Osteogenesis imperfecta (OI) is a congenital disease characterized by bone fragility and low bone mass. Despite the variety of its manifestation and severity, fractures of the maxillofacial lesion occur very infrequently.
Here, we report a case of an infant diagnosed with OI after mandibular and lower limb fractures.
Case Report
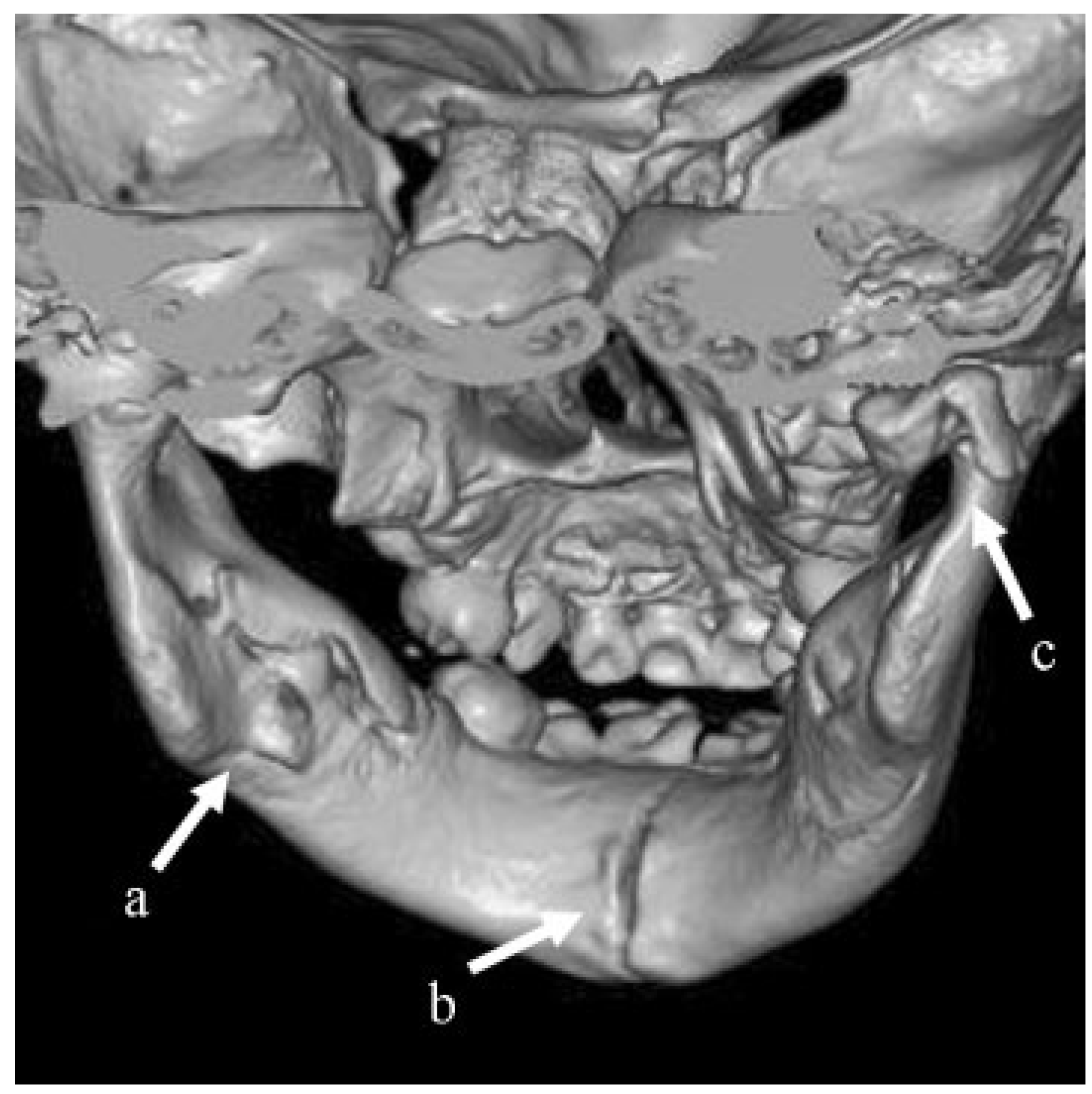
A boy aged 1 year and 3 months was brought to the emergency outpatient service of his neighboring hospital with a complaint of facial injury caused by falling from a baby carriage. He did not receive any treatment following the emergency physician’s assessment and returned home on the same day. Two days after the injury, he and his family visited the division of oral and maxillofacial surgery in the hospital. He was admitted the hospital on the same day, and a computed tomography (CT) scan was performed under sedation. CT images revealed multiple mandibular fractures: green-stick fracture in the left angle, complete fracture in the symphysis, and dislocated condylar fracture on the right side (
Figure 1). Operation for the body fracture was planned; however, because of complication of bronchitis, the anesthesiologists decided that it was unsafe to perform general anesthesia.
The infant was transferred to undergo operation to our hospital, which can provide pediatric perioperative management 3 days after the injury. We found trismus, difficulty in feeding, runny nose, and coughing. Although concrescent of lower left deciduous incisor teeth was found, other malformation of teeth, including dentinogenesis imperfecta, was not detected.
Because of the impossibility of oral ingestion, we inserted a nasogastric tube to start tube feeding. The pediatrician started preoperative care with the administration of antibiotics and inhalant. Because trismus and mobility of fractured segments remained, we performed open reduction and internal fixation (ORIF) under general anesthesia 7 days after the injury.
Via the transcutaneous approach, internal fixation with absorbable plate and screws was performed. This approach was selected with reference to preoperative CT images to avoid damaging the dental germs of permanent teeth. From a 2-cm-long submental skin incision, the inferior border of the mandible, including the fracture line, was exposed. Although callus was observed between the fractured ends, mobility of the segments remained. The segments were fixed with absorbable implants: a four-hole mini plate and two screws (5-mm long). We chose conservative treatment for the left angle and right condyle. The postoperative course was favorable, and he started oral ingestion after 2 days and left hospital 7 days after the surgery. Because he was unable to understand our instructions as a result of his age, we permitted early oral feeding as postoperative rehabilitation.
Two months later, he suffered a fall at home and fractured his right lower limb, which was treated at the neighboring orthopedic clinic. Following this, his mother requested us to investigate whether his injury was because of a bone metabolism disorder. We consulted the orthopedic division at our hospital and reported these accidents to the child consultation center considering the possibility of abuse. Later, the apprehension of abuse was denied. On examination by the orthopedist, blue sclera of this patient was indicated. Some family history was declared: blue scleras were also detected in his mother, maternal grand-mother, and grandaunt who has bone metabolism disorder. In addition, his mother had experienced multiple fractures because of a slight tumble in her youth. All of them were diagnosed as having OI type IA. The patient has received periodical medical examination by an orthopedist and will be administered bone-modifying agents, such as bisphosphonate, if he suffers from frequent fractures accompanied with increasing daily activity.
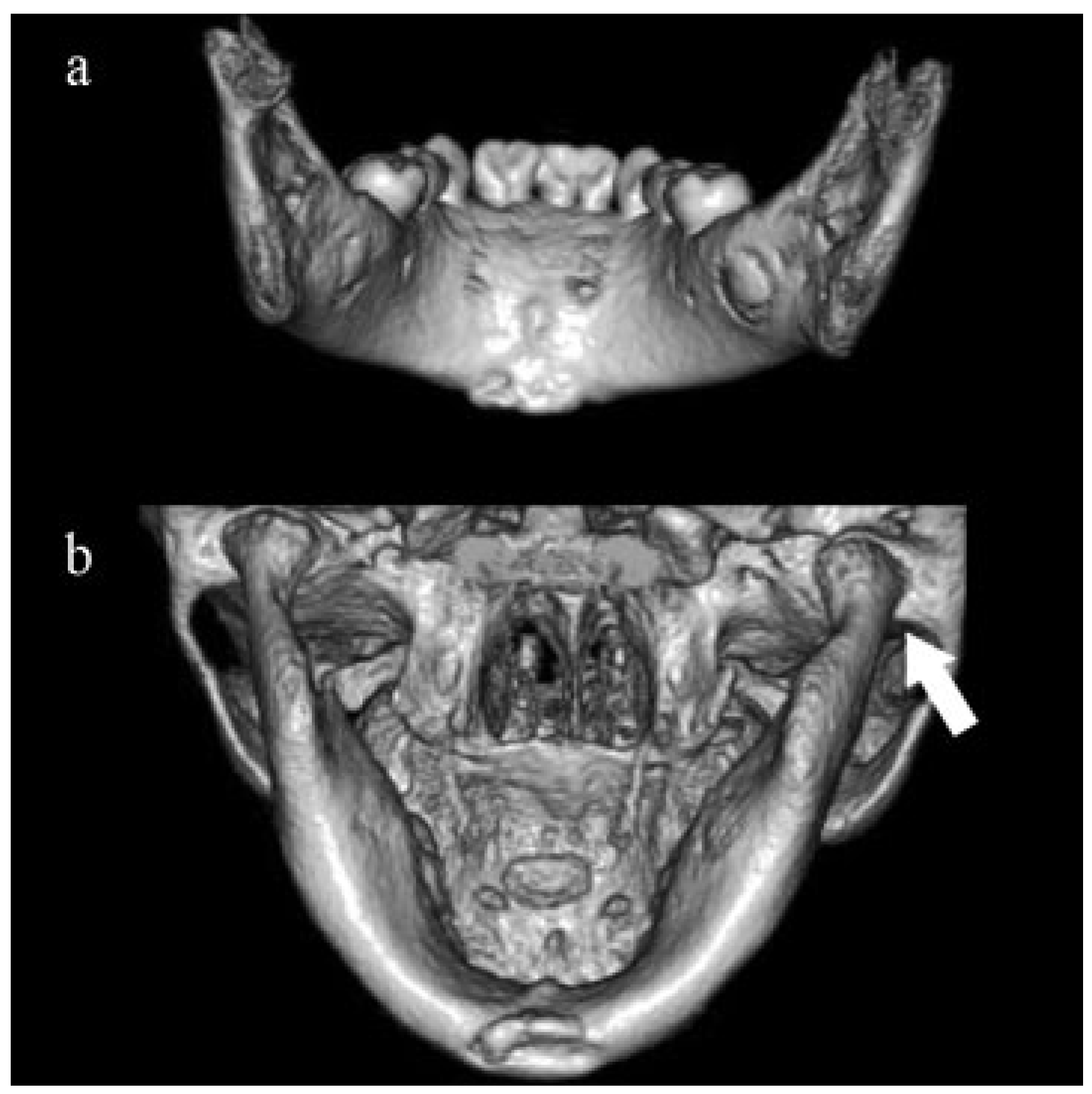
The clinical course was good; hinge movement of the mandible and interocclusion were normal at 1-month post-operative examination. In 1-year postoperative CT images, although plate and screws were remaining, bone reunion and reposition of the right condylar head were observed without temporomandibular joint ankylosis (
Figure 2). We will continue follow-up until the eruption of central incisors, which could be affected by surgical stress.
Discussion
OI is a congenital disease mostly caused by alterations in the metabolism of type I collagen, which is a constituent of the connective tissue. With regard to the disease type or severity, various manifestations are observed such as bone fragility, bone deformities, blue sclera, dentinogenesis imperfecta, hearing impairment, hyperlaxity of ligaments and skin, spinal curvature, short stature, and mental retarda tion.[
1,
2] Its overall incidence ranges from 1:5,000 to 1:20,000 live births, with no racial or ethnic predilections.[
1] Severity varies widely, ranging from intrauterine fractures and perinatal lethality to very mild forms without fractures. The most common classification, type I to IV, proposed by Sillence et al.[
3] reflects severity and is effective for diagnosis. These four types have a mutation in one of the two genes that encode the α chains of collagen type 1 (COL1A1 and COL1A2).[
4] Nowadays, types V through VIII without the collagen type 1 mutation have been identified.[
2,
5] Heredity follows an autosomal-dominant pattern in types I through V, and it is autosomal recessive in types VI through VIII.
In the past, the pivotal treatment for patients with OI has been physiotherapy, rehabilitation, and orthopedic surgery. However, cyclical intravenous pamidronate treatment for children and adolescents with severe OI is actively used after the report by Glorieux et al. in 1998.[
6] Decreasing the activity of osteoclast results in the therapeutic benefit of reduced bone pain, increased bone mineral density, corrected bone deformation, and increased bone strength. Since then, several groups have reported on applying pharmacotherapy generally used for osteoporosis, for example, alendronate, zoledronate, teriparatide, and denosumab. The introduction of these types of bone-modifying agents requires close attention, because they could cause side effects such as osteonecrosis of the jaws or drug-induced osteopetrosis.
Although OI type I, which was observed in this case, is the most frequent, its symptoms are generally milder than those of other types, and many patients of this type may live with no fractures. However, fractures occurring in the maxillofacial lesion are very rare in all types of OI, and only two cases were reported as per our knowledge. Gallego et al.[
7] reported a case of an adult male with OI type I who had been treated with alendronate and underwent ORIF for mandibular body fracture, resulting in successful treatment without osteonecrosis or delayed healing. Feifel[
8] reported a case of treatment of a mandibular fracture, including bilateral subcondylar fractures, in an 8-year-old child with OI type IV B using microplate and postoperative orovestibular plates with springs.
Haug and Foss[
9] mentioned that estimates regarding the incidence of pediatric facial fractures range between 0.87 and 1% for victims of injury under the age of 5. They also noted that the most frequently encountered pediatric facial fracture is that of the mandible (15–86.7%), followed by the midface (8–54%) and upper face (12–45%). The condyle is the most common site of mandibular fractures in pediatric patients, followed by the symphysis.[
10] Pediatric patients often sustain either a minimally displaced fracture or a green-stick fracture of the mandible because of the greater elasticity of the mandible and the presence of developing tooth buds.[
11]
For a long time, it has been said that the most common strategy for children’s mandibular fractures is closed reduction with circumferential wiring. Of course, although the superiority of this method for incomplete or nondisplaced fractures is universal, many surgeons have mentioned that ORIF is desirable to achieve reliable stability for displaced fractures. Because there is a fear of influences upon the potential growth and teeth disturbances and difficulty in secondary removal if needed, absorbable implants have the advantages of rigid metal fixation.[
12] We think that our choice of using absorbable implants for this case was correct. We should consider the combination of circumferential wiring because the subcondylar fracture was accompanied with this case. However, we succeeded in minimizing the invasion because postoperative jaw movement was smooth and the condylar head was replaced. As mentioned in many reviews, observation without surgical treatment for green-stick fracture in the mandibular body and minimally displaced condylar fracture should be considered to avoid growth restriction.[
9,
10] We decided on open reduction for the left angle and right condyle of the mandible because long-time general anesthesia would not benefit in this case with complicated bronchitis.
We consulted an orthopedist regarding the lower limb fracture and reported to a child consultation center considering the possibility of abuse. Abuse must be taken into account as a possibility of the cause of child injury. Well-trained oral and maxillofacial surgeons can provide valuable information about oral and facial aspects of child abuse to other physicians.[
13] In addition, although blue sclera is not a common finding for oral and maxillofacial surgeons, it is characteristic and suggestive.
Conclusions
We report a case of OI, which was diagnosed after mandibular and lower limb fractures. Although the manifestation or severity varies, we think that OI should be considered as a risk factor of fracture in a maxillofacial lesion. Oral and maxillofacial surgeons should suspect the relationship with a systemic disorder in the treatment of multiple mandibular fractures in infants.
Note
The authors declare that they have no financial or personal relationships with other people or organizations that could inappropriately influence their work. This study did not receive support from any research grants or any other sources.