Biomechanical Comparison of Four Mandibular Angle Fracture Fixation Techniques
Abstract
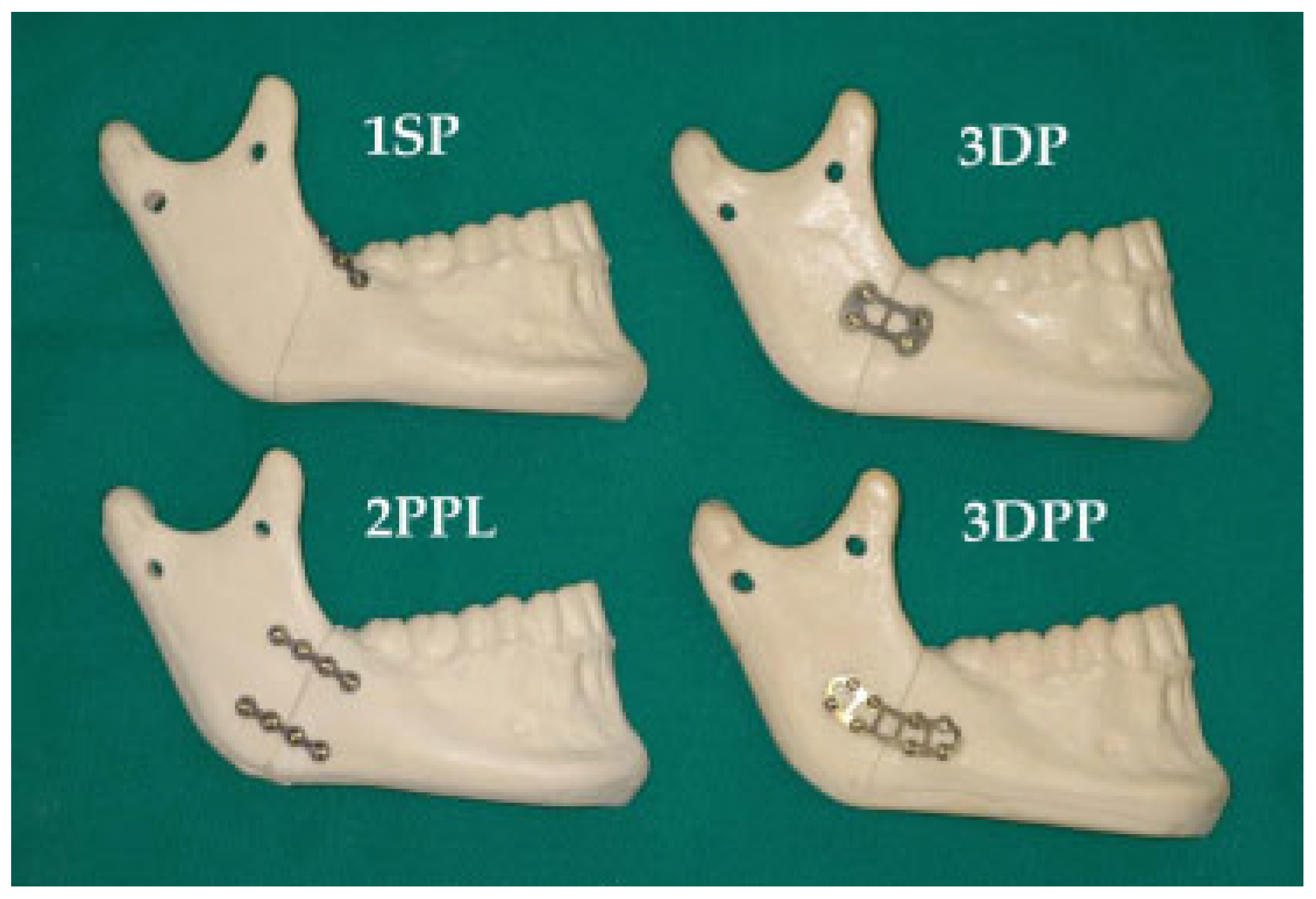
:Materials and Methods
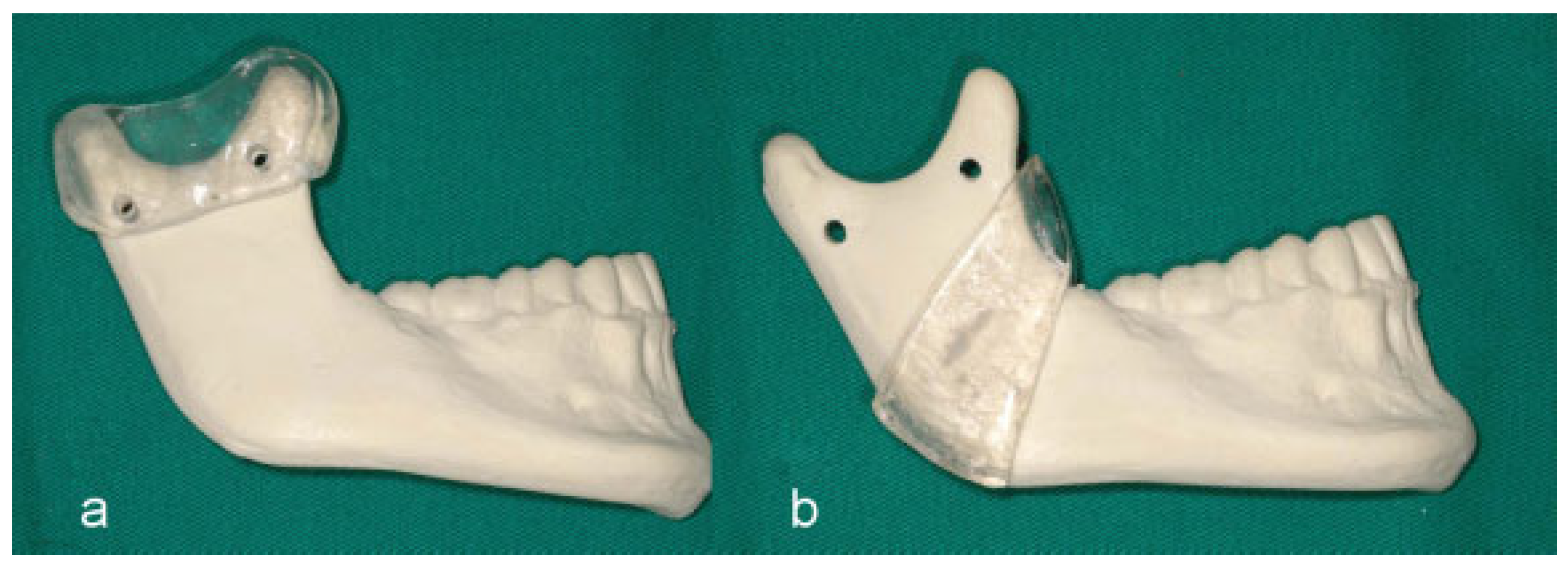
Sample Preparation
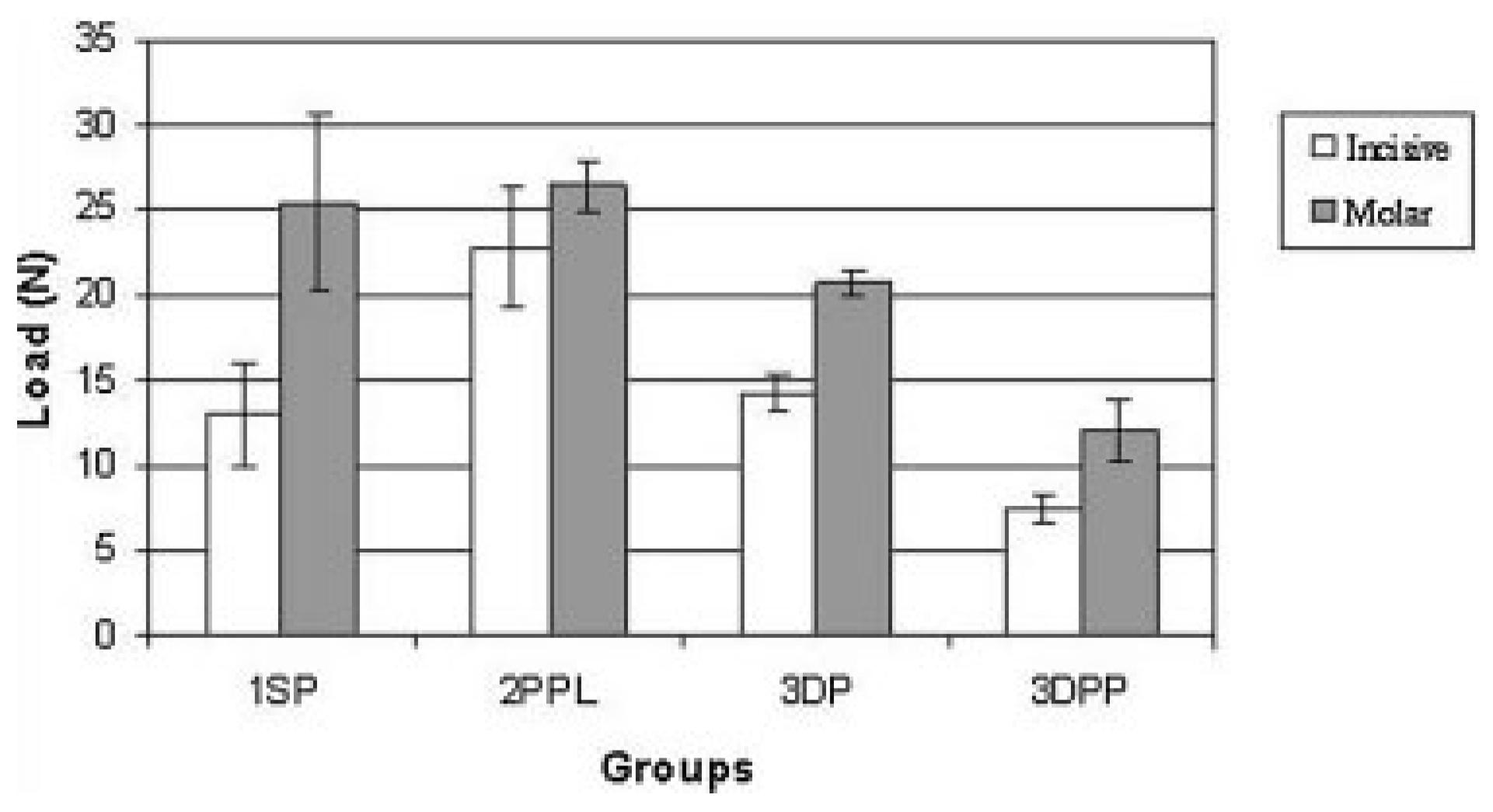
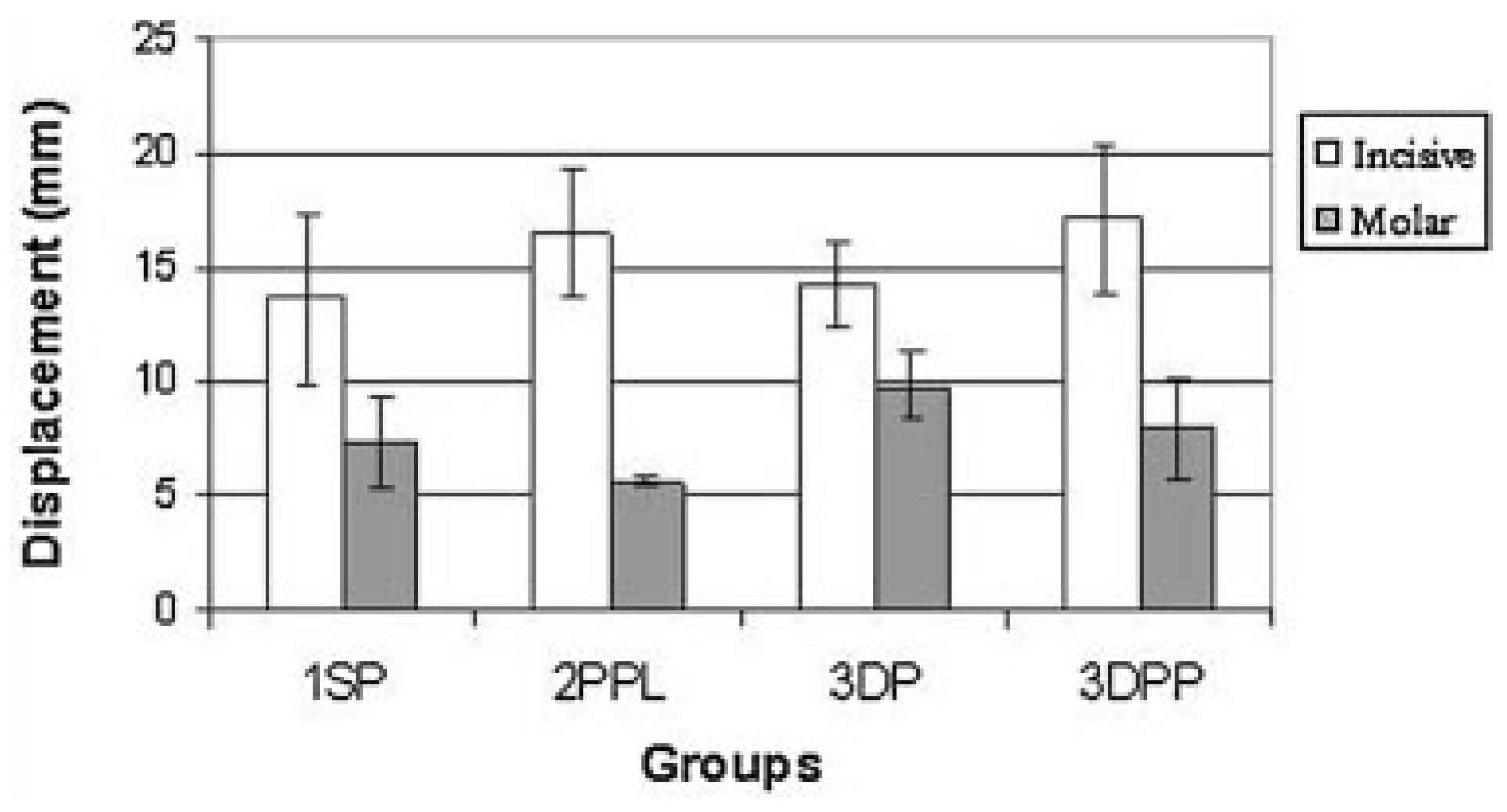
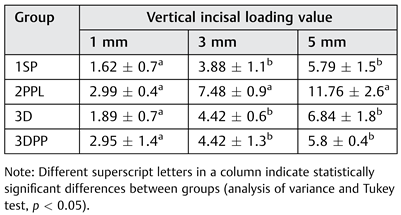
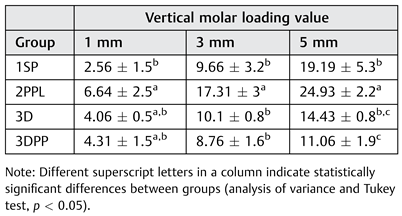
Results
Discussion
Acknowledgments
References
- Hogg, N.J.; Stewart, T.C.; Armstrong, J.E.; Girotti, M.J. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma 2000, 49, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Safdar, N.; Meechan, J.G. Relationship between fractures of the mandibular angle and the presence and state of eruption of the lower third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995, 79, 680–684. [Google Scholar] [CrossRef] [PubMed]
- Brasileiro, B.F.; Passeri, L.A. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006, 102, 28–34. [Google Scholar] [CrossRef]
- Champy, M.; Loddé, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg 1978, 6, 14–21. [Google Scholar] [CrossRef]
- Michelet, F.X.; Deymes, J.; Dessus, B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J Maxillofac Surg 1973, 1, 79–84. [Google Scholar] [CrossRef]
- Passeri, L.A.; Ellis, E., III; Sinn, D.P. Complications of nonrigid fixation of mandibular angle fractures. J Oral Maxillofac Surg 1993, 51, 382–384. [Google Scholar] [CrossRef]
- Ellis, E., III. Treatment of mandibular angle fractures using the AO reconstruction plate. J Oral Maxillofac Surg 1993, 51, 250–254, discussion 255. [Google Scholar] [CrossRef]
- Schierle, H.P.; Schmelzeisen, R.; Rahn, B.; Pytlik, C. One- or two-plate fixation of mandibular angle fractures? J Craniomaxillofac Surg 1997, 25, 162–168. [Google Scholar] [CrossRef]
- Haug, R.H.; Fattahi, T.T.; Goltz, M. A biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg 2001, 59, 1199–1210. [Google Scholar] [CrossRef]
- Fox, A.J.; Kellman, R.M. Mandibular angle fractures: Two-miniplate fixation and complications. Arch Facial Plast Surg 2003, 5, 464–469. [Google Scholar] [CrossRef]
- Alkan, A.; Celebi, N.; Ozden, B.; Baş, B.; Inal, S. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007, 104, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Feledy, J.; Caterson, E.J.; Steger, S.; Stal, S.; Hollier, L. Treatment of mandibular angle fractures with a matrix miniplate: A preliminary report. Plast Reconstr Surg 2004, 114, 1711–1716. [Google Scholar] [CrossRef] [PubMed]
- Kalfarentzos, E.F.; Deligianni, D.; Mitros, G.; Tyllianakis, M. Biomechanical evaluation of plating techniques for fixing mandibular angle fractures: The introduction of a new 3D plate approach. Oral Maxillofac Surg 2009, 13, 139–144. [Google Scholar] [CrossRef]
- Hochuli-Vieira, E.; Ha, T.K.; Pereira-Filho, V.A.; Landes, C.A. Use of rectangular grid miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg 2011, 69, 1436–1441. [Google Scholar] [CrossRef]
- Cabrini Gabrielli, M.A.; Real Gabrielli, M.F.; Marcantonio, E.; Hochuli-Vieira, E. Fixation of mandibular fractures with 2.0-mm miniplates: Review of 191 cases. J Oral Maxillofac Surg 2003, 61, 430–436. [Google Scholar] [CrossRef]
- Bormann, K.H.; Wild, S.; Gellrich, N.C.; et al. Five-year retrospective study of mandibular fractures in Freiburg, Germany: Incidence, etiology, treatment, and complications. J Oral Maxillofac Surg 2009, 67, 1251–1255. [Google Scholar] [CrossRef]
- Vieira e Oliveira, T.R.; Passeri, L.A. Mechanical evaluation of different techniques for symphysis fracture fixation—An in vitro polyurethane mandible study. J Oral Maxillofac Surg 2011, 69, e141–e146. [Google Scholar] [CrossRef]
- Bredbenner, T.L.; Haug, R.H. Substitutes for human cadaveric bone in maxillofacial rigid fixation research. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000, 90, 574–580. [Google Scholar] [CrossRef]
- Bos, R.R. Treatment of pediatric facial fractures: The case for metallic fixation. J Oral Maxillofac Surg 2005, 63, 382–384. [Google Scholar]
- Potter, J.; Ellis, E., III. Treatment of mandibular angle fractures with a malleable noncompression miniplate. J Oral Maxillofac Surg 1999, 57, 288–292, discussion 292–293. [Google Scholar] [CrossRef]
- Gear, A.J.; Apasova, E.; Schmitz, J.P.; Schubert, W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 2005, 63, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H.; Yoo, J.H.; Kim, K.N.; Kang, H.S. Stability testing of a two miniplate fixation technique for mandibular angle frac-tures. An in vitro study. J Craniomaxillofac Surg 1995, 23, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H.; Suh, C.H. Technique for applying 2 miniplates for treatment of mandibular angle fractures. J Oral Maxillofac Surg 2001, 59, 353–354. [Google Scholar] [CrossRef]
- Ellis, E., III; Walker, L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 1994, 52, 1032–1036, discussion 1036–1037. [Google Scholar] [CrossRef]
- Ellis, E., III. A prospective study of 3 treatment methods for isolated fractures of the mandibular angle. J Oral Maxillofac Surg 2010, 68, 2743–2754. [Google Scholar] [CrossRef]
- Siddiqui, A.; Markose, G.; Moos, K.F.; McMahon, J.; Ayoub, A.F. One miniplate versus two in the management of mandibular angle fractures: A prospective randomised study. Br J Oral Maxillofac Surg 2007, 45, 223–225. [Google Scholar] [CrossRef]
- Guimond, C.; Johnson, J.V.; Marchena, J.M. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg 2005, 63, 209–214. [Google Scholar] [CrossRef]
- Zix, J.; Lieger, O.; Iizuka, T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg 2007, 65, 1758–1763. [Google Scholar] [CrossRef]
- Fedok, F.G.; Van Kooten, D.W.; DeJoseph, L.M.; et al. Plating techniques and plate orientation in repair of mandibular angle fractures: An in vitro study. Laryngoscope 1998, 108 (8 Pt 1), 1218–1224. [Google Scholar] [CrossRef]
- Throckmorton, G.S.; Buschang, P.H.; Ellis, E., III. Improvement of maximum occlusal forces after orthognathic surgery. J Oral Maxillofac Surg 1996, 54, 1080–1086. [Google Scholar] [CrossRef]


 |
 |
© 2014 by the author. The Author(s) 2008.
Share and Cite
Muñante-Cardenas, J.L.; Passeri, L.A. Biomechanical Comparison of Four Mandibular Angle Fracture Fixation Techniques. Craniomaxillofac. Trauma Reconstr. 2015, 8, 123-128. https://doi.org/10.1055/s-0034-1393737
Muñante-Cardenas JL, Passeri LA. Biomechanical Comparison of Four Mandibular Angle Fracture Fixation Techniques. Craniomaxillofacial Trauma & Reconstruction. 2015; 8(2):123-128. https://doi.org/10.1055/s-0034-1393737
Chicago/Turabian StyleMuñante-Cardenas, Jose Luis, and Luis Augusto Passeri. 2015. "Biomechanical Comparison of Four Mandibular Angle Fracture Fixation Techniques" Craniomaxillofacial Trauma & Reconstruction 8, no. 2: 123-128. https://doi.org/10.1055/s-0034-1393737
APA StyleMuñante-Cardenas, J. L., & Passeri, L. A. (2015). Biomechanical Comparison of Four Mandibular Angle Fracture Fixation Techniques. Craniomaxillofacial Trauma & Reconstruction, 8(2), 123-128. https://doi.org/10.1055/s-0034-1393737



