Abstract
Searching for new materials for bone substitution, fixation, and reconstruction is a challenging task that attracts scientists and researchers of different fields of medicine. During the last few decades, much interest has been paid to polymeric materials, polyethylene in particular. The aim of this study is to present generalizations about our own experience in the employment of polyethylene miniplates for the surgical treatment of mandibular fractures. Ninety patients with 139 uniand bilateral mandibular fractures in different locations were involved. Treatment modalities included open reduction and internal fixation with self-made polyethylene miniplates of straight, T-shaped, Y-shaped, and X-shaped configurations and titanium screws. In 88 (97.8%) cases of surgical treatment of mandibular fractures using polymer miniplates, good anatomical and functional results were achieved. Regardless of the necessity for improvement of some mechanical properties of polyethylene, the results obtained in our clinical investigation allow us to recommend polyethylene miniplates for routine practice.
Nowadays, the employment of titanium or stainless steel miniplates for osteosynthesis is regarded as the gold standard in the treatment of patients with traumatic injuries of the maxillofacial area. Possible complications of this method are corrosion, provocation of allergic reactions, and metallosis; difficult adaptation of metal devices to the bone surface, metal “fatigue,” and exposure of miniplates in the tooth-bearing area have also been described previously [1,2]. In countries with low economic development, particularly the Ukraine, the high cost of titanium devices and instrumentation considerably restricts their routine practical application. On the other hand, the wide employment of bioresorbable plates is limited by the high cost of the devices and their expected degradation in vivo, as well as their weak mechanical properties.
To date, polymeric materials, especially high-molecularweight polyethylene (HMWPE), in medicine have been well studied, although investigations of their employment in different areas are still conducted. There are many successful results of employment of HMWPE in facial skeletal reconstructions, chin reconstructions, and other augmentations [3,4,5,6]. All authors emphasized its availability, easy and precise contouring, stability, long-term functional and aesthetic appearance, and low incidence of revisional surgical procedures. Carboni et al compared three types of alloplastic materials in the aesthetic restoration of the face and recognized porous polyethylene employment as optimal [7]. But there are few studies of the use of polyethylene in patients with facial fractures [8].
Accordingly, we proposed the use of biostable nonporous HMWPE miniplates in treatment of patients with facial trauma. Our previous mechanical, morphological, and toxicological investigations of this material confirmed its wellknown biocompatibility, absence of resorption or degeneration, long-term stability, lack of surrounding tissue reaction, and so on. Thus, the aim of this study was to review our own experience of employment of polymeric miniplates for the surgical treatment of mandibular fractures.
Materials and Methods
We, in close collaboration with specialists of Lviv National Technical University, Ukraine, invented an original method of fabrication of HMWPE miniplates of four various configurations (straight, T-shaped, X-shaped, Y-shaped) with a profile height 1.5 mm from biostable nonporous HMWPE (Figure 1), which was certified and allowed for medical usage in Ukraine.
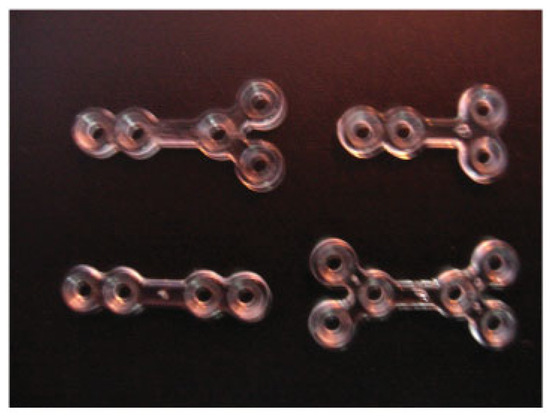
Figure 1.
Polymeric miniplates (Y-shaped, T-shaped, straight, X-shaped).
The clinical study was performed at the Department of Oral and Maxillofacial Surgery, Lviv National Medical University, Ukraine, between 2006 to 2010 and included 90 patients with 139 uniand bilateral mandibular fractures of different locations (28 condylar fractures, 88 angle fractures, 15 mental and body fractures, eight symphyseal fractures) treated surgically using HMWPE plates of our own construction and titanium screws (Synthes®, Solothurn, Switzerland; Conmet®, Moscow, Russia Federation) for their fixation. The age of the patients ranged from 18 to 65 years with a mean of 27 years. The indications for osteosynthesis were total or subtotal adentia, considerable displacement of bone fragments, ineffective conservative methods, and patient refusal for prolonged maxillomandibular fixation (MMF). Typical surgical protocol included extraor intraoral exposure of the fracture site (Figure 2) under general or local anesthesia, anatomical reduction of bone fragments (Figure 3), adaptation of the miniplate, drilling of the screw holes depending on preferred monoor bicortical insertion (Figure 4), fixation of the mini-plate with titanium screws (Figure 5), and suturing of the wound. Patients were administered analgesic antibiotics for 5 to 7 days in routine dosages as well as antiseptic solution for regular mouthwash. All patients were observed clinically for 12 to 16 months postoperatively with a mean of 14 months.

Figure 2.
Typical surgical protocol. Extraoral exposure of the fracture site in the angular area.
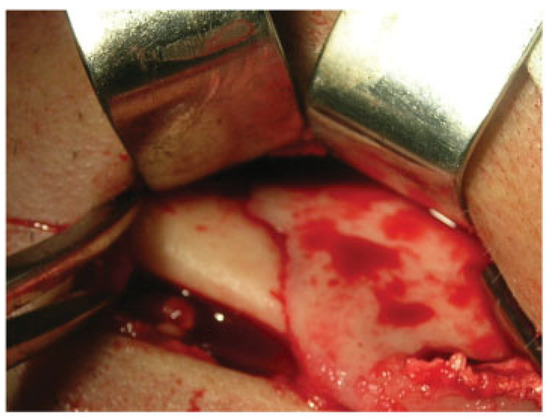
Figure 3.
Typical surgical protocol. Anatomical reduction of bone fragments in the angular area.
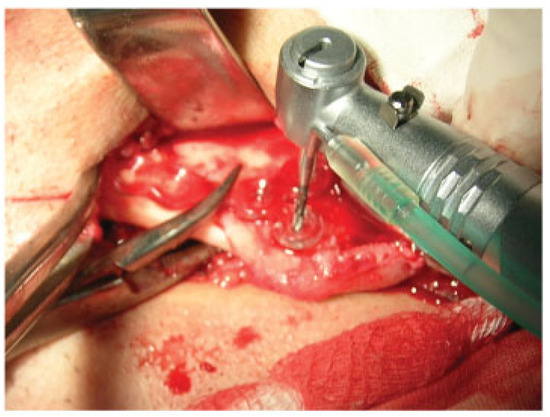
Figure 4.
Typical surgical protocol. Adaptation of the miniplate, drilling of the screw holes.
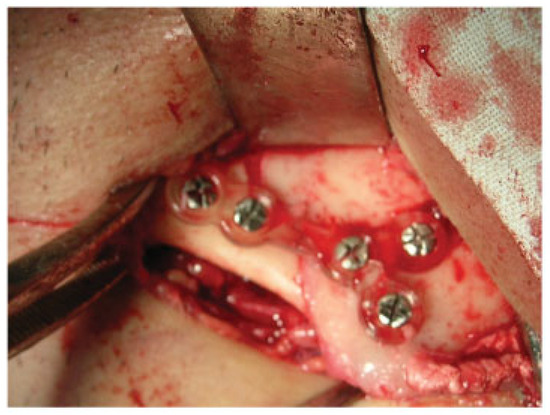
Figure 5.
Typical surgical protocol. Fixation of the miniplate with titanium screws.
X-ray examination was performed before treatment, immediately after osteosynthesis, and 3 to 4 weeks postoperatively for evaluation of fragment consolidation. Additional MMF was used intraoperatively for achieving occlusion in the vast majority of patients and was prolonged to 1 to 2 weeks only in socially unreliable subjects.
Results
In 88 (97.8%) cases of surgical treatment of mandibular fractures using HMWPE miniplates, we evaluated both anatomical and functional results as good. In all of these patients, the clinical course of the disease was uncomplicated. The average duration of the patients’ hospitalization was equal to 9.5 2 days versus 16 1 in patients treated conservatively. In one (1.1%) patient, inflammation of the surrounding soft tissue occurred 3 weeks after surgery, which was caused by late prescription of antibiotics and violation of hospital regimen and demanded special treatment. In another case (1.1%), a miniplate fractured in an emergency setting after anesthesiologists conducted appropriate measures in the oral cavity. The control X-ray examination immediately after osteosynthesis revealed an anatomical reduction of bone fragments in all cases and confirmed their consolidation 3 weeks postoperatively in 88 (97.8%) patients.
Clinical Case
A 23-year-old patient was admitted to the Department of Oral and Maxillofacial Surgery at Lviv National Medical University with complaints of swelling of the cheek, intraoral bleeding, and “bad” bite associated with falling from a bicycle. After complete clinical and roentgenological examination, a diagnosis of traumatic fracture in the right mandibular angle area with fragment displacement and impaction of tooth no. 48 in the fracture line was established (Figure 6). He underwent removal of tooth no. 48 from the fracture line, open reduction, and internal fixation of the mandible with two HMWPE miniplates via combined intraoral and transbuccal approaches (Figure 7). A control X-ray obtained the day after osteosynthesis revealed perfect anatomical reduction and fixation of bone fragments (Figure 8). Temporary MMF was maintained for 3 days after osteosynthesis. The postoperative recovery was uneventful, and good mouth opening was achieved. The duration of the patient’s hospitalization was 8 days.

Figure 6.
Fragment of orthopantomogram in a 23-year-old patient. Diagnosis was traumatic fracture of right mandibular angle with fragment displacement. Impaction of tooth no. 48 in the fracture line.

Figure 7.
Intraoperative view. An employment of transbuccal system (Synthes®, Solothurn, Switzerland) during fixation of polymeric miniplates.
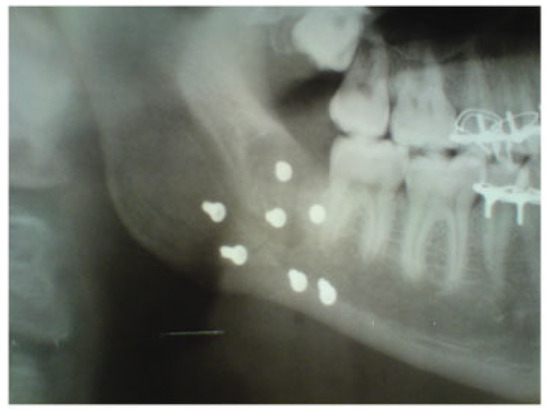
Figure 8.
Fragment of orthopantomogram in a 23-year-old patient. One day after osteosynthesis. Anatomical reduction and fixation of mandibular angle fracture with two high-molecular-weight polyethylene miniplates.
Discussion
Despite positive experience with polyethylene implants in facial reconstruction and aesthetic surgery, the possibility of their employment in traumatic injuries is still debated. One of the important disadvantages of polymeric materials is their low mechanical properties, which do not allow to provide rigid or functionally stable fixation of bone fragments, especially in cases of load-bearing osteosynthesis [9,10]. To improve the mechanical properties of polymer, Wang et al proposed a hydroxyapatite-polyethylene composite [11]. Scientists have been able to show experimentally that fragment stability depends on adequate positioning of the polymeric device much more than fracture topography [12,13,14]. A comparative analysis of employment of 2.5 resorbable miniplates (Inion CPS, Finland) and two titanium miniplates for fixation of mandibular fractures performed by Laughlin et al revealed a convincingly lower complication rate in cases of polymeric osteosynthesis [15]. Absence of a significant difference between polymeric and metal miniplates for fixation of osteotomized mandibular and maxillary fractures with additional MMF was described by Ueki et al and by Cheung et al. [16,17]. Moreover, employment of metal miniplates in the areas of permanent load leads to local osteoporosis due to the acute disparity of some mechanical properties, elastic modulus in particular, of bone and metal [18,19]. Positive results of employment of biostable polymeric miniplates were also confirmed by us in the this study. The radiological transparency of polymeric miniplates, in our opinion, is an advantage rather than a drawback due to an unimpeded visualization of the fracture line postoperatively. For the determination of implant location and its interrelationship with surrounding tissues, a method of multidetector spiral computed tomography was proposed [20]. Among other evident advantages of polymeric fixation devices, the possibility of fast intraoperative correction of their shape as well as adaptation to the bone surface should be emphasized.
Conclusion
On the basis of experimental and clinical investigations performed, we concluded that HMWPE plates in surgical treatment of mandibular fractures are efficient. The proposed method of osteosynthesis improves postoperative anatomical and functional results, shortens the terms of patients’ hospitalization, and possess a low incidence of complications. One of the possible directions for future studies is a creation of polymeric-hydroxyapatite compositions with improved osteointegrative and mechanical properties.
References
- Martines-Villalobos Castillo, S. Osteosintesis maxilofacial con titanio. Rev Esp Cirug Maxilofac 2004, 26, 46–60. [Google Scholar] [CrossRef]
- Acero, J.; Calderon, J.; Salmeron, J.I.; Verdaguer, J.J.; Concejo, C.; Somacarrera, M.L. The behaviour of titanium as a biomaterial: microscopy study of plates and surrounding tissues in facial osteosynthesis. J Craniomaxillofac Surg 1999, 27, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Yaremchuk, M.J. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconstr Surg 2003, 111, 1818–1827. [Google Scholar] [CrossRef] [PubMed]
- Menderes, A.; Baytekin, C.; Topcu, A.; Yilmaz, M.; Barutcu, A. Craniofacial reconstruction with high-density porous polyethylene implants. J Craniofac Surg 2004, 15, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Choe, K.S.; Stucki-McCormick, S.U. Chin augmentation. Facial Plast Surg 2000, 16, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Yaremchuk, M.J. Improving aesthetic outcomes after alloplastic chin augmentation. Plast Reconstr Surg 2003, 112, 1422–1432, discussion 1433–1434. [Google Scholar] [CrossRef] [PubMed]
- Carboni, A.; Gasparini, G.; Perugini, M.; Renzi, G.; Matteini, C.; Becelli, R. Evaluation of homologous bone graft versus biomaterials in the aesthetic restoration of the middle third of the face. Minerva Chir 2002, 57, 283–287. [Google Scholar] [PubMed]
- Romano, J.J.; Iliff, N.T.; Manson, P.N. Use of Medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg 1993, 4, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Chacon, G.E.; Dillard, F.M.; Clelland, N.; Rashid, R. Comparison of strains produced by titanium and poly D, L-lactide acid plating systems to in vitro forces. J Oral Maxillofac Surg 2005, 63, 968–972. [Google Scholar] [CrossRef] [PubMed]
- Landes, C.A.; Ballon, A.; Roth, C. Maxillary and mandibular osteosyntheses with PLGA and P(L/DL)LA implants: a 5-year inpatient biocompatibility and degradation experience. Plast Reconstr Surg 2006, 117, 2347–2360. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Joseph, R.; Bonfield, W. Hydroxyapatite-polyethylene composites for bone substitution: effects of ceramic particle size and morphology. Biomaterials 1998, 19, 2357–2366. [Google Scholar] [CrossRef] [PubMed]
- Akiko, K.; Nagasao, T.; Kaneko, T.; Miyamoto, J.; Nakajima, T. A comparative study of most suitable miniplate fixation for mandibular symphysis fracture using a finite element model. The Kejo J Med 2007, 55, 1–8. [Google Scholar]
- Tams, J.; Van Loon, J.P.; Otten, B.; Bos, R.R. A computer study of biodegradable plates for internal fixation of mandibular angle fractures. J Oral Maxillofac Surg 2001, 59, 404–407, discussion 407–408. [Google Scholar] [CrossRef] [PubMed]
- Lovald, S.T.; Khraishi, T.; Wagner, J.; Baack, B.; Kelly, J.; Wood, J. Comparison of plate-screw systems used in mandibular fracture reduction: finite element analysis. J Biomech Eng 2006, 128, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, R.M.; Block, M.S.; Wilk, R.; Malloy, R.B.; Kent, J.N. Resorbable plates for the fixation of mandibular fractures: a prospective study. J Oral Maxillofac Surg 2007, 65, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Ueki, K.; Marukawa, K.; Shimada, M.; Nakagawa, K.; Alam, S.; Yamamoto, E. Maxillary stability following Le Fort I osteotomy in combination with sagittal split ramus osteotomy and intraoral vertical ramus osteotomy: a comparative study between titanium miniplate and poly-L-lactic acid plate. J Oral Maxillofac Surg 2006, 64, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.K.; Chow, L.K.; Chiu, W.K. A randomized controlled trial of resorbable versus titanium fixation for orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004, 98, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, V.K.; Ramakrishna, K.; Ghista, D.N. Biomechanics of bonefracture fixation by stiffness-graded plates in comparison with stainless-steel plates. Biomed Eng Online 2005, 4, 46. [Google Scholar] [CrossRef] [PubMed]
- Cordey, J.; Perren, S.M.; Steinemannz, S.G. Stress protection due to plates: myth or reality? A parametric analysis made using the composite beam theory. Injury Int J Care Injured 2000, 31, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Coskun, U.; Ozturk, S.; Zor, F.; Turgut, A.T.; Sengezer, M. Imaging of porous polyethylene implant by using multidetector spiral computed tomography. J Craniofac Surg 2008, 19, 156–158. [Google Scholar] [CrossRef] [PubMed]
© 2008 by the author. The Author(s) 2008.