Influence of Masks Protecting against SARS-CoV-2 on Thermal Comfort
Abstract
1. Introduction
- Carrying out hand hygiene before putting on the mask,
- Correctly covering the mouth and nose when putting the mask on, so that there are no gaps between the mask and the face,
- Avoiding touching the mask and, if it happens, washing hands or disinfecting them,
- Removing the mask using the appropriate technique,
- Replacement of the mask with a new one as soon as it becomes wet,
- Not re-using the disposable mask after use,
- Throwing the used mask into a closed container, and in the case of material masks, handling it in such a way as not to contaminate other objects,
- Sanitizing hands again after removing the mask [3].
2. Materials and Methods
- 1
- Dressed manikin without face mask,
- 2
- Dressed manikin with a mask of the FFP2 type,
- 3
- Dressed manikin with a cotton mask,
- 4
- Dressed manikin with a medical mask,
- 5
- Dressed manikin with a PM2.5 mask,
- 6
- Dressed manikin with half-face protective shield plastic,
- 7
- Dressed manikin with full-face protective shield plastic.
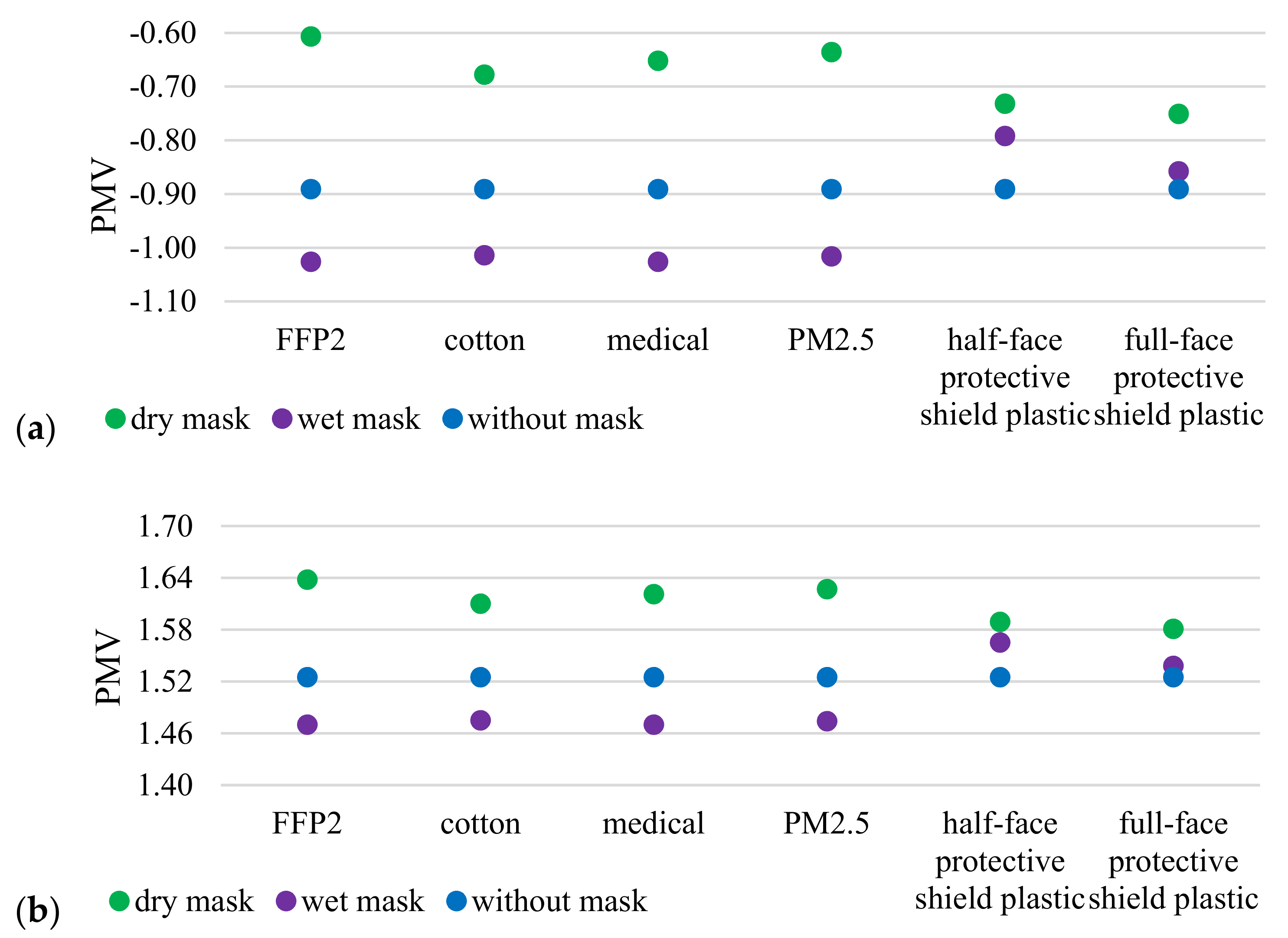
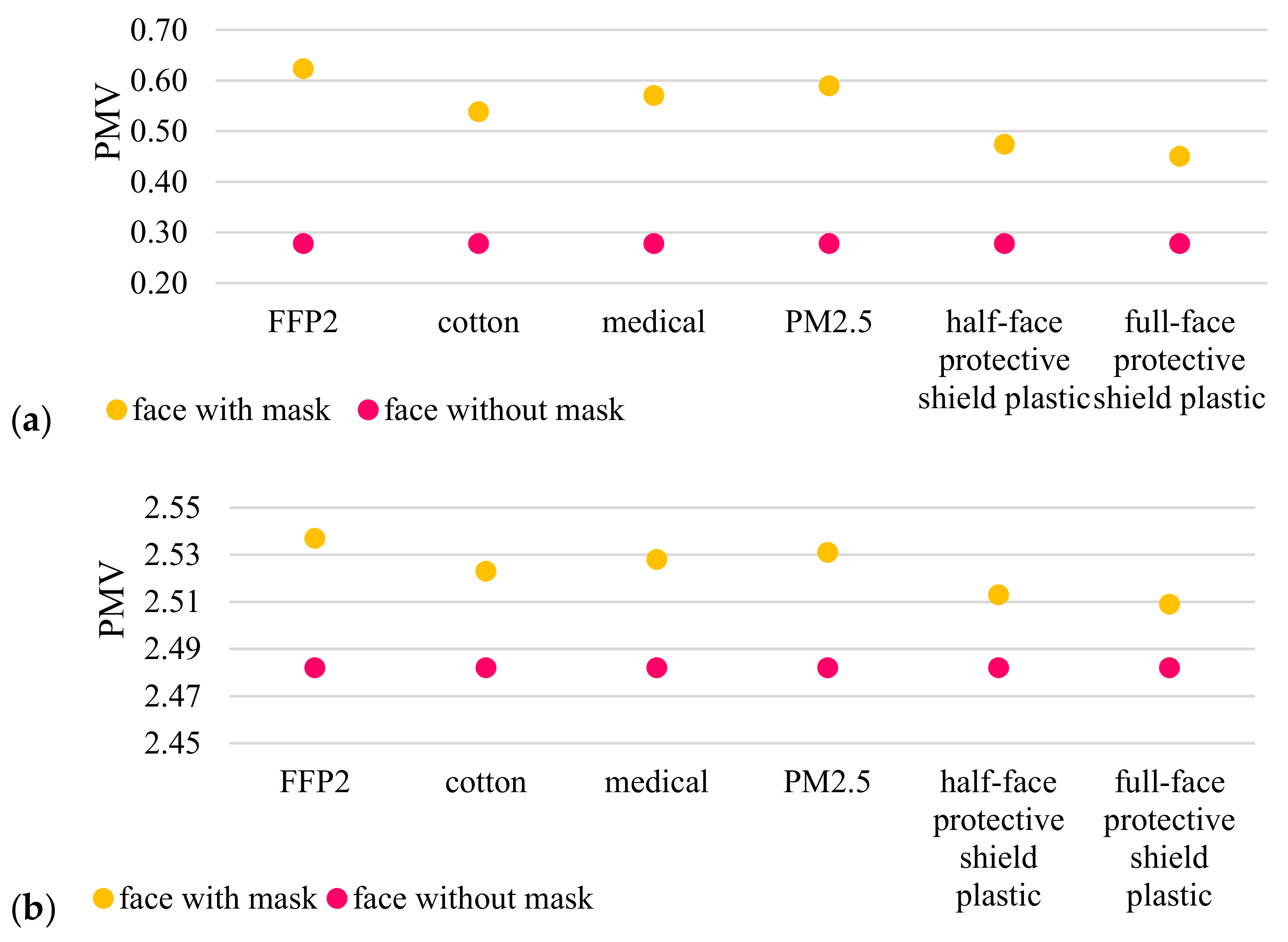
3. Results and Discussion
4. Conclusions
- Greater general discomfort at higher temperature with a dry mask on face compared to no mask;
- Greater general comfort at a lower temperature with a dry mask on face compared to no mask;
- Greater general discomfort at a lower temperature with a wet mask on face compared to no mask;
- Less general discomfort at higher temperatures with a wet mask on face compared to no mask;
- Slight difference in the feeling of general thermal comfort when using the following masks: FFP2, cotton, medical and PM2.5;
- Greater thermal comfort at a lower temperature when using half-face protective shield plastic and full-face protective shield plastic regardless of their wetting;
- Greater discomfort at higher temperatures when using half-face protective shield plastic and full-face protective shield plastic regardless of their wetting;
- At a lower temperature, greater local comfort within the face when the mask is on the face than without it;
- At a higher temperature, local discomfort in the face when the mask is on the face is greater than without it.
- At lower temperatures, more heat flux is needed;
- The use of dry masks requires less heat flux than the use of wet masks;
- The use of dry masks requires less heat flux than no masks;
- The use of wet masks requires more heat flux than no masks.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Felter, C.; Bussemaker, N. Which Countries Are Requiring Face Masks? Council on Foreign Relations: New York, NY, USA, 2020. [Google Scholar]
- Rizki, S.A.; Kurniawan, A. Efficacy of cloth mask in redusing COVID-19 transmission: A literaturę review. Kesmas J. Kesehat. Masy. Nas. Natl. Public Health J. 2020, 1, 43–48. [Google Scholar] [CrossRef]
- World Health Organization. Advice on the Use of Masks in the Community, during Home Care, and in Health Care Settings in the Context of the Novel Coronavirus (2019-nCov) Outbreak: Interim Guidance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Guy, G.P., Jr.; Lee, F.C.; Sunshine, G.; McCord, R.; Howard-Williams, M.; Kompaniyets, L.; Dunphy, C.; Gakh, M.; Weber, R.; Sauber-Schatz, E.; et al. Association of state-issued mask mandates and allowing on-premises restaurant dining with county-level COVID-19 case and death growth rates—United States, 1 March–31 December 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 350–354. [Google Scholar] [CrossRef]
- Bo, Y.; Guo, C.; Lin, C.; Zeng, Y.; Li, H.B.; Zhang, Y.; Hossain, S.; Chan, J.W.; Yeung, D.W.; Kwok, K.O.; et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021, 102, 247–253. [Google Scholar] [CrossRef]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Liu, Y.; Li, M.; Qian, X.; Dai, S.Y. Mask or no mask for COVID-19: A public health and market study. PLoS ONE 2020, 15, e0237691. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Morawska, L.; Cao, J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ. Int. 2020, 139, 105730. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Lloyd-Smith, J.O.; De Wit, E.; Munster, V.J.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.; Leung, D.Y.; Ho, T. Evidence of Airborne Transmission of the Severe Acute Respiratory Syndrome Virus. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- El-Atab, N.; Qaiser, N.; Badghaish, H.S.; Shaikh, S.F.; Hussain, M.M. Flexible Nanoporous Template for the Design and Development of Reusable Anti-COVID-19 Hydrophobic Face Masks. ACS Nano 2020, 14, 7659–7665. [Google Scholar] [CrossRef] [PubMed]
- Do Surgical Masks Protect Workers? OSH Answers Fact Sheets. Canadian Centre for Occupational Health and Safety. Available online: https://www.ccohs.ca/oshanswers/prevention/respiratory_protection.html (accessed on 15 March 2021).
- Yassi, A.; Bryce, E. Protecting the Faces of Health Care Workers: Knowledge Gaps and Research Priorities for Effective Protection against Occupationally—Acquired Respiratory Infectious Diseases. Final Report; Occupational Health and Safety Agency for Healthcare in BC: Vancouver, BC, Canada, 2004. [Google Scholar]
- Lee, S.-A.; Hwang, D.-C.; Li, H.-Y.; Tsai, C.-F.; Chen, C.-W.; Chen, J.-K. Particle Size-Selective Assessment of Protection of European Standard FFP Respirators and Surgical Masks against Particles-Tested with Human Subjects. J. Healthc. Eng. 2016, 2016, 8572493. [Google Scholar] [CrossRef]
- Grinshpun, S.A.; Haruta, H.; Eninger, R.M.; Reponen, T.; McKay, R.T.; Lee, S.-A. Performance of an N95 Filtering Facepiece Particulate Respirator and a Surgical Mask During Human Breathing: Two Pathways for Particle Penetration. J. Occup. Environ. Hyg. 2009, 6, 593–603. [Google Scholar] [CrossRef]
- De Araújo, E.S.A.; Amaral, F.M.B.H.; Park, D.; Cameira, A.P.C.; da Cunha, M.A.M.; Karl, E.G.; Henderson, S.J. Teach, and teach and teach: Does the average citizen use masks correctly during daily activities? Results from an observational study with more than 12,000 participants. medRxiv 2020. preprint. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; Amagasa, S.; et al. Incorrect Use of Face Masks during the Current COVID-19 Pandemic among the General Public in Japan. Int. J. Environ. Res. Public Health 2020, 17, 6484. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Shiu, E.Y.C.; Gao, H.; Wong, J.Y.; Fong, M.W.; Ryu, S.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures. Emerg. Infect. Dis. 2020, 26, 967–975. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Seale, H.; Dung, T.C.; Hien, N.T.; Nga, P.T.; Chughtai, A.A.; Rahman, B.; Dwyer, D.E.; Wang, Q. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open 2015, 5, e006577. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, J. The importance of wearing masks in curtailing the COVID-19 pandemic. J. Fam. Med. Prim. Care 2020, 9, 2606–2607. [Google Scholar] [CrossRef]
- Ong, J.J.; Bharatendu, C.; Goh, Y.; Tang, J.Z.; Sooi, K.W.; Tan, Y.L.; Tan, B.Y.; Teoh, H.; Ong, S.T.; Allen, D.M.; et al. Headaches Associated with Personal Protective Equipment–A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache J. Head Face Pain 2020, 60, 864–877. [Google Scholar] [CrossRef]
- Jacobs, J.L.; Ohde, S.; Takahashi, O.; Tokuda, Y.; Omata, F.; Fukui, T. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial. Am. J. Infect. Control 2009, 37, 417–419. [Google Scholar] [CrossRef]
- Beder, A.; Büyükkoçak, Ü.; Sabuncuoğlu, H.; Keskil, Z.; Keskil, S. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugía 2008, 19, 121–126. [Google Scholar] [CrossRef]
- Shehade, H.; Acolty, V.; Moser, M.; Oldenhove, G. Cutting Edge: Hypoxia-Inducible Factor 1 Negatively Regulates Th1 Function. J. Immunol. 2015, 195, 1372–1376. [Google Scholar] [CrossRef] [PubMed]
- Savransky, V.; Nanayakkara, A.; Li, J.; Bevans, S.; Smith, P.L.; Rodriguez, A.; Polotsky, V.Y. Chronic Intermittent Hypoxia Induces Atherosclerosis. Am. J. Respir. Crit. Care Med. 2007, 175, 1290–1297. [Google Scholar] [CrossRef]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. CMAJ 2016, 188, 567–574. [Google Scholar] [CrossRef]
- Scarano, A.; Inchingolo, F.; Lorusso, F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. Int. J. Environ. Res. Public Health 2020, 17, 4624. [Google Scholar] [CrossRef] [PubMed]
- Farquharson, C.; Baguley, K. Responding to the severe acute respiratory syndrome (SARS) outbreak: Lessons learned in a Toronto emergency department. J. Emerg. Nurs. 2003, 29, 222–228. [Google Scholar] [CrossRef]
- ASHRAE Standard 55-Thermal Environmental Conditions for Human Occupancy; ANSI/ASHRAE Standard: Atlanta, GA, USA, 2020.
- Potchter, O.; Cohen, P.; Lin, T.-P.; Matzarakis, A. Outdoor human thermal perception in various climates: A comprehensive review of approaches, methods and quantification. Sci. Total Environ. 2018, 631, 390–406. [Google Scholar] [CrossRef] [PubMed]
- EN ISO 7730:2005 Ergonomics of the Thermal Environment. Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. Available online: https://www.iso.org/standard/39155.html (accessed on 5 November 2020).
- EN 16798-1:2019 Energy Performance of Buildings—Ventilation for Buildings—Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Acoustics#x2014;Module M1-6. Available online: https://standards.iteh.ai/catalog/standards/cen/b4f68755-2204-4796-854a-56643dfcfe89/en-16798-1-2019 (accessed on 5 November 2020).
- ISO 17772-1:2017 Energy Performance of Buildings—Indoor Environmental Quality—Part 1: Indoor Environmental Input Parameters for the Design and Assessment of Energy Performance of Buildings. Available online: https://www.iso.org/standard/60498.html (accessed on 5 November 2020).
- Fanger, P.O. Thermal Comfort; McGraw Hill: New York, NY, USA, 1970. [Google Scholar]
- Khattabi, E.M.; Zouini, M.; Jamil, M.O. The Thermal Constituting of the Air Provoking the Spread of (COVID-19). SSRN Electron. J. 2020, 3560374. preprint. [Google Scholar] [CrossRef]
- Thapa, S.; Singh, R.; Bundele, M.; Thapa, S.; Thadathil, G.; Jakhar, Y.K. Study of thermal comfort in the residents of different climatic regions of India—Effect of the COVID-19 lockdown. Indoor Air 2021, 31, 899–917. [Google Scholar] [CrossRef] [PubMed]
- Cheshmehzangi, A. Housing and health evaluation related to general comfort and indoor thermal comfort satisfaction during the COVID-19 lockdown. J. Hum. Behav. Soc. Environ. 2020, 31, 184–209. [Google Scholar] [CrossRef]
- Davey, S.; Lee, B.; Robbins, T.; Randeva, H.; Thake, C. Heat stress and PPE during COVID-19: impact on healthcare workers’ performance, safety and well-being in NHS settings. J. Hosp. Infect. 2021, 108, 185–188. [Google Scholar] [CrossRef]
- Xu, X.; Gonzalez, J.A.; Karis, A.J.; Rioux, T.P.; Potter, A.W. Use of Thermal Mannequins for Evaluation of Heat Stress Imposed by Personal Protective Equipment. In Performance of Protective Clothing and Equipment: 10th Volume, Risk Reduction through Research and Testing; Shiels, B., Lehtonen, K., Eds.; ASTM International: West Conshohocken, PA, USA, 2016; pp. 285–295. [Google Scholar] [CrossRef]
- Morooka, H.; Wada, T.; Nakahashi, M. Thermal Comfort Evaluation of Clothing using Thermal Mannequin with Sweating and Walking Function. Netsu Bussei 2015, 27, 157–163. [Google Scholar] [CrossRef][Green Version]
- EN 342:2017—Protective Clothing: Ensembles and Garments for Protection against Cold. 2018. Available online: https://www.sis.se/en/produkter/environment-health-protection-safety/protective-equipment/protective-clothing/ss-en-3422017/ (accessed on 15 November 2017).
- EN ISO 15831:2006—Clothing—Physiological Effects—Measurement of Thermal Insulation by Means of a Thermal Manikin; ISO: Geneva, Switzerland, 2006.
- d’Ambrosio Alfano, F.R.; Olesen, B.W.; Palella, B.I.; Pepe, D.; Riccio, G. Fifty years of PMV model: reliability, implementation and design of software for its calculation. Atmosphere 2020, 11, 49. [Google Scholar] [CrossRef]
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020, 14, 6339–6347. [Google Scholar] [CrossRef] [PubMed]
- Maseczki Ochronne–Rodzaje, Zalecenia i Zagrożenia. Available online: https://loveair.pl/zdrowie/maseczki-ochronne#maski-chirurgiczne (accessed on 5 November 2020).


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zender-Świercz, E.; Telejko, M.; Galiszewska, B. Influence of Masks Protecting against SARS-CoV-2 on Thermal Comfort. Energies 2021, 14, 3315. https://doi.org/10.3390/en14113315
Zender-Świercz E, Telejko M, Galiszewska B. Influence of Masks Protecting against SARS-CoV-2 on Thermal Comfort. Energies. 2021; 14(11):3315. https://doi.org/10.3390/en14113315
Chicago/Turabian StyleZender-Świercz, Ewa, Marek Telejko, and Beata Galiszewska. 2021. "Influence of Masks Protecting against SARS-CoV-2 on Thermal Comfort" Energies 14, no. 11: 3315. https://doi.org/10.3390/en14113315
APA StyleZender-Świercz, E., Telejko, M., & Galiszewska, B. (2021). Influence of Masks Protecting against SARS-CoV-2 on Thermal Comfort. Energies, 14(11), 3315. https://doi.org/10.3390/en14113315







