Management of Mandibular Angle Fractures by Two Conventional 2.0-mm Miniplates: A Retrospective Study of 389 Patients
Abstract
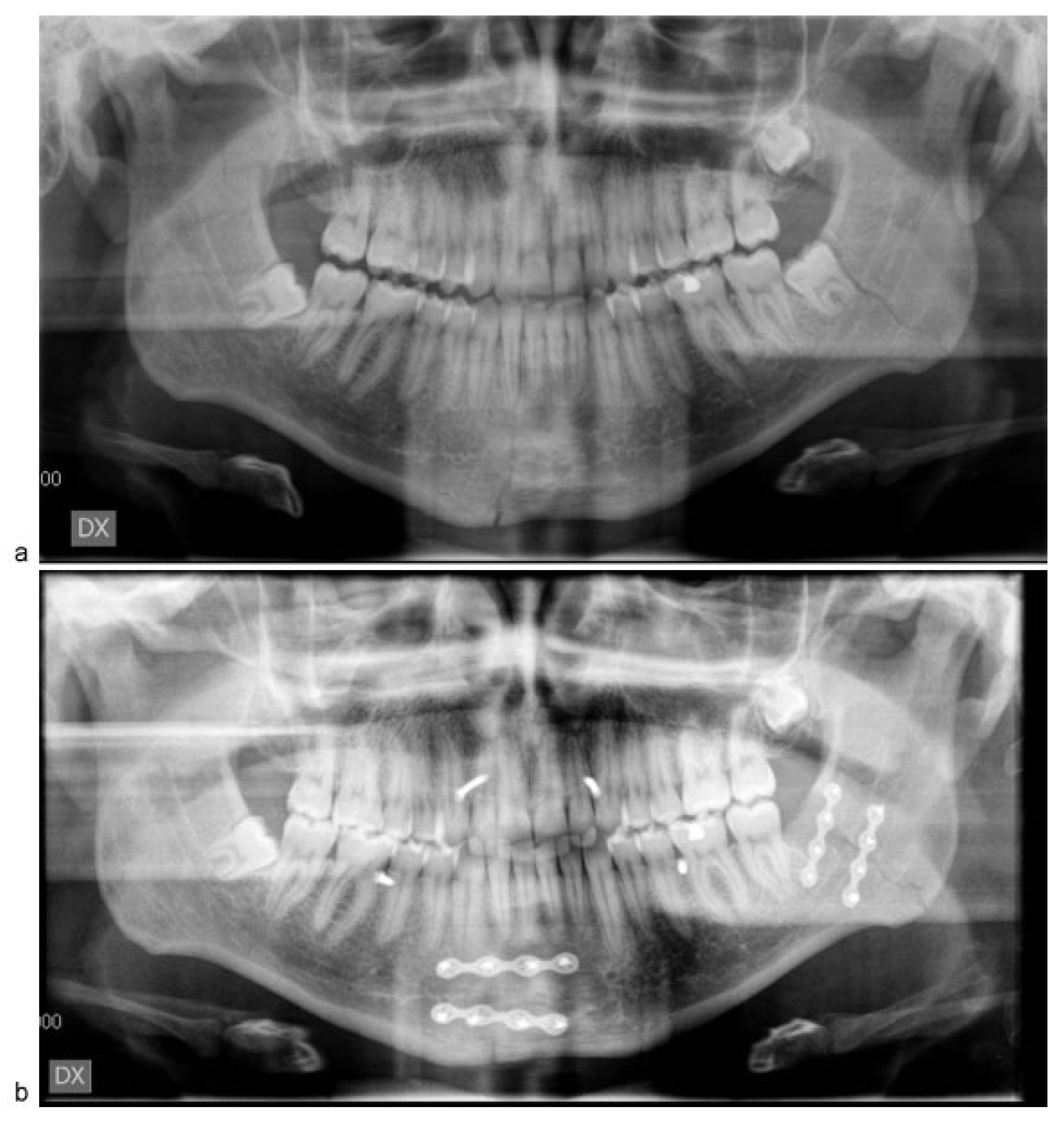
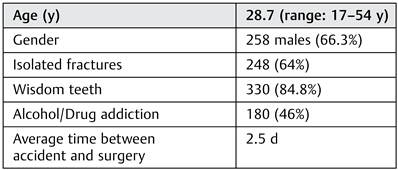
:Patients and Methods
Results
Discussion
Conclusion
Financial Disclosure
Funding
References
- Ellis, E., III; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: An analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol 1985, 59, 120–129. [Google Scholar] [CrossRef]
- Barry, C.P.; Kearns, G.J. Superior border plating technique in the management of isolated mandibular angle fractures: A retrospective study of 50 consecutive patients. J Oral Maxillofac Surg 2007, 65, 1544–1549. [Google Scholar] [CrossRef]
- Sugar, A.W.; Gibbons, A.J.; Patton, D.W.; et al. A randomised controlled trial comparing fixation of mandibular angle fractures with a single miniplate placed either transbuccally and intra-orally, or intra-orally alone. Int J Oral Maxillofac Surg 2009, 38, 241–245. [Google Scholar] [CrossRef]
- Schmelzeisen, R.; McIff, T.; Rahn, B. Further development of titanium miniplate fixation for mandibular fractures. Experience gained and questions raised from a prospective clinical pilot study with 2.0 mm fixation plates. J Craniomaxillofac Surg 1992, 20, 251–256. [Google Scholar] [CrossRef]
- Passeri, L.A.; Ellis, E.I.I.I.; Sinn, D.P. Complications of non-rigid fixation of mandibular angle fractures. J Oral Maxillofac Surg 1993, 51, 22. [Google Scholar] [CrossRef] [PubMed]
- Niederdellmann, H.; Akuamoa-Boateng, E.; Uhlig, G. Lag-screw osteosynthesis: A new procedure for treating fractures of the mandibular angle. J Oral Surg 1981, 39, 938–940. [Google Scholar] [PubMed]
- Michelet, F.X.; Deymes, J.; Dessus, B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J Maxillofac Surg 1973, 1, 79–84. [Google Scholar] [CrossRef]
- Champy, M.; Loddé, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg 1978, 6, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H.; Yoo, J.H.; Kim, K.N.; Kang, H.S. Stability testing of a two miniplate fixation technique for mandibular angle fractures. An in vitro study. J Craniomaxillofac Surg 1995, 23, 123–125. [Google Scholar] [CrossRef]
- Levy, F.E.; Smith, R.W.; Odland, R.M.; Marentette, L.J. Monocortical miniplate fixation of mandibular angle fractures. Arch Otolaryngol Head Neck Surg 1991, 117, 149–154. [Google Scholar] [CrossRef]
- Ellis, E., III; Walker, L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 1994, 52, 1032–1036, discussion 1036–1037. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Lindqvist, C. Rigid internal fixation of fractures in the angular region of the mandible: An analysis of factors contributing to different complications. Plast Reconstr Surg 1993, 91, 265–271, discussion 272–273. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Lindqvist, C.; Hallikainen, D.; Paukku, P. Infection after rigid internal fixation of mandibular fractures: A clinical and radiologic study. J Oral Maxillofac Surg 1991, 49, 585–593. [Google Scholar] [CrossRef]
- Paza, A.O.; Abuabara, A.; Passeri, L.A. Analysis of 115 mandibular angle fractures. J Oral Maxillofac Surg 2008, 66, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.; Markose, G.; Moos, K.F.; McMahon, J.; Ayoub, A.F. One miniplate versus two in the management of mandibular angle fractures: A prospective randomised study. Br J Oral Maxillofac Surg 2007, 45, 223–225. [Google Scholar] [CrossRef]
- Bormann, K.H.; Wild, S.; Gellrich, N.C.; et al. Five-year retrospective study of mandibular fractures in Freiburg, Germany: Incidence, etiology, treatment, and complications. J Oral Maxillofac Surg 2009, 67, 1251–1255. [Google Scholar] [CrossRef]
- Fox, A.J.; Kellman, R.M. Mandibular angle fractures: Two-miniplate fixation and complications. Arch Facial Plast Surg 2003, 5, 464–469. [Google Scholar] [CrossRef]
- Seemann, R.; Schicho, K.; Wutzl, A.; et al. Complication rates in the operative treatment of mandibular angle fractures: A 10-year retrospective. J Oral Maxillofac Surg 2010, 68, 647–650. [Google Scholar] [CrossRef]
- Maloney, P.L.; Lincoln, R.E.; Coyne, C.P. A protocol for the management of compound mandibular fractures based on the time from injury to treatment. J Oral Maxillofac Surg 2001, 59, 879–884, discussion 885–886. [Google Scholar] [CrossRef]
- Webb, L.S.; Makhijani, S.; Khanna, M.; et al. A comparison of outcomes between immediate and delayed repair of mandibular fractures. Can J Plast Surg 2009, 17, 124–126. [Google Scholar] [CrossRef]
- Maloney, P.L.; Welch, T.B.; Doku, H.C. Early immobilization of mandibular fractures: A retrospective study. J Oral Maxillofac Surg 1991, 49, 698–702, discussion 702–703. [Google Scholar] [CrossRef] [PubMed]
- Biller, J.A.; Pletcher, S.D.; Goldberg, A.N.; Murr, A.H. Complications and the time to repair of mandible fractures. Laryngoscope 2005, 115, 769–772. [Google Scholar] [PubMed]
- Serena-Gómez, E.; Passeri, L.A. Complications of mandible fractures related to substance abuse. J Oral Maxillofac Surg 2008, 66, 2028–2034. [Google Scholar] [PubMed]
- Choi, B.H.; Kim, K.N.; Kang, H.S. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995, 79, 692–695. [Google Scholar]
 |
 |
© 2016 by the author. The Author(s) 2016.
Share and Cite
Spinelli, G.; Lazzeri, D.; Arcuri, F.; Valente, D.; Agostini, T. Management of Mandibular Angle Fractures by Two Conventional 2.0-mm Miniplates: A Retrospective Study of 389 Patients. Craniomaxillofac. Trauma Reconstr. 2016, 9, 206-210. https://doi.org/10.1055/s-0036-1582457
Spinelli G, Lazzeri D, Arcuri F, Valente D, Agostini T. Management of Mandibular Angle Fractures by Two Conventional 2.0-mm Miniplates: A Retrospective Study of 389 Patients. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(3):206-210. https://doi.org/10.1055/s-0036-1582457
Chicago/Turabian StyleSpinelli, Giuseppe, Davide Lazzeri, Francesco Arcuri, Domenico Valente, and Tommaso Agostini. 2016. "Management of Mandibular Angle Fractures by Two Conventional 2.0-mm Miniplates: A Retrospective Study of 389 Patients" Craniomaxillofacial Trauma & Reconstruction 9, no. 3: 206-210. https://doi.org/10.1055/s-0036-1582457
APA StyleSpinelli, G., Lazzeri, D., Arcuri, F., Valente, D., & Agostini, T. (2016). Management of Mandibular Angle Fractures by Two Conventional 2.0-mm Miniplates: A Retrospective Study of 389 Patients. Craniomaxillofacial Trauma & Reconstruction, 9(3), 206-210. https://doi.org/10.1055/s-0036-1582457



