Abstract
The aim of this study was to assess through biomechanical testing if different synthetic materials used to fabricate test specimens have a different biomechanical behavior in comparison with other materials when simulating in vitro load resistance of a fixation method established for sagittal split ramus osteotomy (SSRO). Thirty synthetic and standardized human hemimandible replicas with SSRO were divided into three groups of 10 samples each. Group A—ABS plastic; Group B—polyamide; and Group C—polyurethane. These were fixated with three bicortical position screws (16 mm in length, 2.0-mm system) in an inverted l pattern using perforation guide and 5-mm advancement. Each sample was submitted to linear vertical load, and load strength values were recorded at 1, 3, 5, 7, and 10 mm of displacement. The means and standard deviation were compared using the analysis of variance (p < 0.05) and the Tukey test. A tendency for lower values was observed in Group B in comparison with Groups A and C. At 3 and 5 mm of displacement, a difference between Groups A and C was found in comparison with Group B (p < 0.05). At 7 and 10 mm of displacement, a difference was found among the three groups, in which Group C showed the highest values and Group B the lowest (p < 0.05). Taking into consideration the results obtained and the behavior of each material used as a substrate, significant differences occurred among the materials when compared among them.
Fixation techniques used in sagittal split ramus osteotomy (SSRO) of the mandible have significantly improved stability, primary bone healing, maximum contact between the bone segments, maxillomandibular fixation, and early return of function. Therefore, the indication for surgical procedure is facilitated by using internal fixation.[1]
Fixation techniques for SSRO may be performed in three ways: using three bicortical screws in an inverted l pattern or “in-line”; one or two plates with monocortical screws; and a hybrid technique that uses a plate and monocortical screws associated with another bicortical screw in the retromolar area.[2,3]
Mandibular osteotomies fixated with an inverted l pattern present greater rigidity and strength in comparison with other screw placement patterns for fixation of SSRO when submitted to strength tests.[4,5]
Irrespective of the fixation method used, stability is an essential factor for the surgical success of the SSRO technique and it may be assessed by using biomechanical tests. However, strength tests of the osteosynthesis method present variables such as size, number, material configuration, and type of material used.[2,3]
In vitro biomechanical testing of methods of bone fixation of SSRO generally depends on the simulation models and this is considerably important with regard to the clinical applicability.[6,7] Laboratory experiments and simulations can show and help one to select the best fixation techniques, with regard to their potential to withstand loads that could destabilize the osseous union between the osteotomized segments, by simulating the bite force and displacement vectors[2,3,4,6,7,8,9,10] and showing, by comparison, those that could be potentially be safely used in patients.
Test specimens are used to conduct biomechanical tests, and these can be produced in the laboratory by means of rapid prototyping techniques or replication using synthetic materials, with the purpose of simulating bone anatomy, or simply using bone segments from animals or cadavers, or vegetables.
Among the substrates or test specimens of animal origin, there are studies in the literature that have used human cadaver mandibles,[5,8,11,12,13,14] fresh sheep mandibles,[15,16] bovine ribs,[17,18,19] and porcine ribs.[4]
Over the last few decades, the development of computing associated with a significant increase in precision mechanical engineering and availability of materials have allowed real synthetic models to be rapidly obtained from virtual models, creating the concept of rapid prototyping or solid free form manufacturing. This technology is used in many areas of knowledge, namely, architecture, paleontology, biochemistry, and medical applications,[20] and it can produce test specimens to simulate human anatomy in detail, as opposed to other techniques of manufacturing synthetic test specimens. Polyurethane is the material of choice for fabricating mandibular test specimens of synthetic origin.[2,3,6,7,10,21,22,23,24,25] Up to the present, we have not found any studies in the literature that have used another type of synthetic material, other than expandable polyurethane foam, or any other technique or technology to produce the test specimens specifically for testing the fixation of SSRO.
The aim of this study was to assess, by means of biomechanical testing, if different synthetic materials used to fabricate test specimens have a significantly different biomechanical behavior in comparison with other materials when simulating in vitro load resistance of a fixation method established for SSRO.
Material and Methods
To conduct the in vitro study, a model for cantilever bending fatigue test was used on synthetic and standardized human hemimandible replicas produced with SSRO, and fixated with three bicortical screws placed in an inverted l pattern. The hemimandibles were divided into three groups of 10 samples each, according to the synthetic material used: Group A—ABS plastic; Group B—polyamide; and Group C—polyurethane.
To fabricate the samples of Groups A and B, a computed tomography (CT) of the mandible considered healthy was selected. The CT images were initially processed in the computer program InVesalius version 2.1 (3DT Lab, CTI, Campinas, Sao Paulo, Brazil) generating a three-dimensional image of the entire mandible from reconstructed axial CT images.
After this, the computer program Magics RP version 16 (16.0.2.1) × 32 (Materialise NV, Leuven, Belgium) was used to virtually section the reconstructed three-dimensional image at the midline, keeping only the three-dimensional image of the right hemimandible. A virtual SSRO was simulated by separating the image of the hemimandible into two parts that referred to the proximal and distal segments (Figure 1).
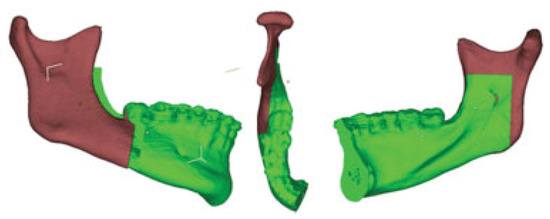
Figure 1.
Virtual models of SSRO design.
Next, the images were transformed into the standard triangle language (STL) format for physical production of samples, using two rapid prototyping technologies from the 3D Technology Laboratory (CTI, Campinas, Sao Paulo, Brazil). Ten Ten hemimandibles with simulated SSRO were made using ABS-type thermoplastic material (Group A) obtained with the rapid prototyping technique by fused deposition modeling (FDM) in the FDM Vantage i machine model (Stratasys Inc., Eden Prairie, MN, USA). Another 10 samples were made of polyamide (Group B) via rapid prototyping using the selective laser sintering technique (SLS) in the Sinterstation HiQ SLS machine system (3D Systems, Inc., Rock Hill, SC).
The 10 hemimandibles in Group C were fabricated using the replica technique from physical models of a hemimandible with SSRO. The synthetic material used was expanded polyurethane foam and two segments—proximal and distal — were also fabricated to simulate SSRO (Nacional Ossos. Jaú, Sao Paulo, Brazil).
To facilitate sample preparation, all the hemimandibles were fabricated in two segments, simulating SSRO. This procedure eliminated the need to perform manual osteotomy in the samples with a drill or saw, a procedure that could create variations in the osteotomy design, and possible damage could cause changes in the biomechanical test results, as it is impossible to reproduce SSRO manually in an equal manner in all samples.[2,13]
To fixate the proximal and distal segments and to maintain a standardized mandibular advancement of 5 mm and equal position of the screws for all samples, a virtual fixation guide was developed with the aid of the computer program Magics RP version 16 (16.0.2.1) × 32 (Materialise NV). The CT image data from a matrix-encased hemimandible with SSRO were used. The guide was made of ABS plastic by the FDM rapid prototyping technique and it was adapted perfectly to the samples produced by the rapid prototyping techniques in ABS plastic (Group A) and polyamide (Group B) (Figure 2).

Figure 2.
Fixation guide and virtual perforation of hemimandibles.
Because the polyurethane hemimandibles (Group C) were different from an anatomical point of view in comparison with the prototyped samples (Groups A and B), it was necessary to fabricate a second standardized guide for fixation and mandibular advancement. For this purpose, the reverse engineering prototyping technique was used to digitize the physical models. The polyurethane samples were manually scanned with a handheld 3D Scanner EXAscan (Creaform, Québec, Canada) generating digitized images that enabled a second guide to be manufactured for the hemimandibles, also using rapid prototyping and ABS plastic. The location of the perforations and 5-mm advancement followed the same patterns as those of the guide used for Groups A and B.
The samples were prepared for use of the inverted l technique, and 1.6-mm diameter bur was used for the perforations. A total of 90 self-tapping position screws, 16-mm long, 2.0 mm in diameter (MDT, Rio Claro, Sao Paulo, Brazil), made of commercially pure grade II titanium alloy (Ti-6Al-4V) were used to fixate the samples. Each sample in all groups received three position screws (Figure 3).
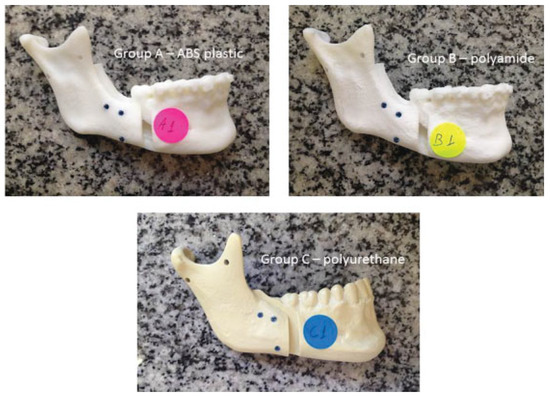
Figure 3.
Samples of Groups A, B, and C fixated with inverted l screws.
The biomechanical load test was performed in a universal load testing machine (Instron Universal 4411, Instron, Inc. Canton, MA) using rigid connections. The prepared samples were fixated on a metal support by means of two holes in the ascending ramus of hemimandibles, which enabled the samples to be correctly positioned on the test holder, using two screws, so that the mandibular occlusal plane was perpendicular to the force application device.
The samples in all groups were submitted to the application of linear vertical force from the top to the bottom in the occlusal region of the first molar (Figure 4), which required the fabrication of a groove to prevent the sample from sliding off the machine. The load was applied by a device coupled to the load cell of 50 kgf, with the machine programmed to apply progressive force at a displacement speed of 10 mm/min.

Figure 4.
Direction and location of force application during biomechanical testing.
Results
The strength values were obtained in newtons (N) by the program Bluehill 2 (Instron Corporation, Norwood, MA) coupled to the test machine during testing. The load value was recorded when displacement reached 1, 3, 5, 7, and 10 mm for each of the samples. From the data obtained, the Shapiro–Wilk test was initially applied to determine the normality of the data, which was confirmed (p > 0.05). Thus, for the intergroup comparison within each displacement assessed, the analysis of variance (ANOVA) was applied and the Tukey test was used to determine whether differences were detected. The SAS 9.01 (SAS Institute, Cary, NC) software was used at a level of significance of 5% for all the tests.
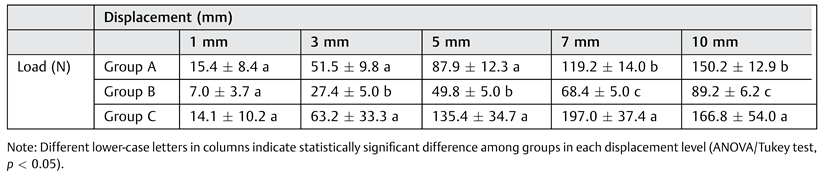
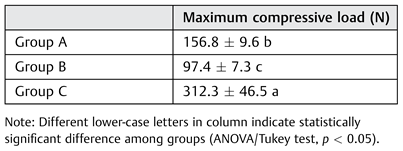
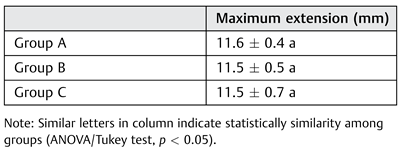
Table 1 shows the mean values obtained in each group for each displacement after the biomechanical test. Additionally, Figure 5 shows the vertical loading best-fit exponential tendency curves. Data indicated statistical difference among the groups in the displacements of 3 and 5 mm, with a lower strength values in Group B than in Group A and C (p < 0.05). At displacements of 7 and 10 mm, difference was found among the three groups, with Group C showing the highest values and Group B the lowest (p < 0.05). With regard to the maximum compressive load values (Table 2), Group B showed lowest maximum load (p < 0.05). However, Group C presented a higher maximum compressive value than other groups, A and B (p < 0.05). For maximum extension (Table 3), no statistically significant difference was found among the groups (p > 0.05).

Table 1.
Mean values (N ± standard deviation) for each group (N) within every displacement.
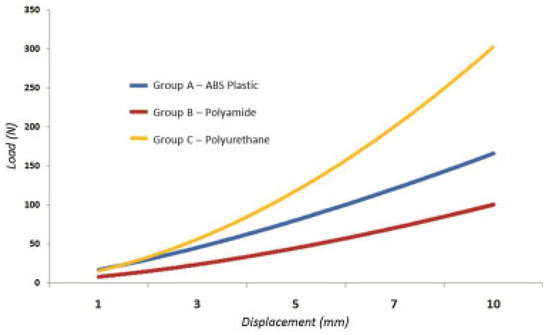
Figure 5.
Vertical loading best-fit exponential tendency curves.

Table 2.
Maximum compressive load (newton).

Table 3.
Maximum extension (mm).
Discussion
Although many studies have assessed the behaviors of different fixation methods for SSRO submitted to in vitro mechanical tests, no study has compared the differences among test specimens used for the tests in the same study. That is, the test specimens used were always made of the same synthetic, animal or vegetable material.
Fixation Method
Screws, whose properties have been studied in depth,[2] are the most common types of implants used in orthopedic and maxillofacial surgeries. The use of three 2.0-mm diameter position screws is considered the most cost effective, rigid, and predictable way to fixate SSRO.[2,6,7,8,9,10,26] The most common way to fixate SSRO is with the use of three bicortical position screws, generally in an inverted l or triangular pattern, placed perpendicular to the bone surface using percutaneous guides.[2,3]
It is important to note that the geometric disposition of the screws seems to affect the stability and resistance to functional forces, which is a more important characteristic than the diameter of the screws, and the use of larger screw diameters may not be necessary for adequate fixation.[7,27]
The pattern used—inverted l—is considered a resistant and stable fixation method for SSRO.[4,5]
Brasileiro et al[2,3] used guides made of chemically active acrylic resin with the purpose of standardizing perforation and the position of screws and plates inserted into the test specimens, minimizing the variations of the technique used. With the same purpose, standardized fixation guides were developed to standardize the positions of screws and segments of test specimens, with an advancement of 5 mm between segments; in addition, the guides facilitated sample preparation.
Biomechanical Properties
Among the biomechanical properties of a given material, bending is the most important property with regard to the type of load in biomechanics, which is determined by the effect of force applied perpendicular to the long axis of a test specimen.[2] Cantilever bending is the most common; that is, it is the effect of force applied to the extremity of the body fixated to another extremity.[13,28] Several other studies simulating the properties of internal fixation methods in synthetic samples have also been based on resistance to displacement by the cantilever bending forces as adopted in the present study.[2,3,7,8,9,10,19,21,22,23,24]
Rigidity is the parameter used to describe the force necessary to obtain a given structural deformation and it may be summarized as follows: “rigidity” = “load” divided by “deformation,” in which we can consider “load” as forces, moments, stresses, and “deformation” as displacement, deformation, curvature.[29,30]
For comparison of the biomechanical properties of synthetic substrates, such as human mandibular bone, the elastic modulus or Young modulus can be used. The elastic modulus of an object is defined as the slope of its stress–strain curve in the elastic deformation region. As such, a stiffer material will have a higher elastic modulus.[31] For human long bones, such as the femur, the Young modulus varies between 8 and 22.8 GPa.[32] Specifically for mandibular bone, the values found in the literature for Young modulus are widely dispersed and vary between 1.5 and 29.8 GPa.[33] However, various factors may influence determination of the mechanical or physical properties of human bone, such as the size of the sample, location, load conditions (static or dynamic), experimental method, and the manner in which the bone sample was handled and stored.[33]
Many types of substrates have been used in several in vitro studies, always associating them with characteristics closer to those of human bone for simulation. In this study, the samples of Group C were prepared with rigid expandable polyurethane foam. The mechanical properties and microstructure characterization of a series of graded commercial rigid polyurethane foams commonly used to mimic trabecular bone in testing orthopedic devices were reported by Calvert et al.[34] Compressive testing of rigid polyurethane foams used as bone analogs for implant testing was conducted by the authors according to the ASTM standard F1839-08—Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments[35] and provided an elastic modulus ranging from 0.115 to 0.794 GPa.[34] Depending on the density of the rigid expandable polyurethane foam used by manufacturer, it allows the production of more rigid specimens, compatible with the rigid material used in this experiment.
In comparison with the samples of the Groups A and B, the standard elastic modulus informed by the rapid prototyping machine manufacturers was 0.001627 GPa for specimens made of ABS plastic (extremely flexible) and 1.6 GPa for the polyamide samples. However, it is suggested that these values related to the modulus of elasticity of each material may be changed, because they are dependent on the programming parameters recorded in the rapid prototyping machines for sample production.
Test Specimens
When using synthetic test specimens for testing internal fixation, many variables and difficulties associated with the handling of human cadaver mandibles or animal bones are eliminated, such as the selection of standardized samples.[13]
With regard to the synthetic materials of choice for test specimen fabrication, specimens made of polyurethane have been reported to be the only material cited and used as a synthetic test specimen for biomechanical testing associated with internal fixation of SSRO.[2,3,6,7,10,21,22,23,24,25] In this context, we opted to test different materials, such as ABS plastic and polyamide in a same study, to verify whether there are significant differences between the samples, after the loading tests.
The mandibular samples of ABS plastic and polyamide used as test specimens in this study were fabricated using the rapid prototyping technique. The technique enabled better detailed structural and anatomical reproduction of mandible, both of the cortical bone and cancellous bone, as well as of the tooth roots inserted into the bone in comparison with the polyurethane samples.
The synthetic mandibles produced with polyurethane have been used as test specimens in many studies that simulated mandibular bone fixation of SSRO.[2,3,7,25] However, in comparison with other materials used in this study, polyurethane only allowed the reproduction of the external anatomy of the mandibular bone. Internally, the polyurethane test specimen is totally solid and there is no differentiation between the cortical bone and cancellous bone. Consequently, we found that this important characteristic of the polyurethane samples allowed greater engagement and a larger contact surface of the entire body of the screw inserted into the test specimen to simulate fixation of the segments, influencing the increase of fixation rigidity in these samples. This did not occur with the ABS plastic and polyamide samples due to the better reproduction of the internal anatomy of the cortical bone and cancellous bone. In the samples of Groups A and B, the cancellous bone was reproduced as an empty space between the cortical bones and it was even possible to identify the roots of the mandibular teeth inserted into the alveolar bone with engagement and contact surface of the body of the screws only in the cortical walls, as it occurs clinically (Figure 6).
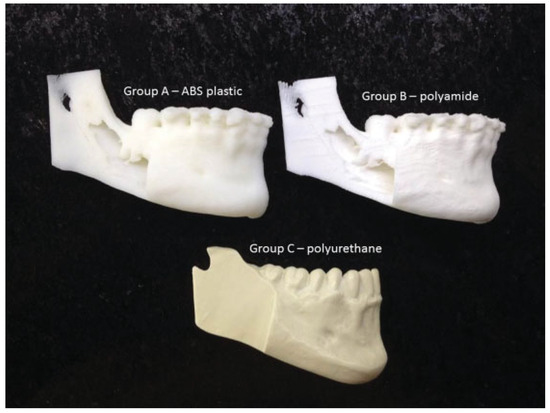
Figure 6.
ABS plastic, polyamide, and polyurethane test specimens—internal anatomy in detail.
An important feature of the synthetic materials used in this study is related to the quality and finishing of the samples fabricated by the previously mentioned prototyping techniques. The quality of the ABS plastic and polyamide models, as regards their anatomical details and hardness, in comparison with the polyurethanes samples, suggests a different mechanical behavior toward linear loading, than the behaviors shown in earlier studies in which only test specimens fabricated exclusively from polyurethane were used. The prototyped test specimens (Groups A and B) simulated the internal and external mandibular anatomy more accurately for the cortical, cancellous, and alveolar bones. When the polyurethane samples (Group C) were compared, although they simulated the external anatomy of the human mandible very well, the internal anatomy was limited to a totally solid model, which obviously generated greater rigidity and compatible results to loading tests, when compared with those of Groups A and B.
However, as found in another study related to biomechanical testing,[30] it is important to point out that laboratory measurements are auxiliary methods to determine the potential of simulated fixation methods and these must be carefully extrapolated to the clinical behavior of real methods, since the test specimen may generate interferences. Thus, the more reliable the model, the more it is possible to extrapolate the results obtained with it to clinical situations.
Considering the results obtained, we found that the samples from Group B were shown to require lower loading to achieve the proposed displacements with a lower loading value and without deformation of the fixation material or breakage of the system. Group A, in turn, showed intermediate loading values compatible with flexibility and resistance shown by the ABS plastic; and Group C showed extremely high loading values in comparison with the other groups being compatible with the rigidity of solid polyurethane samples.
With regard to the clinical applicability and the results obtained, an in-depth study of the biomechanical characteristics of each synthetic material is indicated to compare the properties of the human mandibular bone and those of the synthetic substrates used in in vitro tests. The specimens, depending on the synthetic material used to manufacture them, must be shown to be more homogeneous, with characteristics closer to those of natural bone. Many types of substrates have been used in several studies that have analyzed fixation methods for SSRO in vitro, always associating them with characteristics closer to those of human bone, for the purpose of simulation. When we compared rigid substrates with flexible substrates, the results obtained in loading tests would probably differ, due to the fact that if the substrates differ from the one that is being analyzed, it may mask the result and its clinical applicability.
Based on the methodology used for the production of samples for Groups A and B (rapid prototype technologies, in comparison with the samples of Group C), it was possible to define some of the advantages:
- Easy reproduction of the internal mandibular anatomy
- Greater precision and reproducibility of the osteotomies (computerized)
- Better reproduction of the anatomic details of the human mandible
- Greater uniformity of the samples
- Greater flexibility for strategic changes during the study, if necessary.
Therefore, the type of methodology used for sample production could influence the result of the loading tests, since the same technique and fixation material were always used for all the groups, with variation only of the method and types of material used for test specimen fabrication.
Taking into consideration the results obtained and the behavior of each material used as a substrate, the ABS plastic was shown to be more flexible and polyurethane more rigid. Polyamide was the material that required less loading to obtain a given maximum displacement in this study in comparison with the other materials tested. Therefore, significant differences in relation to loading were found when we used synthetic materials for fabricating different test specimens and the same fixation method for SSRO. However, the precise simulation of the human anatomy found in synthetic test specimens from Groups A and B and used in this study is not sufficient to affirm that the biomechanical behavior of the samples is similar to that of the human mandible, but these models can be used for simulation and extrapolated to clinical situations.
References
- Van Sickels, J.E.; Richardson, D.A. Stability of orthognathic surgery: a review of rigid fixation. Br J Oral Maxillofac Surg 1996, 34, 279–285. [Google Scholar] [CrossRef]
- Brasileiro, B.F.; Grempel, R.G.; Ambrosano, G.M.; Passeri, L.A. An in vitro evaluation of rigid internal fixation techniques for sagittal split ramus osteotomies: advancement surgery. J Oral Maxillofac Surg 2009, 67, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Brasileiro, B.F.; Grotta-Grempel, R.; Ambrosano, G.M.; Passeri, L.A. An in vitro evaluation of rigid internal fixation techniques for sagittal split ramus osteotomies: setback surgery. J Oral Maxillofac Surg 2012, 70, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Foley, W.L.; Frost, D.E.; Paulin, W.B., Jr.; Tucker, M.R. Internal screw fixation: comparison of placement pattern and rigidity. J Oral Maxillofac Surg 1989, 47, 720–723. [Google Scholar] [CrossRef]
- Kim, H.C.; Essaki, S.; Kameyama, T. Comparison of screw placement patterns on the rigidity of the sagittal split ramus osteotomy: technical note. J Craniomaxillofac Surg 1995, 23, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Hammer, B.; Ettlin, D.; Rahn, B.; Prein, J. Stabilization of the short sagittal split osteotomy: in vitro testing of different plate and screw configurations. J Craniomaxillofac Surg 1995, 23, 321–324. [Google Scholar] [CrossRef]
- Scaf de Molon, R.; de Ávila, É.D.; Scartezini, G.R.; et al. In vitro comparison of 1.5. mm vs. 2.0 mm screws for fixation in the sagittal split osteotomy. J Craniomaxillofac Surg 2011, 39, 574–577. [Google Scholar] [CrossRef]
- Ardary, W.C.; Tracy, D.J.; Brownridge, G.W., 2nd.; Urata, M.M. Comparative evaluation of screw configuration on the stability of the sagittal split osteotomy. Oral Surg Oral Med Oral Pathol 1989, 68, 125–129. [Google Scholar] [CrossRef]
- Murphy, M.T.; Haug, R.H.; Barber, J.E. An in vitro comparison of the mechanical characteristics of three sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg 1997, 55, 489–494, discussion 494–495. [Google Scholar] [CrossRef]
- Peterson, G.P.; Haug, R.H.; Van Sickels, J. A biomechanical evaluation of bilateral sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg 2005, 63, 1317–1324. [Google Scholar] [CrossRef]
- Bouwman, J.P.B.; Tuinzing, D.B.; Kostense, P.J. A comparative in vitro study on fixation of sagittal split osteotomies with Würzburg screws, Champy miniplates, and Biofix (biodegradable) rods. Int J Oral Maxillofac Surg 1994, 23, 46–48. [Google Scholar] [CrossRef]
- Schwimmer, A.; Greenberg, A.M.; Kummer, F.; Kaynar, A. The effect of screw size and insertion technique on the stability of the mandibular sagittal split osteotomy. J Oral Maxillofac Surg 1994, 52, 45–48. [Google Scholar] [CrossRef]
- Kohn, D.H.; Richmond, E.M.; Dootz, E.R.; Feinberg, S.E.; Pietrzak, W.S. In vitro comparison of parameters affecting the fixation strength of sagittal split osteotomies. J Oral Maxillofac Surg 1995, 53, 1374–1383, discussion 1383–1385. [Google Scholar] [CrossRef]
- Tharanon, W. Comparison between the rigidity of bicortical screws and a miniplate for fixation of a mandibular setback after a simulated bilateral sagittal split osteotomy. J Oral Maxillofac Surg 1998, 56, 1055–1058. [Google Scholar] [CrossRef] [PubMed]
- Foley, W.L.; Beckman, T.W. In vitro comparison of screw versus plate fixation in the sagittal split osteotomy. Int J Adult Orthodon Orthognath Surg 1992, 7, 147–151. [Google Scholar] [PubMed]
- Uckan, S.; Schwimmer, A.; Kummer, F.; Greenberg, A.M. Effect of the angle of the screw on the stability of the mandibular sagittal split ramus osteotomy: a study in sheep mandibles. Br J Oral Maxillofac Surg 2001, 39, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Anucul, B.; Waite, P.D.; Lemons, J.E. In vitro strength analysis of sagittal split osteotomy fixation: noncompression monocortical plates versus bicortical position screws. J Oral Maxillofac Surg 1992, 50, 1295–1299. [Google Scholar] [CrossRef]
- Armstrong, J.E.; Lapointe, H.J.; Hogg, N.J.; Kwok, A.D. Preliminary investigation of the biomechanics of internal fixation of sagittal split osteotomies with miniplates using a newly designed in vitro testing model. J Oral Maxillofac Surg 2001, 59, 191–195. [Google Scholar] [CrossRef]
- Trivellato, A.E.; Passeri, L.A. Evaluation of osteotomy fixation changing the number, the extension and the location of the plates. Br J Oral Maxillofac Surg 2006, 44, 377–381. [Google Scholar] [CrossRef]
- Silva, J.V.L.; Gouveia, M.F.; Santa Barbara, A.; Meurer, E.; Zavaglia, C.A.C. Rapid prototyping applications in the treatment of craniomaxillofacial deformities—utilization of bioceramics. Key Eng Mater 2004, 16, 687–690. [Google Scholar] [CrossRef]
- Van Sickels, J.E.; Peterson, G.P.; Holms, S.; Haug, R.H. An in vitro comparison of an adjustable bone fixation system. J Oral Maxillofac Surg 2005, 63, 1620–1625. [Google Scholar] [CrossRef] [PubMed]
- Sato, F.R.; Asprino, L.; Consani, S.; de Moraes, M. Comparative biomechanical and photoelastic evaluation of different fixation techniques of sagittal split ramus osteotomy in mandibular advancement. J Oral Maxillofac Surg 2010, 68, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Junior, P.D.; Magro-Filho, O.; Shastri, K.A.; Papageorge, M.B. In vitro biomechanical evaluation of the use of conventional and locking miniplate/screw systems for sagittal split ramus osteotomy. J Oral Maxillofac Surg 2010, 68, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Zizelmann, C.; Hammer, B.; Gellrich, N.C.; Kokemüller, H.; Bormann, K.H.; Rohner, D. In vitro biomechanical comparison of the effect of pattern, inclination, and size of positional screws on load resistance for bilateral sagittal split osteotomy. J Oral Maxillofac Surg 2011, 69, 1458–1463. [Google Scholar] [CrossRef]
- Aymach, Z.; Nei, H.; Kawamura, H.; Bell, W. Biomechanical evaluation of a T-shaped miniplate fixation of a modified sagittal split ramus osteotomy with buccal step, a new technique for mandibular orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011, 111, 58–63. [Google Scholar] [CrossRef]
- Ochs, M.W. Bicortical screw stabilization of sagittal split osteotomies. J Oral Maxillofac Surg 2003, 61, 1477–1484. [Google Scholar] [CrossRef]
- Obeid, G.; Lindquist, C.C. Optimal placement of bicortical screws in sagittal split-ramus osteotomy of mandible. Oral Surg Oral Med Oral Pathol 1991, 71, 665–669. [Google Scholar] [CrossRef]
- Cordey, J. Introduction: basic concepts and definitions in mechanics. Injury 2000, 31 (Suppl. 2), S-B1–S-B13. [Google Scholar] [CrossRef]
- Baumgart, E. Stiffness—an unknown world of mechanical science? Injury 2000, 31 (Suppl. 2), S-B14–S-B23. [Google Scholar]
- Vieira e Oliveira, T.R.; Passeri, L.A. Mechanical evaluation of different techniques for symphysis fracture fixation—an in vitro polyurethane mandible study. J Oral Maxillofac Surg 2011, 69, e141–e146. [Google Scholar] [CrossRef]
- Askeland, D.R.; Phulé, P.P. The Science and Engineering of Materials, 5th ed.; Cengage Learning: Toronto, ON Canada, 2006; p. 198. [Google Scholar]
- Bosisio, M.R.; Talmant, M.; Skalli, W.; Laugier, P.; Mitton, D. Apparent Young’s modulus of human radius using inverse finite-element method. J Biomech 2007, 40, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
- Odin, G.; Savoldelli, C.; Bouchard, P.O.; Tillier, Y. Determination of Young’s modulus of mandibular bone using inverse analysis. Med Eng Phys 2010, 32, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J Mater Sci Mater Med 2010, 21, 1453–1461. [Google Scholar] [CrossRef] [PubMed]
- ASTM International. ASTM Standard F1839–08 Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instruments; ASTM International, 2012. [Google Scholar]
© 2014 by the author. The Author(s) 2014.