Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models
Abstract
1. Introduction
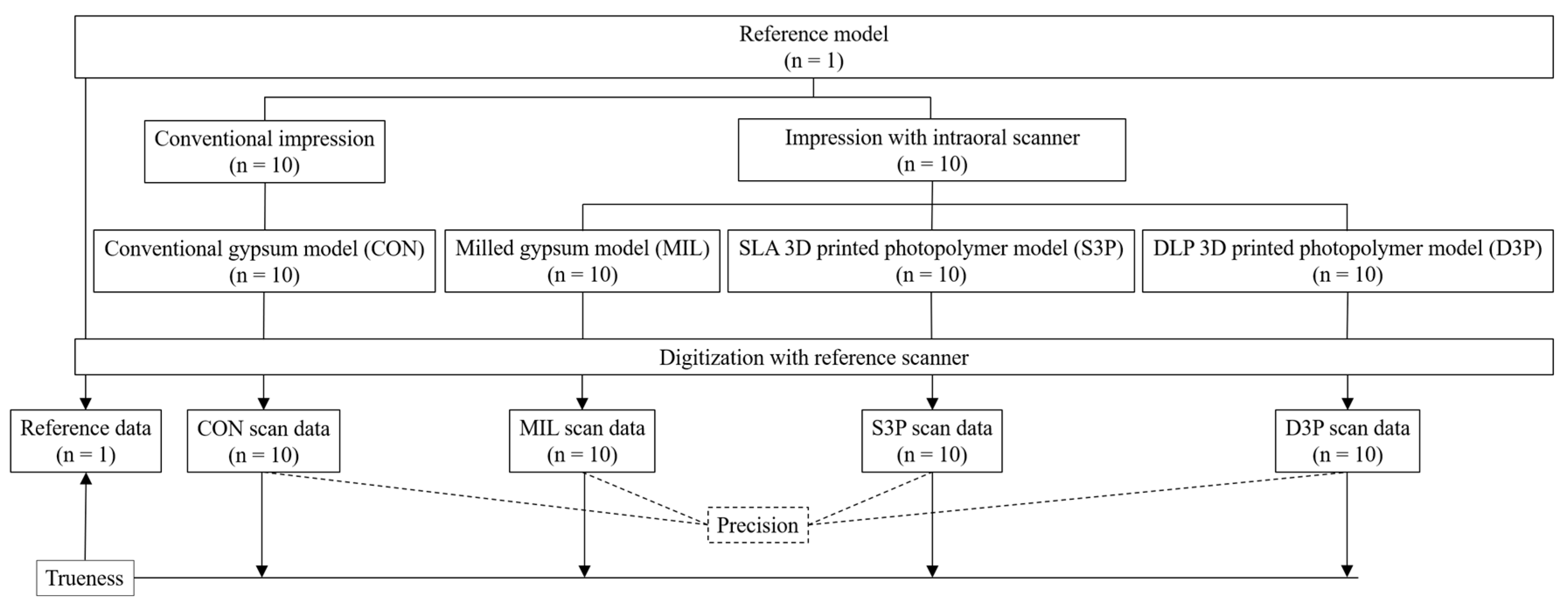
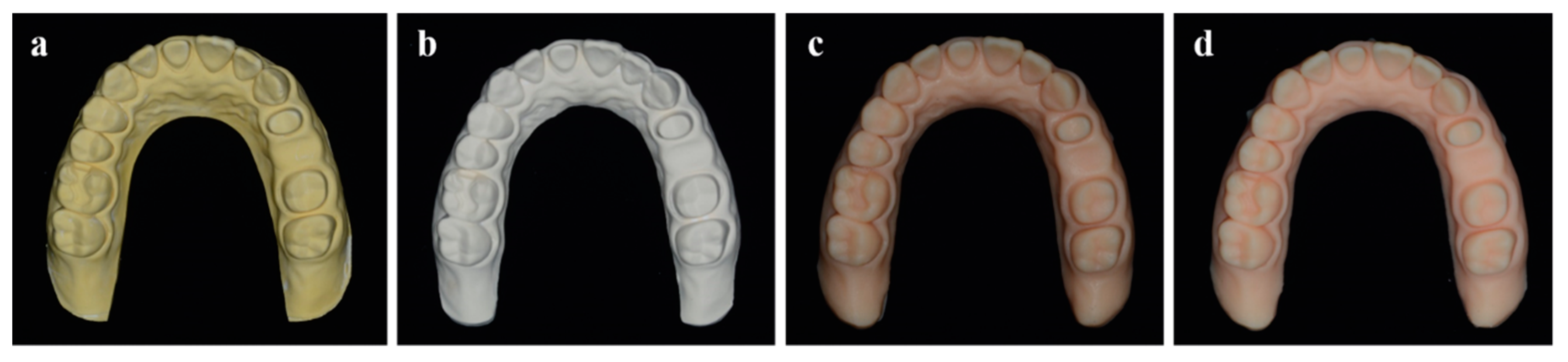
2. Materials and Methods
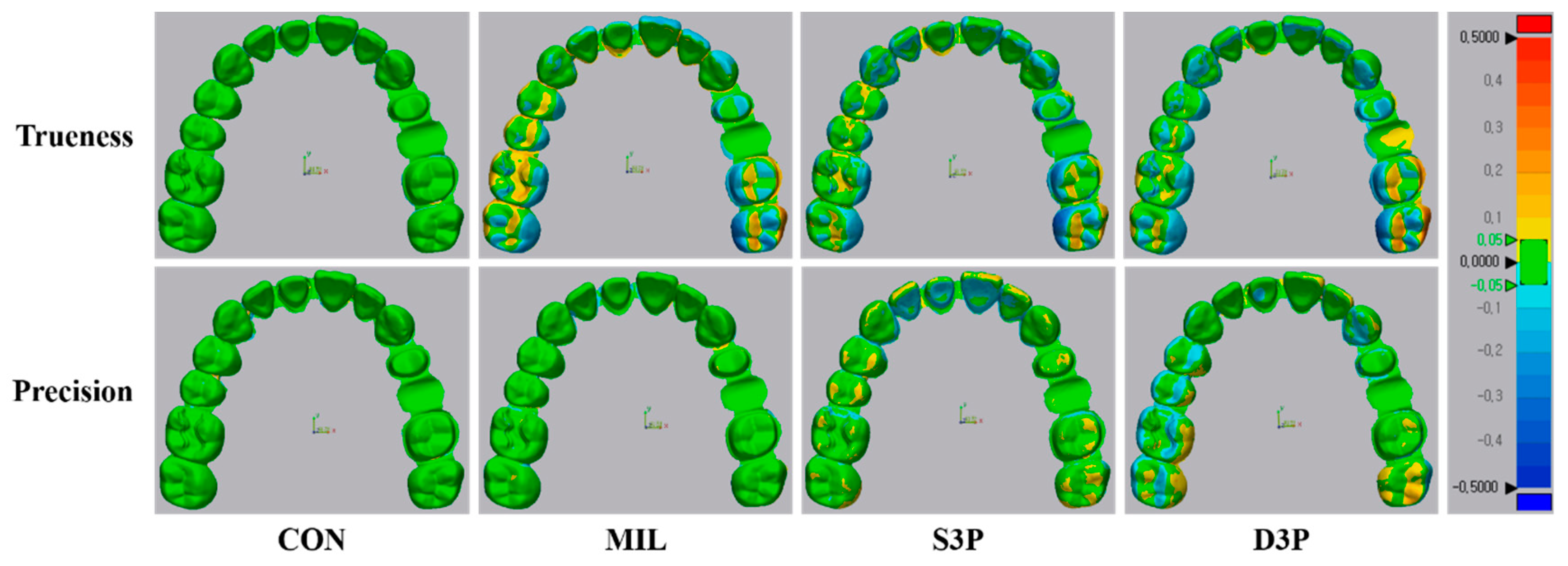
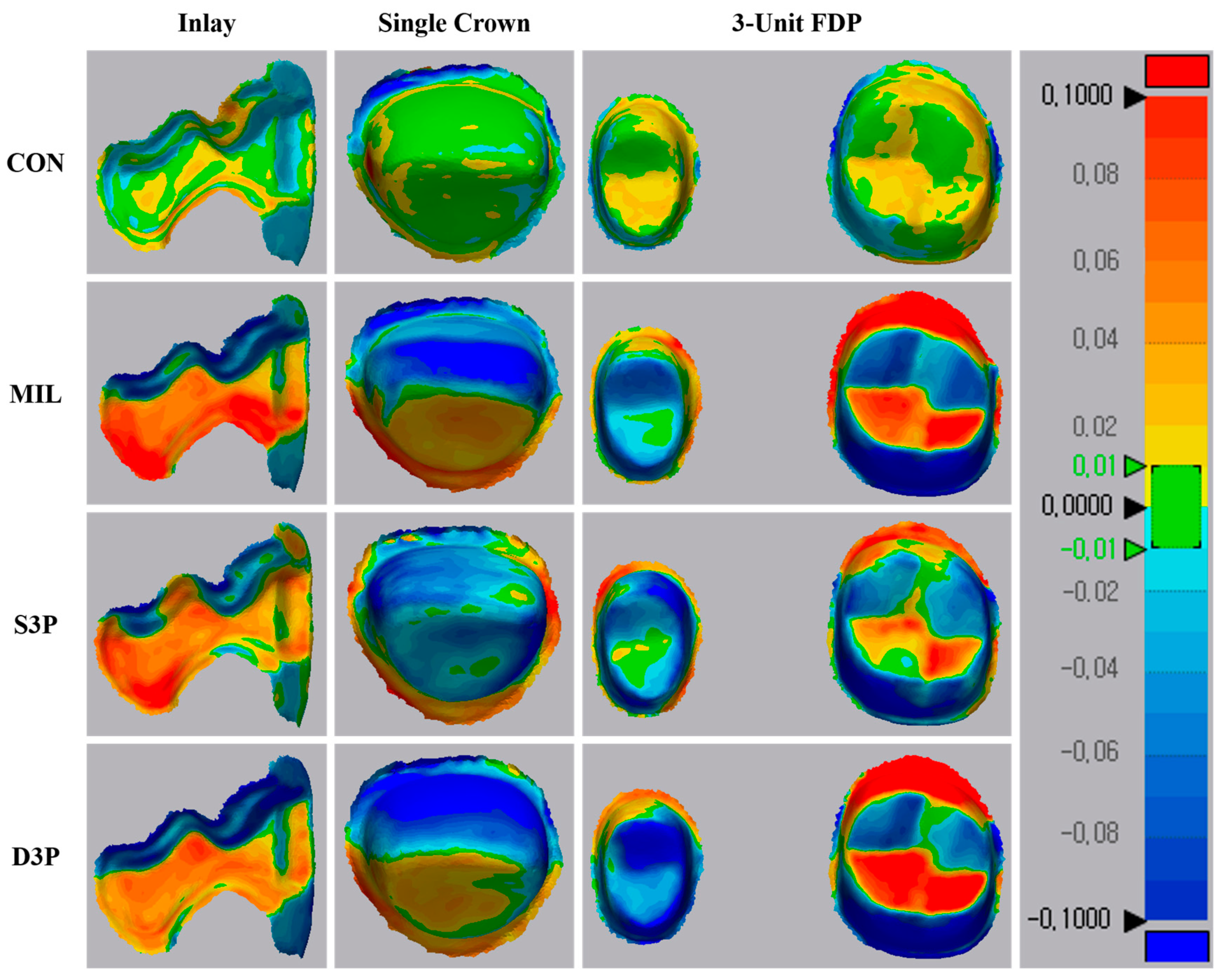
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Persson, A.S.; Andersson, M.; Odén, A.; Sandborgh-Englund, G. Computer aided analysis of digitized dental stone replicas by dental CAD/CAM technology. Dent. Mater. 2008, 24, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Clancy, J.M.; Scandrett, F.R.; Ettinger, R.L. Long-term dimensional stability of three current elastomers. J. Oral. Rehabil. 1983, 10, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. The state of fixed prosthodontic impressions: Room for improvement. J. Am. Dent. Assoc. 2005, 136, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, O.; Schmidt, M.; Goebel, R.; Kuepper, H. Qualitative and quantitative three-dimensional accuracy of a single tooth captured by elastomeric impression materials: An in vitro study. J. Prosthet. Dent. 2012, 108, 165–172. [Google Scholar] [CrossRef]
- Christensen, G.J. Impressions are changing: Deciding on conventional, digital or digital plus in-office milling. J. Am. Dent. Assoc. 2009, 140, 1301–1304. [Google Scholar] [CrossRef] [PubMed]
- Patzelt, S.B.; Bishti, S.; Stampf, S.; Att, W. Accuracy of computer-aided design/computer-aided manufacturing-generated dental casts based on intraoral scanner data. J. Am. Dent. Assoc. 2014, 145, 1133–1140. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, C.J.; Gallucci, G.O.; Doukoudakis, A.; Weber, H.P.; Chronopoulos, V. Accuracy of implant impressions for partially and completely edentulous patients: A systematic review. Int. J. Oral. Maxillofac. Implants 2014, 29, 836–845. [Google Scholar] [CrossRef]
- Pani, S.C.; Hedge, A.M. Impressions in cleft lip and palate—A novel two stage technique. J. Clin. Pediatr. Dent. 2008, 33, 93–96. [Google Scholar] [CrossRef]
- Sim, J.Y.; Jang, Y.; Kim, W.C.; Kim, H.Y.; Lee, D.H.; Kim, J.H. Comparing the accuracy (trueness and precision) of models of fixed dental prostheses fabricated by digital and conventional workflows. J. Prosthodont. Res. 2019, 63, 25–30. [Google Scholar] [CrossRef]
- Park, M.E.; Shin, S.Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, e1–e861. [Google Scholar] [CrossRef]
- Lin, W.S.; Harris, B.T.; Zandinejad, A.; Morton, D. Use of digital data acquisition and CAD/CAM technology for the fabrication of a fixed complete dental prosthesis on dental implants. J. Prosthet. Dent. 2014, 111, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Braian, M.; Jimbo, R.; Wennerberg, A. Production tolerance of additive manufactured polymeric objects for clinical applications. Dent. Mater. 2016, 32, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Krahenbuhl, J.T.; Cho, S.H.; Irelan, J.; Bansal, N.K. Accuracy and precision of occlusal contacts of stereolithographic casts mounted by digital interocclusal registrations. J. Prosthet. Dent. 2016, 116, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. Trueness of four different milling procedures used in dental CAD/CAM systems. Clin. Oral. Investig. 2017, 21, 551–558. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. Accuracy of complete-arch dental impressions: A new method of measuring trueness and precision. J. Prosthet. Dent. 2013, 109, 121–128. [Google Scholar] [CrossRef]
- Ziegler, M. Digital impression taking with reproducibly high precision. Int. J. Comput. Dent. 2009, 12, 159–163. [Google Scholar]
- Camardella, L.T.; de Vasconcellos Vilella, O.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lee, S.H.; Cho, S.K.; Jeong, C.M.; Jeon, Y.C.; Yun, M.J.; Huh, J.B. Comparison of the accuracy of digitally fabricated polyurethane model and conventional gypsum model. J. Adv. Prosthodont. 2014, 6, 1–7. [Google Scholar] [CrossRef][Green Version]
- Jeong, Y.G.; Lee, W.S.; Lee, K.B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Al-Imam, H.; Gram, M.; Benetti, A.R.; Gotfredsen, K. Accuracy of stereolithography additive casts used in a digital workflow. J. Prosthet. Dent. 2018, 119, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Koch, G.K.; Gallucci, G.O.; Lee, S.J. Accuracy in the digital workflow: From data acquisition to the digitally milled cast. J. Prosthet. Dent. 2016, 115, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Schaefer, O.; Thompson, G.A.; Guentsch, A. Comparison of accuracy and reproducibility of casts made by digital and conventional methods. J. Prosthet. Dent. 2015, 113, 310–315. [Google Scholar] [CrossRef]
- Jin, S.J.; Kim, D.Y.; Kim, J.H.; Kim, W.C. Accuracy of Dental Replica Models Using Photopolymer Materials in Additive Manufacturing: In Vitro Three-Dimensional Evaluation. J. Prosthodont. 2019, 28, e557–e562. [Google Scholar] [CrossRef]
- White, A.J.; Fallis, D.W.; Vandewalle, K.S. Analysis of intra-arch and interarch measurements from digital models with 2 impression materials and a modeling process based on cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2010, 137, e1–e456. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Al Mortadi, N.; Eggbeer, D.; Lewis, J.; Williams, R.J. CAD/CAM/AM applications in the manufacture of dental appliances. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 727–733. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Mehl, A.; Ender, A.; Mörmann, W.; Attin, T. Accuracy testing of a new intraoral 3D camera. Int. J. Comput. Dent. 2009, 12, 11–28. [Google Scholar]
- Ender, A.; Mehl, A. Full arch scans: Conventional versus digital impressions—An in-vitro study. Int. J. Comput. Dent. 2011, 14, 11–21. [Google Scholar] [PubMed]
- Brosky, M.E.; Major, R.J.; DeLong, R.; Hodges, J.S. Evaluation of dental arch reproduction using three-dimensional optical digitization. J. Prosthet. Dent. 2003, 90, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Stimmelmayr, M.; Erdelt, K.; Güth, J.F.; Happe, A.; Beuer, F. Evaluation of impression accuracy for a four-implant mandibular model—A digital approach. Clin. Oral. Investig. 2012, 16, 1137–1142. [Google Scholar] [CrossRef] [PubMed]
- Caputi, S.; Varvara, G. Dimensional accuracy of resultant casts made by a monophase, one-step and two-step, and a novel two-step putty/light-body impression technique: An in vitro study. J. Prosthet. Dent. 2008, 99, 274–281. [Google Scholar] [CrossRef]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral. Implants Res. 2015, 26, 715–719. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. In-vitro evaluation of the accuracy of conventional and digital methods of obtaining full-arch dental impressions. Quintessence Int. 2015, 46, 9–17. [Google Scholar]
- Zhang, Z.C.; Li, P.L.; Chu, F.T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Luthardt, R.G.; Kühmstedt, P.; Walter, M.H. A new method for the computer-aided evaluation of three-dimensional changes in gypsum materials. Dent. Mater. 2003, 19, 19–24. [Google Scholar] [CrossRef]
- Pham, D.T.; Ji, C. Design for stereolithography. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2000, 214, 635–640. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- Lin, M.; Firoozi, N.; Tsai, C.T.; Wallace, M.B.; Kang, Y. 3D-printed flexible polymer stents for potential applications in inoperable esophageal malignancies. Acta Biomater. 2019, 83, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Thongthammachat, S.; Moore, B.K.; Barco, M.T., 2nd; Hovijitra, S.; Brown, D.T.; Andres, C.J. Dimensional accuracy of dental casts: Influence of tray material, impression material, and time. J. Prosthodont. 2002, 11, 98–108. [Google Scholar] [CrossRef] [PubMed]
- González de Villaumbrosia, P.; Martínez-Rus, F.; García-Orejas, A.; Salido, M.P.; Pradíes, G. In vitro comparison of the accuracy (trueness and precision) of six extraoral dental scanners with different scanning technologies. J. Prosthet. Dent. 2016, 116, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Treesh, J.C.; Liacouras, P.C.; Taft, R.M.; Brooks, D.I.; Raiciulescu, S.; Ellert, D.O.; Grant, G.T.; Ye, L. Complete-arch accuracy of intraoral scanners. J. Prosthet. Dent. 2018, 120, 382–388. [Google Scholar] [CrossRef]
- Güth, J.F.; Keul, C.; Stimmelmayr, M.; Beuer, F.; Edelhoff, D. Accuracy of digital models obtained by direct and indirect data capturing. Clin. Oral. Investig. 2013, 17, 1201–1208. [Google Scholar] [CrossRef]
- Schmitz, T.L.; Ziegert, J.C.; Canning, J.S.; Zapata, R. Case study: A comparison of error sources in high-speed milling. Precision Eng. 2008, 32, 126–133. [Google Scholar] [CrossRef]
- De Souz a, A.F.; Diniz, A.E.; Rodrigues, A.R.; Coelho, R.T. Investigating the cutting phenomena in free-form milling using a ball-end cutting tool for die and mold manufacturing. Int. J. Adv. Manuf. Technol. 2014, 71, 1565–1577. [Google Scholar] [CrossRef]
- Dikova, T.D.; Dzhendov, D.A.; Ivanov, D.; Bliznakova, K. Dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printing processes. Arch. Mater. Sci. Eng. 2018, 94, 65–75. [Google Scholar] [CrossRef]
- Kim, R.J.; Park, J.M.; Shim, J.S. Accuracy of 9 intraoral scanners for complete-arch image acquisition: A qualitative and quantitative evaluation. J. Prosthet. Dent. 2018, 120, 895–903. [Google Scholar] [CrossRef]
| Group | Root Mean Square (RMS) (µm) | |||
|---|---|---|---|---|
| Trueness | Precision | |||
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| CON | 27.9 ± 2.7a | 26.0–29.8 | 20.0 ± 3.1a | 19.1–21.0 |
| MIL | 94.0 ± 11.5b | 85.8–102.3 | 37.8 ± 7.0b | 35.7–39.9 |
| S3P | 85.2 ± 13.1b | 75.9–94.6 | 49.6 ± 12.1c | 45.9–53.2 |
| D3P | 105.5 ± 22.5b | 89.4–121.6 | 52.8 ± 17.5c | 47.6–58.1 |
| p | <0.001 | <0.001 | ||
| Group | Root Mean Square (RMS) (µm) | |||
|---|---|---|---|---|
| Inlay | Single Crown | 3-Unit FDP | p | |
| Mean ± SD (95% CI) | Mean ± SD (95% CI) | Mean ± SD (95% CI) | ||
| CON | 20.9 ± 1.4aA (19.9–21.9) | 30.5 ± 8.4aB (24.5–36.5) | 22.2 ± 2.3aA (20.6–23.8) | 0.005 |
| MIL | 72.8 ± 12.4bA (63.9–81.7) | 65.2 ± 6.6bB (60.5–69.9) | 95.8 ± 29.1bcA (74.9–116.6) | 0.007 |
| S3P | 60.7 ± 12.1bA (52.1–69.4) | 62.0 ± 10.6bA (53.0–68.0) | 81.5 ± 14.1bB (71.4–91.6) | 0.004 |
| D3P | 66.9 ± 20.9bA (51.9–81.8) | 84.3 ± 22.5cB (68.2–100.4) | 117.3 ± 38.5cC (89.8–144.8) | 0.001 |
| p | <0.001 | <0.001 | <0.001 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-W.; Ahn, J.-J.; Son, K.; Huh, J.-B. Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models. Materials 2019, 12, 3499. https://doi.org/10.3390/ma12213499
Choi J-W, Ahn J-J, Son K, Huh J-B. Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models. Materials. 2019; 12(21):3499. https://doi.org/10.3390/ma12213499
Chicago/Turabian StyleChoi, Jae-Won, Jong-Ju Ahn, Keunbada Son, and Jung-Bo Huh. 2019. "Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models" Materials 12, no. 21: 3499. https://doi.org/10.3390/ma12213499
APA StyleChoi, J.-W., Ahn, J.-J., Son, K., & Huh, J.-B. (2019). Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models. Materials, 12(21), 3499. https://doi.org/10.3390/ma12213499






