Abstract
This article presents a case report of an adult patient with chronic sinusitis related to the presence of two erupted ectopic teeth located atypically in the maxillary sinus roof/orbital floor after a long latency period associated with childhood facial trauma. This article aims to show the treatment of chronic sinusitis of odontogenic origin by surgical removal of ectopic teeth in an unusual position by direct visualization. This case report discusses the signs and symptoms of chronic sinusitis linked to the presence of ectopic elements and associated with an inflammatory cyst, the choice of complementary tests for diagnosis and surgical treatment through the Caldwell-Luc procedure. After a 2-year follow-up period, the patient presently shows clinical improvement, thus demonstrating the success of the chosen treatment.
Dental development occurs by means of a complex interaction between the oral epithelium and the mesenchymal tissue. Abnormal interactions during this development can cause abnormalities such as ectopies or morphological changes [1,2,3,4]. Dental ectopia may occur in primary, permanent, or supernumerary teeth, the last being found on the palate, maxillary sinus, nasal cavity, condyle, coronoid process, orbit, and ethmoid sinus [1,5,6,7,8,9]. This condition predominantly occurs in males (60%), although there is no anatomical site predisposition [6,7].
Although its etiology is uncertain, some conditions are thought to lead to the development of this pathology, such as tooth displacement by trauma or cysts, odontogenic or rhinogenic infections, excessive bone density, teething obstruction, primary tooth retention, cleft palate, and genetic factors [7,10,11,12].
Clinically, these elements may or may not be associated with symptoms. Patients generally remain asymptomatic throughout life, and these elements are only detected in routine radiographic examination. The symptomatic condition on the maxillary sinus may cause nasal edema, headache, runny nose, and nasomaxillary anatomy deviation [5,8,13]. The treatment of these pathological entities should, whenever possible, include tooth removal [10].
This study aims to show a case of chronic sinusitis associated with the presence of two ectopic teeth in the maxillary sinus in an atypical position and closely related to the orbital floor and its surgical treatment.
Case Report
A 60-year-old male patient was referred to the Department of Oral and Maxillofacial Surgery of the Dentistry School showing discomfort in his left maxilla and claiming breathing and phonatory difficulties. He reported the occurrence of facial trauma at the age of 6, when he was kicked by a horse in this area, having been taken to the emergency room where a blunt injury on his left hemiface with loss of teeth and left maxillary fracture were observed. The trauma was not surgically treated. He also mentioned that his permanent dentition had erupted in an irregular and malpositioned pattern and had been extracted over time.
Left-sided facial scars without evidence of changes that could point to the occurrence of an acute infectious process were observed in the extraoral physical examination. The intraoral examination revealed total upper edentulism and the use of a dental prosthesis; the presence of an oroantral fistula with spontaneous purulent drainage and bulging of the area was observed in the posterior area of the left maxilla. The lack of bone support at the bottom of the vestibular sulcus and a mild discomfort during the procedure were observed during palpation. The patient showed signs and symptoms consistent with chronic sinusitis. A cone beam computed tomographic (CT) scan of the maxilla and paranasal sinuses was performed, revealing the presence of foreign bodies lodged in the roof and the medial wall of the left maxillary sinus, with morphological characteristics of teeth. Also, the sinus was veiled, confirming the diagnosis of chronic sinusitis, in this case caused by foreign bodies (Figure 1a,b). The patient had no change in visual acuity or ocular mobility due to the presence of the teeth in sinus roof/orbital floor.
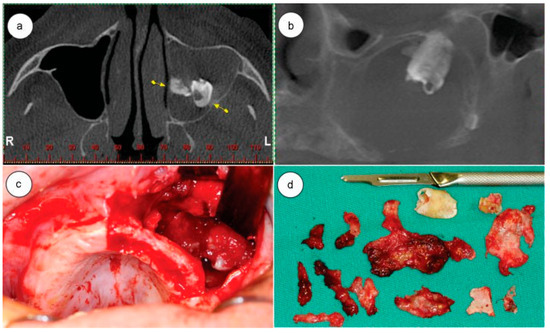
Figure 1.
(a) Computed tomography (CT) axial slice, arrows are showing the teeth in maxillary sinus; (b) CT coronal slice showing the teeth in maxillary sinus roof; (c) surgical approach showing the tooth; (d) teeth and removed tissue.
The removal of the teeth under general anesthesia was decided due to their proximity to the orbital floor and the extensive involvement of the maxillary sinus.
Although literature recommends the use of an endoscope in relation to direct access or the Caldwell-Lucprocedure [14,15], the access was chosen due to the possibility of direct visualization of the surgical site, the size and location of foreign bodies, as well as the unavailability of an endoscope in the department. An incision in the alveolar ridge (due to decreased alveolar height), exposure and removal of the anterior part of the maxillary sinus, and the removal of the dental elements located on the medial wall and roof of the maxillary sinus were performed. After inspecting the interior of the maxillary sinus to rule out the presence of any other foreign body, the sinus mucosa was removed and sent for histopathological examination, which revealed a cyst of inflammatory nature. The flap was repositioned and sutured with 4.0 resorbable Vicryl wire (Figure 1c,d).
The patient was treated with 875 mg amoxicillin + 125 mg Clavulanate Potassium 1 capsule every 12 hours for 14 days, 1 tablet 100 mg Nimesulide every 12 hours for 4 days, and 1 tablet 750 mg paracetamol every 6 hours in case of pain or fever. After 10 days, the suture was removed, upon which a tiny buccosinusal communication was noted. We opted to wait for a better cicatrization of the area to confirm the clinical picture and eventually perform reconstructive surgery. A CT scan was performed in the immediate postoperative period, in which the complete removal of ectopic structures and the preservation of the maxillary roof sinus and orbital floor could be observed (Figure 2a).
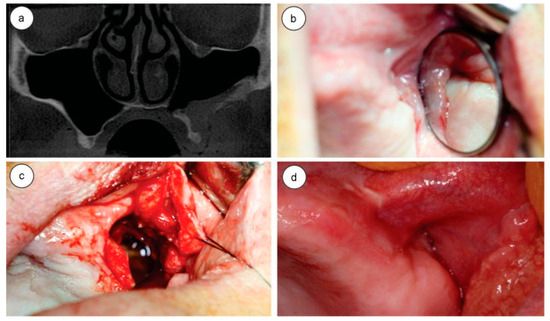
Figure 2.
(a) Postoperative computed tomography coronal slice showing the healing sinus; (b) postoperative oroantral communication; (c) oroantral communication closure surgery; (d) postoperative 3 years follow-up.
Within 2 weeks after surgery, the patient showed an improvement with respect to respiration and phonation. Clinical examination showed a buccosinusal communication, and after certifying that the maxillary sinus was healthy through its irrigation with 0.9% saline, the communication was closed with the combination of a marginal flap with a vestibular flap performed under local anesthesia (Figure 2b,c).
After a 3-year postoperative follow-up period, the patient has not shown any sinusitis, buccosinusal communication, diplopia, limitation of ocular movements, or any other complaints. The patient is still being followed up (Figure 2d).
Discussion
After the identification of ectopic elements in the maxillofacial region, an investigation is needed to determine possible causes and adjacent lesions. In the case reported in this study, it is believed that, due to the history of the patient, the facial trauma that occurred during childhood was responsible for the displacement of the tooth germs in formation into the maxillary sinus, where the tooth development process and dental ectopia occurred [2,9,12,13].
The presence of ectopic teeth in the maxillary sinus can cause symptoms such as chronic sinusitis, purulent discharge, pain, severe headache, ostiomeatal complex and nasolacrimal duct obstruction, facial edema and asymmetry, epistaxis, and hemoptysis [2,5,9,12,13,14]. These teeth may also be associated with cysts and pathologies in the area. The dentigerous and inflammatory cysts are the most commonly found pathologies [1,3,15].
In this case report, the patient was referred to the department with a chronic sinusitis condition due to the presence of teeth on the maxillary sinus roof associated with an empyema with oral drainage and oral and facial edema.
Some studies have reported that panoramic radiography should be the elective examination for the detection of ectopic teeth in maxillofacial structures, because of the distinctness of the exam in the detection of such structures and the low level of radiation to which the patient is subjected. On the other hand, Waters radiographic exposure is inadequate for the diagnosis of these lesions because of bone overlap [12,15]. Cone beam CT scan was performed in the region, inasmuch as it allows a larger area detailing, thus optimizing surgical planning, once it is possible to visualize the tooth structure morphology, and root inclination and position in relation to the underlying structures. Thus, it is possible to predict eventual transoperative intercurrences, postoperative complications, and prognosis [1,8,16,17]. In this case, the CT scan allowed the observation of the exact location of both ectopic structures, which were inserted into the roof of the maxillary sinus and the medial wall, closely related to the orbital floor and nasal cavity, respectively.
The treatment of choice for these pathologic entities should, whenever possible, include the removal of the dental elements. However, in asymptomatic cases without associated pathologies, only a rigid clinical and radiological control may suffice [9].
Historically, among existing surgical techniques used in the removal of foreign bodies from the maxillary sinus, the Caldwell-Luc procedure has been considered as the first choice of treatment, even though complications such as epistaxis, periorbital injuries, damage to extrinsic eye muscles, and orbital hemorrhage have been reported in literature. The main advantage of this access is the direct visualization of structures and pathologies in the maxillary sinus. The removal of maxillary mucosa for histopathological evaluation is also recommended. Extraction via transnasal endoscopy can be performed to remove small teeth located near the maxillary ostium [2,3,14].
In the case discussed, the Caldwell-Luc procedure was chosen due to the need to remove the cyst adjacent to ectopic elements and the sinus mucosa, as well as to the possibility of correcting defects in the maxillary sinus roof and the unavailability of an endoscope in the department.
Conclusion
In spite of being rare, the occurrence of ectopic teeth in the maxillary sinus has been reported in the literature. In this case report, the presence of unusually positioned teeth in the orbital floor/maxillary sinus roof, causing disagreeable sinus disturbances, was observed, and the removal of the dental elements was necessary so that a final resolution of the problem could be reached. Thus, high-quality imaging exams are essential for an accurate diagnosis and appropriate surgical planning.
References
- Saleem, T.; Khalid, U.; Hameed, A.; Ghaffar, S. Supernumerary, ectopic tooth in the maxillary antrum presenting with recurrent haemoptysis. Head Face Med. 2010, 6, 26. [Google Scholar] [CrossRef]
- Mohan, S.; Kankariya, H.; Harjani, B.; Sharma, H. Ectopic third molar in the maxillary sinus. Natl. J. Maxillofac. Surg. 2011, 2, 222–224. [Google Scholar] [CrossRef]
- Goh, Y.H. Ectopic eruption of maxillary molar tooth—an unusual cause of recurrent sinusitis. Singapore Med J 2001, 42, 80–81. [Google Scholar] [PubMed]
- Ramanojam, S.; Halli, R.; Hebbale, M.; Bhardwaj, S. Ectopic tooth in maxillary sinus: case series. Ann Maxillofac Surg 2013, 3, 89–92. [Google Scholar] [CrossRef]
- Jude, R.; Horowitz, J.; Loree, T. A case report. Ectopic molars that cause osteomeatal complex obstruction. J Am Dent Assoc 1995, 126, 1655–1657. [Google Scholar] [CrossRef] [PubMed]
- Yeung, K.H.; Lee, K.H. Intranasal tooth in a patient with a cleft lip and alveolus. Cleft Palate Craniofac J 1996, 33, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Lee, F.P. Endoscopic extraction of an intranasal tooth: a review of 13 Cases. Laryngoscope 2001, 111, 1027–1031. [Google Scholar] [CrossRef]
- Bodner, L.; Tovi, F.; Bar-Ziv, J. Teeth in the maxillary sinus—imaging and management. J Laryngol Otol 1997, 111, 820–824. [Google Scholar] [CrossRef]
- Erkmen, N.; Olmez, S.; Onerci, M. Supernumerary tooth in the maxillary sinus: case report. Aust Dent J 1998, 43, 385–386. [Google Scholar] [CrossRef]
- Moreano, E.H.; Zich, D.K.; Goree, J.C.; Graham, S.M. Nasal tooth. Am J Otolaryngol 1998, 19, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Gupta, Y.K.; Shah, N. Intranasal tooth as a complication of cleft lip and alveolus in a four year old child: case report and literature review. Int J Paediatr Dent 2001, 11, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Baykul, T.; Doğru, H.; Yasan, H.; Cina Aksoy, M. Clinical impact of ectopic teeth in the maxillary sinus. Auris Nasus Larynx 2006, 33, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Alexandrakis, G.; Hubbell, R.N.; Aitken, P.A. Nasolacrimal duct obstruction secondary to ectopic teeth. Ophthalmology 2000, 107, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Viterbo, S.; Griffa, A.; Boffano, P. Endoscopic removal of an ectopic tooth in maxillary sinus. J Craniofac Surg 2013, 24, e46–e48. [Google Scholar] [CrossRef] [PubMed]
- Buyukkurt, M.C.; Omezli, M.M.; Miloglu, O. Dentigerous cyst associated with an ectopic tooth in the maxillary sinus: a report of 3 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010, 109, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.T.A.; Luk, Y.S.; Fung, K.H. Anomalous morphology of an ectopic tooth in the maxillary sinus on three-dimensional computed tomography images. J Radiol Case Rep 2013, 7, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Hong, J.H. Headache induced by an ectopic tooth. Headache 2012, 52, 307–308. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. The Author(s) 2016.