Orbitozygomaticomaxillary complex (OZMC) fractures are commonly encountered by the craniomaxillofacial trauma surgeon and may, in fact, be the most common type of orbital fracture [
1,
2,
3,
4]. Disruption of articulation with the frontal and sphenoid bones causes disruption of the internal orbital skeleton, which can result in diplopia from extraocular muscle swelling or entrapment, or enophthalmos from increased orbital volume. Although there is significant energy transferred to the orbit in these injuries, blindness and intra- orbital hematoma are, fortunately, relatively rare complications, typically seen pre- or postoperatively [
5,
6,
7]. In this report, we describe the development of acute intraorbital hemor-rhage following reduction of a displaced OZMC fracture.
1. Case Report
An otherwise healthy 22-year-old male was brought to the emergency department for evaluation of left-sided facial injuries sustained following blunt trauma. The patient sustained a mechanical fall onto concrete, hitting the left side of his face. There was no reported loss of consciousness. On initial presentation, he complained of mild pain over the left midface and periorbital region. He denied pain with eye movement, blurred/double vision, tearing, difficulty with mouth opening, facial numbness, headaches, or photophobia.
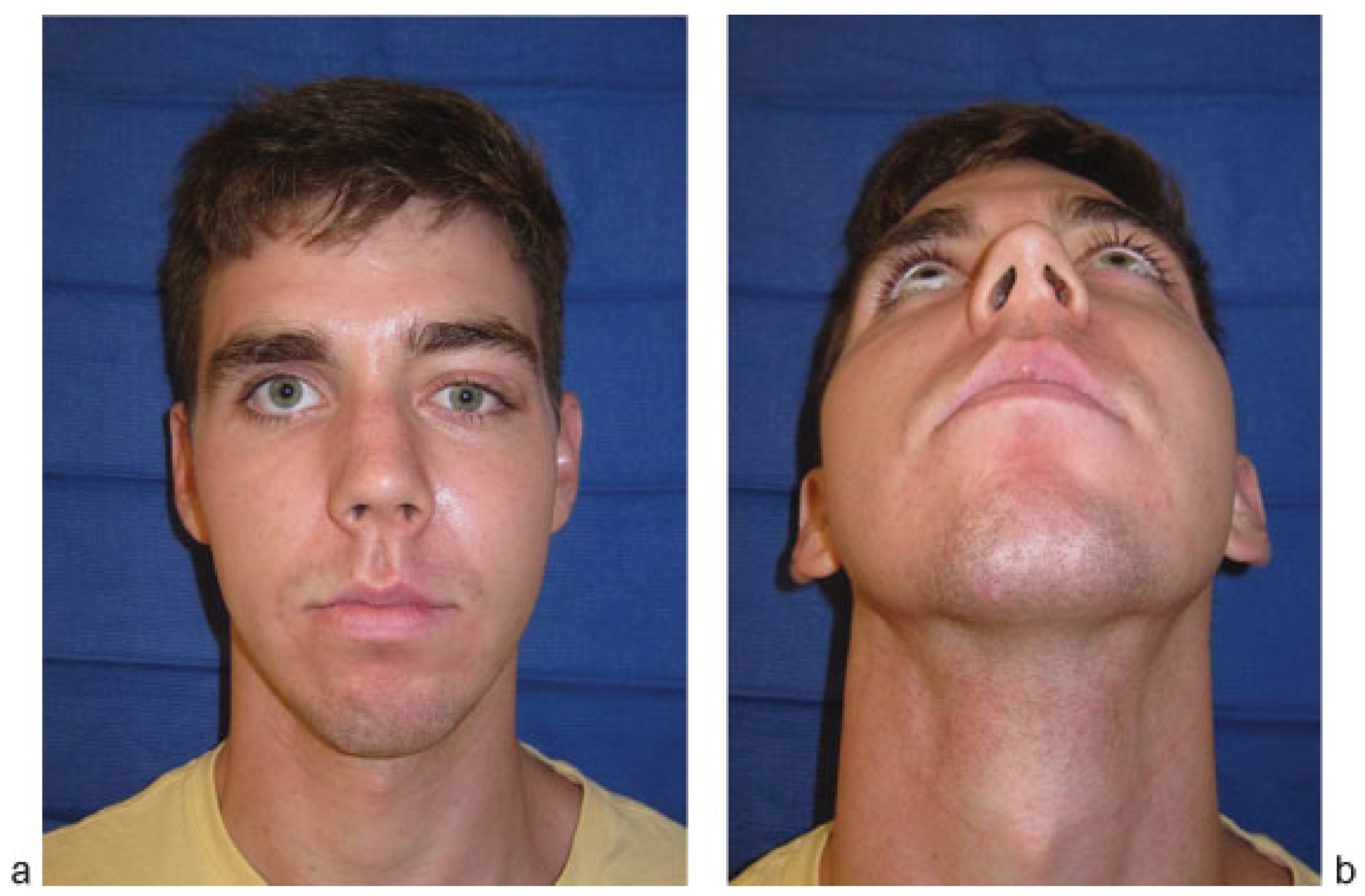
Physical examination (
Figure 1) was notable for mild left-sided periorbital edema and ecchymosis, with a 5-mm super-ficial laceration lateral to the left lateral canthus. The left zygomatic prominence was flattened relative to the right. Extraocular movements were fully intact in all directions. An ophthalmologic evaluation demonstrated visual acuity of 20/ 20 in both eyes with mild anisocoria (3 mm OD, 4 mm OS) with bilateral papillary response to light (3/4 mm → 2 mm). Intraocular pressures were 15 mm Hg in both eyes. There was no obvious subconjunctival hemorrhage or hyphema noted. The examination was otherwise unremarkable.
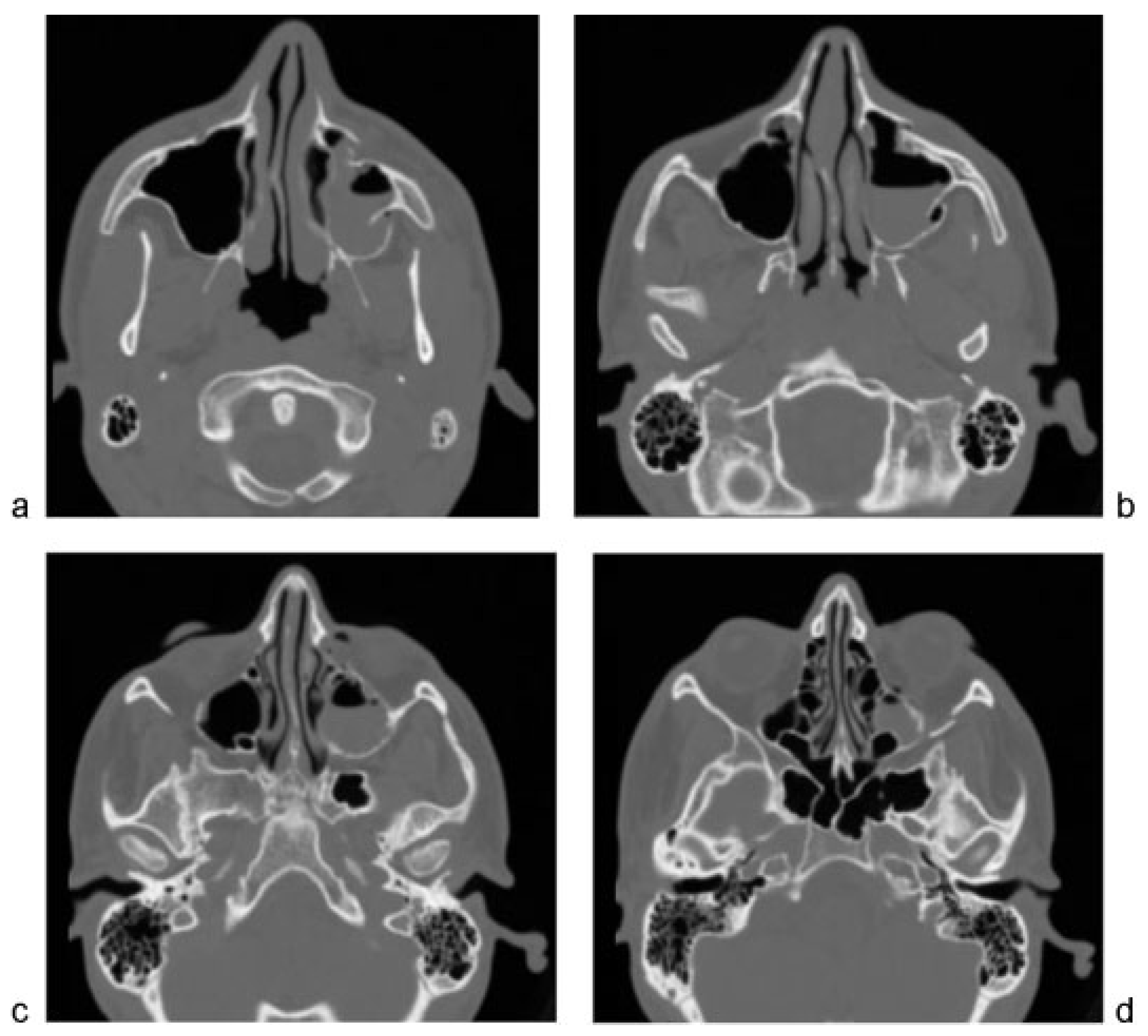
Maxillofacial computed tomography demonstrated a displaced, nonrotated left OZMC fracture (
Figure 2). There was no evidence of extraocular muscle entrapment, large orbital floor defect, retrobulbar, or intraorbital hematoma. Routine preoperative laboratory evaluation, including coagulation studies, was unremarkable.
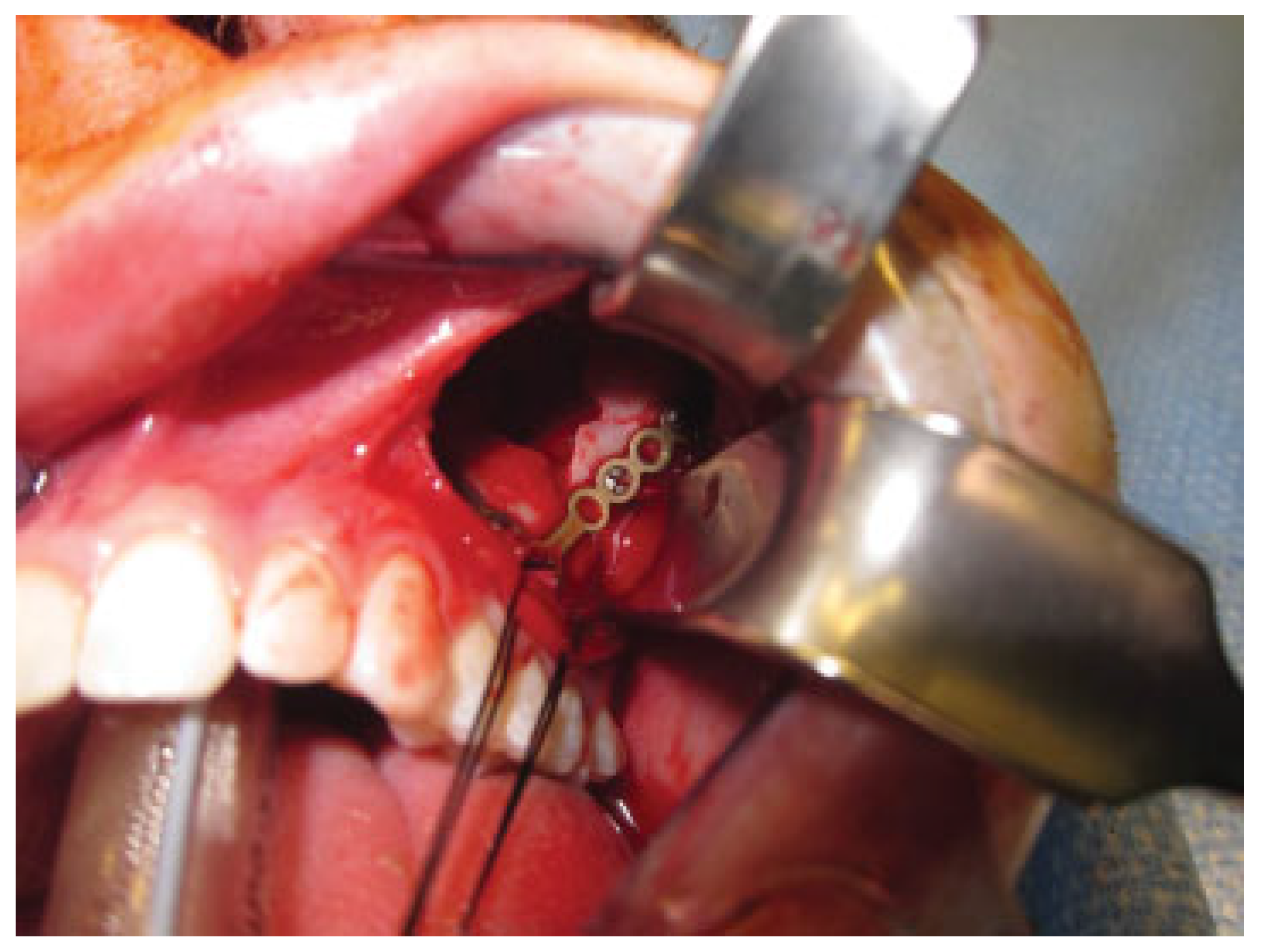
The patient was taken to the operating room approximately 16 hours following injury for open reduction and internal fixation. He was intubated orally and a corneal shield was placed for protection of the left globe. The left zygomatico-maxillary buttress was subsequently exposed using a standard gingivobuccal sulcus incision (
Figure 3). The body of the zygoma was mobilized using a curve Kelly clamp and reduction was achieved at the zygomaticomaxillary buttress. The infraorbital rim was directly visualized and noted to be in anatomic alignment. Palpation of the frontozygomatic suture did not reveal obvious step-off. As such, fixation was applied at the zygomaticomaxillary buttress using a 0.7-mm-thick L-shaped 1.5 medium plate (DePuy Synthes, West Chester, PA) (
Figure 4).
Following completion of reduction and fixation, forced duction testing was planned, as per routine. However, examination of the left globe revealed significant proptosis, with the globe under tension, and a dilated and nonreactive pupil. A lateral orbital decompression was immediately performed via an upper blepharoplasty incision. Upon accessing the lateral orbit, there was active, venous bleeding, with approximately 15 mL of blood immediately evacuated from the lateral orbit. The area was packed with epinephrine soaked patties and the bleeding subsequently stopped. Direct visualization of the sphenozygomatic and frontozygomatic sutures was notable for anatomic reduction at these sites (
Figure 5). Following decompression, the proptosis improved and the globe was less taut. Forced ductions were unrestricted. As no discrete bleeding vessel was identified, definitive surgical hemostasis was precluded. Therefore, two 1/4″ Pen- rose drains (Cardinal Health, Dublin, OH) were placed into the lateral orbit to prevent reaccumulation of fluid (
Figure 6).
The patient was subsequently extubated and visual acuity was noted to be intact, with papillary light response present before leaving the operating room. He was taken to the postanesthesia care unit in stable condition and was evaluated by the ophthalmology service immediately postoperatively. Visual acuity was noted to be consistent with baseline (20/ 20 OD, 20/20 OS), without afferent pupillary defect. Extra- ocular movements were intact. Elevated intraocular pressures were observed in the left globe (25 mm Hg), consistent with edema from surgical intervention.
The hematology service was consulted for evaluation of possible coagulopathy. Repeat coagulation testing and cofactor studies for bleeding diatheses were normal.
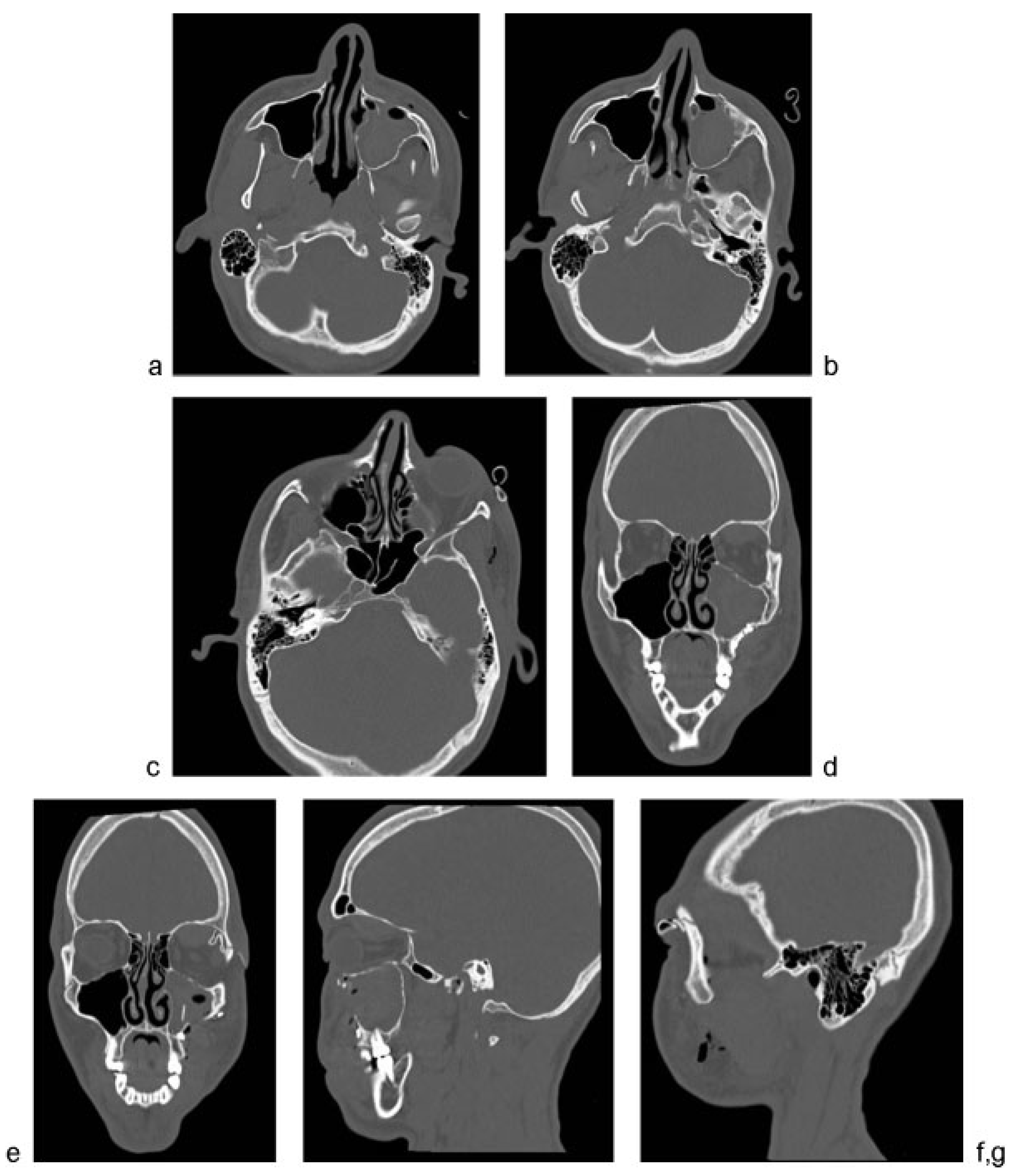
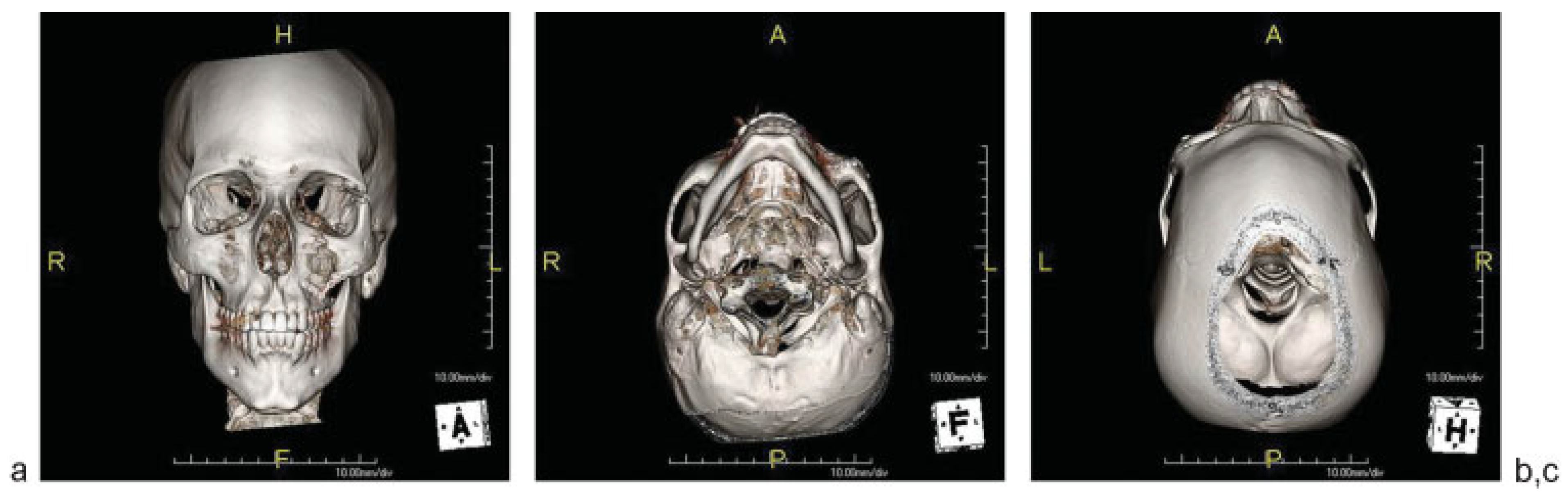
Postoperative imaging demonstrated anatomic reduction of the OZMC at all articulations (
Figure 7 and
Figure 8).
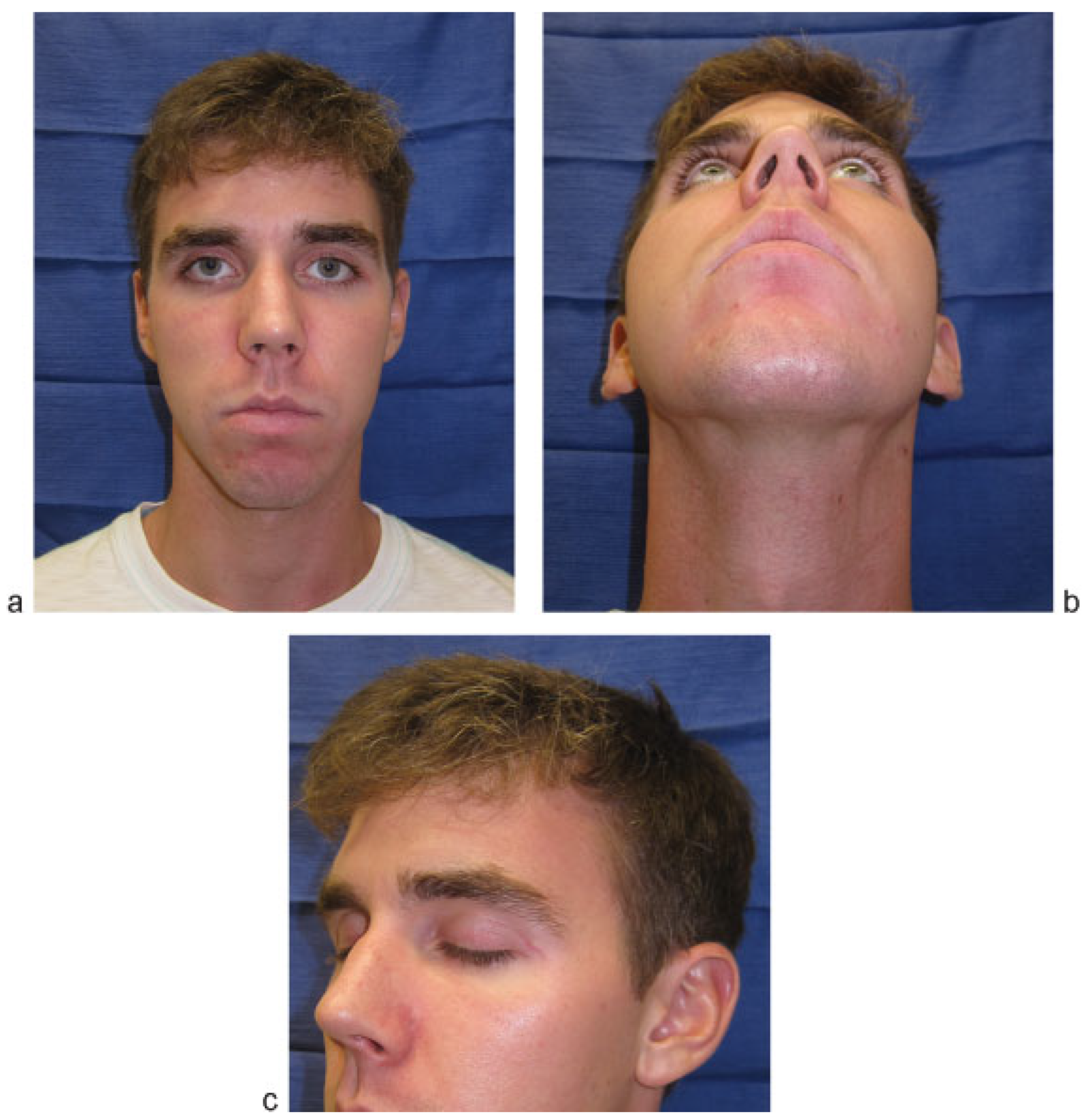
The patient was treated with a short course of high-dose steroids postoperatively. His swelling and proptosis continued to improve and he was noted to have full vision bilaterally on discharge, with no diplopia. The Penrose drains were removed before discharge on postoperative day 2. He was noted to be doing very well, with full vision and extraocular movements bilaterally, and restored zygomatic projection and facial symmetry at 10 days postoperatively (
Figure 9). At 6-month follow-up, the patient was noted to have excellent zygomatic projection and a symmetric face. The upper eyelid incision was well-healed, with minimal scarring (
Figure 10).
2. Discussion
Zygomaticomaxillary complex fractures, more appropriately referred to as OZMC fractures, are among the most frequently seen facial injuries in trauma centers [
1,
2,
3,
4]. Although there remain controversies regarding the most appropriate methods of exposure and fixation, surgeons are generally in agreement about the need for management within the acute or subacute period [
1,
2,
3,
8,
9,
10,
11]. Accurate anatomical reduction is necessary to prevent secondary deformities, which can be extremely difficult to correct.
Among the complications of fractures involving the OZMC are those related to injury to the internal orbital skeleton and globe. Major injuries, such as globe rupture and retinal hemorrhage, have been reported in up to 10% of patients with OZMC fractures, with traumatic optic neuropathy noted in 6% of patients [
7]. Among patients with OZMC fractures and concomitant open globe injuries, there is an increased risk of blindness [
12]. In addition, a systematic review of blindness associated with facial fractures showed a strong association between high-energy zygoma fractures and blindness [
6]. Ret-robulbar hemorrhage is a relatively rare complication that can result from the initial injury or subsequent operative manipulation. The incidence of postoperative retrobulbar hemor-rhage has been estimated to be 0.03% [
13]. Although these data offer sufficient rationale for ophthalmologic evaluation at the time of injury and judicious inspection of the globe during and after operative intervention, there are no reports, to our knowledge, of acute intraorbital hemorrhage immediately following anatomic reduction of an OZMC fracture.
The blood supply of the internal orbit includes several disparate venous structures, including the superior and inferior ophthalmic veins, and the infraorbital vein. It is likely that energy transfer during reduction may have damaged one of these vessels, resulting in acute hemorrhage, proptosis, and signs of optic nerve compression. Prompt recognition and intraoperative decompression prevented injury to the optic nerve.
It is imperative that the craniomaxillofacial surgeon be cognizant not only of the potential for intraorbital hemorrhage following OZMC injury but also following reduction, as described herein. While rare, the consequences of unrecognized hemorrhage can be devastating and should be completely avoidable. Meticulous inspection of the globe following reduction, including assessment of pupillary size and movement (via forced ductions) should be undertaken before extubating the patient. Visual acuity and light perception should be checked as soon as permitted by patient status.