Reconstruction of skeletal defects is crucial in modern maxillofacial surgery. Commonly these defects are results of radicalism of ablative surgery and might be associated with significant impact on anatomy, function, and esthetics, which provoke deterioration of overall quality of life (QoL) of the patient. Nevertheless, the most difficult task in the facial reconstruction is the reconstruction of the frontal part of the mandible because of its convex–concave anatomy and specific impact of mandible on function and esthetics of the whole face. Various flaps and techniques are available for the reconstruction of subtotal defects of the mandible, including free fibula, iliac crest, etc. [
1]. Yet free fibula seems to be work horse for mandibular reconstruction. The key point of this procedure is an adequate restoration of anatomy of resected region by means of rigid fixation and correct adaptation of plates and bone as well as creation of the best suitable background for the further prosthodontic rehabilitation [
2]. Commonly prosthodontic rehabilitation requires performing several subsequent steps in a systematic manner which lasts over 1 year. Within this period, patient is out of normal nutrition, speech, and esthetics, thereby normal life. Moreover, deformation of adjacent soft tissues may occur; this makes further prosthodontic manipulations even more difficult. We found recent articles concerning acceleration of these procedures, such as prefabrication and osteotomy of free flap prior to transfer and perineal artery transection [
3], insertion of dental implants prior to free flap transfer [
1], insertion of the dental implants immediately after transfer with further period of integration [
4], and primary reconstruction of the mandible with immediate dental implants placement and prosthodontics rehabilitation in 1 day [
5]. The aim of this study was to improve outcomes of reconstruction of postablative defects of mandible and its prosthodontic rehabilitation by using preoperative three-dimensional planning and navigation principles without application of medical rapid prototyping (MRP) technology.
Case Report
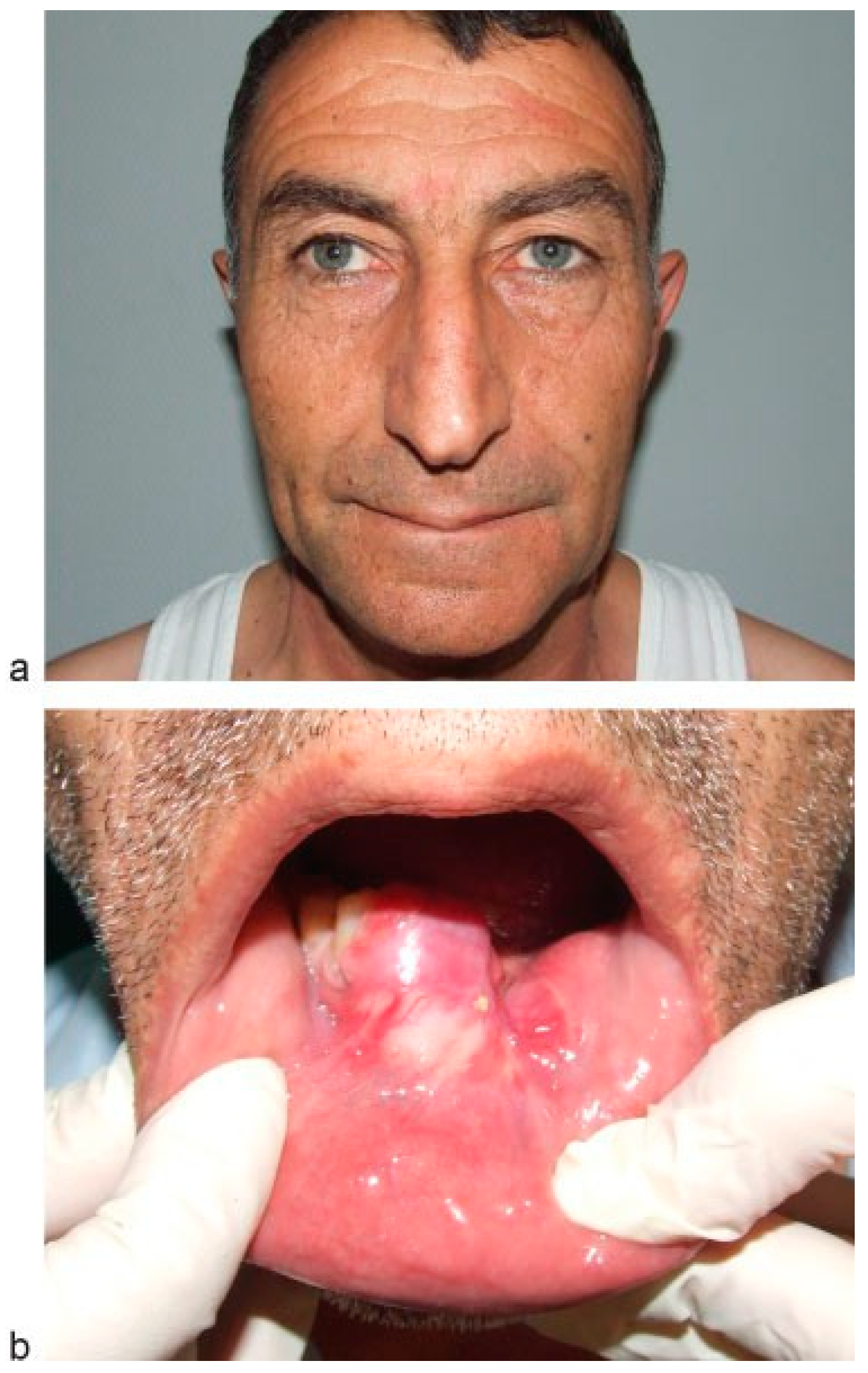
A 56-year-old man presents with complains of lesion in the symphysis of the mandible. Upon anamnesis, first signs of disease noted a year ago after the extraction of the 31st and 32th teeth. The tumor developed within the socket after tooth extraction. The tumor was “excochleated”, and a year later the tumor recurred. Clinically, the tumor was found in the region of alveolar process limited by premolars and spreading to oral mucosa of the floor of the mouth (
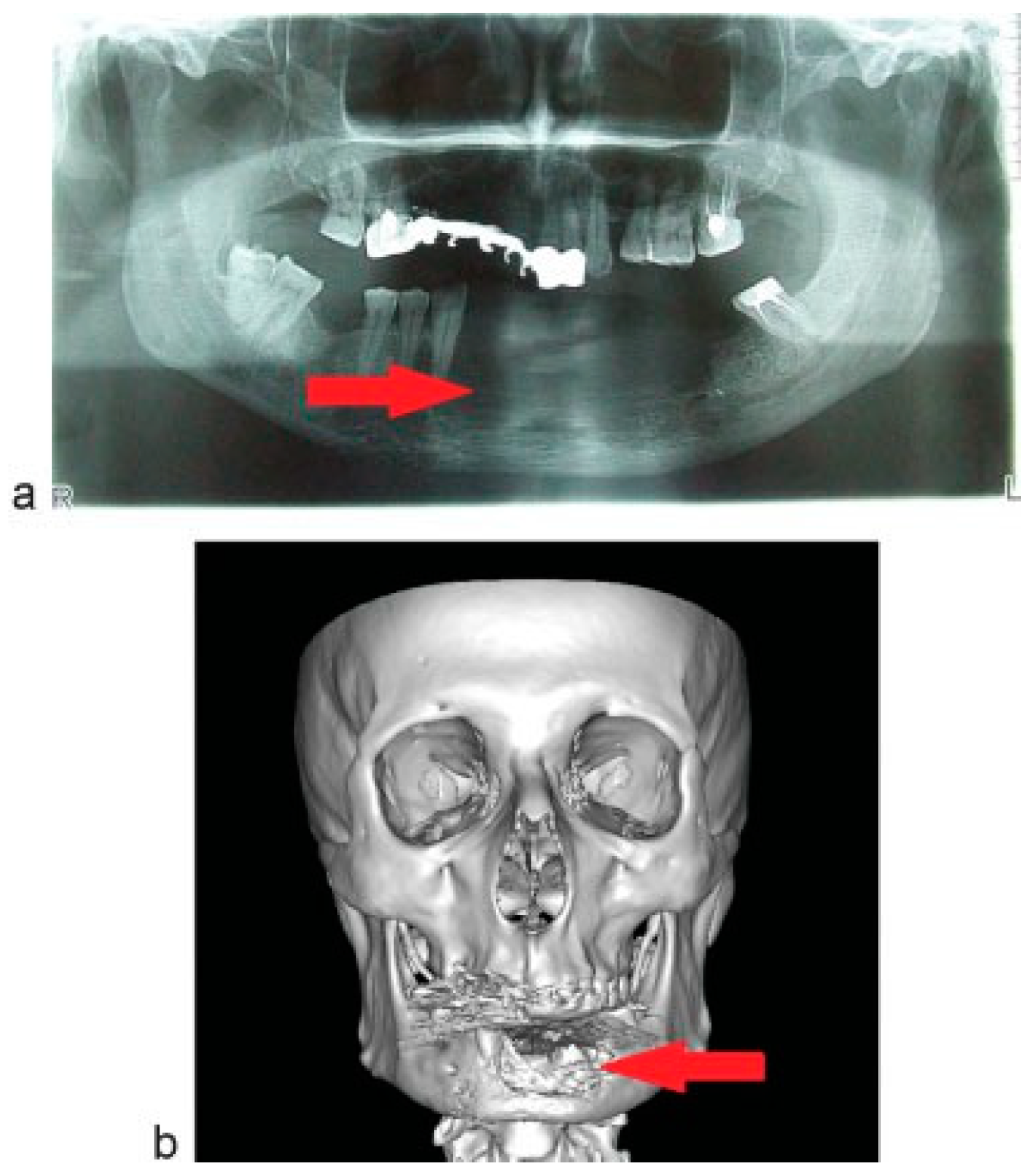
Figure 1a,b). Orthopantomogram (OPG) and computed tomographic (CT) scan showed the area of bone erosion (
Figure 2a,b).
Virtual Planning of Surgical Procedure
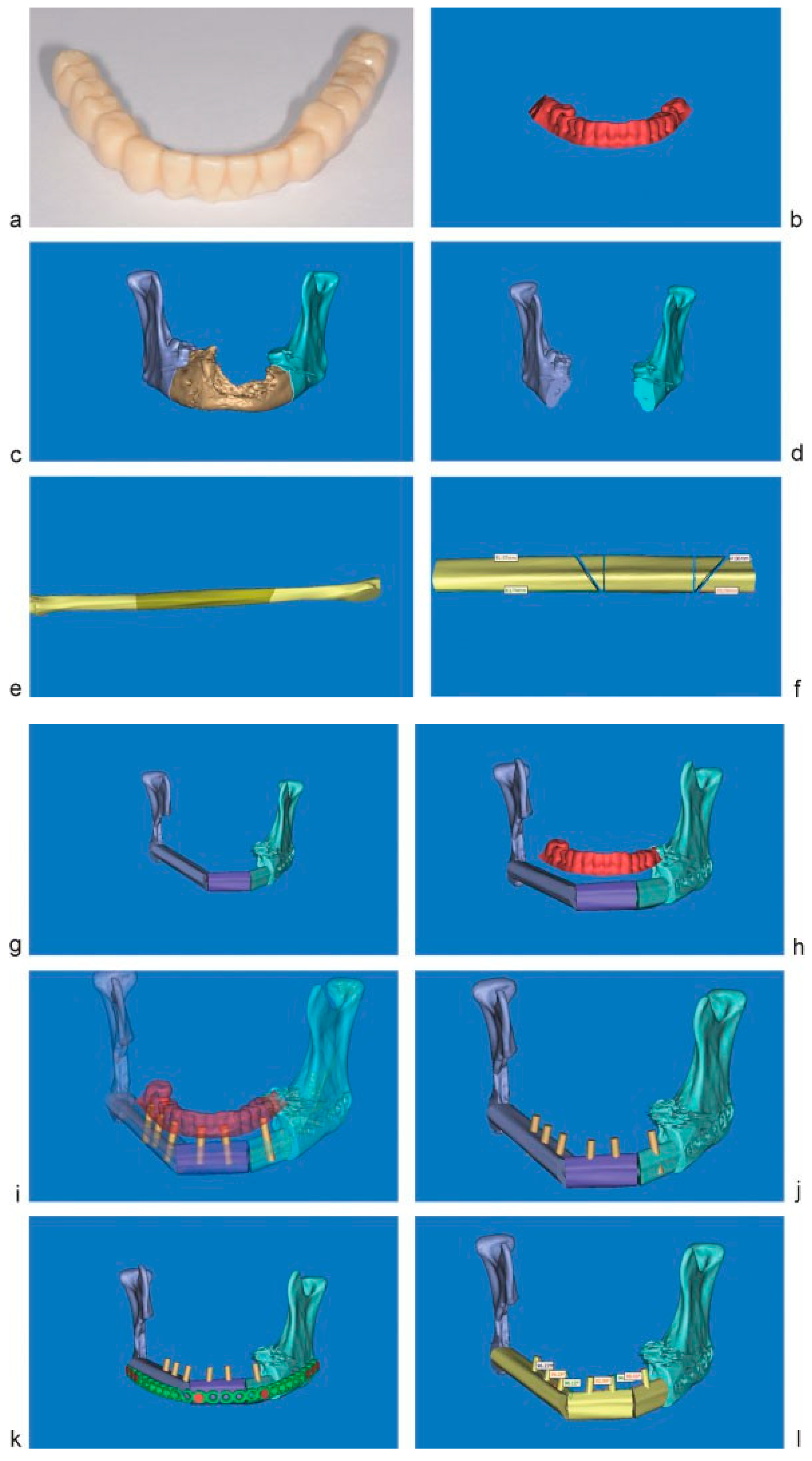
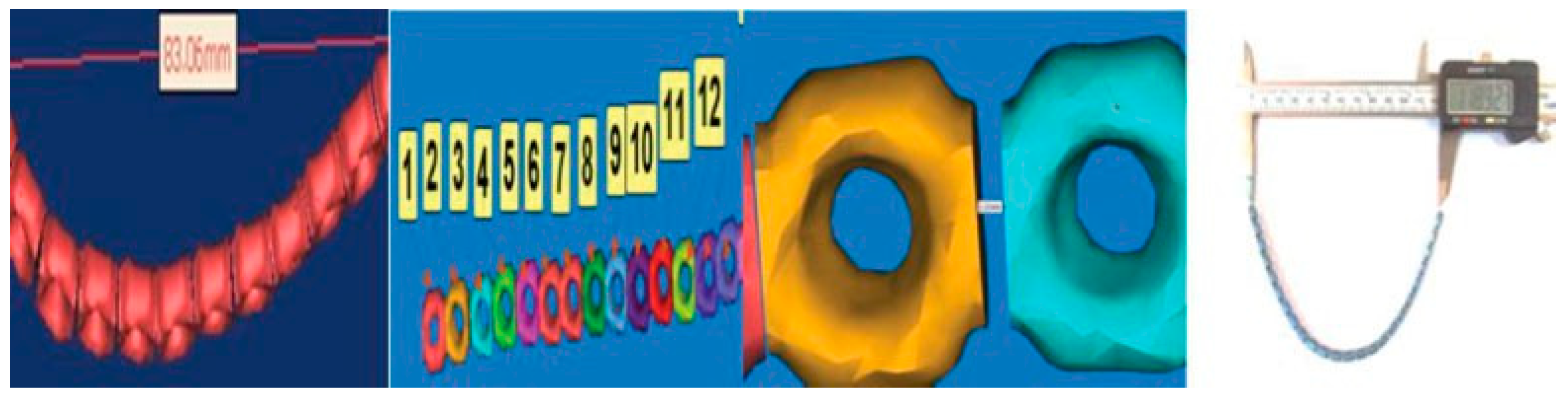
Within preoperative planning, after achieving impression from healthy upper jaw, fixed bridge device for the mandible fabricated from acrylic, fixed to rigid frame and it was scanned on CT scanner (
Figure 3a,b).
By using MIMICS software (Materialise NV, Leuven, Belgium), virtual marking of pathological area and the site of mandibular resection was done (
Figure 3c,d). Then by using the contour of the lower margin of the mandible, virtual prebending of fixing the flap reconstructive plate was done according to protocol of virtual plate bending [
6].
Virtual plate bending. After scanning the straight reconstructive plate (2.7 mm, Conmet, Moscow, Russia), and performing its segmentation according to the holes on the plate, each segment is adapting to the bone surface within healthy and pathological sites—modeling the shape of the plate similar to the shape of the mandibular body before resection.
After virtual jaw resection (
Figure 3d), the donor site on the fibula bone is determined and the osteotomy lines are drawn for further segmentation and adaption to jaw defect.
(
Figure 3e–g). Pre-scanned bridge prosthesis is adapted to the bone graft and by means of its three-dimensional shape and form, the number, and type of dental implants as well as their positioning within graft, is determined. The length, diameter, and angle of positioning of the implant are calculated, as well as volume of soft-tissue compound around the dental implants (
Figure 3h–j). Reconstructive plate is adapted to the bone graft and the sites of the screws are marking out apart to dental implants (
Figure 3k). Finally, virtual measurements of angulation and distance between implants were asses (
Figure 3l).
Technical Step: Fabrication of Navigation Templates
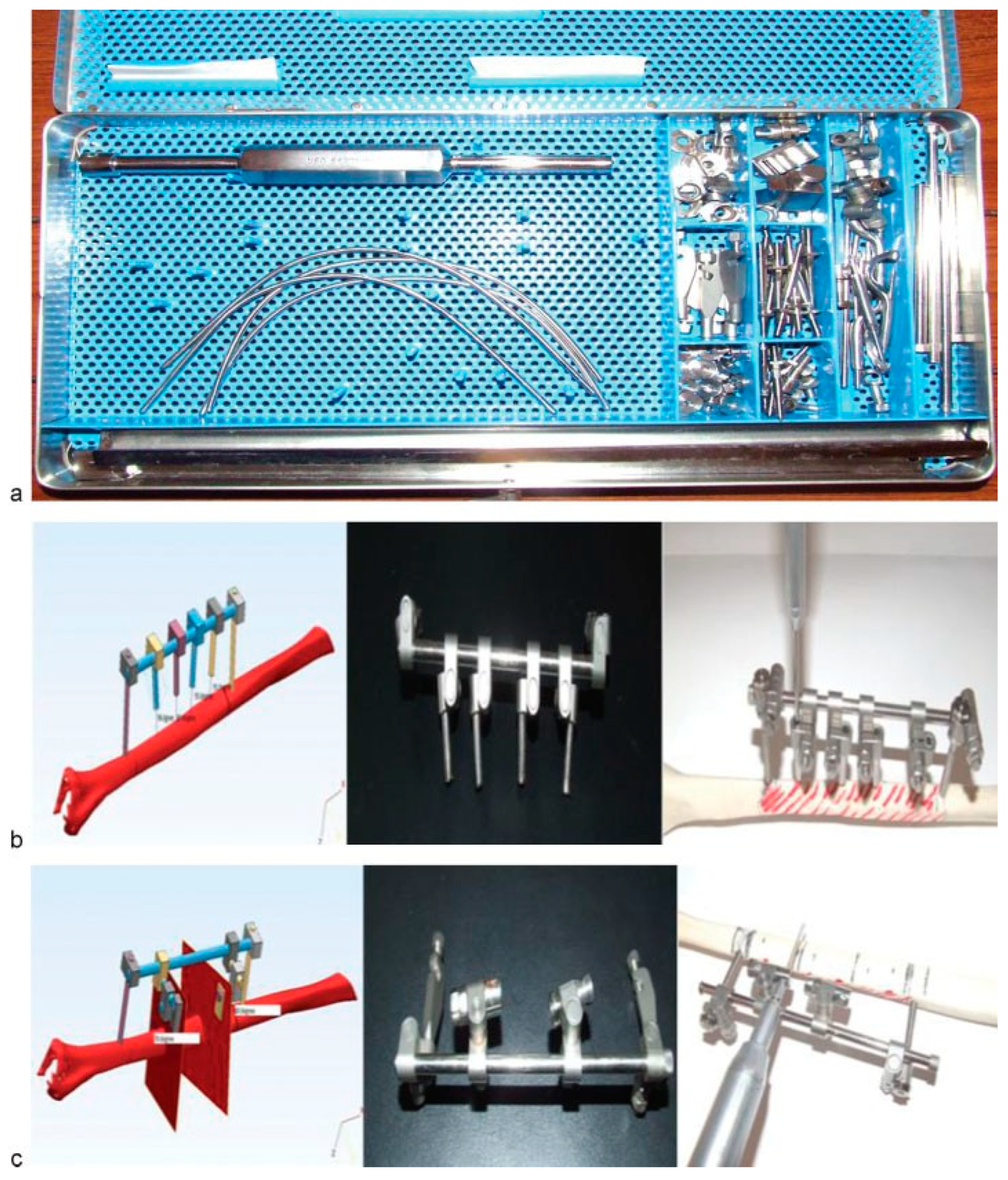
The data of virtual modeling of dental implants insertion and fibula bone osteotomy lines were transferred to navigation templates fabricated from standard tray for external fixation of mandibular fractures (Grimm & Norton, Plainview, NY, USA) (
Figure 4a).
While fabrication of navigation templates for dental implants positioning, we determined virtually the angles of their direction within the bone; adjust the sleeves; directed and then the accuracy of their direction was assess during real simulation on plastic matrix (
Figure 4b). In case of fabrication of navigation template for fibula osteotomy, we also determined the direction of sleeves for the osteotomy and later assessed position accuracy on the plastic matrix during real simulation (
Figure 4c).
Technical Step: Preoperative Prebending of Reconstructive Plate
Transfer of the data of virtual plate bending to reconstructive plate. Preoperative bending of fixing the flap reconstructive plate was done on virtual model and transferred according to the aforementioned method [
6]. After achieving virtual model of the plate, numbering of the segments is done and determined where within segments the plate will bend by performing vertical, horizontal, and axial spindle. All data are imputing to protocol of plate bending and after selecting the standard reconstructive plate with appropriate length and shape (angled or straight), it is bending through segment according to worked out protocol (
Figure 5).
Navigation templates and reconstruction plate are sent for sterilization prior to surgery.
Surgical Step
After performing tracheostomy under intratracheal general anesthesia, transection of the lower lip and continued incision to submandibular area for elevation of labio-buccal flap was done (
Figure 6a). The resection of the mandible was performed within both angels including oral mucosa of the floor of the mouth, so tumor was excised en block (
Figure 6b). Additional neck dissection on the left site with visualization of superior thyroid artery for the further microvascular anastomosis was also performed. At the same time, another team of surgeons exposed fibular bone. The navigation template for dental implants placement was adapted to the fibula bone prior to transection of nutrient vessels. According to the direction of navigation sleeves, six dental implants were positioned within the bone to the whole height of the bone (Alpha Bio, Israel, D ¼ 3.75 mmd, L ¼ 11.5 mm) (
Figure 6c). Navigation template for dental implants was then replaced by navigation template for osteotomy, and the osteotomy of the flap was done by preserving the cortex for further flap bending (
Figure 6d). According to this lines, only cortical plate was osteotomized within places of further flap bending. One was performed in isolation of the fragment of the bone to be transferred with dissection of perineal artery and vein. On the next step, flap forming (with subfracture of cortex) was done according to prebended reconstruction plate and all segments were fixed by screws to the plate (
Figure 6e). After completing this, the donor artery and vein were transected and the flap was introduced to jaw defect and fixed to the rest of the mandible; the anastomoses of the perineal artery and vein were performed with superior thyroid artery and internal jugular vein (
Figure 6f). Thus, the flap’s ischemia time was significantly reduced.
The skin paddle was used to cover dental implants while abutments were placed through cuts within; the wound closure was also done. A great attention was paid to the adaptation of soft tissue around abutments (
Figure 6g).
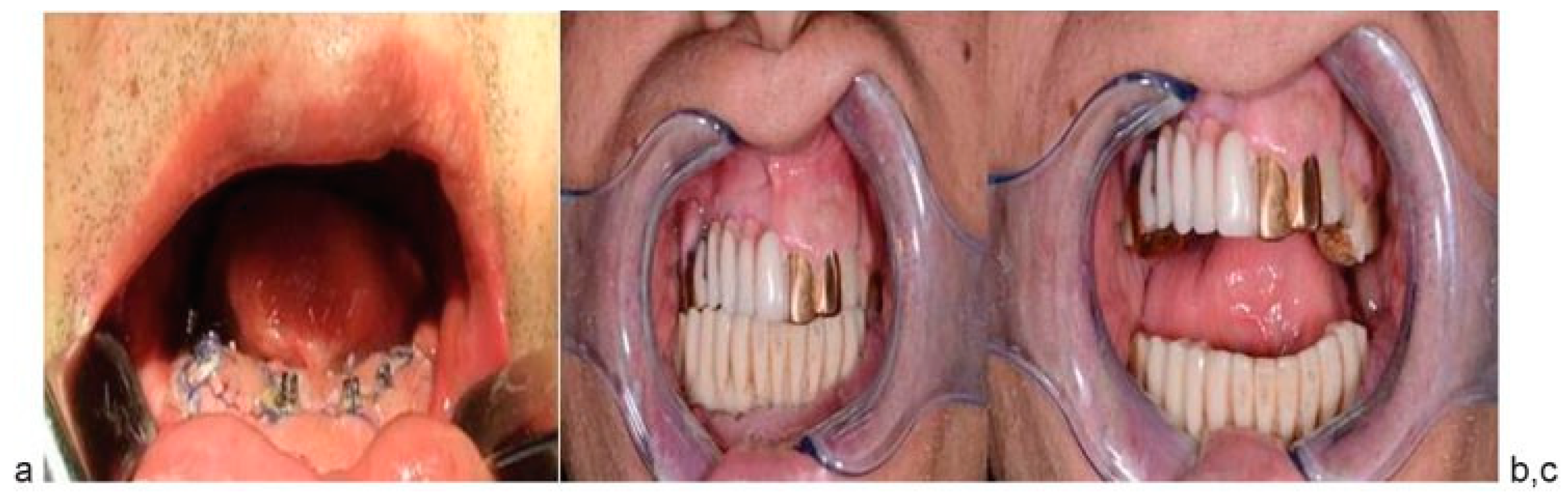
Orthopedic Step
The parallelism of six abutments was cheeked. Sterile and polished temporary bridge prosthesis was fixed on abutments (
Figure 7a). Occlusion and mouth opening were checked (
Figure 7b,c). Adaptation of orthopedic device in one step with surgical intervention allows achieving full value orthopedic rehabilitation in early postoperative period.
Three months later, after checking of osseous integration of dental implants, the final prosthesis was applied to one.
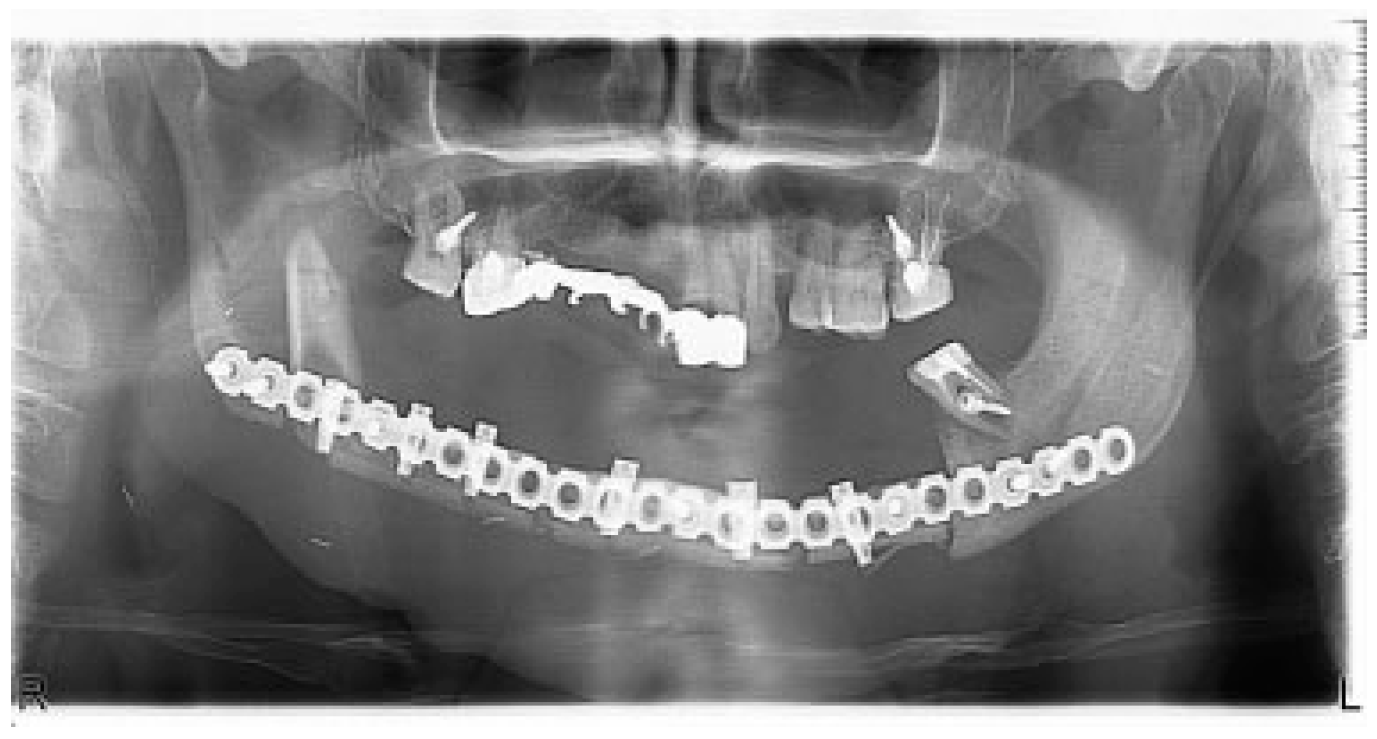
Results
There were no significant complications postoperatively. Postoperative CT and OPG showed bone graft, dental implants, and reconstructive plate to be positioned in accurate anatomical relationship to each other and facial skeleton (
Figure 8). A half year later, reconstructive plate was replaced by titanium miniplates (
Figure 9).
At this stage, the facial appearance with new mandible does not show any significant changes (
Figure 10a,b).
This article shows the application of virtual planning and fabrication of navigation surgical templates in preoperative period, which significantly increases efficiency of reconstructive procedure in case of extensive defect of maxillofacial region and reduces operative time. Elevation of appropriate site of fibular bone, its osteotomy for bending according to the shape of defect, and proper placement of dental implants were done by the help of navigation templates which were achieved with virtual planning and no MRP technology was used. It allows inserting dental implants and osteotomizing the bone prior to transection of nutrient artery, in which intraosseous circulation was not disturbed. Prebended reconstructive plate was used as the template for the determination of exact curvature of the flap, precise localization of condylar heads of the mandible, and facial contours, and its application required minimal time. It accelerated the time of anastomosis for recirculation of the flap in recipient site. The operation time was also reduced, which is important in case of long-lasting surgical procedures.
Intraoperative application of fixed orthopedic device allowed complete restoration of occlusion, mastication, symmetry, and facial esthetic.
The patient who had extensive surgical resection of the mandible because of widespread tumor obtained one-stage total reconstruction of the jaw and dental rehabilitation, which had great impact to overall QoL and speed up recovery time and ability to work.
Discussion
Reconstruction of acquired defects of the facial skeleton is one of the most frequent and complicated tasks within facial reconstructive surgery because of the complexity of structure of the facial skeleton, implying function and the causes of development of these defects and deformities. Although the most frequent cause is traumatism, radicalism of modern ablative surgery introduces a pool of defects with complex anatomy and violated function. Frequently, these defects are associated with compromised speech, meal, and have great impact on facial esthetics and harmony. Taking into account the current concept of importance of the QoL for oncological patients, it becomes more challenging because of numerous tasks that should be solved within reconstruction and rehabilitation of the patient.
Usually reconstruction of postablative defect includes autogenic free flaps and grafts transfer, performing dental implants insertion next to reconstruction and recovery, and prosthodontic rehabilitation after integration of dental implants within bone. It takes approximately 9 to 12 months depending on the adjuvant therapy indicated for total rehabilitation of the patient. On the other hand, the QoL in this period decreases and further deformity and contraction of the adjacent soft tissues may occur. Recently, several articles dedicated to rapid rehabilitation of the patient have been published. The aim of these studies was to accelerate both surgical and prosthodontic reconstruction procedures. Methods such as prefabrication and osteotomy of free flap prior to transfer and perineal artery transection,
3 insertion of dental implants several months prior to free flap transfer,
1 and insertion of the dental implants immediately after free flap transfer with further period of integration were noted [
4]. Yet all procedures require time for integration of bone segments or dental implants in it, which means that it can be used either because of principles of ablation or from the acceleration point of view. Another important factor of successful rehabilitation is success at all steps of reconstruction, which makes free flap mobility, dental implants failure, and prosthodontic device positioning which is critical for the final success. In spite of numerous studies on free flaps design and donor site selection, dental implants placement, and mechanical stress of the bone, there are no data found in the literature regarding dental implants placement prior to flap transfer to reduce ischemia time.
Common adaptation of reconstructive plate, free flap osteotomy, and further dental implants placement is achieving intraoperatively by trial and error method, which makes the outcome unpredictable and depends on multiple stages of reconstruction [
7]. All these require extensive operating time and various steps of treatment.
Today computer-assisted treatment planning allows surgeons and prosthodontists to proceed quick and very precise preoperative planning in comparison with conventional one [
8,
9]. It is very beneficial, because the final decision could be made together with prosthodontist based on the pre-planned surgical procedure. This method gives possibility to create three-dimensional reconstruction not only of certain anatomical structures, such as bones, muscles, or airways, but also of the elements of prosthesis. The three-dimensional data can be analyzed by some software programs such as polygon meshes, where some corrections, depending on the software, can also be done [
10,
11]. Thereby reconstruction of acquired defects in maxillofacial region as well as preoperative planning might be done virtually prior to surgery with the same three-dimensional geometry.
Within this clinical study, it was shown that preoperative virtual planning could significantly improve outcomes of reconstruction and rehabilitation of the patient. The application of combination of virtual planning, virtual bending, and virtual implants insertion protocol, with subsequent osteotomy and implants navigation guides fabrication, can significantly improve postoperative outcomes and accelerate the rehabilitation of the patient. It shows that the application of navigation guides fabricated from the external fixation set considerably reduce operation time and increase the accuracy of dental implants insertion and osteotomy of the fibula free flap. Moreover, the reconstructive titanium plates could be prebent according to virtual bending method prior to surgery with reasonable degree of accuracy, which makes this plate both the element of rigid fixation and the template for the best anatomical shape of neomandible [
6].
This technique gives possibility to reduce significantly surgical time and improve postoperative functional and esthetic result, compared with conventional methods. However, minor corrections could always be done during surgery if some planning errors are found.
Nevertheless, there were no incidences of incorrect contouring, positioning, or osteotomy in this particular case. It is important to note that the virtual planning allows one to determine appropriate length of the plates, screws, and dental implants, as well as future prosthodontic devices in advance, direction and regions where they could be used more effectively. On the other hand, MRP technology and usage of stereolithographic models can also be used for preoperative planning of mandibular reconstruction and prosthodontic rehabilitation [
6,
12,
13,
14]. Surgical templates can be prepared for intraoperative plates bending and bone grafts shaping by using this method. In fact, stereolithography models can be sterilized and used as templates [
15]. However, the cost for MRP manufacturing in our country ranges from approximately 200 to 300€ and it takes some time for fabrication of these models. Moreover, two to three models might be required for such a complex reconstructive procedure. Therefore, it is difficult to use this method in a routine practice. On the contrary, virtual planning requires only several hours to complete virtual reconstruction.
Conclusions
Rapid and successful rehabilitation of the patients with extensive tumors of the maxillofacial area might be achieved by means of detailed preoperative planning supported by virtual computer simulation, including adequate tumor resection, plates prebending, dental implants insertion, and selection of appropriate prosthodontic device. The surgical step includes simultaneous tumor resection, dental implants insertion into free fibula flap by the help of navigation templates prior to flap transfer, further osteotomy, flap transfer, flap forming according to cuts done within bone guided by navigation templates, and rigid fixation within recipient site by means of reconstructive plates. The immediate prosthesis fabricated in advance and supported by dental implants was used to complete the surgical procedure. The application of virtual planning, navigation guides, and immediate dental implants insertion prior to free flap transfer reduces the risk of insertion, while acute ischemia of the bone flap develops immediately after osteotomy and transection of perineal artery and finally influences osteointegration process within the transferred bone. This application of virtual planning and navigation templates allows adequate reconstruction of extensive defects of the jaws and provides rapid prosthodontic rehabilitation of the patients, which naturally have great impact on QoL.