of Engineered Vascularized Bone Biphasic Constructs via Dual 3D Bioprinting: Integrating Regional Bioactive Factors into Architectural Design. Adv. Healthc. Mater. 2016, 5, 2174–2181. [Google Scholar] [CrossRef]
- Cui, H.; Zhu, W.; Holmes, B.; Zhang, L.G. Biologically Inspired Smart Release System Based on 3D Bioprinted Perfused Scaffold for Vascularized Tissue Regeneration. Adv. Sci. 2016, 3, 1600058. [Google Scholar] [CrossRef]
- Kuo, C.K.; Ma, P.X. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: Part 1. Structure, gelation rate and mechanical properties. Biomaterials 2001, 22, 511–521. [Google Scholar] [CrossRef]
- Galis, Z.S.; Khatri, J.J. Matrix metalloproteinases in vascular remodeling and atherogenesis: The good, the bad, and the ugly. Circ. Res. 2002, 90, 251–262. [Google Scholar] [CrossRef]
- Nichol, J.W.; Koshy, S.T.; Bae, H.; Hwang, C.M.; Yamanlar, S.; Khademhosseini, A. Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials 2010, 31, 5536–5544. [Google Scholar] [CrossRef]
- Benton, J.A.; DeForest, C.A.; Vivekanandan, V.; Anseth, K.S. Photocrosslinking of gelatin macromers to synthesize porous hydrogels that promote valvular interstitial cell function. Tissue Eng. Part A 2009, 15, 3221–3230. [Google Scholar] [CrossRef]
- Ong, C.S.; Yesantharao, P.; Huang, C.Y.; Mattson, G.; Boktor, J.; Fukunishi, T.; Zhang, H.; Hibino, N. 3D bioprinting using stem cells. Pediatr. Res. 2018, 83, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Sawkins, M.J.; Mistry, P.; Brown, B.N.; Shakesheff, K.M.; Bonassar, L.J.; Yang, J. Cell and protein compatible 3D bioprinting of mechanically strong constructs for bone repair. Biofabrication 2015, 7, 035004. [Google Scholar] [CrossRef] [PubMed]
- Kuss, M.A.; Harms, R.; Wu, S.; Wang, Y.; Untrauer, J.B.; Carlson, M.A.; Duan, B. Short-term hypoxic preconditioning promotes prevascularization in 3D bioprinted bone constructs with stromal vascular fraction derived cells. RSC Adv. 2017, 7, 29312–29320. [Google Scholar] [CrossRef] [PubMed]
- Uccelli, A.; Moretta, L.; Pistoia, V. Mesenchymal stem cells in health and disease. Nat. Rev. Immunol. 2008, 8, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Tanabe, K.; Ohnuki, M.; Narita, M.; Ichisaka, T.; Tomoda, K.; Yamanaka, S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 2007, 131, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Vodyanik, M.A.; Smuga-Otto, K.; Antosiewicz-Bourget, J.; Frane, J.L.; Tian, S.; Nie, J.; Jonsdottir, G.A.; Ruotti, V.; Stewart, R.; et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 2007, 318, 1917–1920. [Google Scholar] [CrossRef]
- Sabapathy, V.; Kumar, S. hiPSC-derived iMSCs: NextGen MSCs as an advanced therapeutically active cell resource for regenerative medicine. J. Cell. Mol. Med. 2016, 20, 1571–1588. [Google Scholar] [CrossRef]
- Tricomi, B.J.; Dias, A.D.; Corr, D.T. Stem cell bioprinting for applications in regenerative medicine. Ann. N. Y. Acad. Sci. 2016, 1383, 115–124. [Google Scholar] [CrossRef]
- Ashammakhi, N.; Hasan, A.; Kaarela, O.; Byambaa, B.; Sheikhi, A.; Gaharwar, A.K.; Khademhosseini, A. Advancing Frontiers in Bone Bioprinting. Adv. Healthc. Mater. 2019, 8, 1801048. [Google Scholar] [CrossRef]
- Lee, J.; Sing, S.; Yeong, W. Bioprinting of Multimaterials with Computer-aided Design/Computer-aided Manufacturing. Int. J. Bioprint. 2020, 6, 65–73. [Google Scholar] [CrossRef]
- O’Brien, F.J. Biomaterials & scaffolds for tissue engineering. Mater. Today 2011, 14, 88–95. [Google Scholar] [CrossRef]
- Ashammakhi, N.; Ahadian, S.; Xu, C.; Montazerian, H.; Ko, H.; Nasiri, R.; Barros, N.; Khademhosseini, A. Bioinks and bioprinting technologies to make heterogeneous and biomimetic tissue constructs. Mater. Today Bio 2019, 1, 100008. [Google Scholar] [CrossRef] [PubMed]
- Hardin, J.O.; Ober, T.J.; Valentine, A.D.; Lewis, J.A. Microfluidic Printheads for Multimaterial 3D Printing of Viscoelastic Inks. Adv. Mater. 2015, 27, 3279–3284. [Google Scholar] [CrossRef] [PubMed]
- Shahabipour, F.; Ashammakhi, N.; Oskuee, R.K.; Bonakdar, S.; Hoffman, T.; Shokrgozar, M.A.; Khademhosseini, A. Key components of engineering vascularized 3-dimensional bioprinted bone constructs. Transl. Res. 2020, 216, 57–76. [Google Scholar] [CrossRef]
- Kolesky, D.B.; Truby, R.L.; Gladman, A.S.; Busbee, T.A.; Homan, K.A.; Lewis, J.A. 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv. Mater. 2014, 26, 3124–3130. [Google Scholar] [CrossRef]
- Wu, W.; DeConinck, A.; Lewis, J.A. Omnidirectional Printing of 3D Microvascular Networks. Adv. Mater. 2011, 23, H178–H183. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Shen, Y.-F.; Ho, C.-C.; Yu, J.; Wu, Y.-H.A.; Wang, K.; Shih, C.-T.; Shie, M.-Y. Osteogenic and angiogenic potentials of the cell-laden hydrogel/mussel-inspired calcium silicate complex hierarchical porous scaffold fabricated by 3D bioprinting. Mater. Sci. Eng. C 2018, 91, 679–687. [Google Scholar] [CrossRef]
- Chiesa, I.; De Maria, C.; Lapomarda, A.; Fortunato, G.M.; Montemurro, F.; Di Gesù, R.; Tuan, R.S.; Vozzi, G.; Gottardi, R. Endothelial cells support osteogenesis in an in vitro vascularized bone model developed by 3D bioprinting. Biofabrication 2020, 12, 025013. [Google Scholar] [CrossRef]
- Fan, W.; Crawford, R.; Xiao, Y. Enhancing in vivo vascularized bone formation by cobalt chloride-treated bone marrow stromal cells in a tissue engineered periosteum model. Biomaterials 2010, 31, 3580–3589. [Google Scholar] [CrossRef]
- Boyette, L.B.; Creasey, O.A.; Guzik, L.; Lozito, T.; Tuan, R.S. Human bone marrow-derived mesenchymal stem cells display enhanced clonogenicity but impaired differentiation with hypoxic preconditioning. Stem Cells Transl. Med. 2014, 3, 241–254. [Google Scholar] [CrossRef]
- Mamalis, A.A.; Cochran, D.L. The therapeutic potential of oxygen tension manipulation via hypoxia inducible factors and mimicking agents in guided bone regeneration. A review. Arch. Oral Biol. 2011, 56, 1466–1475. [Google Scholar] [CrossRef]
- Li, S.-D.; Huang, L. Non-viral is superior to viral gene delivery. J. Control. Release 2007, 123, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Cunniffe, G.M.; Gonzalez-Fernandez, T.; Daly, A.; Sathy, B.N.; Jeon, O.; Alsberg, E.; Kelly, D.J. Three-Dimensional Bioprinting of Polycaprolactone Reinforced Gene Activated Bioinks for Bone Tissue Engineering. Tissue Eng. Part A 2017, 23, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Norotte, C.; Marga, F.S.; Niklason, L.E.; Forgacs, G. Scaffold-free vascular tissue engineering using bioprinting. Biomaterials 2009, 30, 5910–5917. [Google Scholar] [CrossRef] [PubMed]
- Phamduy, T.B.; Raof, N.A.; Schiele, N.R.; Yan, Z.; Corr, D.T.; Huang, Y.; Xie, Y.; Chrisey, D.B. Laser direct-write of single microbeads into spatially-ordered patterns. Biofabrication 2012, 4, 025006. [Google Scholar] [CrossRef][Green Version]
- Tan, Y.; Richards, D.J.; Trusk, T.C.; Visconti, R.P.; Yost, M.J.; Kindy, M.S.; Drake, C.J.; Argraves, W.S.; Markwald, R.R.; Mei, Y. 3D printing facilitated scaffold-free tissue unit fabrication. Biofabrication 2014, 6, 024111. [Google Scholar] [CrossRef]
- Anada, T.; Pan, C.-C.; Stahl, A.M.; Mori, S.; Fukuda, J.; Suzuki, O.; Yang, Y. Vascularized bone-mimetic hydrogel constructs by 3D bioprinting to promote osteogenesis and angiogenesis. Int. J. Mol. Sci. 2019, 20, 1096. [Google Scholar] [CrossRef]
- Bhise, N.S.; Shmueli, R.B.; Sunshine, J.C.; Tzeng, S.Y.; Green, J.J. Drug delivery strategies for therapeutic angiogenesis and antiangiogenesis. Expert Opin. Drug Deliv. 2011, 8, 485–504. [Google Scholar] [CrossRef]
- Ferrara, N.; Gerber, H.-P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef]
- Kim, S.; Kang, Y.; Krueger, C.A.; Sen, M.; Holcomb, J.B.; Chen, D.; Wenke, J.C.; Yang, Y. Sequential delivery of BMP-2 and IGF-1 using a chitosan gel with gelatin microspheres enhances early osteoblastic differentiation. Acta Biomater. 2012, 8, 1768–1777. [Google Scholar] [CrossRef]
- Devraj, G.; Beerlage, C.; Brüne, B.; Kempf, V.A.J. Hypoxia and HIF-1 activation in bacterial infections. Microbes Infect. 2017, 19, 144–156. [Google Scholar] [CrossRef]
- Ribatti, D.; Tamma, R. Hematopoietic growth factors and tumor angiogenesis. Cancer Lett. 2019, 440–441, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Schmidmaier, G.; Schwabe, P.; Strobel, C.; Wildemann, B. Carrier systems and application of growth factors in orthopaedics. Injury 2008, 39, S37–S43. [Google Scholar] [CrossRef]
- Bessa, P.C.; Casal, M.; Reis, R.L. Bone morphogenetic proteins in tissue engineering: The road from laboratory to clinic, part II (BMP delivery). J. Tissue Eng. Regen. Med. 2008, 2, 81–96. [Google Scholar] [CrossRef]
- Ritz, U.; Gerke, R.; Götz, H.; Stein, S.; Rommens, P.M. A New Bone Substitute Developed from 3D-Prints of Polylactide (PLA) Loaded with Collagen I: An In Vitro Study. Int. J. Mol. Sci. 2017, 18. [Google Scholar] [CrossRef] [PubMed]
- García, J.R.; García, A.J. Biomaterial-mediated strategies targeting vascularization for bone repair. Drug Deliv. Transl. Res. 2016, 6, 77–95. [Google Scholar] [CrossRef]
- Chu, H.; Wang, Y. Therapeutic angiogenesis: Controlled delivery of angiogenic factors. Ther. Deliv. 2012, 3, 693–714. [Google Scholar] [CrossRef]
- Tao, Z.; Chen, B.; Tan, X.; Zhao, Y.; Wang, L.; Zhu, T.; Cao, K.; Yang, Z.; Kan, Y.W.; Su, H. Coexpression of VEGF and angiopoietin-1 promotes angiogenesis and cardiomyocyte proliferation reduces apoptosis in porcine myocardial infarction (MI) heart. Proc. Natl. Acad. Sci. USA 2011, 108, 2064–2069. [Google Scholar] [CrossRef]
- Fiedler, J.; Röderer, G.; Günther, K.-P.; Brenner, R.E. BMP-2, BMP-4, and PDGF-bb stimulate chemotactic migration of primary human mesenchymal progenitor cells. J. Cell. Biochem. 2002, 87, 305–312. [Google Scholar] [CrossRef]
- Eppler, S.M.; Combs, D.L.; Henry, T.D.; Lopez, J.J.; Ellis, S.G.; Yi, J.-H.; Annex, B.H.; McCluskey, E.R.; Zioncheck, T.F. A target-mediated model to describe the pharmacokinetics and hemodynamic effects of recombinant human vascular endothelial growth factor in humans. Clin. Pharmacol. Ther. 2002, 72, 20–32. [Google Scholar] [CrossRef]
- Kempen, D.H.R.; Lu, L.; Heijink, A.; Hefferan, T.E.; Creemers, L.B.; Maran, A.; Yaszemski, M.J.; Dhert, W.J.A. Effect of local sequential VEGF and BMP-2 delivery on ectopic and orthotopic bone regeneration. Biomaterials 2009, 30, 2816–2825. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.N.; Kasper, F.K.; Mikos, A.G. Strategies for controlled delivery of growth factors and cells for bone regeneration. Adv. Drug Deliv. Rev. 2012, 64, 1292–1309. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.-M.; Zhang, M.; Wu, Z.-F. Toward delivery of multiple growth factors in tissue engineering. Biomaterials 2010, 31, 6279–6308. [Google Scholar] [CrossRef] [PubMed]
- Kearney, C.J.; Mooney, D.J. Macroscale delivery systems for molecular and cellular payloads. Nat. Mater. 2013, 12, 1004–1017. [Google Scholar] [CrossRef]
- Poldervaart, M.T.; Gremmels, H.; van Deventer, K.; Fledderus, J.O.; Oner, F.C.; Verhaar, M.C.; Dhert, W.J.A.; Alblas, J. Prolonged presence of VEGF promotes vascularization in 3D bioprinted scaffolds with defined architecture. J. Control. Release 2014, 184, 58–66. [Google Scholar] [CrossRef]
- Gerry, C.J.; Schreiber, S.L. Unifying principles of bifunctional, proximity-inducing small molecules. Nat. Chem. Biol. 2020, 16, 369–378. [Google Scholar] [CrossRef]
- Rodriguez-Miguelez, P.; Lee, N.; Tucker, M.A.; Csányi, G.; McKie, K.T.; Forseen, C.; Harris, R.A. Sildenafil improves vascular endothelial function in patients with cystic fibrosis. Am. J. Physiology-Heart Circ. Physiol. 2018, 315, H1486–H1494. [Google Scholar] [CrossRef]
- Saghiri, M.A.; Orangi, J.; Asatourian, A.; Sorenson, C.M.; Sheibani, N. Functional role of inorganic trace elements in angiogenesis part III: (Ti, Li, Ce, As, Hg, Va, Nb and Pb). Crit. Rev. Oncol. Hematol. 2016, 98, 290–301. [Google Scholar] [CrossRef]
- Santulli, G.; Ciccarelli, M.; Palumbo, G.; Campanile, A.; Galasso, G.; Ziaco, B.; Altobelli, G.G.; Cimini, V.; Piscione, F.; D’Andrea, L.D.; et al. In vivo properties of the proangiogenic peptide QK. J. Transl. Med. 2009, 7, 41. [Google Scholar] [CrossRef]
- Wang, X.; Horii, A.; Zhang, S. Designer functionalized self-assembling peptide nanofiber scaffolds for growth, migration, and tubulogenesis of human umbilical vein endothelial cells. Soft Matter 2008, 4, 2388–2395. [Google Scholar] [CrossRef]
- Lu, J.; Guan, F.; Cui, F.; Sun, X.; Zhao, L.; Wang, Y.; Wang, X. Enhanced angiogenesis by the hyaluronic acid hydrogels immobilized with a VEGF mimetic peptide in a traumatic brain injury model in rats. Regen. Biomater. 2019, 6, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Jose, S.; Hughbanks, M.L.; Binder, B.Y.K.; Ingavle, G.C.; Leach, J.K. Enhanced trophic factor secretion by mesenchymal stem/stromal cells with Glycine-Histidine-Lysine (GHK)-modified alginate hydrogels. Acta Biomater. 2014, 10, 1955–1964. [Google Scholar] [CrossRef] [PubMed]
- Klontzas, M.E.; Reakasame, S.; Silva, R.; Morais, J.C.F.; Vernardis, S.; MacFarlane, R.J.; Heliotis, M.; Tsiridis, E.; Panoskaltsis, N.; Boccaccini, A.R.; et al. Oxidized alginate hydrogels with the GHK peptide enhance cord blood mesenchymal stem cell osteogenesis: A paradigm for metabolomics-based evaluation of biomaterial design. Acta Biomater. 2019, 88, 224–240. [Google Scholar] [CrossRef] [PubMed]
- Massa, S.; Sakr, M.A.; Seo, J.; Bandaru, P.; Arneri, A.; Bersini, S.; Zare-Eelanjegh, E.; Jalilian, E.; Cha, B.-H.; Antona, S.; et al. Bioprinted 3D vascularized tissue model for drug toxicity analysis. Biomicrofluidics 2017, 11, 044109. [Google Scholar] [CrossRef]
- Bhise, N.S.; Manoharan, V.; Massa, S.; Tamayol, A.; Ghaderi, M.; Miscuglio, M.; Lang, Q.; Shrike Zhang, Y.; Shin, S.R.; Calzone, G.; et al. A liver-on-a-chip platform with bioprinted hepatic spheroids. Biofabrication 2016, 8, 014101. [Google Scholar] [CrossRef]
- Zhou, X.; Zhu, W.; Nowicki, M.; Miao, S.; Cui, H.; Holmes, B.; Glazer, R.I.; Zhang, L.G. 3D Bioprinting a Cell-Laden Bone Matrix for Breast Cancer Metastasis Study. ACS Appl. Mater. Interfaces 2016, 8, 30017–30026. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).