Abstract
Nasal bone fractures are the most common among facial fractures. Usually these are adequately treated with closed reduction and internal and/or external stabilization with splints. However, there are clinical situations where the nasal bones are severely displaced, the nasal septum fractured and displaced, or there are external drape lacerations which preclude the use of nasal splints. If the nasal bones are reducible but unstable we consider them “flail” and in this case transmucosal, endonasal Kirschner wires are used for dorsal support until sufficient healing occurs. The technique is simple, quick, and predictable and causes minimal discomfort to the patients.
Nasal bone fractures are the most common among craniofacial fractures and third most common skeletal fractures due to its prominence and central location in the face [1]. Closed reduction is considered as the first treatment option in nasal bone fractures due to speed, facility, and hence cost-effective-ness [2,3]. Identifying and appropriately and predictably treating complex nasal fractures are the keys in decreasing the need for revision surgery. The goal of closed reduction of nasal bones is to anatomically realign the osseous and cartilaginous skeleton. Revision rhinoplasty may be required if closed reduction failed to achieve the functional and aesthetic goals. Internal packing and external splints are the most commonly used materials to stabilize nasal fractures. How- ever, complex, compound, or severely displaced fractures cannot always be adequately stabilized using packing and splints. In some cases the nasal fractures are combined with severe soft tissue injuries with compromised blood supply to the skin. In these cases placement of compressive splints is contraindicated. Here we describe the application of Kirschner wires (K-wires) or pins for stabilization of unstable or “flail” nasal fractures. First introduced by Martin Kirschner in 1909, these sharp stainless steel wires are extensively used in orthopedic procedures and are inexpensive and readily avail- able in most hospitals [4].
Clear understanding of nasal anatomy and function is crucial for proper diagnosis and treatment of nasal bone fractures. The nose is made of osteocartilaginous skeleton, mucosal lining, muscles, and skin drape [5,6]. Structurally, the external drape is composed of the skin and subcutaneous layers. The thickness of the skin varies depending on site, sex, and race. There are five subdermal layers: the superficial fatty layer, the fibromuscular superficial musculoaponeurotic system layer which envelopes each of the nasal muscles, the deep fatty layer, the periosteum and perichondrium, and the ligaments of the nose (interdomal, intercartilaginous, and dermatocartilaginous in some individuals of African de- scent) [7]. The other structural components of the nose are the osseous and the cartilaginous framework and the nasal septum. Superiorly, the paired nasal bones are attached to the frontal and lacrimal bones. Inferiorly, the nasal bones articulate with the ascending process of maxilla. The nasal bone is thick at the nasofrontal junction and tapers as it connects with the upper lateral cartilages (ULC) at the dorsum. The nasal bones overlap the ULC for ~6 to 8 mm. The lower lateral cartilages are connected to the ULC at the scroll area and makes up the lower third of the nose. The septum is composed of the perpendicular plate of the ethmoid, the vomer, the quadrangular cartilage, and membranous septum.
1. Patients and Methods
All patients were treated at The Mount Sinai Hospital, Elm- hurst Hospital Center and at Maxillofacial Surgery Services between June of 2009 and July of 2011. No institutional review board approval was deemed necessary as the nature of this technique is not considered experimental. There were 9 patients, all male aged between 22 and 53 years. All patients sustained direct trauma to their noses, which resulted in severe, comminuted, and sometimes compound nasal fractures which were unstable, “flail” despite adequate intra-operative reduction (Figure 1, Figure 2, Figure 3 and Figure 4). If the nasal bones are reducible but unstable we consider them “flail.” In these cases internal nasal packing is inadequate to support the position of the reduced nasal bones and external pressure from nasal splint will displace the fragments unpredictably. For these particular cases we believe that internal, tenting support with K-wires anchored in the frontal bone will provide ideal immobilization conditions for adequate healing with minimal disturbance of adjacent soft tissues, which would have been the case with application of internal fixation devices (plates and screws). The patients were evaluated by clinical examination and computed tomography (CT). One of the patients in this series had associated naso-orbitoethmoidal (NOE) fractures (Figure 1D,E). None of the patients had cerebrospinal rhinorrhea. Three patients sustained concomitant severe soft tissue lacerations (Figure 5 and Figure 6) precluding use of external, compressive splints. All patients were treated within 7 days of the initial trauma. The procedures were done under general, endotracheal anesthesia. All patients were released from the hospital within 24 h after surgery.
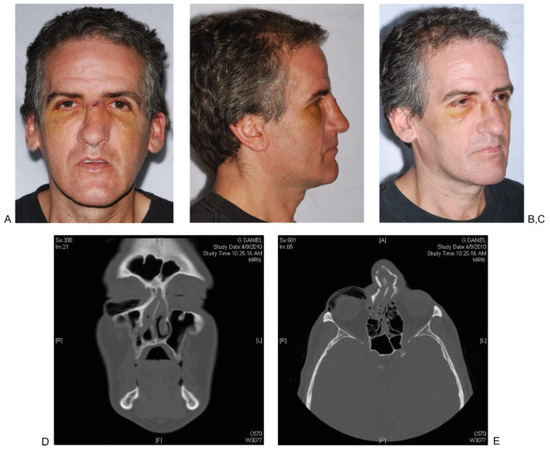
Figure 1.
(A–E) Preoperative facial photographs and coronal and axial computed tomographic scans of a patient with severe, unstable, “flail” nasal fractures. Note that the patient also has naso-orbitoethmoidal fracture, which is minimally displaced.

Figure 2.
(A–E) Postoperative clinical photographs and radiographs of the patient from Figure 1 at 4 weeks. Note silicone tubing covered K-wires protruding from the nostrils. Note parallelism of the K-wires as well as location of cephalad portion of the wires beneath frontal sinus on facial radiographs.

Figure 3.
(A–C) Preoperative clinical photographs of patient with severe, unstable, “flail” nasal fractures.

Figure 4.
(A–C) Postoperative clinical photographs of the patient from Figure 3.
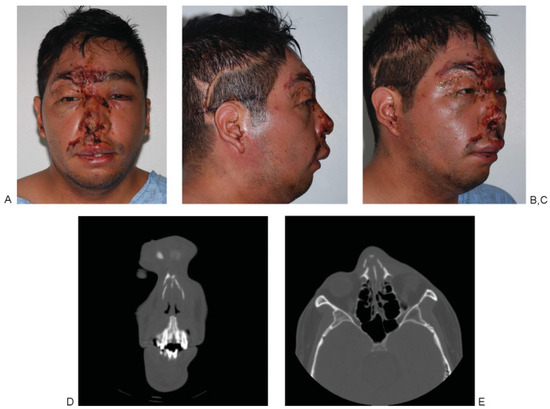
Figure 5.
(A–E) Preoperative clinical photographs and coronal and axial computed tomographic scans of a patient with severe, compound, complex nasal fractures and deep, avulsive soft tissue injuries precluding the use of compressive nasal splints.

Figure 6.
(A–C) Postoperative clinical photographs of the patient from Figure 5. Note adequate healing of the nasal skin and restoration of nasal symmetry.
2. Surgical Technique
Neuro-Patties soaked in vasoconstrictive agent (Afrin; Schering-Plough Health Care, Kenilworth, NJ) were placed inside the nasal aperture. The intranasal packing was removed after 15 min. Local and regional blocks of the supraorbital, supratrochlear, anterior ethmoidal, infraorbital, and nasopalatine nerves were done using 1% lidocaine with 1:100,000 epinephrine. A Goldman elevator was then inserted into the nasal apertures with the dominant hand while externally palpating the bony and soft tissues with the opposite hand. The nasal bones were elevated in an anterosuperior direction perpendicular to the nasal dorsum into the correct position. The nasal septum was also reestablished in relation to the ULC and nasal bone. The less dominant hand was used to further mold the bones and soft tissues against the elevator. A forceps or elevators were also used to perform any additional reduction or realign the septum. This involved repositioning of the septum over the nasal crest of the maxillary bone. If appropriate reduction of septum was not possible, submucous resection of the septum by Killian or hemitransfixion incision was performed to produce a straight septum. Two 0.062-in (1.6 mm) K-wires were used. The dorsum was tented with K- wires maintaining ~120-degree nasofrontal angle. Care was taken to ensure that the wires were parallel to the mid-sagittal plane and each other (Figure 7A–C). These wires were drilled monocortical, through the frontal bone below the fractured nasal bones to tent and support the unstable small bone fragments in place. The wires were placed through the nasal mucosa endonasally. Care was taken not to enter the frontal sinus. No intraoperative navigation or fluoroscopy was used. Postoperative radiographs were obtained routinely. The nasal bones were evaluated and ensured to be in correct anatomical position and the nasal dorsum straight. When preoperative severe septal deviations or osteocartilaginous nasal spurs were encountered submucosal septal resections were done. In these cases quilting sutures were placed to prevent septal hematoma formation. Bacitracin impregnated Merocell nasal packing was placed into the nasal passages bilateral. Small piece of silicone tubing was placed onto the end of the K-wire to prevent it from irritating the tissues of the nasal sill. When necessary, external splints were used as well. These were never used on patients with nasal skin lacerations. Placement of external splints in these patients would not have been otherwise possible if internal stabilization was not achieved with the K-wire support. Patients were given home-care instructions. All patients were placed on oral antibiotics and nasal decongestants for 5 to 7 days following surgery. All patients had postoperative lateral cephalograms taken. Patients are seen on postoperative day 2 for evaluation and removal of internal packings. The external splints were maintained for 10 to 14 days. K-wires were removed at 4 weeks.

Figure 7.
(A) Illustration of the tenting of the dorsum with K-wire. Note severely comminuted nasal bone fractures. The wire passes below the lower and upper lateral cartilages as well as nasal bones and is anchored in the frontal bone. (B) Illustration of the placement of the K-wires parallel to the midsagittal plane and each other. Note the right wire is already inserted and cut. (C) Illustration of the placement of the K-wires via tenting of the nasal dorsum and maintaining nasofrontal angle of ~120 degrees.
3. Results
All patients in this series were treated successfully. In one patient one of the K-wires became loose before schedule removal. It was removed at 3 weeks and didn’t cause any adverse consequences. All fractures healed uneventfully. The shortest follow-up in this series was 2 months and the longest 24 months. Patients were all instructed to follow-up as needed after 4 months. All patients were happy with their aesthetics and had good nasal breathing. One patient elected to undergo rhinoplasty to address a preexisting dorsal hump deformity.
4. Discussion
Nasal bone fractures can be treated by close or open techniques. Closed reduction of nasal bone fractures remains a first line of treatment because of safety, technical ease, and comparatively lower cost. Closed treatment of nasal fractures entails reduction of the nasal bones and stabilization with packing placed into the nasal vault and an external splint. External splints do not prevent unstable, flail nasal bones from being displaced medially/posteriorly. When the nasal bones are flail because of comminution or fracture pattern, or one is not able to stabilize them in an anatomic position with nasal packing alone, K-wire stabilization is a viable treatment option. K-wires have been used previously in nasal surgery for prevention of warping of costochondral grafts as well as for stabilization of nasal and NOE fractures [1,8,9,10,11,12]. When used in nasal reconstructive surgery they are inserted centrally in the dorsal component as well as at the columellar fragment. They prevent/reduce the warping of the costal cartilage. The K-wire of the columellar component is inserted in a predrilled hole in the maxillary anterior alveolus, thus affixing it there. In the other instances of fracture repair the wires were placed transcutaneous, sometimes with navigation guidance but again either through maxillary alveolus or anteriorly on either side of the nasal septum or facial bones. Our technique differs in its area of insertion, which is endonasal and parallel to the nasal dorsum and into the frontal bones thus tenting the dorsum and the septum ventrally and cephalad. Placement of K-wires after reduction of the nasal bones and cartilages essentially tents the nasal bones in the correct position, similar to nasal packing, but with rigidity and predictability. Nasal packing, even though if it is packed in a superior direction into the nasal vault often ends up in the oropharynx and must be completely or partially removed. Thus, the meticulous placement of nasal packing in the operating room (OR) to stabilize the fractures often has to be removed earlier than planned. Premature removal of the nasal packing can lead to poor outcome due to instability of nasal bones and cartilages. The use of K-wires alleviates this problem. K-wires provide superior stabilization, acting as an external-fixateur internally. Some foreseeable disadvantages of K-wires can be pin-tract infection, damage to adjacent structures such as the frontal sinus, and loosening of pins requiring premature removal. We believe that even if the frontal sinus is inadvertently entered this should not lead to serious complications as long as the drainage mechanism is not altered. We base this on our experience with craniofacial trauma when often the internal reduction screws are perforating thorough the anterior table of the frontal bone and into the frontal sinus without any short- or long-term con- sequences. The same is true when we use hardware to secure a bone or cartilage graft to the frontal bone in cases of nasal reconstruction/augmentation. Sometimes the hardware penetrates through the anterior table without any adverse effects. None the less, if intraoperative navigation or CT scan is available this should be entertained even though the duration of OR time and hence will be increased. Of the potential drawbacks we encountered only one loose pin at week 3, which had to be removed but didn’t affect the final outcome of surgery. In the treatment of severely displaced, unstable, flail nasal fractures, and those with nasal skin lacerations, closed reduction with transmucosal K-wires is an excellent technique to provide patients with a safe, effective, and predictable aesthetic and functional outcome.
References
- Won Kim, S.; Pio Hong, J.; Kee Min, W.; Wan Seo, D.; Kyu Chung, Y. Accurate, firm stabilization using external pins: A proposal for closed reduction of unfavorable nasal bone fractures and their simple classification. Plast Reconstr Surg 2002, 110, 1240–1246. [Google Scholar] [CrossRef] [PubMed]
- Illum, P. Long-term results after treatment of nasal fractures. J Laryngol Otol 1986, 100, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.C.; Kim, Y.K.; Cha, J.H.; Kang, S.R.; Park, H.S. Septal fracture in simple nasal bone fracture. Plast Reconstr Surg 2004, 113, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Franssen, B.B.; Schuurman, A.H.; Van der Molen, A.M.; Kon, M. One century of Kirschner wires and Kirschner wire insertion techni- ques: A historical review. Acta Orthop Belg 2010, 76, 1–6. [Google Scholar] [PubMed]
- Anastassov, G.E.; Joos, U.; Zöllner, B. Evaluation of the results of delayed rhinoplasty in cleft lip and palate patients. Functional and aesthetic implications and factors that affect successful nasal repair. Br J Oral Maxillofac Surg 1998, 36, 416–424. [Google Scholar] [CrossRef]
- Ortiz-Monasterio, F. Rhinoplasty; W.B. Saunders: Philadelphia, PA, USA, 1994; pp. 14–15. [Google Scholar]
- Pitanguy, I.; Salgado, F.; Radwanski, H.N.; Bushkin, S.C. The surgical importance of the dermocartilaginous ligament of the nose. Plast Reconstr Surg 1995, 95, 790–794. [Google Scholar] [CrossRef]
- Gunter, J.P.; Clark, C.P.; Friedman, R.M. Internal stabilization of autoge- nous rib cartilage grafts in rhinoplasty: A barrier to cartilage warping. Plast Reconstr Surg 1997, 100, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Gunter, J.P.; Cochran, C.S. Management of intraoperative fractures of the nasal septal “L-strut”: Percutaneous Kirschner wire fixation. Plast Reconstr Surg 2006, 117, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.K.; Zhao, L.; Belafsky, P.; Patel, P.K.; Strong, E.B. Technical note: “look-ahead” navigation method for K-wire fixation in rhinoplasty. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008, 105, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Vora, N.M.; Fedok, F.G. Management of the central nasal support complex in naso-orbital ethmoid fractures. Facial Plast Surg 2000, 16, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Yabe, T.; Ozawa, T. Treatment of nasoethmoid-orbital fractures using Kirschner wire fixation of the nasal septum. J Craniofac Surg 2011, 22, 1510–1512. [Google Scholar] [CrossRef] [PubMed]
© 2012 by the author. The Author(s) 2012.