Abstract
Objective assessment of head shape has been an elusive goal in the management of craniosynostosis patients. Clinical judgment, craniometric indices, and computed tomography scans are the primary means through which a surgeon assesses this patient population. The purpose of this study was to examine and discuss the utility of the STARscanner for evaluation of surgical outcomes in metopic synostosis patients. A retrospective chart review of patients with metopic synostosis who underwent frontoorbital advancement with pre- and postoperative STARscanner imaging at Texas Children’s Hospital was performed. Two patients were identified and evaluation and discussion of the data produced by the STARscanner was undertaken. A novel symmetry index created by the authors, called the anterior–posterior volume ratio (APVR), was discussed for use in metopic synostosis patients. The postoperative growth metrics demonstrated an interval increase compared with the preoperative data. The anterior symmetry ratio, posterior symmetry ratio, overall symmetry ratio, cranial vault volumes, cranial vault asymmetry index, and cephalic ratio were not found to be useful in evaluating resolution of dysmorphology after fronto-orbital advancement in metopic synostosis. The APVR does not characterize dysmorphology, but may help show degree of expansion of the anterior cranial vault after fronto-orbital advancement. The STARscanner imaging device does not appear to have significant utility in characterizing head shape for surgical outcomes assessment in metopic synostosis. The minor utility of this device may be that it is a safe and fast way to derive growth parameters for both short-term and long-term follow-up of cranial vault remodeling.
Craniosynostosis occurs in approximately 1 in 2,500 live births. The most common forms of craniosynostosis are sagittal (40–55%) and unilateral coronal (20–25%), with lamboidal (0–5%) being the rarest [1]. Metopic synostosis has been reported to occur in 5 to 15% of cases, but recent reports have noted an increased incidence up to 28% [2].
Metopic synostosis leads to an abnormal head shape termed trigonocephaly. The deformity is characterized byfrontotemporal narrowing, midline forehead prominence, and increased biparietal width in early infancy [3]. This abnormal head shape develops as a result of restricted growth in the anterior cranial vault with compensatory changes in the middle and posterior vaults.
Cranial vault remodeling is the mainstay of treatment for patients with metopic synostosis. The primary surgical goals are normalization of head shape and reversal of craniofacial dysmorphology [4,5]. Multiple indices have been developed utilizing computed tomography (CT)-based craniometric and caliperbased anthropometric analysis to quantify outcomes assessment in synostosis surgery without a clear standard emerging [6,7]. The vast majority of indices are created using linear distances between various internal and external landmarks in an attempt to quantify cranial asymmetry and dysmorphology. These indices along with clinical judgment are used in practice to evaluate surgical outcomes after cranial vault remodeling. Formal, reproducible quantification of head shape is necessary to objectively characterize both the pretreatment cranial dysmorphology and the success of surgical outcomes.
The STARscanner (Orthomerica, Orlando, FL) is a relatively new imaging modality that uses safe low-energy lasers to capture and quantify head shapes in infants. To date, the primary application is for deformational plagiocephaly. In practice, orthotists use the measurements obtained by the STARscanner to make cranial remolding orthoses and assess therapy outcomes. According to Plank et al., the STARscanner is accurate to within 0.5 mm, acquires the data in less than 2 seconds, and generates commonly used anthropometric indices accurately [8].
The purpose of this study was to determine the utility of the STARscanner for evaluation of surgical outcomes in metopic synostosis patients. We conducted a small case series evaluating the application of pre- and postoperative STARscanner data for patients with metopic synostosis. Also, a novel craniometric index for metopic synostosis, called the anterior–posterior volume ratio (APVR), was proposed for assessment of anterior vault expansion.
Methods
An institutional review board-approved retrospective pilot analysis and discussion were performed to assess the utility of a novel imaging modality, the STARscanner, for use in the management of metopic craniosynostosis. Patients who had undergone fronto-orbital advancement for metopic synostosis between 2008 and 2011 at our institution were identified. Only patients with pre- and postoperative STARscanner imaging were identified. All patients had successful correction of cranial dysmorphology (Figure 1 and Figure 2). Patients were excluded if they had concurrent positional plagiocephaly or synostosis of another suture. Two patients were identified that met the inclusion criteria and had both pre- and postoperative scans. These patients were male identical twins. Both patients underwent fronto-orbital advancement by a single plastic surgeon at the ages of 10 and 11 months. The surgeries were staggered by 21 days so that the parents would not have two babies in the hospital at once. Data are presented for discussion purposes as the limited sample size makes it difficult to evaluate. Identifiable information was removed and the subjects were assigned study numbers.
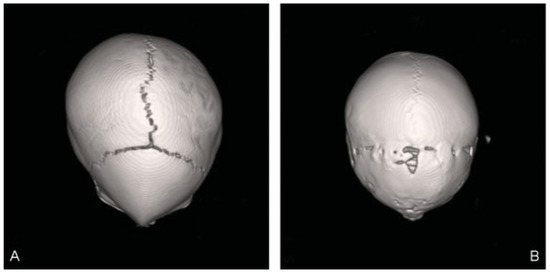
Figure 1.
A 3-D computed tomography reconstruction of patient 1 demonstrating successful resolution of trigonocephalic deformity: (A) 1 month preoperatively and (B) 17 months postoperatively. 3-D, three dimensional.
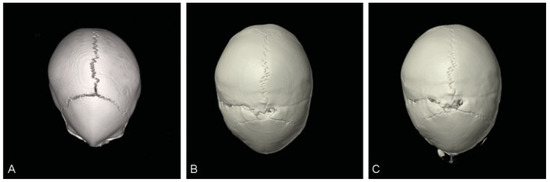
Figure 2.
A 3-D computed tomography reconstruction of patient 2 demonstrating successful resolution of trigonocephalic deformity: (A) 2 months preoperatively, (B) 12 months postoperatively, and (C) 20 months postoperatively. 3-D, three dimensional.
All data was collected using a single STARscanner imaging acquisition system and by a single certified orthotist. This device uses multiple surface lasers to generate a three dimensional (3-D) reconstruction of the patients head based on external landmarks. While the infant is supine, the images are acquired with four eye-safe lasers in approximately 2 seconds. The raw output of the STARscanner is a 3-D representation of the patients head. A certified orthotist technician then denotes a set of soft tissue landmarks on the 3-D image: sellion, left tragus, and right tragus. These landmarks allow the computer to generate an axial reference plane (level 0) and 10 parallel axial planes extending to the vertex of the cranium, similar to a CT scan, which are then used to calculate multiple linear measurements (Figure 3). Level 2 defines the skull base, which is made by a plane that extends from the brow parallel to level 0. The STARscanner software uses the linear measurements to calculate anthropometric indices for each of the 10 levels. These levels are then combined by the software to generate volumetric data for the anterior and posterior segments of the cranial vault. The volume measurements divide the cranial vault into four distinct quadrants, two anterior (left Q1, right Q2) and two posterior (right Q3, left Q4). The left and right segments are defined by a line from the sellion that runs perpendicular to a line made between the left and right tragus. The anterior and posterior portions of the cranium are defined by the tragia bilaterally (Figure 4). The oblique diagonals 1 and 2 are measurements of the anterior to posterior distance of the cranial vault at 30 degree angles from the center. Cranial breadth is the measurement of the width of the cranial vault, and cranial length is the anterior–posterior distance. Upper facial right and left measurements represent the distance from the tragus to the sellion.
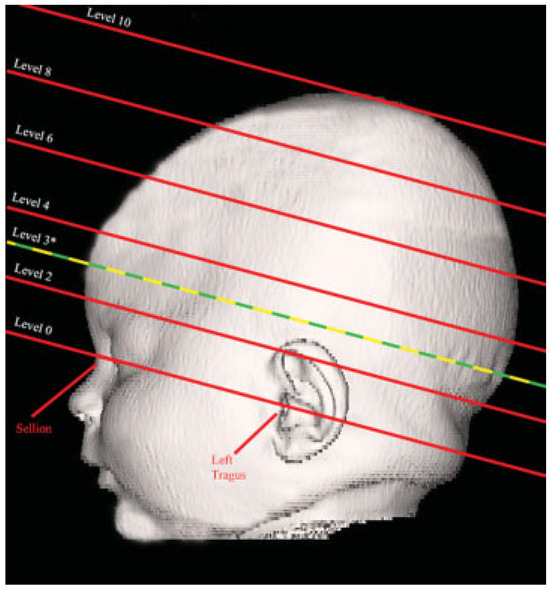
Figure 3.
Schematic representation of the levels for which the STARscanner produces linear measurements and the landmarks that are used for acquisition. * Level 3 was determined to be the most useful plane for analysis.
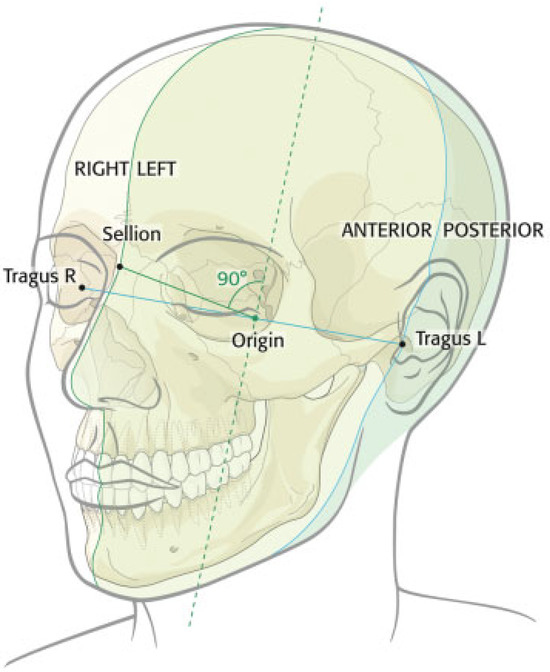
Figure 4.
Line connecting the tragia delineates the anterior and posterior segments and a line from the selion perpendicular to this line divides the cranium into the left and right segments.
The symmetry indices calculated by the STARscanner software that are used in our analysis are the cephalic ratio (CR), anterior symmetry ratio (ASR), posterior symmetry ratio (PSR), overall symmetry ratio (OSR), and the cranial vault asymmetry index (CVAI). The CR is calculated by dividing the cranial length by the cranial breadth, and is similar to the commonly used cranial index. The ASR is calculated by dividing the smaller of Q1 and Q2 by the larger anterior quadrant volume. The PSR is similarly calculated by dividing the smaller of Q3 and Q4 by the larger posterior quadrant volume. OSR is the mean of the ASR and PSR. A ratio of 1 for ASR, PSR, and OSR represents perfect volumetric symmetry. The CVAI is generated by taking the difference between the two oblique measurements at 30 degrees (oblique–diagonal) and dividing by the larger of the two oblique–diagonal lengths. A CVAI of zero represents ideal symmetry.
The radial symmetry index (RSI) is an index that is unique to the STARscanner. The RSI is calculated by summing the absolute values of the differences in length of adjacent radii from the center of the axial plane to the cranium at 15 degree increments. An RSI of zero means the shape is a circle, with all radii having the same length.
Given the unique head shape characteristics of trigonocephaly, we proposed that comparing the anterior to posterior volumes pre- and postoperatively might prove to be a useful index of postoperative change. Both surgical procedures aim to expand the anterior vault volume, so analyzing the change in anterior cranial volume relative to change in posterior volume may prove to be an indicator of successful expansion of the anterior cranium postoperatively. We termed this new index the APVR. It is calculated by summing the anterior volumes (Q1 and Q2) and dividing by the sum of the posterior volumes (Q3 and Q4). A descriptive summary of the various data points generated by the STARscanner is presented in Table 1.

Table 1.
Descriptive summary of the data points produced by the STARscanner imaging device.
All analyzed linear data points were generated by the STARscanner device at the axial plane designated as level 3 since it contains the maximum circumference, length, and width measurements for the head.
Results
Age at time of preoperative scan was 8 months for both patients. Fronto-orbital advancement was performed in the patients at 10 and 11 months of age. Postoperative imaging was acquired at 14 months of age in both patients (Table 2). Table 3 demonstrates the pre- and postoperative measurements and symmetry indices generated by the STARscanner that were used for assessment. The circumference, cranial length, and cranial breadth demonstrated an expected, overall increase when compared with the preoperative variables. No statistical analysis was performed given the limited sample size. Moreover, a formal comparison of the two types of surgical approaches for metopic synostosis is beyond the scope and the intent of this publication.

Table 2.
Age at time of operation, preoperative scan, and postoperative scan.

Table 3.
All pre- and postoperative data generated by the STARscanner device for each patient.
The oblique diagonal differences decreased for patient 1 (7.4–3.0) and patient 2 (9.9–2.2). This was a result of a shorter oblique diagonal line originating from the posterior left side of the head in both patients. In addition, the right and left posterior volumes demonstrated large differences within patients preoperatively. The right posterior volume was 9.4% larger than the left posterior volume for patient 1 (Q3 = 245.7 and Q4 = 224.6) and 9.2% larger in patient 2 (Q3 = 252.9 and Q4 = 231.6). These results represented a degree of left sided deformational plagiocephaly in both patients in addition to the metopic synostosis.
The CR decreased for patients 1 (0.79–0.75) and 2 (0.81–0.79). The RSI decreased in patient 1 (29.9–13.4) and patient 2 (30.6–12.0). The ASR decreased in patient 1 (0.97–0.95) and increased in patient 2 (0.91–0.99). The PSR increased in patient 1 (0.91–0.96) and patient 2 (0.92–0.95). The OSR increased in patient 1 (0.94–0.96) and patient 2 (0.91–0.97). The CVAI decreased in patient 1 (5.1–2.0) and patient 2 (6.8–1.4). Volume measurements increased in all four quadrants for all patients. The APVR increased in patient 1 (0.91–0.96) and patient 2 (0.94–1.01). This ratio increased in both patients since the anterior cranial vault was expanded with surgery relative to the posterior vault.
Discussion
Establishing a reproducible and objective method for quantifying metopic craniosynostosis surgical outcomes has been an elusive goal; however, it is necessary in order for surgeons to objectively evaluate outcomes and assess the longevity of the reconstruction. To date, evaluation of surgical outcomes was based on visual impact assessment, aided by anthropometric data and CT scans. These methods have limitations. Whitaker et al. (1987) established an early classification system for assessing surgical outcomes in craniosynostosis based on need for surgical revision as deemed by the surgeon [9]. Although this scale was clinically meaningful and allowed rudimentary analysis of outcomes, it was inadequate in scope for quantitative assessment of the surgical result. Anthropometric data are useful in evaluation of surgical outcomes given that large normative databases are available for comparison [10,11,12,13]. However, the way in which this data are generated—caliper assessment and CT—lends room for improvement. Caliper-based anthropometric assessment is difficult, time-consuming in young children, and highly dependent on the skill and experience of the observer [14,15]. CT evaluation is constrained by cost, possible need for anesthesia, and radiation exposure. Several studies have indicated a possible increased risk of neoplasm with childhood exposure to CT, making it prudent to reduce CT utilization whenever possible [16,17]. It is imperative to explore novel, noninvasive imaging modalities for evaluation of surgical outcomes.
The laser surface imaging system, STARscanner, has been used with success in quantifying head shape for patients with deformational plagiocephaly before and after helmet therapy [8]. It provides a fast, safe, and accurate means to generate craniometric data and may make an ideal device to facilitate quantification of surgical outcomes for craniosynostosis. Whether the STARscanner data are useful or relevant for patients with metopic craniosynostosis, or any type of synostosis, is unclear. Our study sought to discuss the application and utility of this device in quantifying surgical outcomes in metopic synostosis patients by presenting a small case series.
Symmetry indices are important in the evaluation of craniosynostosis. In this study, we looked at several commonly used anthropometric indices and several unique indices generated by the STARscanner imaging system. The unique symmetry indices generated by the STARscanner are the ASR, PSR, OSR, and RSI. The ASR, PSR, and OSR displayed variable trends in our study, with some patients demonstrating increasing values in one set of data and simultaneously demonstrating decreasing values in another. Given that metopic synostosis is a symmetric deformity in regards to right and left, it is reasonable to say that these indices will not help quantify a deformity that is characterized by stark differences between the anterior skull and posterior skull. Also, the ASR, PSR, and OSR are solely based on volume measurements and give no indication of cranial dysmorphology or head shape that we can discern. How volume reflects contour or skull shape is impossible to tell. Even if the postoperative volume changes are equal between segments, there is no way to determine if these changes were symmetric. These volume based indices are not useful for assessment of metopic synostosis surgical outcomes. It is possible that these may be helpful when unilateral asymmetry is more pronounced, such as in unicoronal synostosis, lamboidal synostosis or deformational plagiocephaly as seen in the study by Plank et al. (2006) [8]. The role of the RSI for evaluation of craniosynostosis is unclear. Plank et al., found RSI to be a useful indicator of asymmetry for deformational plagiocephaly [8]. It is difficult to discern what the value of the RSI indicates. It is understood that a value of zero indicates a perfect circle, but ideal head shape is not meant to mimic a circle. If development of a normative database is undertaken, this may help establish a numerical value for RSI that represents the desired postoperative head shape.
The established anthropometric indices (CVAI and CR) are not helpful for metopic synostosis, as they both fail to capture the symmetric deformity of trigonocephaly. The cranial index, referred to as CR in our study, is a commonly used symmetry index for sagittal synostosis management. The CVAI, which is typically used in deformational plagiocephaly and unicoronal synostosis, is a useful measure of cranial vault asymmetry [18]. The CVAI is more useful in types of synostosis that cause unilateral differences, not metopic synostosis which causes a symmetric deformity of the right and left portions of the skull. Even though it was found to decrease postoperatively in our small study, it is difficult to ascribe meaning to this. These results along with the oblique diagonal difference and the difference in posterior volumes preoperatively were likely a result of left-sided deformational plagiocephaly that decreased in the postoperative period. The STARscanner’s ability to quickly and safely generate commonly used anthropomentric data and indices (CR and CVAI) may prove useful in evaluation of outcomes for patients with other types of craniosynostosis, such as using CR for sagittal synostosis or CVAI for unicoronal synostosis, but further studies need to be undertaken.
For metopic synostosis, the APVR was not helpful in determining resolution of cranial dysmorphology. The APVR values did demonstrate increasing values, which is indicative of a greater increase in the anterior volume relative to the posterior volume after surgery. This is, however, an index derived from volume measurements and does not give the surgeon any concept as to how the global skull shape and contour has changed. It may prove useful for quantifying change in the anterior vault relative to the posterior vault for the purposes of quantifying the degree of correction during fronto-orbital advancement in metopic synostosis patients. This quantification could potentially allow for surgeons to study the ideal amount of correction needed during expansion of the anterior cranium in these procedures using the APVR and clinically successful outcomes.
The ability to safely and quickly evaluate cranial growth parameters in craniosynostosis without the attendant risk of increased radiation exposure is the primary advantage of this technology in metopic synostosis. Two variables that are commonly used for postoperative growth monitoring are head circumference and volume. These are validated indicators of postoperative cranial growth and are easily produced by the STARscanner [19,20]. In our study, we observed cranial growth postoperatively as evidenced by increasing circumference and volume measurements (Q1–Q4) in all patients. Even though cranial growth parameters have an unclear relationship with craniofacial dysmorphology or intracranial pressure, growth monitoring at multiple time points should be a part of the postoperative analysis in these patients [20]. Fearon et al. (2009) found that postoperative skull growth in these patients is restricted and that there is a tendency for the deformity to recur in the years following the operation as a result of skull growth arrest. According to their report, growth restriction is most pronounced perpendicular to the affected suture and more severe for patients with metopic synostosis who had an operation at an earlier age [19]. Dramatic decreases in growth velocities of circumference or volume during follow-up may provide the first clue to growth restriction after surgery. The STARscanner’s ability to generate craniometric data and volume calculations may provide a fast and easy way to follow skull growth. This would allow postoperative monitoring both in the short-term and long-term without the use of ionizing radiation or time-consuming manual anthropometric measurements.
The obvious limitation of this study was the small sample size and lack of statistical analysis. This limited the study to a discussion of the potential utility of the STARscanner, rather than validating its use. One limitation of the STARscanner lies in the fact that a user has to determine soft tissue landmarks on the patient. These landmarks determine the reference plane and all subsequent measurements. If the reference plane is distorted or incorrect, all other planes from which measurements are generated will be incorrect as well. This introduces reliability and accuracy issues. Also, patient motion can adversely affect the 3-D rendition and output data; however, this is easily seen during acquisition and can then be corrected for by repeat examination. Another potential drawback of the STARscanner is that it is a surface scanner and derives all its measurements based on the skin surface and not the bony surface. Temporal hollowing, that is commonly seen after cranial vault remodeling due to manipulation of the temporalis muscle, may lead to decreased circumference and volume measurements. In our institution, the temporalis muscle is elevated with the coronal flap in fronto-orbital advancement. This technique helps prevents manipulation of the temporalis muscle and helps mitigate temporal hollowing.
Conclusions
The STARscanner imaging device does not appear to have significant utility in characterizing craniofacial dysmorphology for surgical outcomes assessment in metopic synostosis. The craniometric indices that are unique to the STARscanner are based on volume measurements and do not help the surgeon characterize successful resolution of dysmorphology after surgery. The minor utility of this device may be that it is a safe and fast way to derive growth parameters (i.e., circumference and volume) from metopic synostosis patients for both short- and long-term follow-up. The APVR is not useful for characterizing the dysmorphology of metopic synostosis; however, it may prove useful for quantifying the degree of expansion of the anterior cranial vault.
Acknowledgments
None.
References
- Cohen, M.M., Jr. Epidemiology of craniosynostosis. In Craniosynostosis, 2nd ed.; Cohen, M.M., Jr., MacLean, R.E., Eds.; Oxford University Press: New York, NY, USA, 2000; pp. 112–118. [Google Scholar]
- Kolar, J.C. An epidemiological study of nonsyndromal craniosynostoses. J Craniofac Surg 2011, 22, 47–49. [Google Scholar] [CrossRef] [PubMed]
- Oi, S.; Matsumoto, S. Trigonocephaly (metopic synostosis). Clinical, surgical and anatomical concepts. Childs Nerv Syst 1987, 3, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Hankinson, T.C.; Fontana, E.J.; Anderson, R.C.E.; Feldstein, N.A. Surgical treatment of single-suture craniosynostosis: An argument for quantitative methods to evaluate cosmetic outcomes. J Neurosurg Pediatr 2010, 6, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Engel, M.; Thiele, O.C.; Mühling, J.; et al. Trigonocephaly: Results after surgical correction of nonsyndromatic isolated metopic suture synostosis in 54 cases. J Craniomaxillofac Surg 2012, 40, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Bottero, L.; Lajeunie, E.; Arnaud, E.; Marchac, D.; Renier, D. Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 1998, 102, 952–958; discussion 959–960. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Correa, S.; Starr, J.R.; Lin, H.J.; et al. New severity indices for quantifying single-suture metopic craniosynostosis. Neurosurgery 2008, 63, 318–324; discussion 324–325. [Google Scholar] [CrossRef] [PubMed]
- Plank, L.H.; Giavedoni, B.; Lombardo, J.R.; Geil, M.D.; Reisner, A. Comparison of infant head shape changes in deformational plagiocephaly following treatment with a cranial remolding orthosis using a noninvasive laser shape digitizer. J Craniofac Surg 2006, 17, 1084–1091. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, L.A.; Bartlett, S.P.; Schut, L.; Bruce, D. Craniosynostosis: An analysis of the timing, treatment, and complications in 164 consecutive patients. Plast Reconstr Surg 1987, 80, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G.; Hreczko, T.M.; Katic, M.J.; Forrest, C.R. Proportion indices in the craniofacial regions of 284 healthy North American white children between 1 and 5 years of age. J Craniofac Surg 2003, 14, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G.; Katic, M.J.; Forrest, C.R. Anthropometric proportion indices in the craniofacial regions of 73 patients with forms of isolated coronal synostosis. Ann Plast Surg 2005, 55, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Marcus, J.R.; Domeshek, L.F.; Loyd, A.M.; et al. Use of a three-dimensional, normative database of pediatric craniofacial morphology for modern anthropometric analysis. Plast Reconstr Surg 2009, 124, 2076–2084. [Google Scholar] [CrossRef] [PubMed]
- Waitzman, A.A.; Posnick, J.C.; Armstrong, D.C.; Pron, G.E. Craniofacial skeletal measurements based on computed tomography: Part II. Normal values and growth trends. Cleft Palate Craniofac J 1992, 29, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Rekate, H.L. Occipital plagiocephaly: A critical review of the literature. J Neurosurg 1998, 89, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Watson, G.H. Relation between side of plagiocephaly, dislocation of hip, scoliosis, bat ears, and sternomastoid tumours. Arch Dis Child 1971, 46, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.J.; Elliston, C.D.; Hall, E.J.; Berdon, W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001, 176, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Pearce, M.S.; Salotti, J.A.; Little, M.P.; et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet 2012, 380, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Loveday, B.P.T.; de Chalain, T.B. Active counterpositioning or orthotic device to treat positional plagiocephaly? J Craniofac Surg 2001, 12, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Fearon, J.A.; Ruotolo, R.A.; Kolar, J.C. Single sutural craniosynostoses: Surgical outcomes and long-term growth. Plast Reconstr Surg 2009, 123, 635–642. [Google Scholar] [CrossRef] [PubMed]
- McKay, D.R.; Davidge, K.M.; Williams, S.K.; et al. Measuring cranial vault volume with three-dimensional photography: A method of measurement comparable to the gold standard. J Craniofac Surg 2010, 21, 1419–1422. [Google Scholar] [CrossRef] [PubMed]
© 2013 by the author. The Author(s) 2013.