From 2002 to 2006, more than 117,000 facial fractures were recorded in the U.S. National Trauma Database. The use of rigid internal fixation is part of the standard of care for various fractures following maxillofacial trauma. Anatomic reduction and rigid fixation offers pain relief and early functional recovery. Fixation may be achieved with the use of a variety of available techniques and fixation systems. The majority of the components are titanium and are designed for permanent implantation. However, the use of internal hardware is not without disadvantages. The literature shows that complications are not rare [
1,
2]. Many of the complications that follow internal fixation of facial fractures require a second operation, thereby increasing morbidity, discomfort, and cost.
This study is designed to examine complications from internal fixation of facial fractures, and to address the need for prospective trials in regard to treatment because of the lack of empirical data available for surgeons faced with these clinical situations. An extensive literature review revealed that no studies directly address this issue. Prospective data regarding the fate of operative complications following maxillofacial trauma are scarce, if not absent. The use of well-vascularized tissue has been shown to increase the salvage rate of exposed hardware in other anatomic locations [
3]. Perhaps the robust blood supply to the facial soft tissues allows for conservative management and bone healing to take place despite the presence of a complication. However, this remains to be seen in the literature. Indications for salvage versus removal of maxillofacial hardware before bony union are not well defined, and there is no standardization of data reporting. The present study was performed to identify the missing data needed to decide upon instances when hardware may be salvaged. The acquisition of such data can contribute toward the creation of a paradigm in algorithm form that uses empirical evidence to determine optimal treatment for patients who experience complications from internal hardware fixture.
Methods
An extensive review of the English-language literature from 1978 to August 2014 was conducted using the PubMed and Web of Science search engines using keywords maxillofacial trauma and hardware complications or indications for hardware removal to determine factors important in complications after hardware use following maxillofacial trauma. Only human studies were included and the search was supplemented by cross-checking all references in each article to identify additional articles relevant to the topic. The search was conducted independently by two investigators. Review and survey articles were excluded.
The inclusion criteria for each article are as follows: (1) electronically available on the MEDLINE database, (2) referred to maxillofacial trauma patients only, (3) addressed specifically internal hardware placement, and (4) gave information regarding complications, removal of hardware, or both. The term maxillofacial trauma includes trauma to the upper face, midface, and mandible. The term upper face includes frontal bone, frontal sinus, and frontonasal suture. The term midface includes zygoma, zygomatic buttress, zygomatic arch, zygomatic-orbital, anterior wall of antrum, orbit, infraorbital rim, piriform region, nose, frontozygomatic suture, nasal, palate, maxilla, nasoethmoidal-orbital, Le Fort I, II, and III, and malar. The term mandible included angle, ramus, condyle, body, symphysis, external oblique line, mental area, and parasymphysis.
Hard copies of all articles that met the inclusion criteria were acquired, and data extraction was performed independently by two investigators using standardized forms. Information that was retrieved from each article included total number of patients, plates or fractures (due to inconsistency in the literature), follow-up period, mean age, type of trauma (i.e., motor vehicle accident, assault, fall, etc.), total complications, type of complication (i.e., infection, hardware exposure, pain, etc.), location of complications (i.e., mandible, midface, upper-face), treatment (when available), and need for hardware removal. Complications were combined into the following groupings: pain (including somatosensory complications), exposure (including exposure of hardware or wound dehiscence), deformity (including resulting deformities, malunion, and palpability of hardware), failure (including loose or broken hardware), infection, nonunion, or other. From the extracted data, complication rates based on the mechanism and anatomic location of the injury were tabulated. These were analyzed with the overall goal of identifying parameters with prognostic relevance for management of hardware-related complications.
Results
Fifteen articles were included. No clinical trial that compared removal and salvage written retrospectively or prospectively was identified. Complication data were presented by patient, fracture, and/or plate without consistency. The data described 1075 fractures, 2961 patients, and 2592 plates, nonexclusive. Complication rates varied from 6 to 8% by fracture, and 6 to 11% by patient.
Most articles described only postoperative complications treated with removal. Two articles included patients treated with either removal or salvage without describing how the choices were made [
1,
2]. When their data were assessed, 50% of complications were treated with plate removal including 46% of complications in the mandible, 50% in the midface, and 50% in the upper face.
Six studies provided a mean age of patients receiving plates (
Table 1) [
4,
5,
6,
7,
8,
9]. The overall mean age was 30.5 years (range: 22–44). Two studies provided the distribution of causes of initial injury (
Table 2) [
4,
9]. The majority of injuries were caused by assault (overall: 64%, range: 61–70%), followed by motor vehicle accidents (overall: 21%, range: 2– 33%), sports (overall: 8%, range: 0–20%), falls (overall: 6%, range: 4–8%), and gunshot wounds (overall: 2%, range: 0–3%).
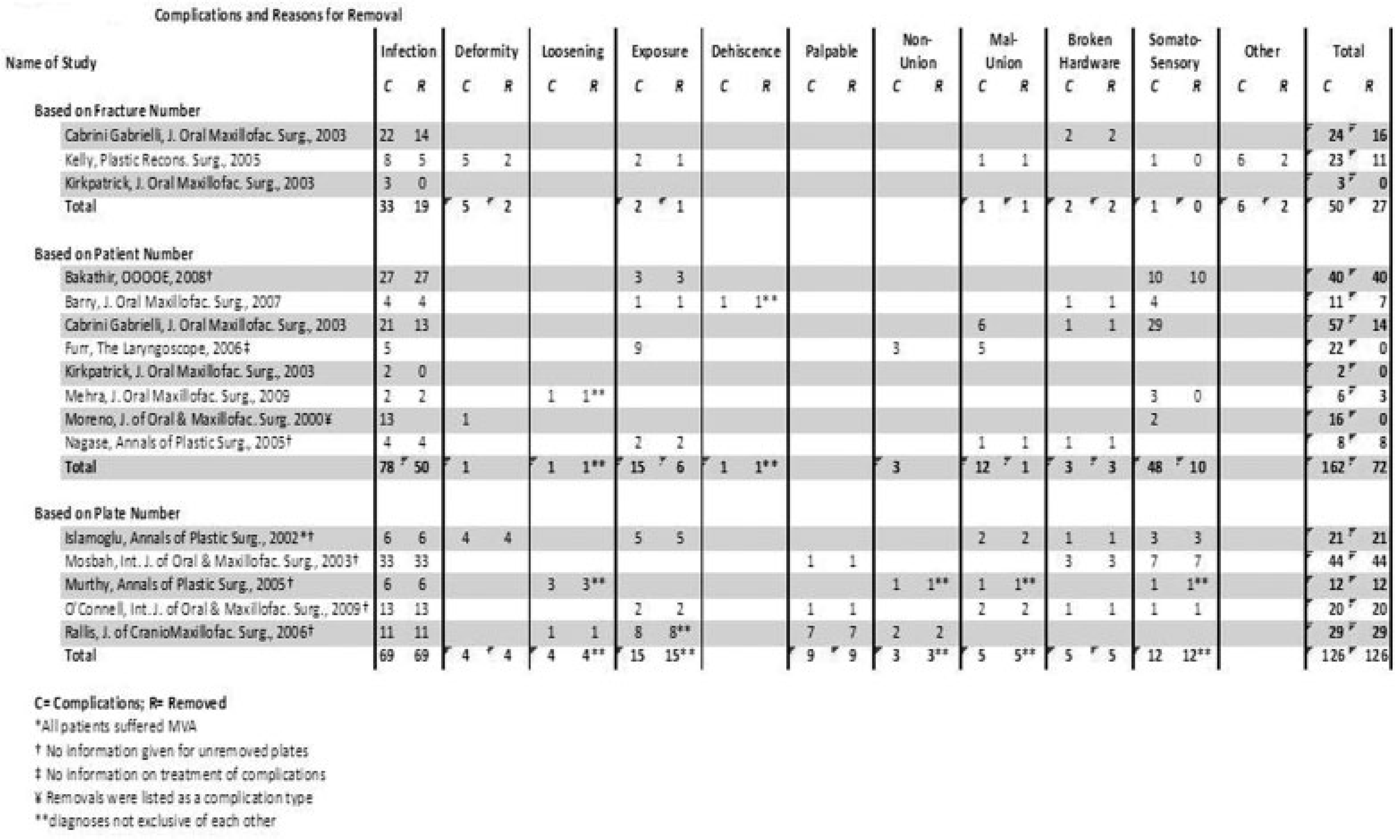
Fourteen studies provided detailed data on complications and removals seen in patients treated by fixation with plates (
Figure 1) [
1,
2,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15]. Data were provided by fracture, patient, and plate, and these data were compiled into complication groupings (
Table 3). These data were not exclusive as some studies provided data in more than one way. The categories of complications were also not exclusive. For instance, some patients presented with more than one complication including infection, exposure, loosening, and broken hardware. Infection was the only complication seen in all 14 studies and was the most common reason for removal when looking at all three categories (68, 34, and 46%, respectively). Other reasons for plate removal varied by study and whether the data were reported by fracture, patient, or plate. Complications such as loosening, nonunion, broken hardware, and severe/prolonged pain were uniformly treated with removal. Some complications caused by exposures, deformities, and infections were treated with salvage. Of the salvaged plates, exposed plates were treated with flaps, plates with deformities were treated with secondary procedures, and plates with infections were treated with antibiotics alone, antibiotics and soft tissue debridement, or antibiotics and tooth extraction.
Three studies provided data on overall complication rates and removal rates (
Table 4) [
1,
2,
11]. When reported by fracture, the overall incidence of plate complication was 7.6 (range: 6.4–7.8%), and by patient, the overall percentage with complication was 10.3 (range: 5.9–11.2%). Removal rate, when calculated by fracture, ranged from 0 to 3.7%. Rate of removal of complications reported by fracture ranged from 0 to 47.8%.
Three studies provided data on the complication and removal rates by location (
Table 5) [
1,
2,
11]. When reported by fracture location, the complication rates were similar among the mandible, midface, and upper face groups (8.6, 5.8, and 13.33%, respectively); the data for the latter two groups were provided by a single study. Removal rates by fracture were also found to be similar among the three groups (3.2, 2.9, and 6.67%, respectively). Rate of removal of complications was found to near 50% in all three locations.
Discussion
The overall outcome of the treatment of facial fractures has improved with advances in surgical technique, as well as plating technology. The current standard of care for the management of maxillofacial trauma involves early anatomic reduction with rigid internal fixation. This is most often accomplished by a combination of miniplates and screws. Greater understanding of the physiology of bone healing and the biomechanics of rigid fixation has allowed for the development of plating systems that are designed to be permanent load-bearing or load-sharing implants. The majority of the literature has focused on surgical technique or indications for device implantation. There is a paucity of literature investigating management of complications involving maxillofacial hardware. Our investigation shows that overall 50% of reported hardware complications ultimately result in hardware removal. The key clinical question becomes how to manage hardware complications when the plates need to remain in situ.
Initial proponents of maxillofacial fracture plating, including Champy et al., Alpert and Seligson, and Cawood, recommended routine removal of the hardware after 3 months of insertion [
15,
16,
17,
18]. Presumably, this was meant to avoid potential complications associated with prosthetic implants. Once bony union is achieved at an average of 4 to 6 weeks, the hardware becomes obsolete. Also, the original miniplates were made from stainless steel, which is less durable and more reactive than the current standard of titanium. Currently, there exists no consensus on the need for routine removal of titanium maxillofacial plates; however, most authors agree that there is less risk in leaving asymptomatic plates in place compared with removing them [
15,
19].
Most studies examining complications with maxillofacial hardware are retrospective and focus on epidemiology, timing, and risk factor identification. The treatment of these complications and eventual outcomes are often not reported, underreported, or not reported in a uniform manner between studies. Moreover, there is no uniform way in which the data are organized, which makes interpretation difficult. For example, the incidence of plate removal in the literature ranges from 5 to 40%, with most studies reporting numbers around 10% [
9,
15,
19]. This is partially due to small numbers within each study, but differences in whether the data are given in terms of fractures, patients, or plates plays a role in the difficulty of interpretation.
Complications following the repair of facial fractures depend on fracture location, injury severity, and various patient factors such as alcohol and tobacco use [
9,
11]. The most common indications for maxillofacial hardware removal in the literature are infection and/or hardware extrusion or exposure. Murthy and Lehman reported that most infections after maxillofacial trauma occur in the mandible, and that these infections are the main cause of plate removal [
9].
Two key issues associated with the management of hardware complications are timing and the morbidity associated with hardware removal. As previously stated, consensus opinion among surgeons is that the risks of removal of asymptomatic hardware outweigh the benefits [
9,
12,
13]. This is true in nearly all cases of internal fixation regardless of anatomic location.
More data are available for the management of hardware complications and hardware exposure in lower extremity injuries [
3]. Hardware for internal fixation of orthopedic injuries has been used for much longer than in maxillofacial trauma. In addition, the consequences of hardware failure in the lower extremity are severe and can include amputation. It has become evident that the delicate softtissue envelope of the lower extremity demands timely intervention and ultimately dictates success of the treatment. A meta-analysis of lower extremity trauma by Viol et al. identified several parameters with prognostic value for the salvage of exposed orthopedic hardware [
3]. These include location in the lower extremity, superficial infection or negative wound cultures, duration of infection less than 2 weeks, hardware exposure less than 3 weeks, and absence of hardware loosening.
The timing and nature of the hardware complication is central to the need for, and feasibility of, hardware salvage in the maxillofacial skeleton. Any infection, exposure, pain, or other morbidity that presents itself after bony union should be treated by hardware removal. A majority of the plate removal in the literature occurred within 6 months to 1 year of hardware placement [
6,
9,
15,
19]. Few studies reported plate removal at less than 3 months; however, actual time of diagnosis of the potential problem or any intervention taking place prior to ultimate hardware removal, such as antibiotics or irrigation and debridement, was not reported either. Mechanical hardware failure was generally treated with replacement by more rigid fixation and bone grafting.
The purpose of this study is to identify those specific factors associated with complications of maxillofacial hardware and indications for hardware salvage. No data on the salvage of infected or exposed maxillofacial hardware are currently available in the literature. This study identifies a void in our understanding of facial trauma surgery. There is a need for more examination and better reporting of the management of maxillofacial hardware complications early in postoperative course before bony union has occurred. Based on the senior author’s (P.T.) clinical experience, we have constructed a management algorithm for maxillofacial hardware complications broken down by etiology (
Figure 2).
The algorithm examines hardware complications broken down by etiology because the clinical decision making is guided by the underlying diagnosis. The surgeon must first determine clinically or radiographically if bony union has occurred. The management of all hardware complications that happen after bony union involves hardware removal along with other adjunctive measures specifically related to each mechanism. If bony union has not occurred, the salvage arm of the algorithm is followed. The setting of infection is further subdivided by depth or source of the infectious process. When the infection does not involve underlying bone, the existing plates can generally be salvaged by antibiotics, irrigation, and debridement of the nidus, such as a necrotic tooth or soft tissue. The algorithm provides a logical framework for surgeons to approach maxillofacial hardware complications.
Conclusions
Contrary to classical teaching, some postoperative complications caused by exposure, deformity, and/or infection may be successfully treated with plate salvage, but empirical data that designate which circumstances permit this are scarce. Well-designed clinical trials evaluating hardware removal versus salvage are lacking. Further studies need to be undertaken that examine the outcome of the treatment for these complications. Multiple studies detailed the complications following facial plate insertion, but no studies were found that followed the outcomes after the second medical or surgical intervention. To address the issue of inconsistent methods of data reporting, it is suggested that authors report their findings by anatomic location of fractures to allow for differences in technique. It is proposed that a national databank be created where surgeons can compile their patient information and examine it in a standardized format to further our understanding of clinical management.