Does the Relationship Between Retained Mandibular Third Molar and Mandibular Angle Fracture Exist? An Assessment of Three Possible Causes
Abstract
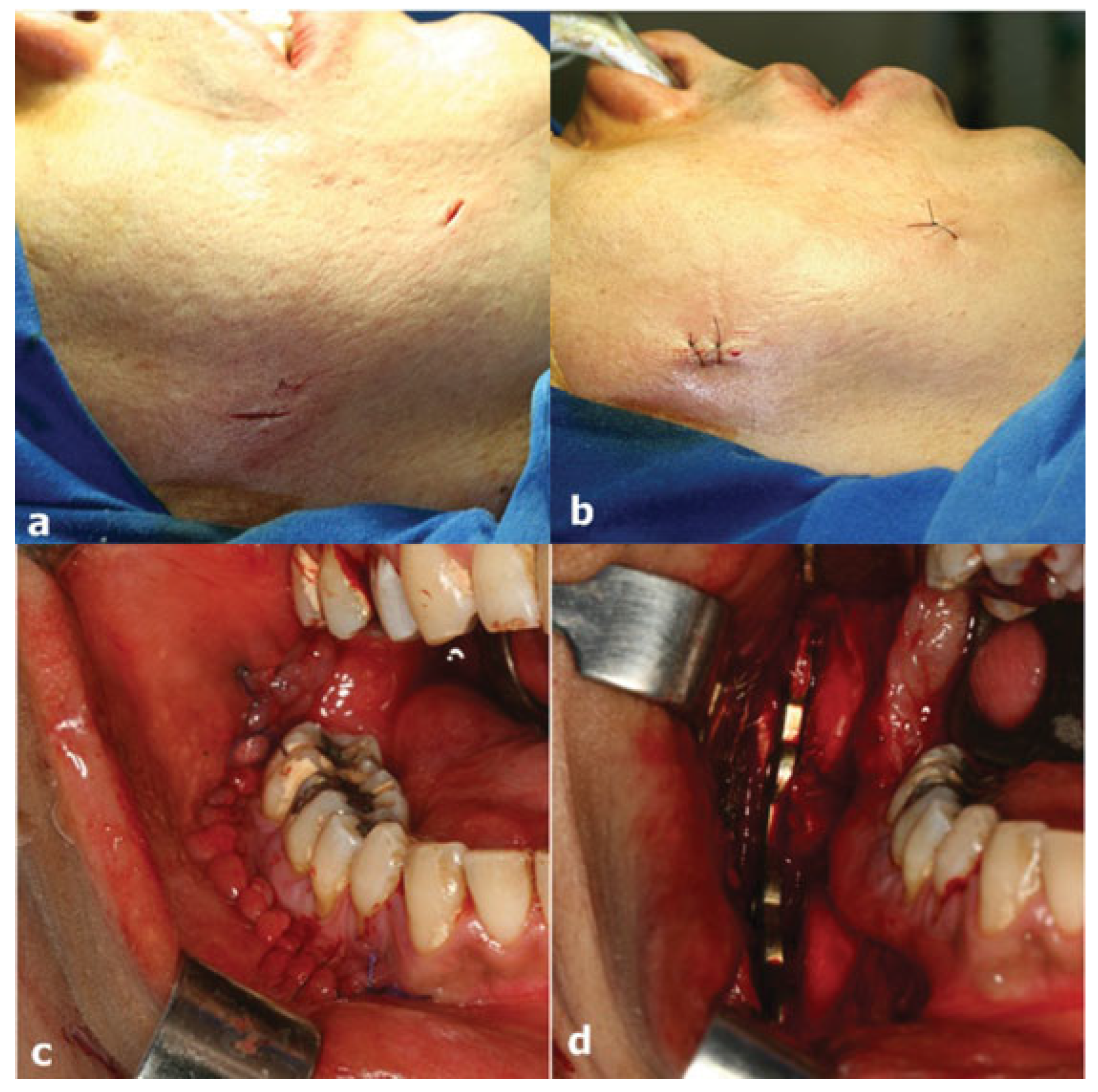
:1. Case Reports
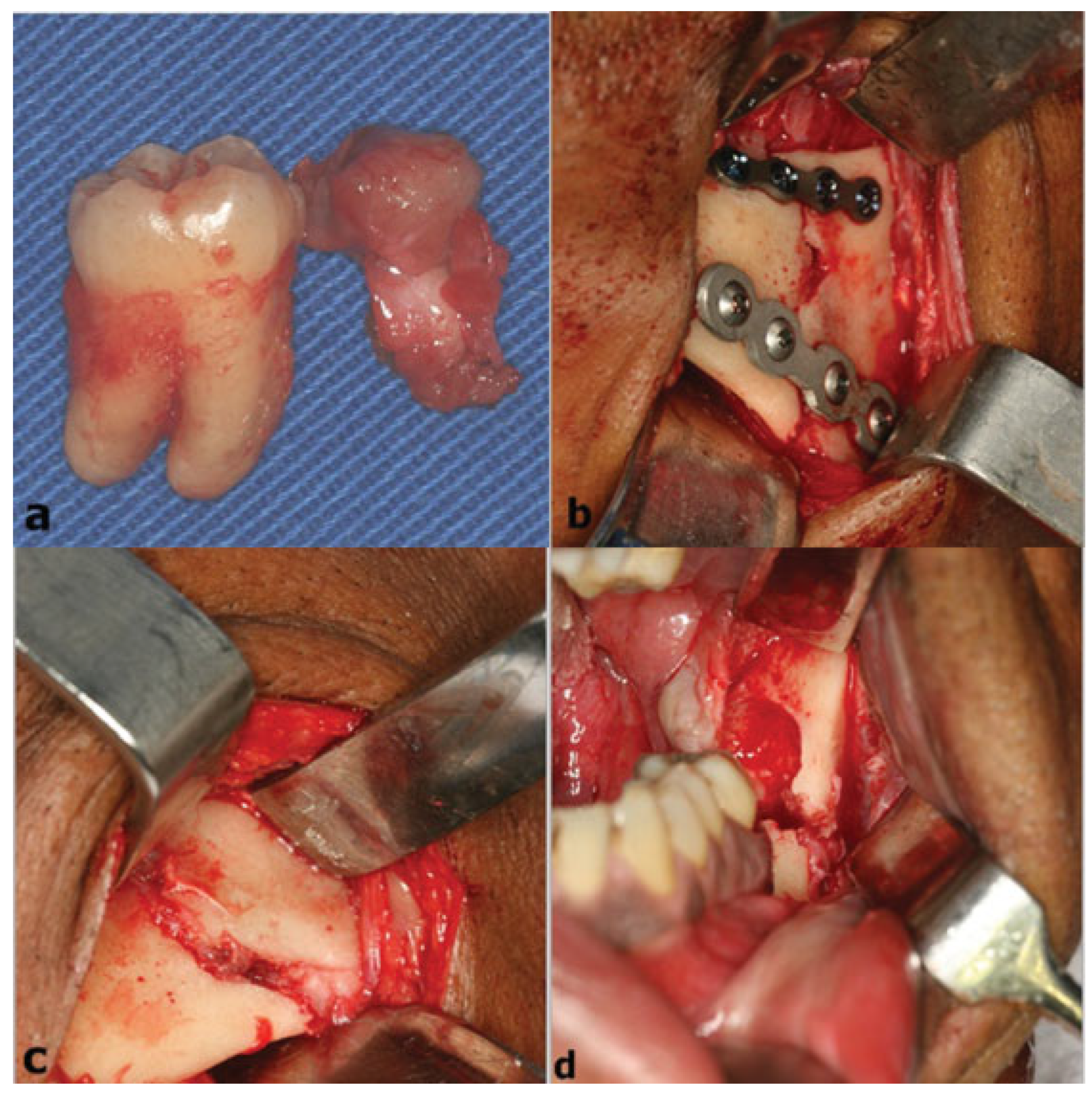
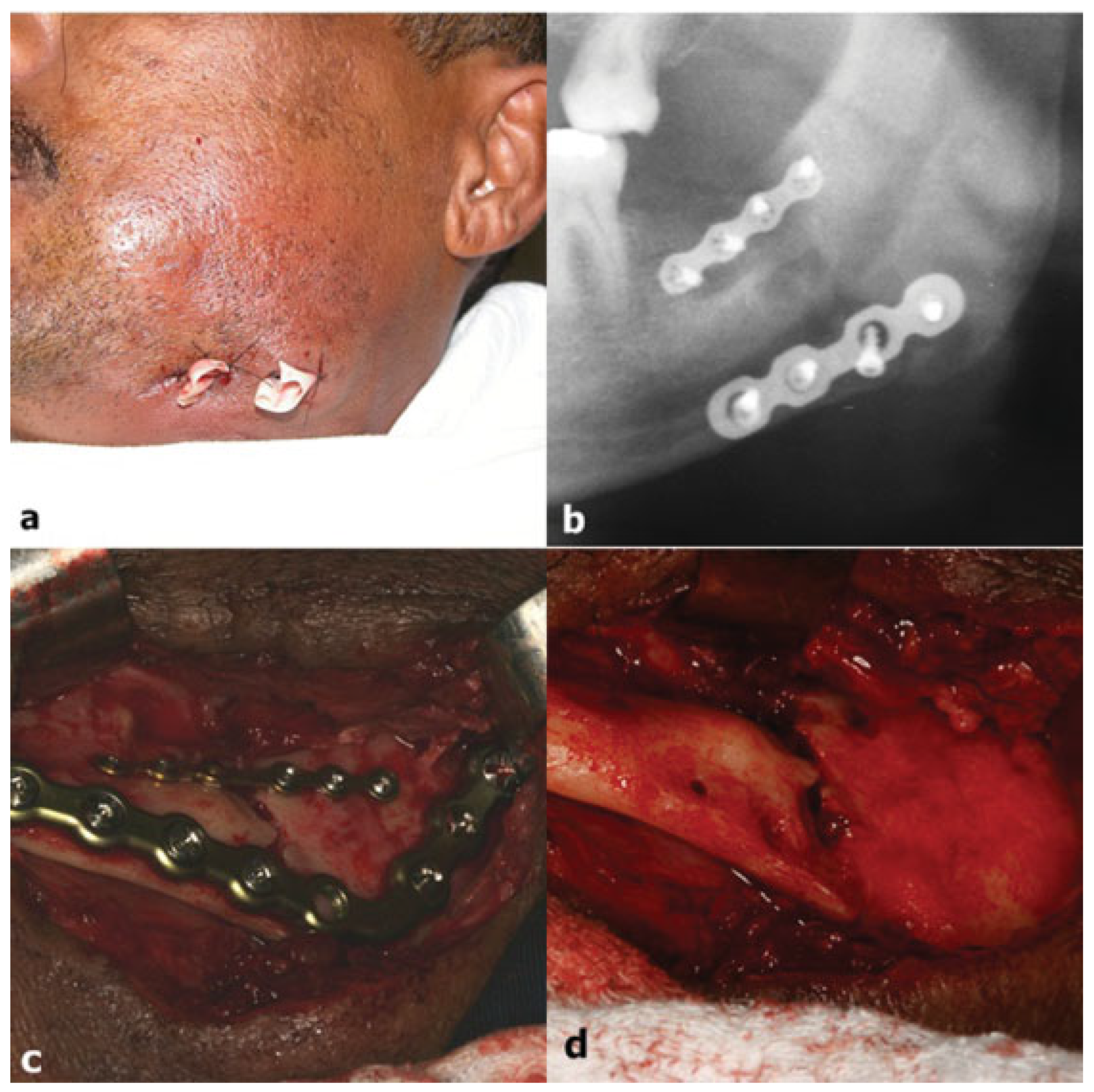
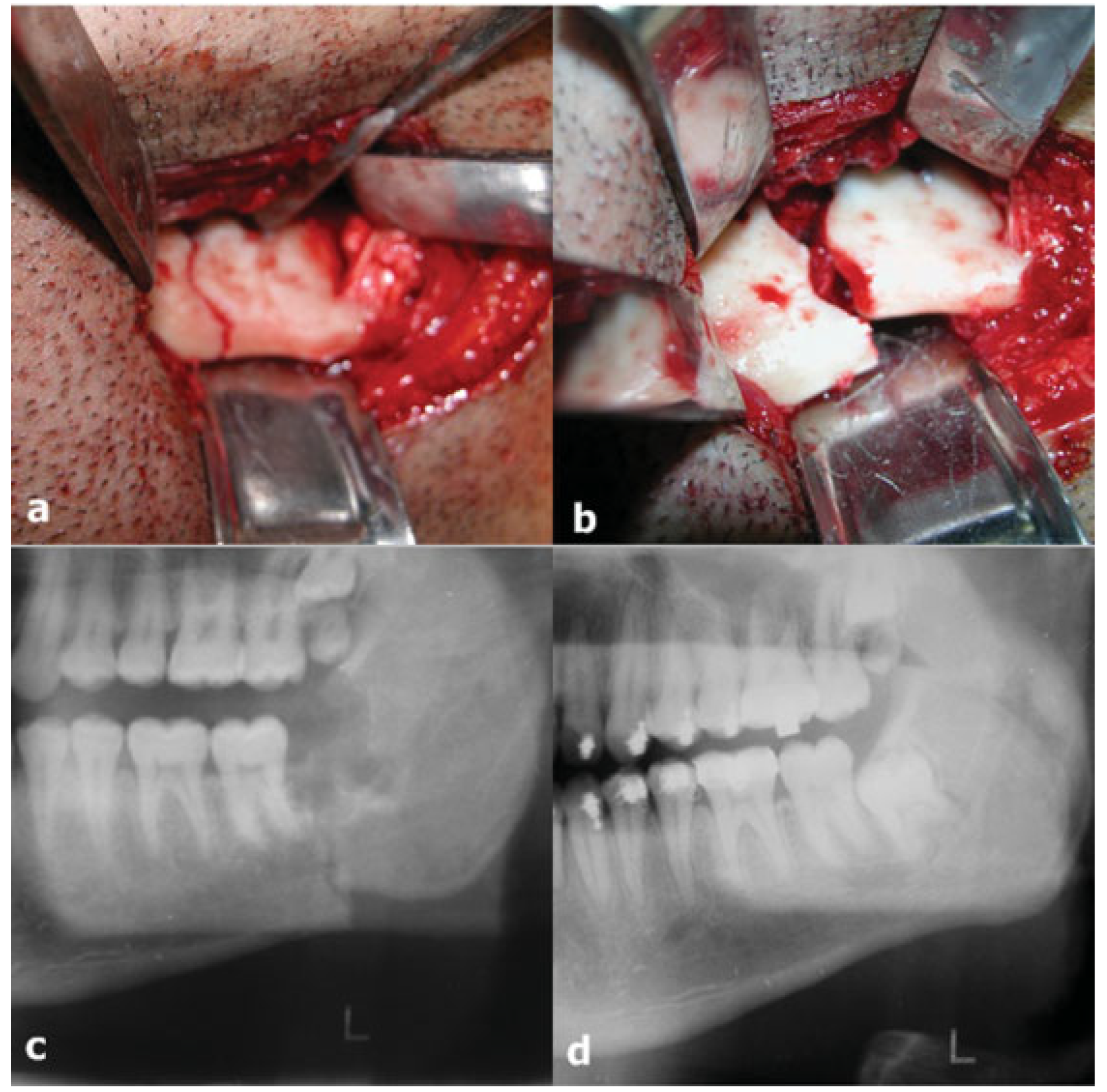
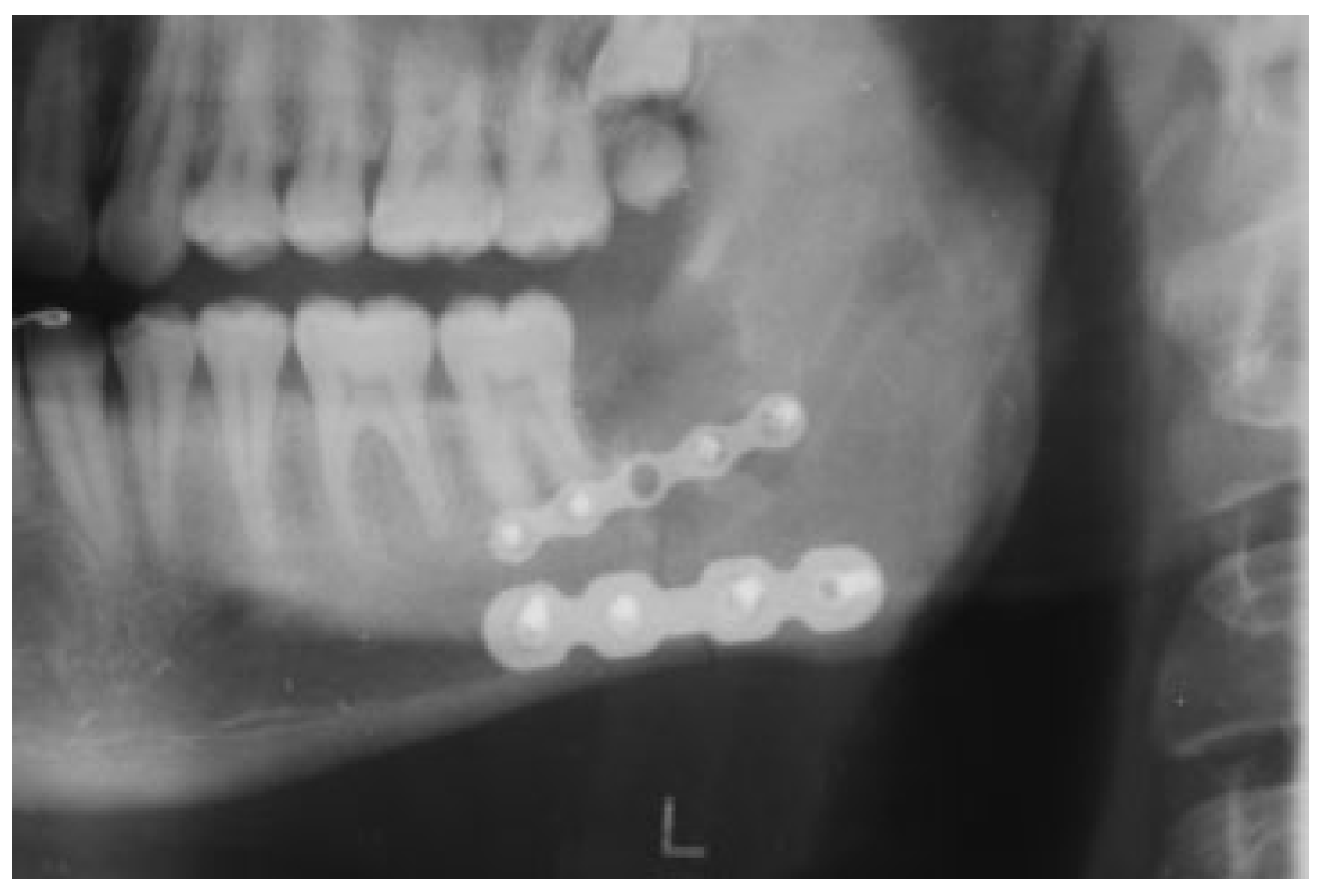
1.1. Case 1
1.2. Case 2
1.3. Case 3
2. Discussion
3. Conclusions
References
- Peterson, L.J.; Ellis, E.I.I.I.; Hupp, J.R.; Tucker, M. Contemporary Oral & Maxillofacial Surgery; Mosby: Saint Louis, 1993; Volume 225–261, pp. 587–610. [Google Scholar]
- Damante, J.H.; Freitas, J.A.S.; Tavano, O.; Alvares, L.C. Interpretação radiográfica. In Curso de Radiologia em Odontologia; Alvares, L.C., Tavano, O., Eds.; Editora Santos: São Paulo, 2009; pp. 129–218. [Google Scholar]
- Al-Khateeb, T.H.; Bataineh, A.B. Pathology associated with impacted mandibular third molars in a group of Jordanians. J Oral Maxillofac Surg 2006, 64, 1598–1602. [Google Scholar] [PubMed]
- Verri, V.A.; Oliveira, M.A.; Grandini, A.S.; et al. Estudo clínico-radio- gráfico da incidência dos dentes inclusos em 3.000 indivíduos. Rev Assoc Paul Cirurg Dent 1973, 27, 274–279. [Google Scholar]
- Marciani, R.D. Third molar removal: an overview of indications, imaging, evaluation, and assessment of risk. Oral Maxillofac Surg Clin North Am 2007, 19, 1–13, v. [Google Scholar]
- Sant’ana, E.; Ferreira Júnior, O.; Pinzan, C.R.M. Avaliação da freqüência da posição dos terceiros molares inferiores não irrompidos. Rev Cir Traumatol Buco-Maxilo-fac 2000, 7, 42–45. [Google Scholar]
- Fuster Torres, M.A.; Gargallo Albiol, J.; Berini Aytés, L.; Gay Escoda, C. Experience in the Master of Oral Surgery and Implantology at Barcelona University Dental School. Evaluation of the indication for surgical extraction of third molars according to the oral surgeon and the primary care dentist. Med Oral Patol Oral Cir Bucal 2008, 13, E499–E504. [Google Scholar]
- Inaoka, S.D.; Carneiro, S.C.A.S.; Vasconcelos, B.C.E.; Leal, J.; Porto, G.G. Relationship between mandibular fracture and impacted lower third molar. Med Oral Patol Oral Cir Bucal 2009, 14, E349–E354. [Google Scholar] [PubMed]
- van der Linden, W.; Cleaton-Jones, P.; Lownie, M. Diseases and lesions associated with third molars. Review of 1001 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995, 79, 142–145. [Google Scholar]
- Farish, S.E.; Bouloux, G.F. General technique of third molar removal. Oral Maxillofac Surg Clin North Am 2007, 19, 23–43, v–vi. [Google Scholar]
- Pell, G.J.; Gregory, B.T. Impacted mandibular third molars classification and modified technique for removal. Dent Dig 1933, 39, 330–338. [Google Scholar]
- Nery, F.S.; Santos, L.D.; Sarmento, V.A.; Santana, E.J.B. Evaluation of prevalence of non erupted lower third molar and of the position and inclination of its long axis in panoramic radiographs. Rev Ci Méd Biol 2006, 5, 222–230. [Google Scholar]
- Yamalik, K.; Bozkaya, S. The predictivity of mandibular third molar position as a risk indicator for pericoronitis. Clin Oral Investig 2008, 12, 9–14. [Google Scholar]
- Sortino, F.; Pedullà, E.; Masoli, V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: comparison of postoperative recovery. J Oral Maxillofac Surg 2008, 66, 2444–2448. [Google Scholar] [PubMed]
- Lee, J.T.; Dodson, T.B. The effect of mandibular third molar presence and position on the risk of an angle fracture. J Oral Maxillofac Surg 2000, 58, 394–398; discussion 399. [Google Scholar] [PubMed]
- Fuselier, J.C.; Ellis, E.E., III; Dodson, T.B. Do mandibular third molars alter the risk of angle fracture? J Oral Maxillofac Surg 2002, 60, 514–518. [Google Scholar] [PubMed]
- Meisami, T.; Sojat, A.; Sàndor, G.K.B.; Lawrence, H.P.; Clokie, C.M.L. Impacted third molars and risk of angle fracture. Int J Oral Maxillofac Surg 2002, 31, 140–144. [Google Scholar]
- Iida, S.; Hassfeld, S.; Reuther, T.; Nomura, K.; Mühling, J. Relationship between the risk of mandibular angle fractures and the status of incompletely erupted mandibular third molars. J Craniomaxillofac Surg 2005, 33, 158–163. [Google Scholar]
- Ma’aita, J.; Alwrikat, A. Is the mandibular third molar a risk factor for mandibular angle fracture? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000, 89, 143–146. [Google Scholar]
- Halmos, D.R.; Ellis, E., III; Dodson, T.B. Mandibular third molars and angle fractures. J Oral Maxillofac Surg 2004, 62, 1076–1081. [Google Scholar]
- Bresaola, M.D.; Assis, D.S.F.R.; Ribeiro Júnior, P.D. Avaliação epidemio- lógica de pacientes portadores de traumatismo facial em um serviço de pronto-atendimento da Região Centro-Oeste do Estado de São Paulo. Rev.Odont Vitoria 2005, 7, 50–57. [Google Scholar]
- Laughlin, R.M.; Block, M.S.; Wilk, R.; Malloy, R.B.; Kent, J.N. Resorbable plates for the fixation of mandibular fractures: a proapective study. J Oral Maxillofac Surg 2007, 65, 89–96. [Google Scholar]
- Subhashraj, K. A study on the impact of mandibular third molars on angle fractures. J Oral Maxillofac Surg 2009, 67, 968–972. [Google Scholar] [PubMed]
- Sakr, K.; Farag, I.A.; Zeitoun, I.M. Review of 509 mandibular fractures treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg 2006, 44, 107–111. [Google Scholar]
- Ellis, E., III. Management of fractures through the angle of the mandible. Oral Maxillofac Surg Clin North Am 2009, 21, 163–174. [Google Scholar] [PubMed]
- Werkmeister, R.; Fillies, T.; Joos, U.; Smolka, K. Relationship between lower wisdom tooth position and cyst development, deep abscess formation and mandibular angle fracture. J Craniomaxillofac Surg 2005, 33, 164–168. [Google Scholar]
- Cabbar, F.; Güler, N.; Comunoğlu, N.; Sençift, K.; Cöloğlu, S. Determination of potential cellular proliferation in the odontogenic epithelia of the dental follicle of the asymptomatic impacted third molars. J Oral Maxillofac Surg 2008, 66, 2004–2011. [Google Scholar]
- Saravana, G.H.L.; Subhashraj, K. Cystic changes in dental follicle associated with radiographically normal impacted mandibular third molar. Br J Oral Maxillofac Surg 2008, 46, 552–553. [Google Scholar] [PubMed]
- Iida, S.; Nomura, K.; Okura, M.; Kogo, M. Influence of the incompletely erupted lower third molar on mandibular angle and condylar fractures. J Trauma 2004, 57, 613–617. [Google Scholar]
- Adeyemo, W.L. Do pathologies associated with impacted lower third molars justify prophylactic removal? A critical review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006, 102, 448–452. [Google Scholar]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am 2007, 19, 117–128, vii. [Google Scholar]
- Duan, D.H.; Zhang, Y. Does the presence of mandibular third molars increase the risk of angle fracture and simultaneously decrease the risk of condylar fracture? Int J Oral Maxillofac Surg 2008, 37, 25–28. [Google Scholar]
- Zhu, S.J.; Choi, B.H.; Kim, H.J.; et al. Relationship between the presence of unerupted mandibular third molars and fractures of the mandibular condyle. Int J Oral Maxillofac Surg 2005, 34, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Wagner, K.W.; Otten, J.-E.; Schoen, R.; Schmelzeisen, R. Pathological mandibular fractures following third molar removal. Int J Oral Maxillofac Surg 2005, 34, 722–726. [Google Scholar] [CrossRef]
- Woldenberg, Y.; Gatot, I.; Bodner, L. Iatrogenic mandibular fracture associated with third molar removal. Can it be prevented? Med Oral Patol Oral Cir Bucal 2007, 12, E70–E72. [Google Scholar]
- Iizuka, T.; Tanner, S.; Berthold, H. Mandibular fractures following third molar extraction. A retrospective clinical and radiological study. Int J Oral Maxillofac Surg 1997, 26, 338–343. [Google Scholar] [CrossRef]
- Zaydon, T.J.; Brown, J.B. Mandibular injuries. In Early Treatment of Facial Injuries; Zaydon, T.J., Brown, J.B., Eds.; Lea & Febiger: Philadelphia, PA, USA, 1964; pp. 112–170. [Google Scholar]
- Paza, A.O.; Abuabara, A.; Passeri, L.A. Analysis of 115 mandibular angle fractures. J Oral Maxillofac Surg 2008, 66, 73–76. [Google Scholar] [CrossRef]
- Kruger, G.O. Kruger, G.O., Ed.; Fracture of the jaws. In Textbook of Oral Surgery; Mosby: Saint Louis, MO, USA, 1974; pp. 314–384. [Google Scholar]
- Gbotolorun, O.M.; Arotiba, G.T.; Ladeinde, A.L. Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg 2007, 65, 1977–1983. [Google Scholar] [CrossRef] [PubMed]
- Almendros-Marqués, N.; Alaejos-Algarra, E.; Quinteros-Borgarello, M.; Berini-Aytés, L.; Gay-Escoda, C. Factors influencing the prophylactic removal of asymptomatic impacted lower third molars. Int J Oral Maxillofac Surg 2008, 37, 29–35. [Google Scholar] [CrossRef]
- Al-Belasy, F.A.; Tozoglu, S.; Ertas, U. Mastication and late mandibular fracture after surgery of impacted third molars associated with no gross pathology. J Oral Maxillofac Surg 2009, 67, 856–861. [Google Scholar] [PubMed]
- Yıldırım, G.; Ataoğlu, H.; Mihmanlı, A.; Kiziloğlu, D.; Avunduk, M.C. Pathologic changes in soft tissues associated with asymptomatic impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008, 106, 14–18. [Google Scholar] [CrossRef]
- Chuang, S.K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg 2007, 65, 1685–1692. [Google Scholar]
- Barry, C.P.; Kearns, G.J. Superior border plating technique in the management of isolated mandibular angle fractures: a retrospec- tive study of 50 consecutive patients. J Oral Maxillofac Surg 2007, 65, 1544–1549. [Google Scholar] [CrossRef] [PubMed]
- Scolozzi, P.; Richter, M. Treatment of severe mandibular fractures using AO reconstruction plates. J Oral Maxillofac Surg 2003, 61, 458–461. [Google Scholar] [PubMed]
- Ellis, E., III. Outcomes of patients with teeth in the line of mandibular angle fractures treated with stable internal fixation. J Oral Max-Illofac Surg 2002, 60, 863–865; discussion 866. [Google Scholar]






© 2012 by the author. The Author(s) 2012.
Share and Cite
Duarte, B.G.; Assis, D.; Ribeiro-Júnior, P.; Gonçales, E.S. Does the Relationship Between Retained Mandibular Third Molar and Mandibular Angle Fracture Exist? An Assessment of Three Possible Causes. Craniomaxillofac. Trauma Reconstr. 2012, 5, 127-135. https://doi.org/10.1055/s-0032-1313355
Duarte BG, Assis D, Ribeiro-Júnior P, Gonçales ES. Does the Relationship Between Retained Mandibular Third Molar and Mandibular Angle Fracture Exist? An Assessment of Three Possible Causes. Craniomaxillofacial Trauma & Reconstruction. 2012; 5(3):127-135. https://doi.org/10.1055/s-0032-1313355
Chicago/Turabian StyleDuarte, Bruno G., Diogo Assis, Paulo Ribeiro-Júnior, and Eduardo Sanches Gonçales. 2012. "Does the Relationship Between Retained Mandibular Third Molar and Mandibular Angle Fracture Exist? An Assessment of Three Possible Causes" Craniomaxillofacial Trauma & Reconstruction 5, no. 3: 127-135. https://doi.org/10.1055/s-0032-1313355
APA StyleDuarte, B. G., Assis, D., Ribeiro-Júnior, P., & Gonçales, E. S. (2012). Does the Relationship Between Retained Mandibular Third Molar and Mandibular Angle Fracture Exist? An Assessment of Three Possible Causes. Craniomaxillofacial Trauma & Reconstruction, 5(3), 127-135. https://doi.org/10.1055/s-0032-1313355


