High-energy trauma to the middle and upper face frequently results in complex three-dimensional injuries affecting multiple tissue types, and poses a unique and challenging reconstructive dilemma. Skin, underlying soft tissue, and bony structures are typically involved with substantial loss of tissue volume. The reconstructive plan must account for replacement of these distinct tissue types to achieve proper restoration of form and function. Local–regional options for tissue rearrangement and coverage are often employed as a primary option. Unfortunately, this approach is frequently inadequate to the task at hand with regard to both tissue volume and structural support, and can result in substandard and unsatisfactory outcomes. Indeed, early intervention with free tissue transfer has become firmly established as the ideal technique for reconstruction of large craniofacial defects arising from traumatic injury, producing optimal outcomes by re-establishing the bony support structure, providing an adequate soft tissue envelope, and preventing extensive scarring and resultant contracture.[
1,
2,
3,
4]
In the event that initial efforts prove to be inadequate, a secondary reconstructive strategy may be required. In this situation, several essential points must be considered when developing the surgical plan. There is often an extensive zone of injury that has undergone disadvantageous healing, with contracture of the remaining soft tissue. In addition, previous surgical efforts may have contributed to a paucity of available local–regional tissue. Thus, free tissue transfer is frequently required in these cases, though with the added complication of unpredictable recipient vasculature available for microanastomosis.[
2,
4] Although the successful use of free fibula or iliac crest bone flaps, and various skin and soft tissue free flaps has been extensively described for the restoration of traumatic craniofacial deformities, more extensive defects may require transfer of larger tissue volumes or multiple tissue types that cannot practically or effectively be accomplished with only a single tissue flap.[
1,
2,
3,
4]
Chimeric free flaps, designed to include multiple component flaps transferred on a single, branching vascular pedicle, offer a solution to many of the aforementioned complex reconstructive challenges. The subscapular system offers assorted permutations of fasciocutaneous, muscular, and osseous flaps, and owing to a lengthy singular vascular pedicle, can be simultaneously transferred with a single microvascular anastomosis, typically outside the zone of injury. Furthermore, as a consequence of the branching vasculature, the individual flap islands can be easily manipulated to optimize three-dimensional inset, providing significant flexibility for the surgeon. Chimera based off this arterial system have been successfully used in the reconstruction of extensive head and neck, as well as upper and lower extremity defects after both oncologic resection and traumatic injury.[
5,
6,
7,
8,
9,
10,
11] Accordingly, these flaps offer a potentially ideal secondary strategy in cases of failed previous reconstructive attempts.[
5,
6] With this small case series, we present and discuss our successful experience using subscapular chimeric free flaps in the secondary reconstruction of composite traumatic defects of the middle and upper face.
Patients and Methods
Between 2009 and 2012, a total of five patients with posttraumatic composite defects of the middle and upper face, all of whom had undergone previous reconstructive surgery with unsatisfactory outcomes, underwent secondary reconstruction using chimeric free flaps harvested from the subscapular arterial system. Three patients were male, and two patients were female. Traumatic injury resulted from gunshot wounds in three patients, and motor vehicle accidents in two patients. Specific tissue defects varied between patients, but included oro-orbital fistulae, oroantral fistulae, enophthalmos, bony defects of the supraorbital rim, infraorbital rim, zygoma, and maxilla, as well as a range of soft tissue deficits. Two patients were reconstructed using chimeric flaps that included scapular bone and latissimus muscle tissue island components, and three patients were reconstructed using chimeric flaps that included scapular bone and thoracodorsal artery perforator (TDAP) fasciocutaneous tissue island components.
Surgical Technique
All patients were placed in a supine position for initial debridement of the recipient site and exposure of the anatomy vital to the reconstruction. All scar tissue, nonviable tissue, and fistula tracts were liberally debrided to healthy tissue, and all alloplastic materials from previous reconstructions were removed. Next the recipient vessels were exposed and prepared for microanastomosis. At this point, the patients were placed into a lateral decubitus position for harvest of the donor tissue.
Specifics of flap harvest were dependent on the individual tissue requirements of each patient; however, the general approach and dissection in these cases were similar. Before incision, the TDAPs are identified and marked using a handheld Doppler. For inclusion of a TDAP, the skin paddle was marked, and dissection began with a lateral incision and continued posteriorly in the subfascial plane until the perforators were encountered and preserved, and the flap was raised. Retrograde dissection proceeded from the perforators toward the thoracodorsal artery, at which point a latissimus muscle island could be included in the harvest. Dissection again continued in a retrograde fashion until the angular branch to the lateral scapula was identified and exposed. The periscapular musculature was elevated to allow osteotomies and harvest of a bone island component as part of the chimera. Dissection continued proximally to the confluence of the thoracodorsal and the circumflex scapular arteries, and the common subscapular artery pedicle was harvested to the length required specific to the reconstructive needs of the case.
After placing drains, the donor site was closed primarily in layers. Modifications could then be made to the bone flap (i.e., additional osteotomies, plates, screws, etc.), and the soft tissue components were able to be shaped appropriately. The patient was placed back into the supine position and the flap inset before microanastomosis.
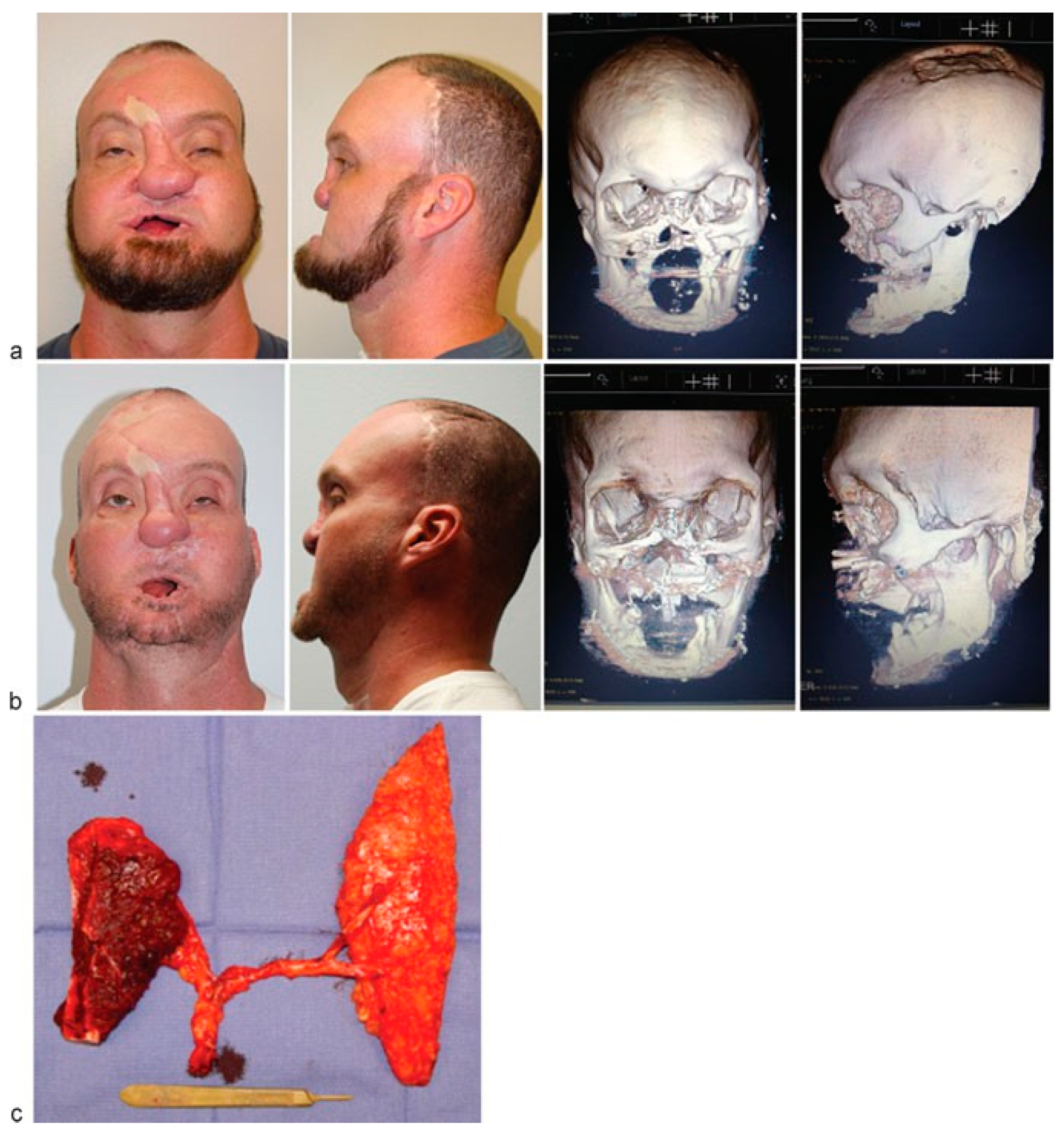
Case 1
J.L. is a 28-year-old female who suffered a gunshot wound to the left face, and had previously undergone multiple attempts at reconstruction. Before her presentation, she had an enucleation of her left globe, and a failed attempt at reconstruction using a local–regional flap and calvarial bone graft. The residual defects included a large oro-orbital fistula and absence of the infraorbital rim on the left. Reconstructive requirements included bone to restore continuity of the infraorbital rim for adequate lid and prosthetic support, and soft tissue to close the fistula and obliterate dead space in the left maxillary sinus (
Figure 1).
A 4.8 × 2.4 cm scapular bone island and a latissimus muscle island were harvested as part of the chimera. The scapular component was trimmed to fit the orbital rim defect and secured in place with a curved plate, while the latissimus portion of the flap was trimmed and positioned to obliterate the maxillary defect. The patient’s immediate postoperative course was significant for a minor salivary fistula at the site of the incision for exploration of the recipient vessels in the left neck, which resolved with nonoperative management. Thirty months after her reconstruction, her oro-orbital fistula remains resolved, she is satisfied with her improved cosmesis, and has experienced no major complications.
Case 2
B.G. is a 30-year-old male who presented status postmotor vehicle accident, having suffered severe left fronto-orbital injuries. He had previously undergone reconstruction of his bony defects with titanium mesh, which had resulted in significant contour deformity at the level of the supraorbital rim, as well as attenuation of the skin overlying the site of the mesh. The patient required transfer of vascularized bone and skin to re-establish appropriate contour at the supraorbital rim, as well as the adjacent soft tissue envelope (
Figure 2).
An 8 × 20 cm TDAP adipocutaneous island and a 3 × 8 cm scapular bone flap island were harvested on the subscapular artery as part of the chimera. The bone flap was positioned to reconstruct the forehead and lateral orbital rim, and a new mesh cranioplasty was positioned over which the de-epithe-lialized adipocutaneous component was inset to re-establish adequate soft tissue contour and bulk.
The patient’s postoperative course was uneventful. He later underwent a secondary procedure in which the scapula was reshaped and reinset to provide better contour to the lateral orbital rim, at which time the soft tissue paddle was also reshaped and repositioned. Although the patient still has some residual dystopia, he is blind in the affected eye as a result of his original trauma, and has expressed overall satisfaction with the improvements obtained with this secondary effort and has experienced no major complications.
Case 3
E.R. is a 37-year-old male who presented several years after a self-inflicted gunshot wound to the face. He had previously undergone over 20 surgical procedures including two free fibula flaps for mandibular and maxillary reconstruction, a forehead flap for attempted nasal reconstruction, and numerous local flaps for reconstruction of the upper and lower lips, though without satisfactory outcomes. At presentation, he had a persistent maxillary defect, a large oronasal fistula, and a significant soft tissue deficiency at the nose and upper lip. The patient also desired to set the stage for future placement of osseointegrated dental implants. He required transfer of bone and skin to obliterate the fistula and re-establish appropriate contour and soft tissue envelope to the midface. Virtual surgical planning was used to plan the contouring of the bony segment (
Figure 3).
A TDAP flap island and 10 × 2 cm scapular bone flap island were harvested as part of the chimera. The bone flap component was shaped using a prefabricated surgical guide created from the preoperative virtual surgical planning, and inset with a precontoured plate. The skin paddle was used to resurface the oral fistula and floor of the nose. In this case, the subscapular pedicle length was not adequate to reach the recipient vessels for microanastomosis, and a saphenous vein graft was required.
The patient’s immediate postoperative course was uneventful, and he suffered no complications. He subsequently underwent de-bulking of the soft tissue portion of his flap and several procedures for upper lip reconstruction.
Discussion
High-energy traumatic injury to the upper face presents a complicated reconstructive challenge. Established tenets of reconstruction of this region include early intervention, transfer of adequate tissue volume, and re-establishment of the buttresses of the facial skeleton to prevent soft tissue contraction and deformity.[
2,
3] Local–regional tissues such as temporalis, forehead, and deltopectoral flaps may be used as a primary option for moderate defects; however, pedicle length can be a problem, and there is often insufficient soft tissue available for mobilization adjacent to the zone of injury.[
1] In addition, nonvascularized bone grafts must be employed if skeletal reconstruction is required, risking resorption, and loss of the bony architecture. Inadequate reconstruction can result in contraction of soft tissues, fistula formation, unacceptable functional, and cosmetic outcomes, and can ultimately require extensive revisions.[
2,
3,
4]
Free tissue transfer has likewise become firmly established as the primary reconstructive option in cases of extensive defects to the head and neck for both traumatic injury and following oncologic resection.[
1,
2] In the hands of technically proficient surgeons, flap survival rates are routinely greater than 93%, and procedural time need not be prohibitive.[
1,
2,
3,
4] The obvious advantages of free flaps include the ability to transfer vascularized bone, muscle, skin, and soft tissue in adequate volumes as needed from unaffected areas of the body.
Affected tissue at the site of injury can be completely debrided, and with adequate pedicle length the vascular anastomosis can be performed with intact recipient vessels outside of the zone of injury. These patients consistently achieve cosmetic and functional outcomes superior to what has been observed with local tissue rearrangement.[
1,
2,
3,
4]
Chimeric free flaps are harvested off of a single vascular pedicle with branching vessels that allow the simultaneous transfer of multiple tissue islands with only a single microanastomosis. Depending on the reconstructive needs of the patient and the donor site selected for harvest, chimera can include islands of varying tissue types—skin, fascia, muscle, bone—in any number of combinations, and allow for the transfer of large volumes of tissue. In addition, the vascular anatomy of these flaps allows for significant freedom and optimization of the three-dimensional inset of the individual components.
Numerous intrinsic arterial systems have been employed for the harvest of chimeric flaps and used successfully in the reconstruction of all areas of the body. The lateral femoral circumflex system, which can include multiple skin paddles, vastus lateralis or vastus intermedius muscle, tensor fasciae latae, and femoral or iliac crest bone components, have been described for lower extremity and head and neck reconstruction.[
12,
13,
14,
15] Peroneal artery chimera that include fibula, soleus muscle, and perforator-based skin paddle components have been used for both upper and lower extremity, as well as head and neck reconstruction.[
16,
17] The deep inferior epigastric system allows for the harvest of chimera that include rectus muscle and perforator-based skin flaps, which have been used for lower extremity reconstruction.[
18]
However, the most commonly described intrinsic chimera are those harvested off of the subscapular arterial system, used extensively in the reconstruction of the head and neck, and lower and upper extremities after oncologic resection, traumatic injury, radiation injury, and congenital deformity.[
5,
6,
7,
8,
9,
10,
19,
20,
21,
22,
23] From the subscapular artery to the thoracodorsal/circumflex scapular bifurcation, branches to the serratus and latissimus, the angular branch to the lateral scapula, and perforators supplying the overlying skin paddles, the anatomy of this system remains relativelyconsistent, with anatomic studies citing an incidence of prohibitive anomalies in roughly 5% of the dissections performed.[
24] Components available for simultaneous transfer include lateral scapula (up to 14 cm segment when including both the angular branch of the thoracodorsal artery and the circumflex scapular artery) and rib osseous flaps, parascapular fascia, latissimus and serratus muscle, TDAP, and parascapular adipocutaneous flaps. The scapula is particularly useful in this setting as a bone flap, as it can be shaped through segmental osteotomies for complex three-dimensional bony reconstruction, and can later be used as a base for placement of osseointegrated dental implants. Overall, there exist greater than four dozen possible permutations based on the subscapular system, with the successful simultaneous transfer of up to five tissue islands having been described.[
5,
11,
19,
22,
23,
24]
Though it is difficult to comment on precise pedicle length due to the branching nature of the vasculature and the degree of variability involved in the flap construct depending on which components are incorporated into the chimera, the available pedicle that can be harvested from this system typically allows for anastomosis outside of the zone of injury without the need for vein grafting.[
5,
9] While donor-site morbidity can vary greatly depending on the extent of the dissection, cosmetic and functional deficits are typically not prohibitive in these cases.[
5,
20]
It is important not to lose sight of the fact that this these procedures are technically challenging and should be undertaken by surgeons experienced specifically in the microsurgical reconstruction of complex craniofacial defects. In addition, the operative times can be extensive, owing to the complicated nature of the dissection, the need to reposition the patient multiple times during the course of the procedure, and the intraoperative challenge of optimizing the three-dimensional inset of the flap components without compromising the vascular supply.
In our experience with the five patients presented in this series, a variety of complex reconstructive challenges were encountered and successfully treated with subscapular chimera. Not only did all of these patients have significant preexisting bony deficits from theretofore inadequate reconstructive attempts, they also suffered from complex soft tissue pathology that included large areas of attenuation, and oronasal and oro-orbital fistulae. By utilizing bone flaps from the scapula transferred simultaneously with one of the available soft tissue islands from the subscapular system, including both adipocutaneous and muscular flaps, we were able to adequately correct both the structural and soft tissue pathologies in a single procedure. Though these are admittedly technically challenging procedures, all of the patients in this series recovered without any significant complications, and all were satisfied with their improved form and function.
Conclusion
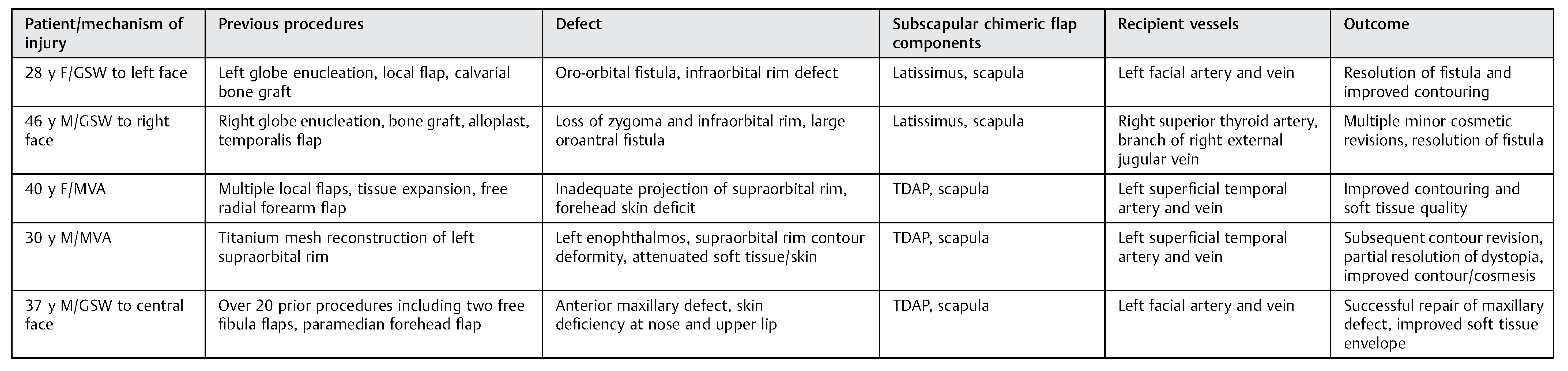
Free tissue transfer has been very successful in the reconstruction of extensive defects of the upper face secondary to trauma. However, there remain instances where complex injuries present reconstructive challenges beyond the scope of what a single tissue island free flap is capable of repairing. There are also times when prior failed attempts at reconstruction may have consumed a surgeon’s ideal flap choices, created the need for extensive debridement of contracted soft tissue, and may have depleted the optimal local vessels available for microanastomosis. Most available reports have focused on optimization of the primary reconstructive efforts of the surgeon. However, these challenging secondary cases require sophisticated solutions, and though the specific needs of these patients must be considered on an individual basis, successful surgical strategies must be developed. The series of cases presented here, and the successful outcomes described, support the notion that chimeric free flaps from the subscapular system should be considered by the experienced surgeon when planning for the secondary reconstruction of traumatic defects to the middle and upper face (
Table 1).