A Review of the Relation between Household Indoor Temperature and Health Outcomes
Abstract
1. Introduction
- -
- How do indoor temperatures affect health outcomes?
- -
- How does housing energy efficiency improve health outcomes?
2. On the Relevance of Indoor Temperature and Housing Energy Efficiency for Health Outcomes
2.1. Relevance of Indoor Temperature for Health Outcomes
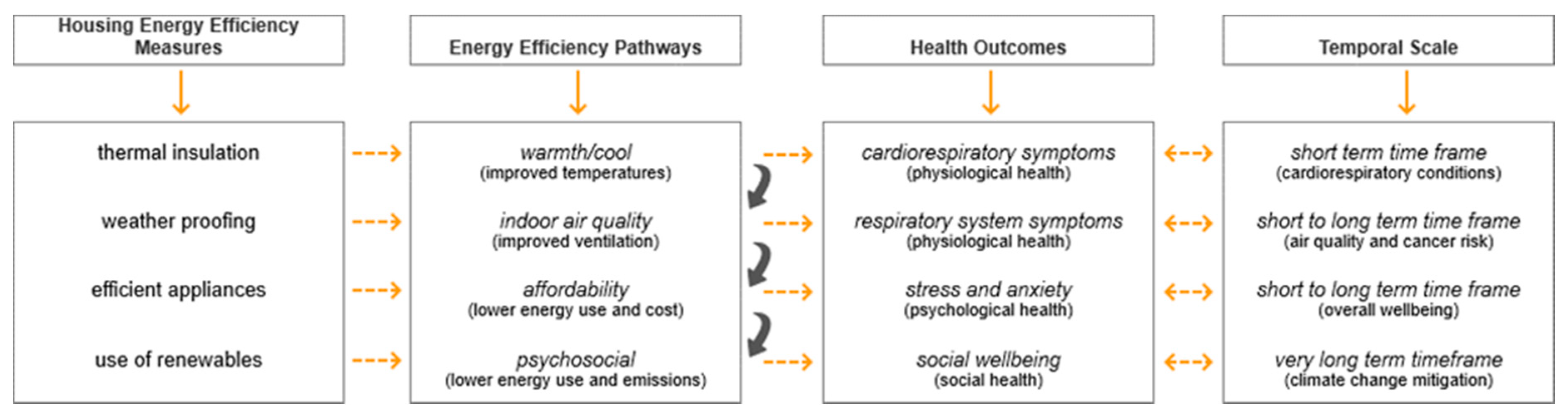
2.2. Relevance of Housing Energy Efficiency for Health Outcomes
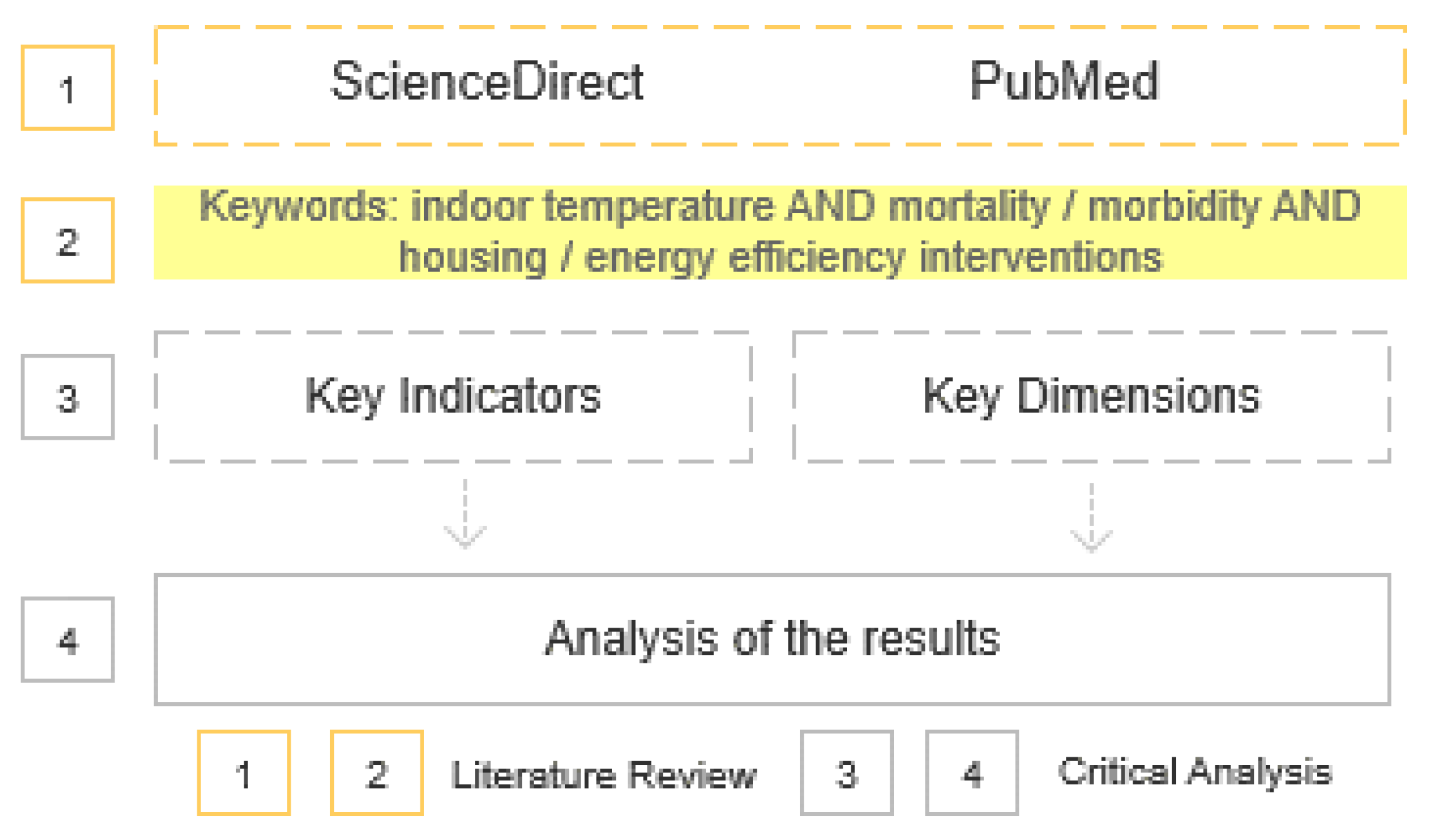
3. Method
- Studies for which full paper is not available on the database;
- Studies addressing health outcomes not related to human and other health outcomes (e.g., vector-borne diseases);
- Studies that are duplicated;
- Studies that are not written in the English language;
- Studies that are not empirical;
- Studies that do not monitor indoor the temperature in loco, with the exception of studies that use empirical indoor temperatures from national surveys;
- Studies that do not assess concurrently indoor temperatures and health outcomes;
- Studies for which the focal point is to assess indoor air quality-related health outcomes;
- Time restrictions are not applied.
4. Results and Critical Analysis
4.1. Analysis of Direct and Indirect Links between Indoor Temperature and Health Outcomes
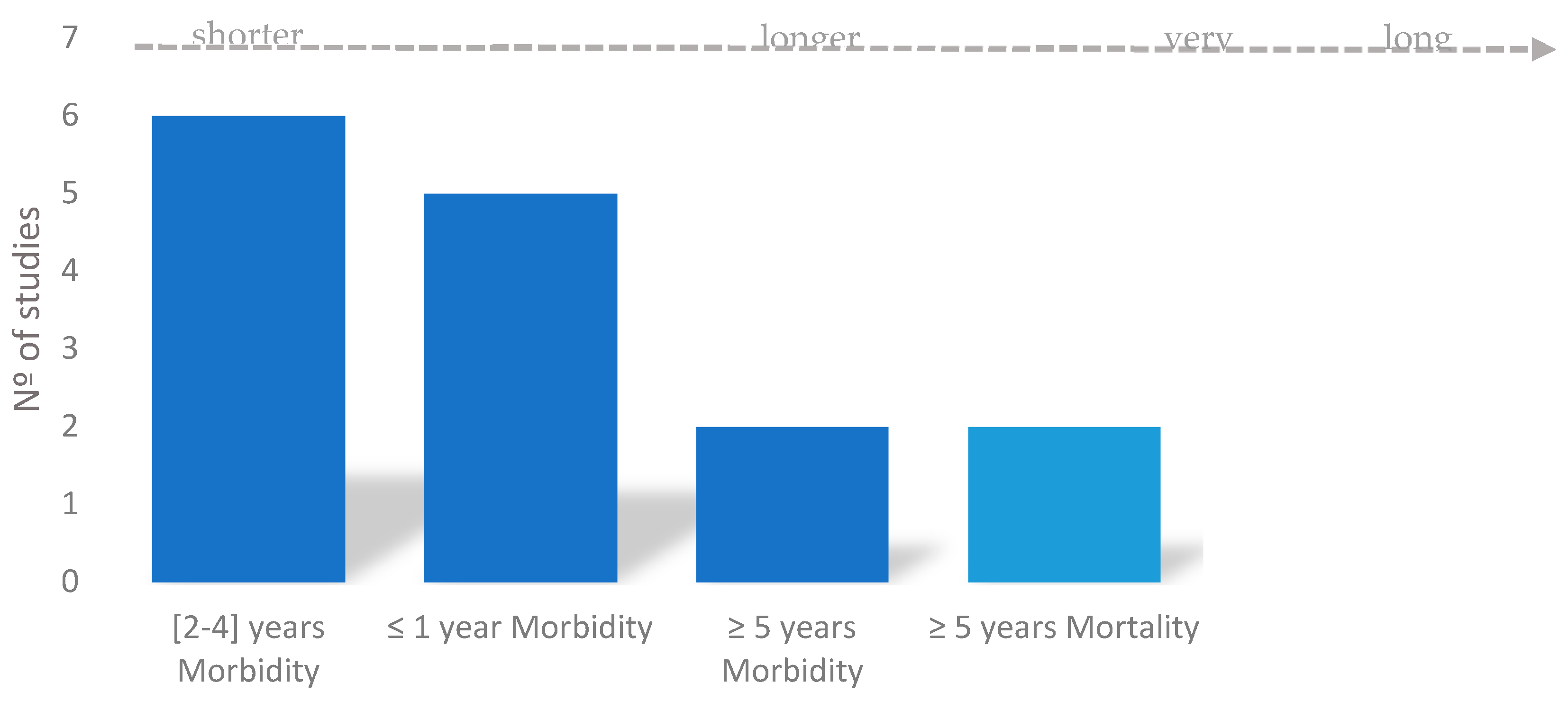
4.2. Analysis of the Relevance of Climate Change Timeframe for Health and Energy Efficiency
4.3. Analysis of Health Outcomes by Study
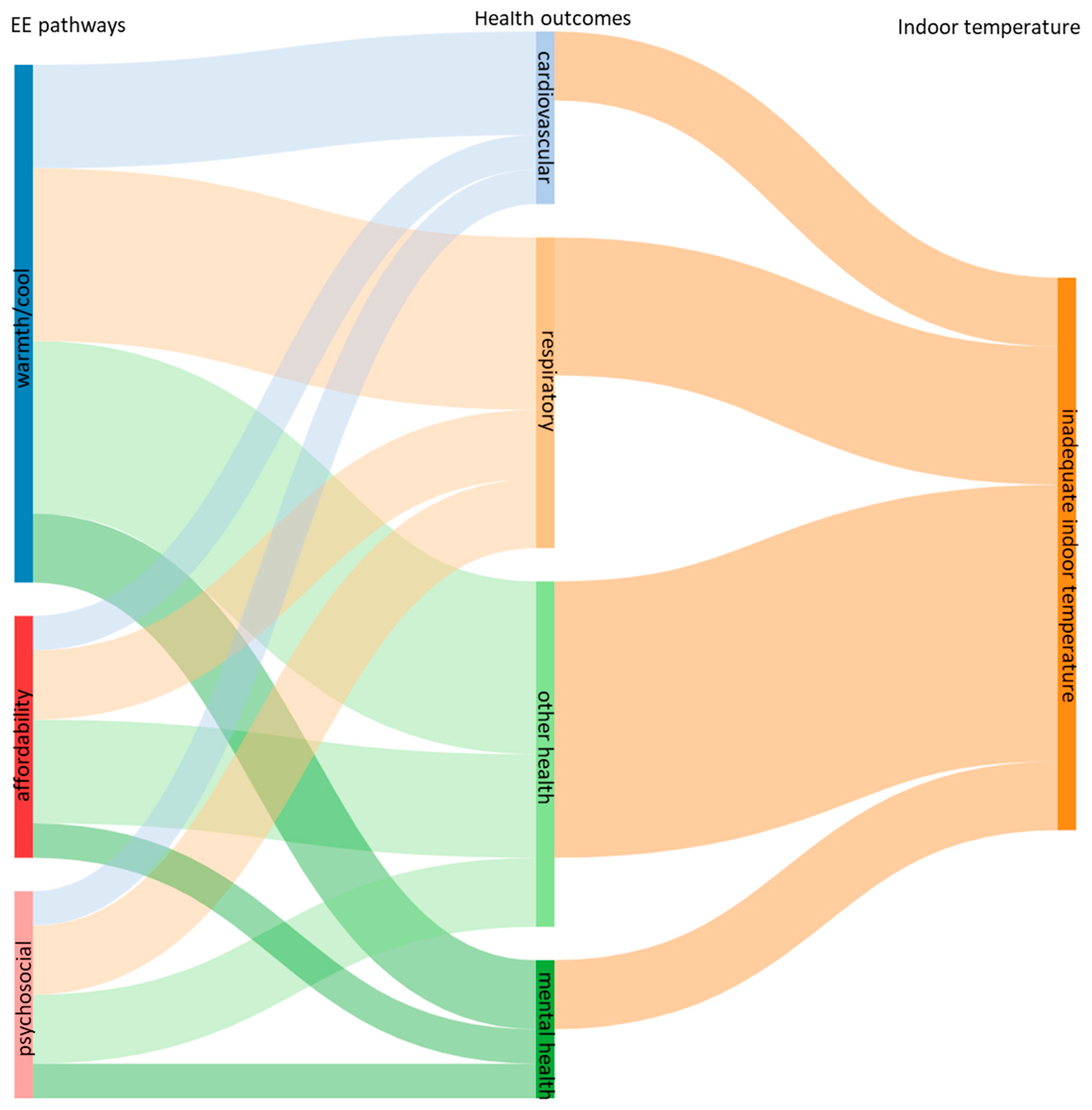
4.4. Analysis of Housing Energy Efficiency and Health
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
List of Acronyms
| EE | energy efficiency |
| HVAC | heating, ventilation and air-conditioning systems |
| HHGL | healthy housing guidelines |
| NCD | non-communicable diseases |
| WHO | World Health Organisation |
| COPD | chronic obstructive pulmonary disease |
References
- Watts, N. Review the Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet 2018, 391, 581–630. [Google Scholar] [CrossRef]
- Vardoulakis, S. Impact of climate change on the domestic indoor environment and associated health risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar] [CrossRef]
- Vandentorren, S. August 2003 heat wave in France: Risk factors for death of elderly people living at home. Eur. J. Public Health 2006, 16, 583–591. [Google Scholar] [CrossRef]
- Liu, C.; Yavar, Z.; Sun, Q. Cardiovascular Responses to Environmental Stress Cardiovascular response to thermoregulatory challenges. Physiol. Heart Circ. Physiol. 2015, 309, H1793–H1812. [Google Scholar] [CrossRef]
- Bunker, A. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef]
- Schneider, A.; Breitner, S. Temperature effects on health—Current findings and future implications. EBioMedicine 2016, 6, 29–30. [Google Scholar] [CrossRef]
- Gasparrini, A. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Freitas, Â.; Santana, P.; Oliveira, M.D.; Almendra, R.; Bana, J.C.; Bana, C.A. Indicators for evaluating European population health: A Delphi selection process. BMC Public Health 2018, 18, 557. [Google Scholar] [CrossRef]
- Howden-chapman, P.; Roebbel, N.; Chisholm, E. Setting Housing Standards to Improve Global Health. Int. J. Environ. Res. Public Health 2017, 14, 1542. [Google Scholar] [CrossRef]
- Ormandy, D.; Ezratty, V. Health and thermal comfort: From WHO guidance to housing strategies. Energy Policy 2012, 49, 116–121. [Google Scholar] [CrossRef]
- Graff, M.; Carley, S. COVID-19 assistance needs to target energy. Nat. Energy 2020, 5, 352–354. [Google Scholar] [CrossRef]
- Intergovernmental Panel for Climate Change (IPCC). In Proceedings of the First Joint Session of Working Groups I and accepted by the 48th Session of the IPCC, Global Warming of 1.5 °C—Summary for Policymakers, Incheon, Korea, 1–5 October 2018.
- Kenny, G.P. Towards establishing evidence-based guidelines on maximum indoor temperatures during hot weather in temperate continental climates. Temperature 2018, 6, 11–36. [Google Scholar] [CrossRef] [PubMed]
- Hansel, N.N.; Mccormack, M.C.; Kim, V. The Effects of Air Pollution and Temperature on COPD ABSTRACT. COPD J. Chronic Obstr. Pulm. Dis. 2016, 13, 372–379. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Non Communicable Diseases (NDC)-Key Facts. Fact Sheets. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 31 December 2018).
- World Health Organisation. Noncommunicable Diseases Country Profles 2018; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Wang, N.; Phelan, P.E.; Harris, C.; Langevin, J.; Nelson, B.; Sawyer, K. Past visions, current trends, and future context: A review of building energy, carbon, and sustainability. Renew. Sustain. Energy Rev. 2018, 82, 976–993. [Google Scholar] [CrossRef]
- Mauree, D.; Naboni, E.; Coccolo, S.; Perera, A.T.D.; Nik, V.M.; Scartezzini, J.-L. A review of assessment methods for the urban environment and its energy sustainability to guarantee climate adaptation of future cities. Renew. Sustain. Energy Rev. 2019, 112, 733–746. [Google Scholar] [CrossRef]
- Taylor, J. Comparison of built environment adaptations to heat exposure and mortality during hot weather, West Midlands region, UK. Environ. Int. 2018, 111, 287–294. [Google Scholar] [CrossRef]
- Taylor, J. Mapping the effects of urban heat island, housing, and age on excess heat-related mortality in London. Urban Clim. 2015, 14, 517–528. [Google Scholar] [CrossRef]
- Healy, J.D. Excess winter mortality in Europe: A cross country analysis identifying key risk factors. J. Epidemiol. Community Health 2003, 57, 784–789. [Google Scholar] [CrossRef]
- Rodgers, S.E. Health impact, and economic value, of meeting housing quality standards: A retrospective longitudinal data linkage study. Public Health Res. 2018, 6, 1–83. [Google Scholar] [CrossRef]
- Miguel-bellod, J.S.; González-martínez, P.; Sánchez-ostiz, A. The relationship between poverty and indoor temperatures in winter: Determinants of cold homes in social housing contexts from the 40s–80s in Northern Spain. Energy Build. 2018, 173, 428–442. [Google Scholar] [CrossRef]
- World Health Organisation. Who Housing and Health Guidelines; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Ortiz, M.A.; Kurvers, S.R.; Bluyssen, P.M. A review of comfort, health, and energy use: Understanding daily energy use and wellbeing for the development of a new approach to study comfort. Energy Build. 2017, 152, 323–335. [Google Scholar] [CrossRef]
- Willand, N.; Ridley, I.; Maller, C. Towards explaining the health impacts of residential energy efficiency interventions—A realist review. Part 1: Pathways. Soc. Sci. Med. 2015, 133, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B. The impact of home energy efficiency interventions and winter fuel payments on winter- and cold-related mortality and morbidity in England: A natural equipment mixed-methods study. Public Health Res. 2018, 6, 1–138. [Google Scholar] [CrossRef] [PubMed]
- Kolokotsa, D.; Santamouris, M. Review of the indoor environmental quality and energy consumption studies for low income households in Europe. Sci. Total Environ. 2015, 536, 316–330. [Google Scholar] [CrossRef]
- Poortinga, W. The health impacts of energy performance investments in low-income areas: A mixed-methods approach. Public Health Res. 2018, 6. [Google Scholar] [CrossRef]
- Ampatzoglou, A.; Bibi, S.; Avgeriou, P.; Verbeek, M.; Chatzigeorgiou, A. Identifying, categorizing and mitigating threats to validity in software engineering secondary studies. Inf. Softw. Technol. 2019, 106, 201–230. [Google Scholar] [CrossRef]
- Zhou, X.; Jin, Y.; Zhang, H.; Li, S.; Huang, X. A map of threats to validity of systematic literature reviews in software engineering. Proc. Asia-Pac. Softw. Eng. Conf. APSEC 2016, 153–160. [Google Scholar] [CrossRef]
- Willand, N.; Maller, C.; Ridley, I. Understanding the contextual influences of the health outcomes of residential energy efficiency interventions: Realist review. Hous. Stud. 2020, 35, 1–28. [Google Scholar] [CrossRef]
- Liddell, C.; Morris, C. Fuel poverty and human health: A review of recent evidence. Energy Policy 2010, 38, 2987–2997. [Google Scholar] [CrossRef]
- van Hoof, J.; Schellen, L.; Soebarto, V.; Wong, J.K.W.; Kazak, J.K. Ten questions concerning thermal comfort and ageing. Build. Environ. 2017, 120, 123–133. [Google Scholar] [CrossRef]
- Jevons, R.; Carmichael, C.; Crossley, A.; Bone, A. Minimum indoor temperature threshold recommendations for English homes in winter—A systematic review. Public Health 2016, 136, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Thomson, H.; Thomas, S.; Sellstrom, E.; Petticrew, M. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst. Rev. 2013, 1–159. [Google Scholar] [CrossRef] [PubMed]
- United Nations. The Sustainable Development Goals Report; United Nations-Department of Economic and Social Affairs: New York, NY, USA, 2018. [Google Scholar]
- Nugent, R. Series The Lancet Taskforce on NCDs and economics 1 Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet 2018, 391, 2029–2035. [Google Scholar] [CrossRef]
- Uejio, C.K.; Tamerius, J.D.; Vredenburg, J.; Asaeda, G.; Isaacs, D.A.; Braun, J.; Freese, J.P. Summer indoor heat exposure and respiratory and cardiovascular distress calls in New York City, NY, US. Indoor Air 2016, 26, 594–604. [Google Scholar] [CrossRef]
- Osman, L.M.; Ayres, J.G.; Garden, C.; Reglitz, K.; Lyon, J.; Douglas, J.G. Home warmth and health status of COPD patients. Eur. J. Public Health 2008, 18, 399–405. [Google Scholar] [CrossRef]
- Saeki, K.; Obayashi, K.; Tone, N.; Kurumatani, N. A warmer indoor environment in the evening and shorter sleep onset latency in winter: The HEIJO-KYO study. Physiol. Behav. 2015, 149, 29–34. [Google Scholar] [CrossRef]
- Saeki, K.; Obayashi, K.; Kurumatani, N. Indoor cold exposure and nocturia: A cross- sectional analysis of the HEIJO-KYO study. BJUI-BJU Int. 2016, 117, 829–835. [Google Scholar] [CrossRef]
- Saeki, K.; Obayashi, K.; Kurumatani, N. Platelet count and indoor cold exposure among elderly people: A cross-sectional analysis of the HEIJO-KYO study. J. Epidemiol. 2017, 27, 562–567. [Google Scholar] [CrossRef]
- van Loenhout, J.A.F. The effect of high indoor temperatures on self-perceived health of elderly persons. Environ. Res. 2016, 146, 27–34. [Google Scholar] [CrossRef]
- Huebner, G.M.; Hamilton, I.; Chalabi, Z.; Shipworth, D. Comparison of indoor temperatures of homes with recommended temperatures and effects of disability and age: An observational, cross-sectional study. BMJ Open 2018, 8, e021085. [Google Scholar] [CrossRef]
- Preval, N.; Keall, M.; Telfar-barnard, L.; Grimes, A.; Howden-chapman, P. Impact of improved insulation and heating on mortality risk of older cohort members with prior cardiovascular or respiratory hospitalisations. BMJ Open 2017, 7, e018079. [Google Scholar] [CrossRef]
- Viggers, H. Effect of insulating existing houses on health inequality: Cluster randomised study in the community. BMJ 2007, 334, 460. [Google Scholar] [CrossRef]
- Osman, L.M.; Ayres, J.G.; Garden, C.; Reglitz, K.; Lyon, J.; Douglas, J.G. A randomised trial of home energy efficiency improvement in the homes of elderly COPD patients. Eur. Respir. J. 2010, 35, 303–309. [Google Scholar] [CrossRef]
- Shiue, I. Cold homes are associated with poor biomarkers and less blood pressure check-up: English Longitudinal Study of Ageing, 2012–2013. Environ. Sci. Pollut. Res. 2016, 23, 7055–7059. [Google Scholar] [CrossRef]
- Shiue, I.; Shiue, M. Indoor temperature below 18 °C accounts for 9% population attributable risk for high blood pressure in Scotland. Int. J. Cardiol. 2014, 171, e1–e2. [Google Scholar] [CrossRef]
- van Hooff, T.; Blocken, B.; Timmermans, H.J.P.; Hensen, J.L.M. Analysis of the predicted effect of passive climate adaptation measures on energy demand for cooling and heating in a residential building. Energy 2016, 94, 811–820. [Google Scholar] [CrossRef]
- Wilson, N.J.; Jacobs, N.D.; Reddy, N.A.; Tohn, T.E.S.E.; Cohen, D.J.; Jacobsohn, D.E. Home RX: The Health Benefits of Home Performance—A Review of the Current Evidence; National Renewable Energy Laboratory for the U.S. Department of Energy (DOE): Columbia, MD, USA, 2016.
- Haines, A. Health and Climate Change 6 Public health benefi ts of strategies to reduce greenhouse-gas emissions: Overview and implications for policy makers. Lancet 2009, 374, 2104–2114. [Google Scholar] [CrossRef]
- Alavy, M.; Li, T.; Siegel, J.A. Energy use in residential buildings: Analyses of high-efficiency filters and HVAC fans. Energy Build. 2020, 209, 109697. [Google Scholar] [CrossRef]
- Jung, W.; Jazizadeh, F. Human-in-the-loop HVAC operations: A quantitative review on occupancy, comfort, and energy-efficiency dimensions. Appl. Energy 2019, 239, 1471–1508. [Google Scholar] [CrossRef]
- Howden-Chapman, P.; Viggers, H.; Chapman, R.; O’Sullivan, K.; Barnard, L.T.; Lloyd, B. Tackling cold housing and fuel poverty in New Zealand: A review of policies, research, and health impacts. Energy Policy 2012, 49, 134–142. [Google Scholar] [CrossRef]
- Xu, X.; Chen, C.F. Energy efficiency and energy justice for U.S. low-income households: An analysis of multifaceted challenges and potential. Energy Policy 2019, 128, 763–774. [Google Scholar] [CrossRef]
- de Cian, E.; Pavanello, F.; Randazzo, T.; Mistry, M.N.; Davide, M. Households’ adaptation in a warming climate. Air conditioning and thermal insulation choices. Environ. Sci. Policy 2019, 100, 136–157. [Google Scholar] [CrossRef]
- Guertler, P.; Smith, P. Cold Homes and Excess Winter Deaths a Preventable Public Health Epidemic That Can No Longer Be Tolerated; February 2018; E3G and National Energy Action (NEA): Newcastle upon Tyne, UK, 2018. [Google Scholar]
- Daniel, L.; Baker, E.; Williamson, T. Cold housing in mild-climate countries: A study of indoor environmental quality and comfort preferences in homes, Adelaide, Australia. Build. Environ. 2019, 151, 207–218. [Google Scholar] [CrossRef]
- Magalhães, S.M.C.; Leal, V.M.S.; Horta, I.M. Predicting and characterizing indoor temperatures in residential buildings: Results from a monitoring campaign in Northern Portugal. Energy Build. 2016, 119, 293–308. [Google Scholar] [CrossRef]
- Willand, N.; Maller, C.; Ridley, I. Addressing health and equity in residential low carbon transitions—Insights from a pragmatic retrofit evaluation in Australia. Energy Res. Soc. Sci. 2019, 53, 68–84. [Google Scholar] [CrossRef]
- Alkire, S.; Samman, E. Mobilizing the Household Data Required to Progress toward the SDGS; University of Oxford: Oxford, UK, 2014. [Google Scholar]
- Bogart, S. SankeyMATIC. 2020. Available online: http://sankeymatic.com/ (accessed on 20 May 2020).
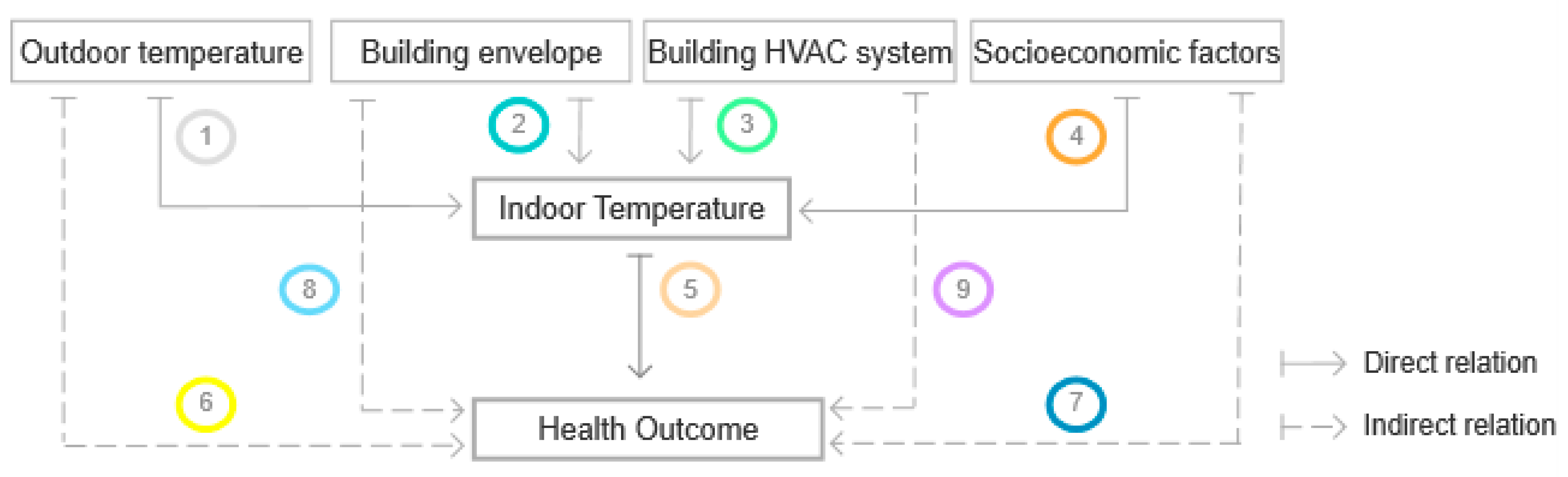

| Links | Studies on Indoor Temperature | |
|---|---|---|
 | outdoor- indoor temperature | [27,29,39,40,41,42,43,44,45,46,47,48,49,50] |
 | building envelope- indoor temperature | [27,29,40,44,46,47,48] |
 | HVAC system- indoor temperature | [22,27,29,44,46,48] |
 | socioeconomic factor- indoor temperature | [27,29,39,40,41,42,43,44,45,46,47,48,49,50] |
 | indoor temperature- health outcome | [27,29,39,40,47,48,49,50] |
 | outdoor temperature- health outcome | [27] |
 | building envelope- health outcome | [22,27,45,46] |
 | HVAC system- health outcome | [22,27,45,46] |
 | socioeconomic factor- health outcome | - |
| Cause-Effect assessed | ||
| [22] | energy efficiency upgrade—low indoor temperature—emergency hospital admissions cardiovascular and respiratory conditions and injuries | |
| [27] | energy efficiency upgrade—low indoor temperature—cardiovascular and respiratory health related conditions | |
| outdoor temperature—cardiovascular and respiratory-related mortality and morbidity | ||
| [29] | high indoor temperature—emergency hospital admissions cardiovascular and respiratory conditions; psychosocial impacts | |
| [39] | low indoor temperature—emergency care for cardiovascular and respiratory conditions | |
| [40] | low indoor temperature—cardiovascular and mental health related biomarkers | |
| [41] | low indoor temperature—cardiovascular and mental health related biomarkers | |
| [42] | low indoor temperature—cardiovascular and mental health related biomarkers | |
| [43] | low indoor temperature—cardiovascular related biomarkers | |
| [44] | high indoor temperature—heat-related health symptoms | |
| [45] | low indoor temperature—long term health disabilities | |
| [46] | energy efficiency upgrades—low indoor temperature cardiovascular and respiratory-related mortality | |
| [47] | energy efficiency upgrade—low indoor temperature general health; respiratory-related conditions and general practitioner’s hospital admissions | |
| [48] | energy efficiency upgrade—low indoor temperature—respiratory related conditions, general health status hospital admissions | |
| [49] | low indoor temperature—cardiovascular related biomarkers | |
| [50] | low indoor temperature—cardiovascular related biomarkers | |
| Health Indicators | Mentioned | Direct Assessment (Measured) |
|---|---|---|
| Mental health disorders | [42] | [22,29,39,45] |
| Altered mental health status | - | [39] |
| Depression | [42] | - |
| Long term mental disability (LTD) | - | [45] |
| Common mental health disorders | - | [22,29] |
| Cardiovascular | [27,42,43,48,50] | [22,29,39,45,46] |
| Cardiac condition | - | [39] |
| Cardiac arrest | - | [39] |
| Cardiovascular condition | - | [22,29,39,46] |
| Myocardial infarction | [41,43] | - |
| Coronary heart disease | [27,42,43] | - |
| Heart attacks | [43,50,51] | - |
| Stroke/Cerebrovascular disease | [27,43,48,50] | - |
| Long term heart disability (LTD) | - | [45] |
| Respiratory | [44,46,47,50] | [22,29,39,40,45,46,47,48,49] |
| Difficulty breathing | [39] | [39,45] |
| Asthma | [46,47] | [22,39] |
| Respiratory conditions | - | [22,29,39,45,46,47,48,49] |
| Pneumonia | [39] | [39] |
| Insufficient cardiac blood flow | - | [39] |
| Lung disease | - | [39] |
| Emphysema/Chronic Obstructive Pulmonary Disease (COPD) | - | [22,39,40,48] |
| Lung function | - | [49] |
| long term breathing disability (LTD) | - | [45] |
| Other health indicators | [27,39,41,42,43,44,48] | [22,27,29,40,41,42,43,44,45,47,48,49,50] |
| Hypertension | [39,42,43,44] | - |
| Diabetes | [39,41,42,43] | - |
| Unconscious | [39] | - |
| Epileptic status | [39] | |
| Annoyance | - | [44] |
| Thirst | - | [44] |
| Sleep disturbance | - | [44] |
| Excessive sweating | - | [44] |
| Dehydration | [44] | - |
| Hyperthermia | [44] | - |
| Malaise | [44] | - |
| Hyponatremia | [44] | - |
| Renal colic and renal failure | [44] | - |
| Dry mouth | [44] | - |
| Impaired endurance | [44] | - |
| Fatigue | [44] | - |
| Sleep onset latency (SOL) | - | [41] |
| All-cause mortality | [27,44,47] | - |
| Excess winter mortality | - | [27] |
| Nocturia | - | [43] |
| Reduced quality of life | [43] | [29] |
| Falls and fractures/injuries | [43] | [22] |
| Blood pressure | - | [50,52,63] |
| Mean arterial pressure | - | [50] |
| Handgrip | - | [50] |
| Blood low-density lipoprotein level | - | [50] |
| Vitamin D level | - | [50] |
| Blood insulin-like growth factor | - | [50] |
| Blood haemoglobin level | - | [50] |
| White Blood cell count | - | [50] |
| Increased Blood viscosity | [52] | - |
| Platelet count (PTL) | - | [44] |
| General health status | - | [40,51,52] |
| Long term vision disability (LTD) | - | [46] |
| Long term hearing disability (LTD) | - | [46] |
| Long term mobility disability (LTD) | - | [46] |
| Long term learning disability (LTD) | - | [46] |
| EE Measures | Studies | Observation Summary |
|---|---|---|
| Insulation | [22] 65.8% of installed wall insulation met housing quality standard; changes in indoor temperature not specified; [21] 31.8% of installed loft insulation met housing quality standard, changes in indoor temperature not specified [27] loft insulation associated to lower increases in temperature than increases associated to cavity and wall insulation; overall modest change in standard indoor temperature, averaging *0.09 °C [29] external wall insulation was the EE alternative that most contributed to increase indoor temperature (1.12 °C, 95% CI); overall indoor temperature increased on average by *0.84 °C; did not change indoor RH levels (−0.60% RH, 95% CI) [46]; [47] insulation retrofits increased on average bedroom temperatures by 0.5 °C, reduced time exposed to temperatures below 10 °C by 1.7 h per day and decreased relative humidity by 2.3% a [48] no adoption of EE alternatives implied lower baseline rating b than EE adoption (4.8 vs. 5.6); fewer hours of baseline hours of warmth above 21 °C in living rooms (48 h vs. 69 h) * | |
| wall | [22,27,29,48] | |
| floor | [46,47,48] | |
| ceilling/roof | [46,47] | |
| loft | [22,27,48] | |
| Windows & doors | [22,27,29,47] | [22] 52.4% of new windows and doors met housing quality standard; changes in indoor temperature not specified [27] double glazing was adopted and not associated with appreciable energy savings; overall modest change in standard indoor temperature, averaging *0.09 °C [29] new windows and doors did not increase indoor air temperatures significantly on average by −0.02 °C, 95% CI); new windows and doors increased indoor relative humidity (RH) on average by (5.15% RH, 95% CI) [47] EE adoption included draught stopping around windows and doors; changes in indoor temperature not specified by this measure |
| Appliances | [22] 77.4% of new heating systems met housing quality standard; changes in indoor temperature not specified [29] new boiler or heating system did not increase indoor air temperatures significantly on average by (−0.19 °C, 95% CI); did not change indoor RH levels (−1.59% RH, 95% CI) [46] heating retrofits with baseline underfloor and ceiling insulation recorded an increased average living room temperature by1.1°C a [48] EE adoption implied improvements in EE rating and fuel costs | |
| heating systems | [22,29,46,48] | |
| Others | [29] gas network connection significantly increased indoor temperature on average by (0.69 °C, 95% CI); increased indoor RH levels by (3.86% RH, 95% CI) [22] 81.1% of kitchen improvements met housing quality standard [22] 81.9% of bathroom improvements met housing quality standards [22] 91.6% of electric system adoption met housing quality standard [22] 30.2% of garden path improvements met standard housing quality | |
| fuel switching | [29] | |
| kitchens | [22] | |
| bathrooms | [22] | |
| electrical systems c | [22] | |
| garden paths | [22] |
| Health Outcome | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiovascular | Respiratory | Mental Health | All Health * | Indoor Temperature | |||||||||
| EE Alternatives | Insulation | Windows & Doors | Heating Systems | Insulation | windows & Doors | Heating Systems | Insulation | windows & Doors | Heating Systems | Insulation | Windows & Doors | Heating Systems | |
| References | |||||||||||||
| [22] | ⁺⁺ a | 0 | 0 | ⁺ a | ⁺⁺ | 0 | ⁺ a | ⁺⁺ | 0 | ↑ | |||
| 0 b | 0 b | 0 d | 0 b | ||||||||||
| [27] | ⁺ d | ↑ | |||||||||||
| [29] | -- | 0 d | 0 d | ↑ | |||||||||
| [46] | ⁺⁺ c | 0 | ⁺ c | 0 | ↑ | ||||||||
| [47] | ⁺⁺ c | ⁺⁺ c | ↑ | ||||||||||
| [48] | ⁺⁺ d | ⁺⁺ d | ↑ | ||||||||||
| Impact level: | |||||||||||||
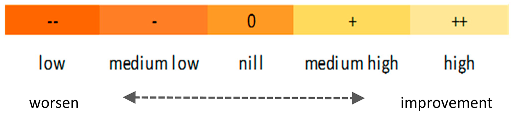 | |||||||||||||
| Studies | Summary of Key Findings |
|---|---|
| [22] | Cardiovascular Condition—Older residents:
|
| [29] |
|
| [22] | Respiratory Condition—Older residents:
|
| [22] | Injuries (falls and burns)—Older residents:
|
| [22] | All health outcomes—All ages:
|
| [27] |
|
| [22] | Respiratory Condition—All ages:
|
| [46] | Cardiovascular and respiratory Condition—All ages:
|
| [46] |
|
| [47] |
|
| [22] | Mental health—All ages:
|
| [29] |
|
| [29] | Wellbeing, thermal satisfaction and social interaction:
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lima, F.; Ferreira, P.; Leal, V. A Review of the Relation between Household Indoor Temperature and Health Outcomes. Energies 2020, 13, 2881. https://doi.org/10.3390/en13112881
Lima F, Ferreira P, Leal V. A Review of the Relation between Household Indoor Temperature and Health Outcomes. Energies. 2020; 13(11):2881. https://doi.org/10.3390/en13112881
Chicago/Turabian StyleLima, Fátima, Paula Ferreira, and Vítor Leal. 2020. "A Review of the Relation between Household Indoor Temperature and Health Outcomes" Energies 13, no. 11: 2881. https://doi.org/10.3390/en13112881
APA StyleLima, F., Ferreira, P., & Leal, V. (2020). A Review of the Relation between Household Indoor Temperature and Health Outcomes. Energies, 13(11), 2881. https://doi.org/10.3390/en13112881