Abstract
The aim of our study was to evaluate the biodegradable plates (PG910/PDO) for reconstruction of various sizes of the orbital floor defects in the blow-out fractures. We included patients who had an impure blow-out fracture. All patients had a recent trauma and also the surgical intervention was done between 1 and 10 days after trauma. The amount of the orbital floor defect was measured in each case through computed tomography scan. In the surgical intervention, a biodegradable plate was used for the reconstruction of the orbital floor defect along with titanium miniplates used for bone fixation in orbital rim. Due to aesthetic reasons, all patients underwent secondary surgery including removal of titanium miniplates after 18 months. The orbital floor was reevaluated during the removal of the miniplates. The clinical evaluation of remnant defects and biodegradable plates (presence of complete or partial resorption) were documented for each patient. In our study a total of 15 patients (10 males and 5 females) underwent the orbital floor reconstruction using biodegradable miniplates. The size of the orbital floor defects was meanly 3.51 1.29 cm2. Results demonstrated that 4 out of 15 patients had a remnant defect after resorption of the biodegradable plate. In 10 out of 15 patients, the biodegradable plates completely replaced with fibrous tissues after 18 months. Remaining five patients had partial resorption of plates. There was not any relationship between the defect size and the remnant defects (p > 0.05). A significant relationship was seen between the defect size and the plates’ resorption rate (p < 0.001). There is a significant relationship between the resorption rate and the remnant defect. The risk to have remnant defects have been increased as the plates had incomplete resorption. The use of biodegradable plates is an appropriate option for reconstruction of the orbital floor defects. The defect size does not have any effect on the stability of the plate. However, incomplete plate resorption increases the risk of remnant defects in the orbital floor. The larger defects lead to slow degradation of biodegradable plates.
The orbit is particularly susceptible to fractures because of its exposed position and thin bone [1]. Orbital floor fractures can be classified as pure blow-out fractures (isolated orbital floor fracture) or impure blow-out fractures (associated with an orbital rim fracture) [2]. Fractures of the orbital floor may cause severe aesthetic and functional deformities and present with diplopia, enophthalmos, displacement of orbital contents, restriction of ocular movements, and impaired facial appearance [3]. The aims of orbital floor reconstruction are restore orbital floor continuity, creating smooth surface, isolation from maxillary sinus, and restoration of orbital volume especially in sever enophthalmos. Several materials are available for reconstruction of orbital floor which consist of autologous, allogeneic, or alloplastic materials. Autologous materials include periosteum, nasoseptal cartilage, rib graft, and mandibular bone [1,4]. The disadvantages of using autolo-gous materials are unpredictable resorption and donor-site morbidity. Alloplast materials do not have such problems; they are permanent foreign bodies and cause late complica-tions such as infection, extrusion, and implant migration [5,6].
These complications may be avoided by using biodegradable implants [2]. Biodegradable materials consist of Poly (lactic acid), Poly (glycolic acid), PLA/PGA implants, polydioxanone and polyglactin 910/PDO implants [7]. Polyglactin 910/PDO (PG910/PDO) flexible membranes have been marketed worldwide under the commercial name Ethisorb (Johnson & Johnson, New Brunswick, NJ) for several years. PG910 (commercial name Vicryl) (Ethicon, Somerville, NJ) is a PLA/PGA copolymer with a weight ratio of PLA to PGA of 1:9, which is commonly used as a material for surgical sutures. It is widely used for reconstruction of orbital floor defects [8]. There are some questionable situations concerning the use of biodegradable plates including whether the biode-gradable plates would be used in the large defects of the orbital floor and the defect size leads to change resorption rate and stability of these plates.
The main purpose of this study was to evaluate the biodegradable plates (PG910/PDO) for reconstruction of var-ious sizes of the orbital floor defects in the blow-out fractures.
Methods and Materials
In this prospective study different parameters using biode-gradable plates for reconstruction of the blow-out fractures were assessed. The study was approved by the research committee of the medical ethics group of Shiraz University of Medical Sciences. The study sample was derived from the patients who referred to the Department of Craniomaxillo-facial Surgery for evaluation and management of orbital fracture between January 2009 and December 2010. Patients eligible for study inclusion had an impure blow-out fracture and there was a need to repair orbital floor and to fix the zygomaticomaxillary complex in a proper position. Patients who had pure blow-out fracture or minimal bone displace-ment in computed tomography (CT) scan views without the enophthalmos or the diplopia were excluded from the study. All the patients had a recent trauma and subsequently surgi-cal intervention was made between 1 and 10 days. A consul-tation was made with ophthalmologist before the surgical intervention. An axial and coronal CT scans were taken through 2-mm cuts for each patient before surgical interven-tion, immediate, and 18 months after surgery (Figure 1 and Figure 2). The amount of the orbital floor defect was measured in each case through CT scan. The surgical approach consisted of mid-lower incision for accessing the orbital rim and floor. Bone reduction and reconstruction was made through biode-gradable plate (PG910/PDO) (Figure 3). Titanium miniplates and screws were used for fixation of fractured infraorbital rim. The thickness of the biodegradable plates (PG910/PDO) was 0.5 mm. All the patients underwent secondary interven-tion to remove the titanium miniplates after 18 months. The orbital floor was reevaluated during the secondary interven-tion. The evaluation of remnant defects and biodegradable plates (complete or partial resorption) was made for every patient (Figure 4).
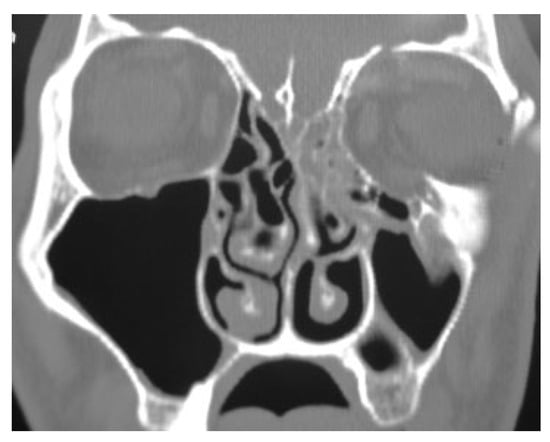
Figure 1.
A coronal view shows the left zygomatic mandibular fracture with the blow-out fracture.
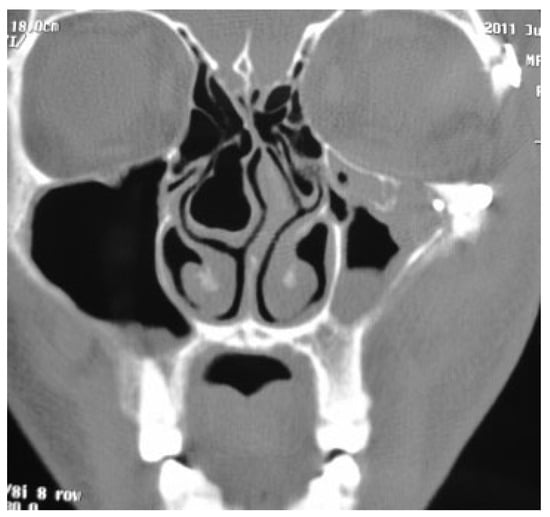
Figure 2.
A coronal view shows a remnant defect 18 months after reconstruction.
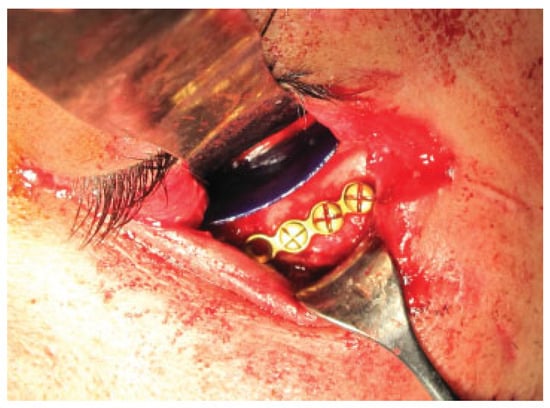
Figure 3.
Image demonstrates placing a biodegradable plate on the orbital floor.
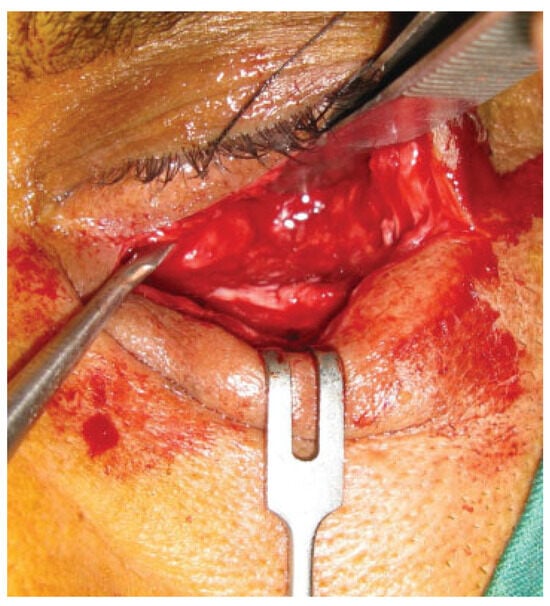
Figure 4.
Image shows a fibrous layer in the orbital floor 18 months after reconstruction without defect.
Statistical Analyses
The statistical analyses were performed using the statistical package SPSS for personal computer, version 19 company (IBM, New York, NY). A Pearson correlation test was used to evaluate the correlation between the defect sizes and pa-tients’ ages. We used independent t test to find a relationship between the defect size and the biodegradable plate condi-tion in the second operation. The Fisher exact test was used to assess the relationship between sex and the biodegradable plate in the secondary intervention.
Results
In our study 15 patients (10 males and 5 females) underwent the orbital floor reconstruction through the biodegradable plates (PG910/PDO). All the patients were between the ages 18 and 65 years and the mean of age was 36.6 13.9. The size of the orbital floor defects was meanly 3.51 1.29 cm2 (Table 1). Pearson correlation test showed no relationship between the orbital floor defect and age (p > 0.05).

Table 1.
Relationship between predictor factors and the remnant defects.
Results demonstrated that 4 out of 15 patients had remnant defects after the resorption of plate. In 10 out of 15 patients biodegradable plates were completely replaced with fibrous tissues after 18 months. In 5 out of 15 patients, partial resorption of plates was observed. There was no relationship between the defect size and the remnant defects (p > 0.05). A significant relationship was seen between the defect size and the plates’ resorption rate (p < 0.001). As a result, when a larger biodegradable plate was used to reconstruct the defect, the plates had partial resorption as compared with the smaller plates that had total resorption after 18 months (Table 2). There is a significant relationship between the resorption rate and the remnant defect. When the plates had incomplete resorption, the risk of the remnant defects to be encountered is increased. Evaluation of the data did not show any correla-tion between patients’ age, remnant defects, and plates’ resorption (p > 0.05). Sex did not have any impact on the defect size, remnant defects, and plates’ resorption (p > 0.05).

Table 2.
Correlation between predictor factors and the resorption condition.
Discussion
Several materials were suggested to repair orbital floor after blow-out fractures. Basically, the goal of an orbital floor implant is to repair the traumatic defect, lifting the eyeball into its correct position, and thereby avoiding enophthalmos. An ideal implant biomaterial should be biocompatible, avail-able in sufficient quantities, strong enough to support the orbital content and the related compressive forces, easy to shape to fit the orbital defect and regional anatomy, easily fixable in situ, not prone to migration, osteoinductive, and biodegradable with minimal foreign body reaction. To find a proper material for orbital floor reconstruction is not an easy task [7]. In our study, the outcome demonstrated that the defect size of the orbital floor did not have any relationship with the stability of the biodegradable plates. However, resorption rate would be significantly affected if the larger plate was used. On the other hand, the risk to be encounter with remnant defects would be increased through incomplete plate resorption.
Absorbable polymers have been widely used for more than 30 years in many fields of surgical practice, and in the 1990s absorbable plate–screw systems were commercially intro-duced as an efficient device for fixation of fractures in the craniomaxillofacial region [9]. Absorbable synthetic polymers exhibit interesting features, as they offer more controllable and predictable absorption kinetics than those of biological grafts and can be easily tailored to obtain an implant of the desired size and shape [10]. It is appeared that size of orbital floor is important to decision using of PG910/PDO sheets. Büchel et al studied 87 patients whose results showed that 21 patients (24.1%) experienced postoperative complications. Of these, only three patients (3.4%) had permanent complica-tions directly related to the Ethisorb membrane (diplopia, enophthalmos). Two of these patients required revision sur-gery. They concluded the effectiveness of Ethisorb in the repair of small-to-moderate orbital floor fracture defects (up to a maximum size of 2 × 2 cm) [2]. Recently one study showed that the reconstruction of moderate-to-extensive orbital floor fractures can be provided with polydioxanone foil or the Ethisorb patch without significant changes in orbital geometry [11]. Another study suggested that PDS is a suitable implant for orbital floor reconstruction with accept-able low rates of infraorbital hypesthesia, bulbus motility disturbances, and enophthalmos. Polydioxanone can also be used for orbital floor defects exceeding 2 cm2 [12].
Conclusions
The use of biodegradable plates is an appropriate option for reconstruction of the orbital floor defects. The defect size does not have any effect on the stability of the plate. However, incomplete plate resorption increases the risk of remnant defects in the orbital floor. The larger defects lead to slow degradation of biodegradable plates.
References
- Tabrizi, R.; Ozkan, T.B.; Mohammadinejad, C.; Minaee, N. Orbital floor reconstruction. J. Craniofac Surg. 2010, 21, 1142–1146. [Google Scholar] [PubMed]
- Büchel, P.; Rahal, A.; Seto, I.; Iizuka, T. Reconstruction of orbital floor fracture with polyglactin 910/polydioxanon patch (ethisorb): a retrospective study. J. Oral. Maxillofac. Surg. 2005, 63, 646–650. [Google Scholar] [PubMed]
- Tong, L.; Bauer, R.J.; Buchman, S.R. A current 10-year retrospective survey of 199 surgically treated orbital floor fractures in a nonur-ban tertiary care center. Plast. Reconstr. Surg. 2001, 108, 612–621. [Google Scholar] [PubMed]
- Jank, S.; Emshoff, R.; Schuchter, B.; Strobl, H.; Brandlmaier, I.; Norer, B. Orbital floor reconstruction with flexible Ethisorb patches: a retrospective long-term follow-up study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2003, 95, 16–22. [Google Scholar] [PubMed]
- Baumann, A.; Burgasser, G.; Gauss, N.; et al. Orbital floor reconstruc-tion with an alloplastic biodegradablepolydioxanone sheet. Int. J. Oral. Maxillofac. Surg. 2002, 31, 367–373. [Google Scholar] [PubMed]
- Jacono, A.A.; Moskowitz, B. Alloplastic implants for orbital wall reconstruction. Facial Plast. Surg. 2000, 16, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Baino, F. Biomaterials and implants for orbital floor repair. Acta Biomater. 2011, 7, 3248–3266. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, W.P.; Mayer-Zuchi, U. The use of polyglactin 910-polydioxanon in the treatment of defects of the orbital roof. J. Oral. Maxillofac. Surg. 1999, 57, 1301–1305. [Google Scholar] [PubMed]
- Francel, T.J.; Birely, B.C.; Ringelman, P.R.; Manson, P.N. The fate of plates and screws after facial fracture reconstruction. Plast. Reconstr. Surg. 1992, 90, 568–573. [Google Scholar] [PubMed]
- Kontakis, G.M.; Pagkalos, J.E.; Tosounidis, T.I.; Melissas, J.; Katonis, P. Bioabsorbable materials in orthopaedics. Acta Orthop. Belg. 2007, 73, 159–169. [Google Scholar] [PubMed]
- Gerressen, M.; Gillessen, S.; Riediger, D.; Hölzle, F.; Modabber, A.; Ghassemi, A. Radiologic and facial morphologic long-term re-sults in treatment of orbital floor fracture with flexible absorb-able alloplastic material. J. Oral. Maxillofac. Surg. 2012, 70, 2375–2385. [Google Scholar] [PubMed]
- Gierloff, M.; Seeck, N.G.; Springer, I.; Becker, S.; Kandzia, C.; Wiltfang, J. Orbital floor reconstruction with resorbable polydioxanone im-plants. J. Craniofac Surg. 2012, 23, 161–164. [Google Scholar] [PubMed]
© 2013 by the author. The Author(s) 2013.