The frontal bone is the strongest component of the craniofacial skeleton. Frontal sinus fractures account for 5 to 15% of all maxillofacial fractures and are usually the result of highvelocity impact during events such as motor vehicle collisions, sports activities, and industrial accidents.
Displaced and comminuted fractures with esthetic and functional impairment require surgical treatment and reconstruction, whereas fractures with no or minimal displacement and no edema are managed conservatively. The goal of frontal sinus fracture management is to create a safe sinus, restore facial contour, and avoid short-term and long-term complications. The best surgical approaches are coronal and hemicoronal, although fractures can also be approached through an existing forehead laceration. If wider access is required, an existing laceration can be extended to improve the surgical field of view and access [
1].
Open reduction is important to restore the bone fragments to their approximate premorbid positions, which can be maintained with internal fixation hardware. Bone grafts are occasionally required for the treatment of severely comminuted fractures that do not allow adequate reduction and fixation [
2]. Severe comminution of the anterior table (with or without involvement of nasofrontal recess injury) may make open reduction with the existing bone fragments very challenging. Mucosal disruption can result in a nonfunctional sinus postoperatively. In this unusual situation, sinus obliteration may be required.
In this article, we introduce a rapid and simple method for the treatment of frontal fractures and restoration of normal forehead contour, named the “bone mesh pull-up technique” (BMPUT). We describe our experience with this technique in seven trauma cases, with emphasis on the technical aspects and clinical results of this new simple method. The BMPUT facilitates the reduction of comminuted anterior-table frontal fractures.
Patients and Methods
Between 2010 and 2011, we treated seven patients who presented at our clinic with comminuted fractures of the anterior table and esthetic deformity of the frontal bone using the BMPUT. Given the retrospective nature of this study, it was granted an exemption in writing by our local institutional review board (
Table 1).
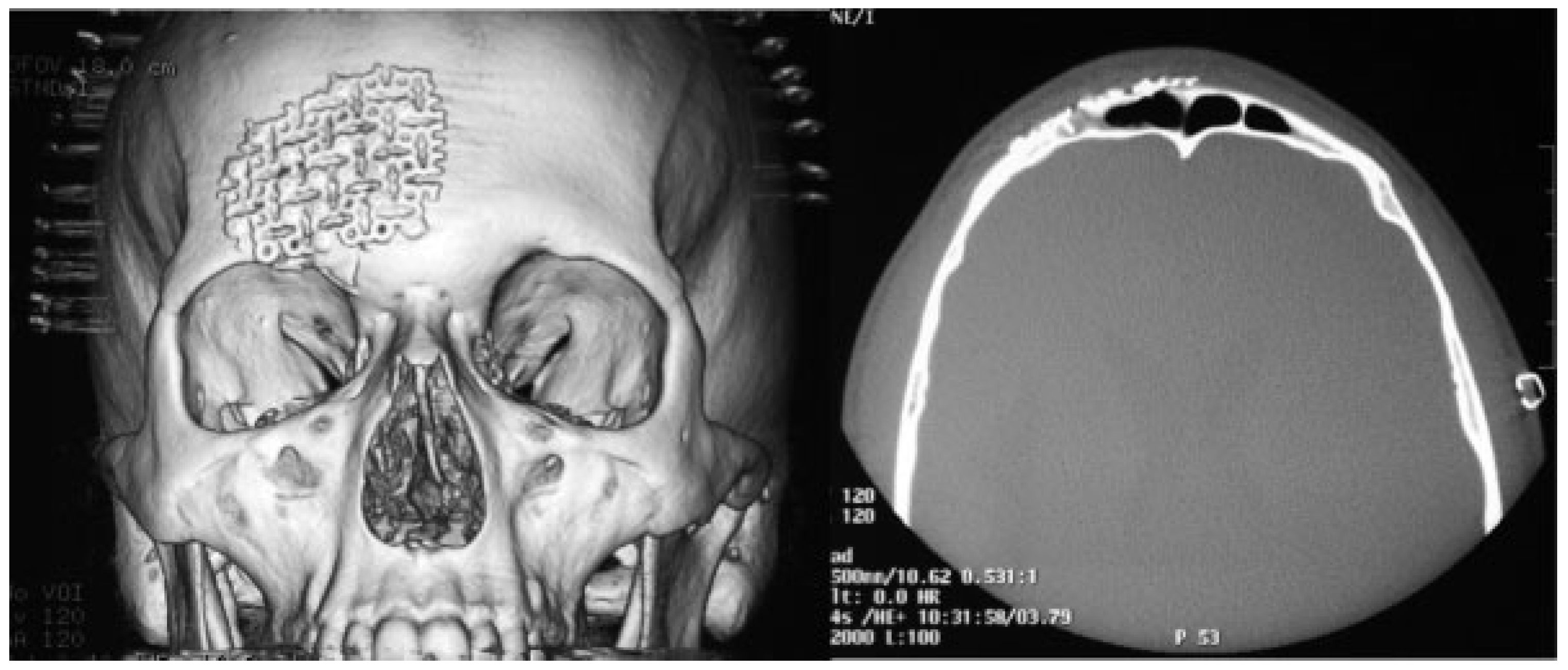
All patients underwent preoperative and postoperative computed tomography (CT) with three-dimensional (3D) reconstruction. The average clinical observation time was 12 months (
Figure 1).
3D CT is the gold standard for the examination of facial fractures; it allows visualization of the degree of frontal sinus fracture and precise planning of surgical correction [
3,
4]. Most injuries in our sample resulted from traffic accidents, and all surgeries were performed within 3 weeks of injury. Surgery to reduce, reconstruct, and fix the fracture was performed under general anesthesia and patients received antibiotics to prevent infection associated with fracture and surgery even for closed anterior table frontal sinus fractures for 2 weeks from diagnosis [
5].
Surgical Technique (BMPUT)
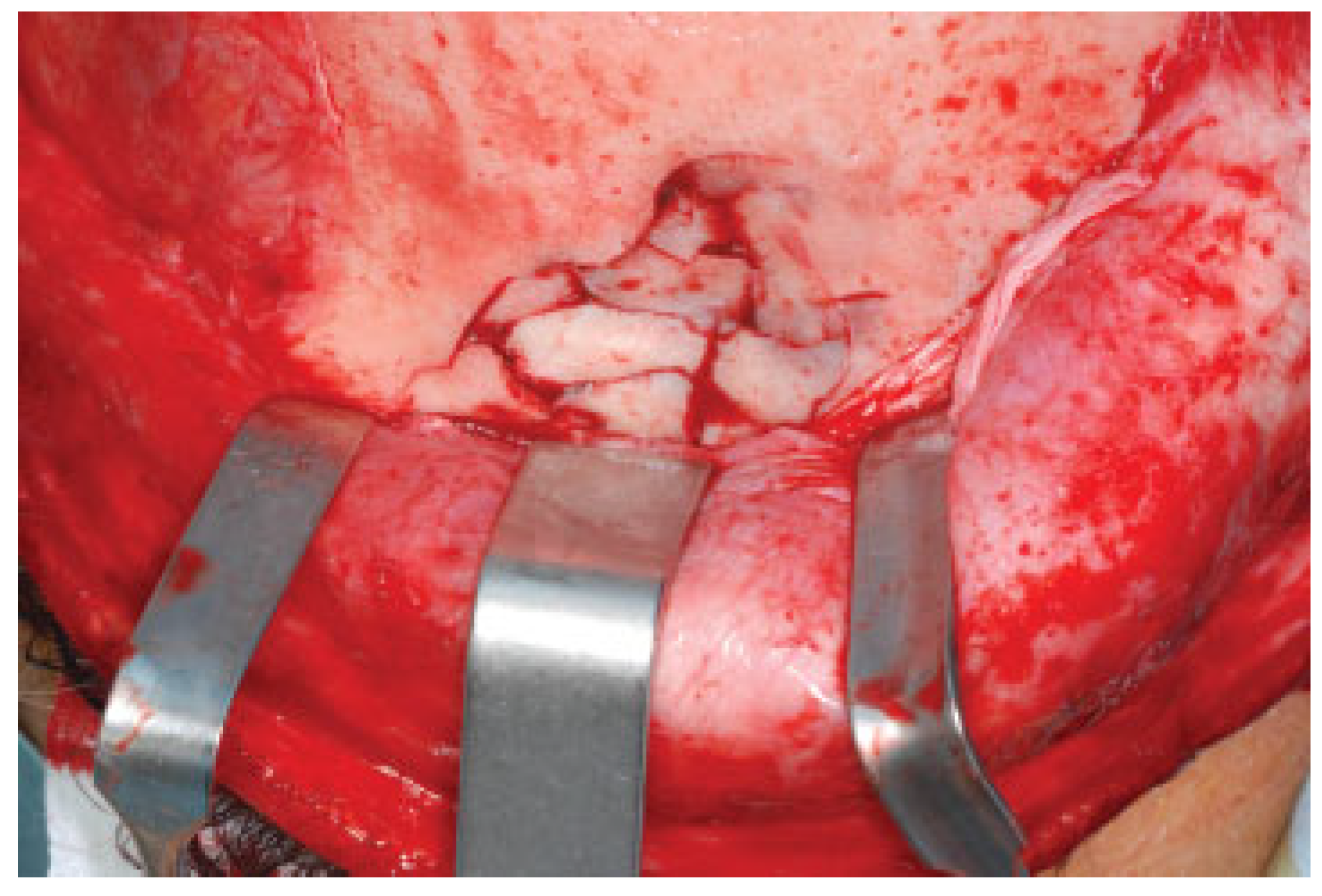
In all patients, a coronal approach was used to expose the comminuted frontal fracture (
Figure 2). Titanium mesh was adapted to the defect and positioned as a template. The central portion of the mesh was then pressed into the defect so that its shape corresponded to the natural inner-table contour (
Figure 3A,B). Each bone fragment was then fixed to the mesh with a mini-screw (
Figure 4A,B). If nonstretching mesh is used, it must be contoured before it is fixed. After fixing all comminuted fragments, we removed the mesh and restored the frontal contour by simultaneously manipulating bone fragments and mesh (
Figure 5A,B). Finally, we fixed the mesh to the intact frontal bone with mini-screws, thereby achieving a perfectly restored frontal sinus contour (
Figure 6).
Results
No complication was observed in all treated cases during 12 months of clinical observation. A good esthetic result with satisfaction of patients was reached. The average time related to the manipulation of bone fragments and their fixation with bone mesh (BMPUT) was 35 minutes.
Discussion
The treatment of frontal sinus fractures is complex and sometimes controversial. The surgical repair of an isolated anterior-table fracture fulfills a primarily esthetic purpose and is generally achieved with open reduction and internal fixation [
6].
The ideal material for plates, mesh, and screws used in fracture management is chemically inert, biocompatible, nonallergenic, noncarcinogenic, cost effective, sterilizable, easy to handle, and radiopaque [
7].
Lakhani et al. in 2001 emphasize the use of titanium mesh as a new option for the repair of severely comminuted fractures of the frontal sinus [
8]. Titanium mesh fulfills these criteria and has been used routinely in the treatment of orbital fractures with excellent results. Badie et al. described the restoration of dural and bone defects in anterior cranial fossa in particularly delicate situations after removal of cranial base tumors [
9]. Sekhar et al. described a similar technique used when free dural margin is not available to sew [
10].
It is thin and easy to contour and stabilize, it maintains its shape and retains all bone fragments, it minimizes delayed complications, and it produces fewer artifacts on CT images than other materials do [
7].
3D CT is fundamental for determination of the size and extent of the fracture and to choose the most appropriate surgical technique and material. Various approaches to frontal sinus fractures have been described; most access the forehead through a coronal or bicoronal incision or existing laceration [
3]. In recent years, surgeons have increasingly used the coronal approach because it provides a better surgical field of view and is associated with minimal postoperative complications, such as neural damage and facial scarring. Approaches through forehead incisions or the extension of small lacerations provide excellent exposure but can result in postoperative paresthesia and poorly hidden scars [
2].
No author has so far described in detail an easy method of fixing bone fragments in comminuted fractures of the anterior cranial vault. Inappropriate management of a frontal sinus fracture not only leads to cosmetic deformities, but it may also result in serious complications, including mucoceles development [
2]. The misdiagnosis of damage to the nasofrontal duct, located posteromedially in the sinus, can lead to this complication [
4]. To avoid mucoceles development, fracture management should include the removal of all frontal sinus mucosa and comminuted bone fragments, which can obstruct the nasofrontal duct, and the sealing of the duct with fat or alloplastic material [
11].
A CT scan with 2- and 3-mm slices should be done to assess the nasofrontal duct, which is very likely to be injured in cases of posteromedial frontal sinus fracture [
7]. It is important to underline the risk when brain and dura are involved, such as meningitis, brain abscess, and cerebrospinal fluid leak. The authors stress other potential complications related to the fixation of the fractured segment such as bone fragments resorption and loose of screw [
8].
The BMPUT is also best performed via a coronal approach, which enables restoration of the ideal frontal bone profile without scarring in the frontal region. The esthetic outcome resembles the preoperative situation. The BMPUT also allows the use of all bone fragments, including small (<1.5 cm) fragments that are typically removed because they are difficult to synthesize with conventional plates and screws. Thus, the continuity of the frontal sinus wall can be reconstructed without a graft, reducing the surgical time. Healing is also improved, sinus sealing is avoided, and the incidence of infective complications and mucoceles is reduced. Probably, the resorption of bone fragments and loose of screws fixation could be prevented from this surgical technique (
Figure 7).
Conclusion
BMPUT is a simple method for the treatment of comminuted fractures of the anterior frontal sinus wall, enables the use of most bone fragments while maintaining the anatomical relationships among them, and restricting the use of graft materials. These advantages ultimately yield a better esthetic result with a reduced procedure time and a lower incidence of complications.