Ankylosing spondylitis (AS) is a chronic, usually progressive, systemic inflammatory joint disease, which predominantly affects the spine and sacroiliac joints [
1,
2,
3,
4,
5,
6,
7,
8]. In these joints, early inflammatory changes are followed by lumbosacral pain and progressive restriction of spinal movement associated with radiologically visible intervertebral ossification [
2,
8]. Peripheral joint involvement occurs in 10 to 30% of patients and shows a predilection for the shoulders, knees, ankles, feet, and wrists [
1,
2]. Temporomandibular joint (TMJ) involvement in patients with AS has been described, and its reported frequency varies from 11 to 35%, depending on the diagnostic criteria, the population studied, and the tools used to asses TMJ involvement [
2,
4,
6,
7]. However, ankylosis of the TMJ is uncommon, and to our knowledge only one documented case has utilized an alloplastic prosthesis for joint replacement [
8,
9]. A case report of bilateral ankylosis of the jaw treated with alloplastic prostheses for total TMJ replacement using a Brazilian system in a patient with AS is presented.
Case Report
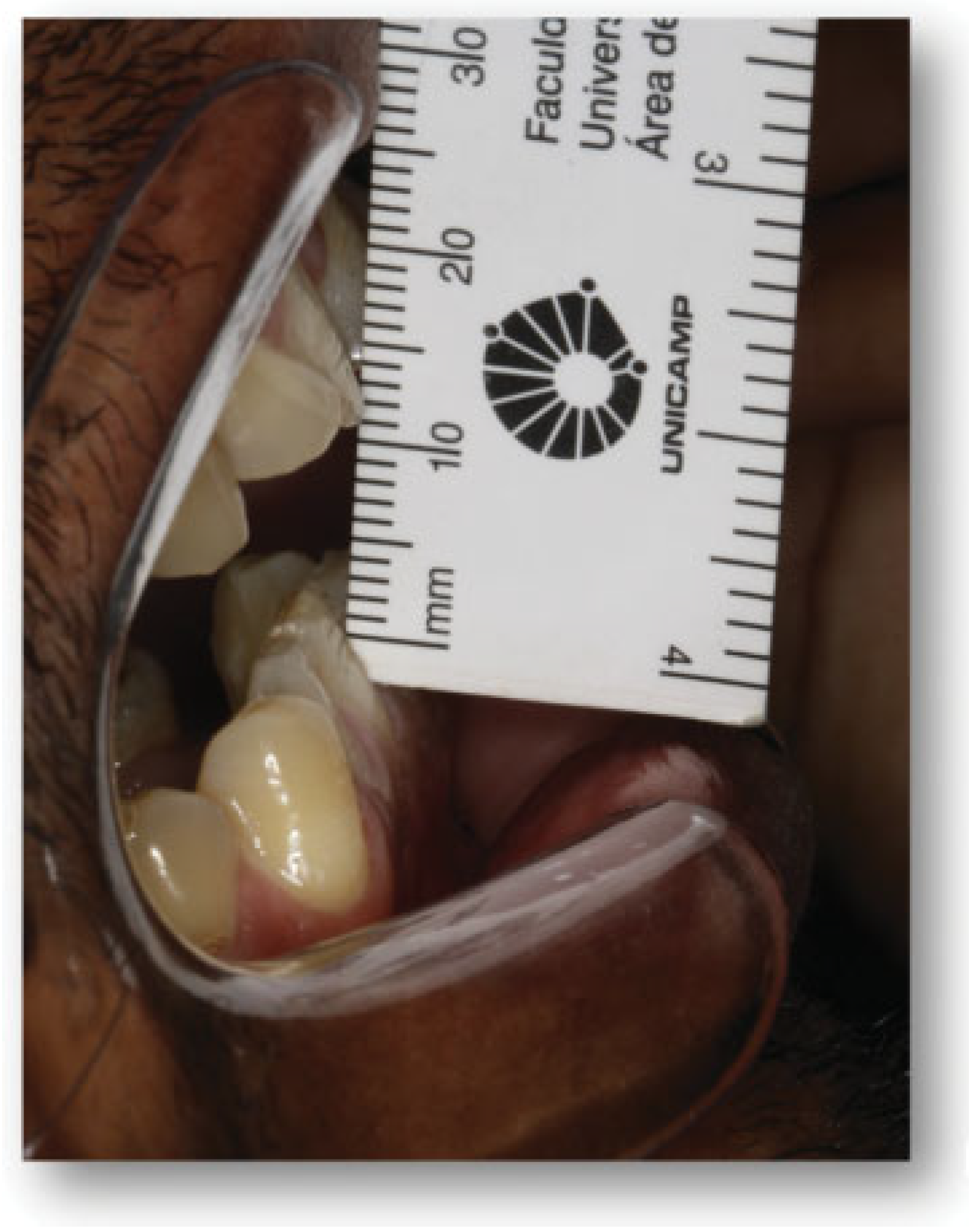
A 38-year-old man with AS was referred to the division of Oral and Maxillofacial Surgery of Piracicaba Dental School for limitation of mouth opening 16 months ago. Examination revealed that he had a 9 mm interincisal opening (
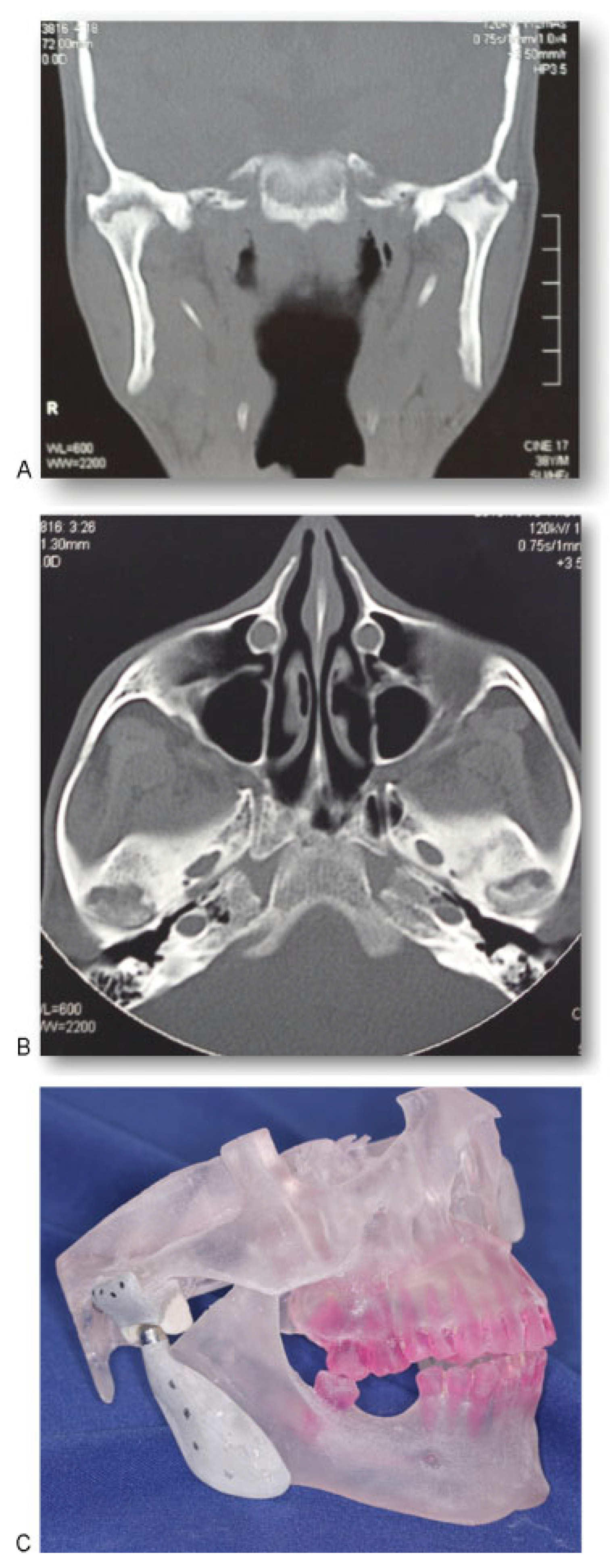
Figure 1), with no lateral or protrusive mandibular movements, including severe rigidity of the cervical, thoracic, and lumbar spine. The patient reported that he underwent surgery on both shoulders in 2006 due to the joint involvement caused by the disease. In 2008, the AS affected the right iliac-femoral joint, and the patient had a femoral prosthesis inserted. The same occurred the following year with the left iliac-femoral joint. Computed tomography (CT) of both TMJs confirmed severe ankylosis (
Figure 2A,B). Because of the extent of his disease, resection of the ankylotic mass and replacement of both TMJs by total alloplastic joint was indicated [
9]. A stereolithographic prototype was built from the CT sections and a mock surgery was done on the prototype for fabrication of individualized prostheses (
Figure 2C). The mandibular component is made of titanium, with the condylar head of cobalt–chromium–molybdenum alloy. The fossa component is designed to replace the articulating surface of the TMJ comprised by the glenoid fossa and the articular eminence. It is made of ultra-high molecular weight polyethylene. Its spherical radius allows excellent articulation to the spherical head of the mandibular component. We decided to use a customized prosthesis because it is easier to adapt at the mandibular ramus, eliminating adjustments; the occlusion is better achieved; the length of the surgery is smaller and, consequently, the morbidity and postoperative pain are reduced. Because of the rigidity of his cervical spine and limitation of mouth opening, the induction of general anesthesia was performed by fiberoptic nasoendoscopy. During the surgery, a bodily tilt of the operating table by 20 degrees on each side was required due to the rigidity of his cervical spine. Surgical access was through bilateral preauricular and submandibular incisions. Via the preauricular approach, the affected condyle was removed, the glenoid fossa was smoothed, and the articular component of the prostheses was inserted (
Figure 3A,B). From the submandibular incision, the coronoid process was removed and the condylar implant inserted. The same operative sequence was done on the opposite side (
Figure 4A,B). Postoperative CT confirmed correct placement of the total joint prostheses (
Figure 5A,B). Wooden spatulas and a Therabite (Atos Medical, West Allis, WI) appliance were used for postoperative physiotherapy, and interincisal distance has been maintained at 20 mm at 1-year follow-up (
Figure 6).
Discussion
AS is an inflammatory chronic arthritis of the spine always involving the sacroiliac joints and in more severe cases can include peripheral joints. The prevalence of this disease in the general population is approximately 0.1% [
2], and there is a male preponderance with a male-to-female ratio varying between surveys from 2.4:1 to 18:1 [
2,
5]. AS causes many debilitating postural characteristics that may affect the function of the entire musculoskeletal system. As the disease progresses and the ankylosis of the spine advances, the posture becomes representative of the disease. In this case report, the patient had to move his entire trunk to change his field of vision. Although TMJ involvement is frequent in patients with AS [
7], there are few documented cases of ankylosis [
8,
10]. To our knowledge, TMJ ankylosis in Brazilian patients associated with AS is not reported to date.
AS has a tendency to involve fibrocartilaginous structures such as the symphysis pubis and intervertebral disks. The sternomanubrial and sternoclavicular joints are also often affected. Therefore, the involvement of the TMJ is of interest in this respect because its joint surfaces are also fibrocartilaginous [
2]. Although previous studies on involvement of the TMJ exist [
1,
2,
3,
4], this has not been considered in recent publications [
8], and progression to complete ankylosis is particularly exceptional.
Concerning the pathogenesis of this disease, two potential mechanisms were described. One explanation addresses the destruction of the capsular/disc attachment, resulting in internal derangement and subsequent degenerative joint disease. The other could be a primary synovitis with direct breakdown of the articular surfaces. Internal derangement would then result from articular surface changes and not precede them [
7]. However, the debilitating postural changes of the disease and its effects may produce TMJ symptoms although the joints may not be involved. The TMJ involvement may be a result of spasm muscle, occlusal factors, and postural imbalance of the neck, rather than of the disease itself. Therefore, initial treatment should be directed toward alleviation of the muscle spasm-pain cycle of the TMJ [
1]. In this case report, we did not treat the patient initially with alleviation with of muscle spasm considering the severity extension of the disease. The improvement of signs and symptoms would be minimal with this choice of therapy. In addition, a gap arthroplasty was not performed initially concerning the increased risk of reankylosis and anterior open bite, especially in bilateral gap arthroplasty cases, as reported previously in the literature [
11].
In this case, the most important concern during surgery was related to the protection of the cervical spine, as the most serious complication encountered in AS is spinal fracture. Even minor trauma to the rigid, fragile spinal column can cause severe damage. Fracture at this site can result in quadriplegia or more severe neural symptoms. AS produced in this patient a rigid “bamboo spine” which restricts neck movement. TMJ involvement also restricted mouth opening. Thus, the induction of general anesthesia was performed by nasoendoscopy with extreme difficulty. In addition, during the surgery, planning the operating table to each side was required to protect the spinal column and avoid these complications.
Despite the long history of total alloplastic TMJ reconstruction, only one study to date has evaluated postsurgical mandibular motion patterns in these patients. The masticatory patterns and range of motion (maximal incisal opening [MIO], protrusion, and lateral excursion) in patients who have had unilateral and bilateral TMJ replacement with an alloplastic prosthesis, were compared with each other and to normal controls. The authors observed that MIO and maximum protrusion were significantly lower for the bilateral group when compared with the control group, with mean values of 24.9 ± 6.2 mm compared with 49.6 ± 5.3 mm for MIO, and 2.5 ± 2.7 mm compared with 6.7 ± 2.1 mm for protrusion, respectively [
12]. After 1-year follow-up, the patient shows an adequate interincisal distance of 20 mm, which was maintained after 2 years and 3 months, and this value is within the expected range in accordance with the previous study. This was achieved not only due the operation, but also after postoperative self-physiotherapy. We recommended opening and closing mouth movements (10 times), left and right laterality (10 times), and protrusion (10 times). These exercisers are repeated during 20 minutes, eight times in a day, until the patient reached a bearable level of pain, during at least 6 weeks. Concerning the prosthesis used in this case report, we expect minimum wear debris, which is clinically irrelevant, and no foreign reaction.
Although the TMJ rarely represents a severe problem for AS patients, the disease has a tendency to involve fibrocartilaginous structures. Because of the fibrocartilaginous surfaces of the TMJ, it is imperative to examine the TMJ in every patient with AS as an early screening method for this rare complication.