Stabilization of Mobile Mandibular Segments in Mandibular Reconstruction: Use of Spanning Reconstruction Plate
Abstract
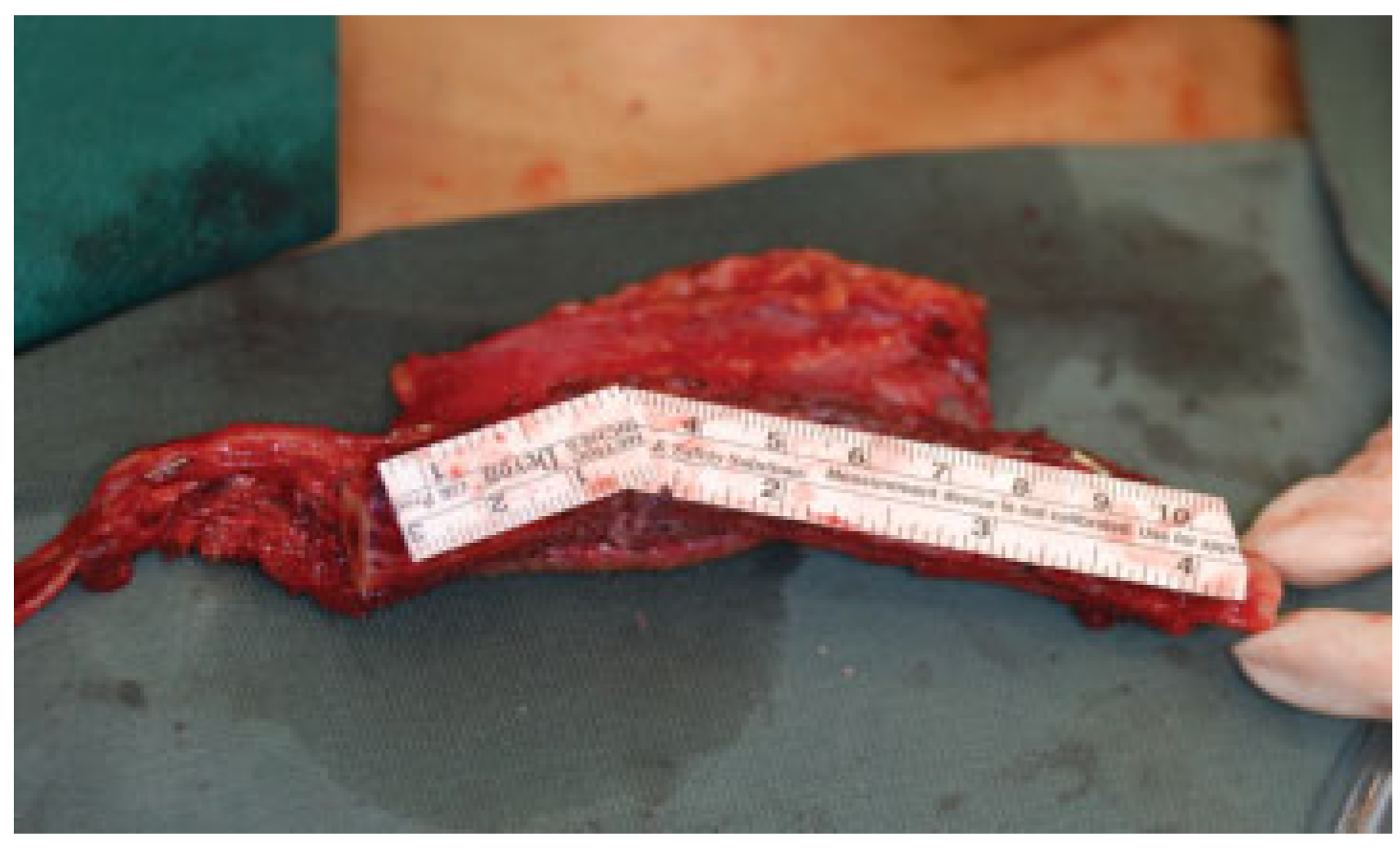
:1. Case Report
2. Technique
3. Discussion
4. Conclusion
References
- Cordeiro, P.G.; Disa, J.J.; Hidalgo, D.A.; Hu, Q.Y. Reconstruction of the mandible with osseous free flaps: A 10-year experience with 150 consecutive patients. Plast Reconstr Surg 1999, 104, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.P.; Deschler, D.G. Mandibular reconstruction in 2004: An analysis of different techniques. Curr Opin Otolaryngol Head Neck Surg 2004, 12, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, C.; Bianchi, A.; Mazzoni, S.; Cipriani, R.; Campobassi, A. Oromandibular reconstruction using a fibula osteocutaneous free flap: Four different “preplating” technique. Plast Reconstr Surg 2006, 118, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; Agrillo, A.; Battisti, A.; Gennaro, P.; Calabrese, L.; Iannetti, G. Surgical planning in reconstruction of mandibular defect with fibula free flap: 15 patients. J Craniofac Surg 2005, 16, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Ung, F.; Rocco, J.W.; Deschler, D.G. Temporary intraoperative external fixation in mandibular reconstruction. Laryngoscope 2002, 112, 1569–1573. [Google Scholar] [CrossRef] [PubMed]
- Kroll, S.S.; Reece, G.P. Aesthetically successful mandibular reconstruc- tion with a single reconstruction plate. Clin Plast Surg 2001, 28, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Reece, G.P.; Martin, J.W.; Lemon, J.C.; Jacob, R.F. Mandible fragment fixation during reconstruction: The splint-and-plate technique. Ann Plast Surg 1993, 31, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Kellman, R.M.; Gullane, P.J. Use of the AO mandibular reconstruction plate for bridging of mandibular defects. Otolaryngol Clin North Am 1987, 20, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Luhr, H.G. The development of modern osteosynthesis. Mund Kiefer Gesichtschir 2000, 4, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, D.; Urken, M.L.; Vickery, C.; Weinberg, H.; Biller, H.F. Bone contouring and fixation in functional, primary microvascular mandibular reconstruction. Head Neck 1991, 13, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Rohner, D.; Jaquiéry, C.; Kunz, C.; Bucher, P.; Maas, H.; Hammer, B. Maxillofacial reconstruction with prefabricated osseous free flaps: A 3-year experience with 24 patients. Plast Reconstr Surg 2003, 112, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Aesthetic improvements in free-flap mandible recon- struction. Plast Reconstr Surg 1991, 88, 574–585; discussion 586–587. [Google Scholar] [CrossRef] [PubMed]
- Thankappan, K.; Trivedi, N.P.; Subash, P.; et al. Three-dimensional computed tomography-based contouring of a free fibula bone graft for mandibular reconstruction. J Oral Maxillofac Surg 2008, 66, 2185–2192. [Google Scholar] [CrossRef] [PubMed]
- Strackee, S.D.; Kroon, F.H.; Jaspers, J.E.; Bos, K.E. Modeling a fibula transplant in mandibular reconstructions: Evaluation of the effects of a minimal number of osteotomies on the contour of the jaw. Plast Reconstr Surg. 2001, 108, 1915–1921; discussion 1923–1923. [Google Scholar] [CrossRef] [PubMed]
- Chiodo, A.A.; Gur, E.; Pang, C.Y.; et al. The vascularized pig fibula bone flap model: Effect of segmental osteotomies and internal fixation on blood flow. Plast Reconstr Surg 2000, 105, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Sun, J.; He, Y.; Weng, Y.Q.; Jiang, J.D. [Axial split osteotomy of free fibular flap for mandibular angle reconstruction: A clinical study]. Shanghai Kou Qiang Yi Xue 2005, 14, 355–358, 369. [Google Scholar] [PubMed]
- Guyot, L.; Richard, O.; Cheynet, F.; et al. “Axial split osteotomy” of free fibular flaps for mandible reconstruction: Preliminary results. Plast Reconstr Surg 2001, 108, 332–335. [Google Scholar] [CrossRef] [PubMed]



© 2012 by the author. The Author(s) 2012.
Share and Cite
Yap, Y.L.; Lim, J.; Ong, W.C.; Yeo, M.; Lee, H.; Lim, T.C. Stabilization of Mobile Mandibular Segments in Mandibular Reconstruction: Use of Spanning Reconstruction Plate. Craniomaxillofac. Trauma Reconstr. 2012, 5, 123-126. https://doi.org/10.1055/s-0032-1313354
Yap YL, Lim J, Ong WC, Yeo M, Lee H, Lim TC. Stabilization of Mobile Mandibular Segments in Mandibular Reconstruction: Use of Spanning Reconstruction Plate. Craniomaxillofacial Trauma & Reconstruction. 2012; 5(3):123-126. https://doi.org/10.1055/s-0032-1313354
Chicago/Turabian StyleYap, Yan Lin, Jane Lim, Wei Chen Ong, Matthew Yeo, Hanjing Lee, and Thiam Chye Lim. 2012. "Stabilization of Mobile Mandibular Segments in Mandibular Reconstruction: Use of Spanning Reconstruction Plate" Craniomaxillofacial Trauma & Reconstruction 5, no. 3: 123-126. https://doi.org/10.1055/s-0032-1313354
APA StyleYap, Y. L., Lim, J., Ong, W. C., Yeo, M., Lee, H., & Lim, T. C. (2012). Stabilization of Mobile Mandibular Segments in Mandibular Reconstruction: Use of Spanning Reconstruction Plate. Craniomaxillofacial Trauma & Reconstruction, 5(3), 123-126. https://doi.org/10.1055/s-0032-1313354


