Degloving Injuries of the Oral Cavity Change the Operative Approach to Fractures of the Anterior Segment of the Mandible
Abstract
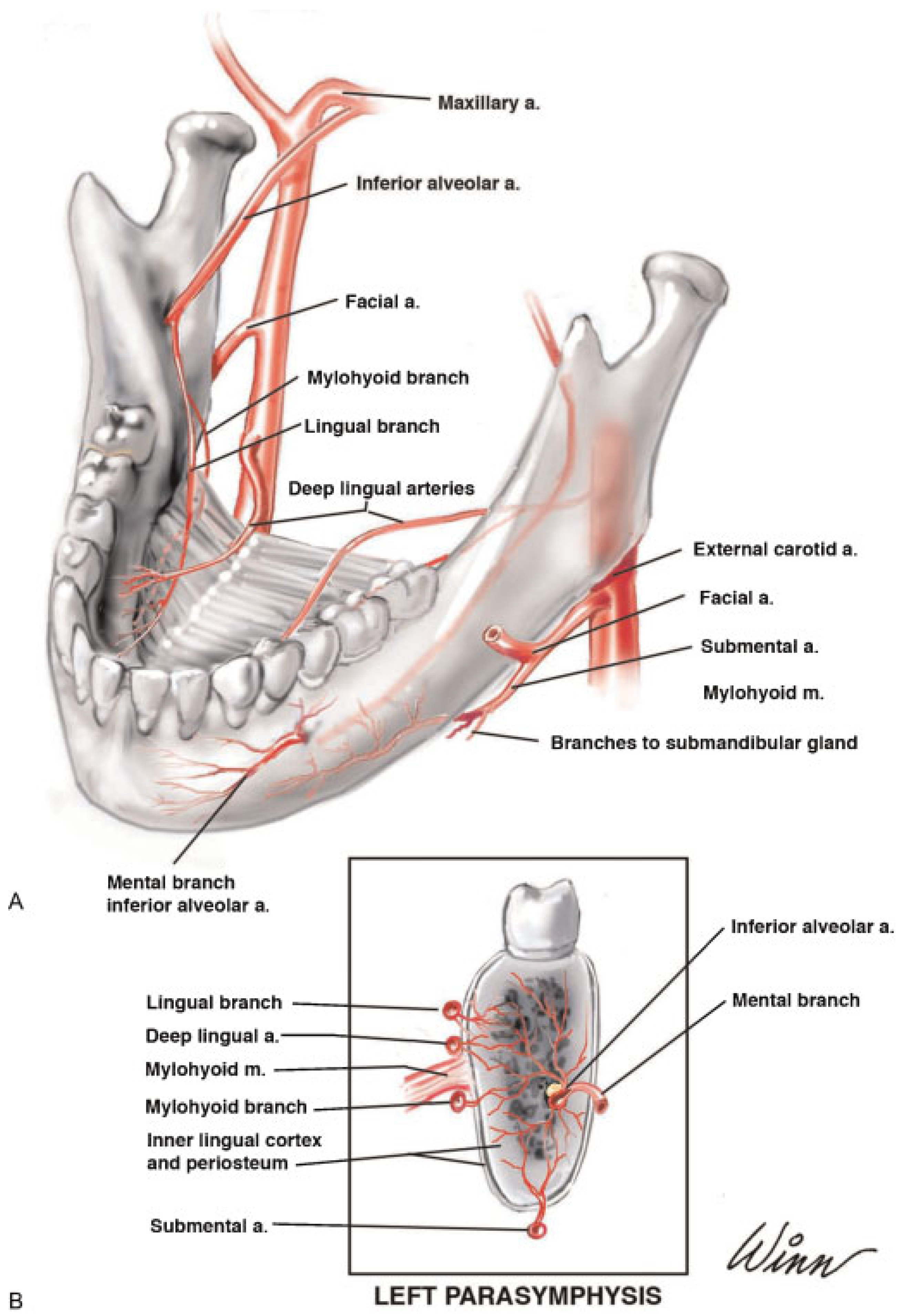
:Vascular Anatomy of the Anterior Segment
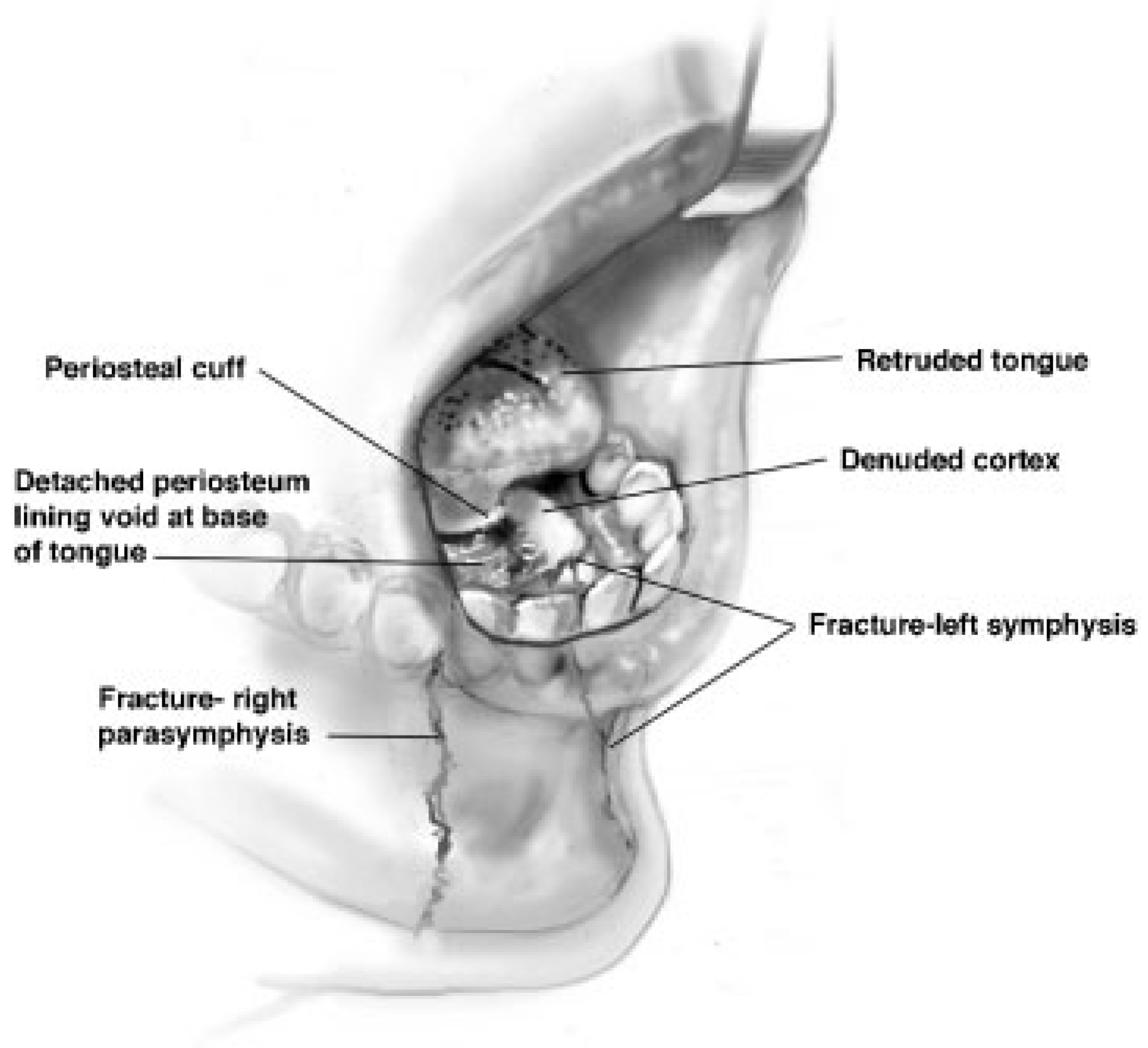
Pathomechanics of Lingual Degloving
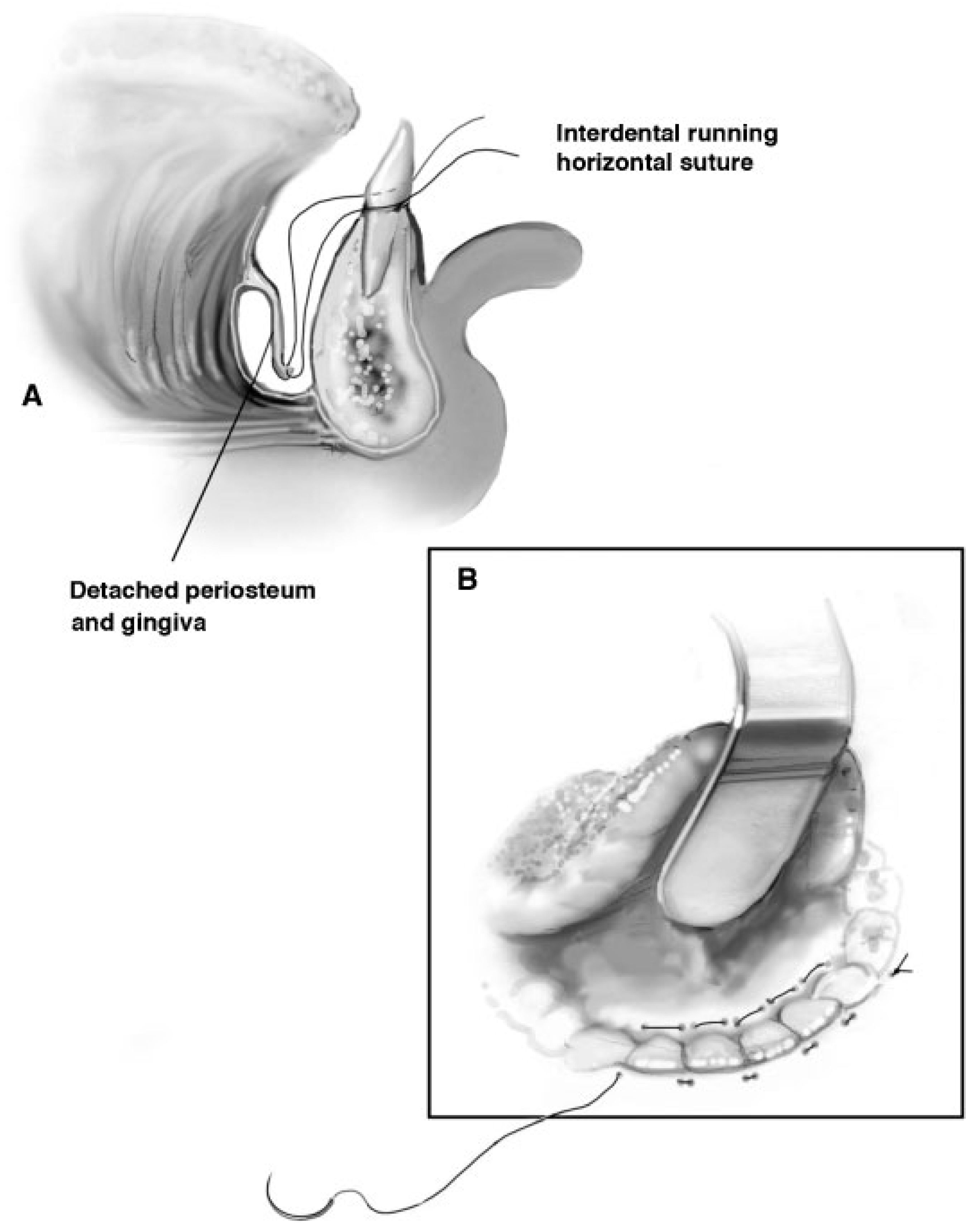
Case Report
Discussion
Conclusion
- The periosteal blood supply to the inner cortex, provided by the lingual and mylohyoid branches of the inferior alveolar artery and the deep lingual artery, is compromised.
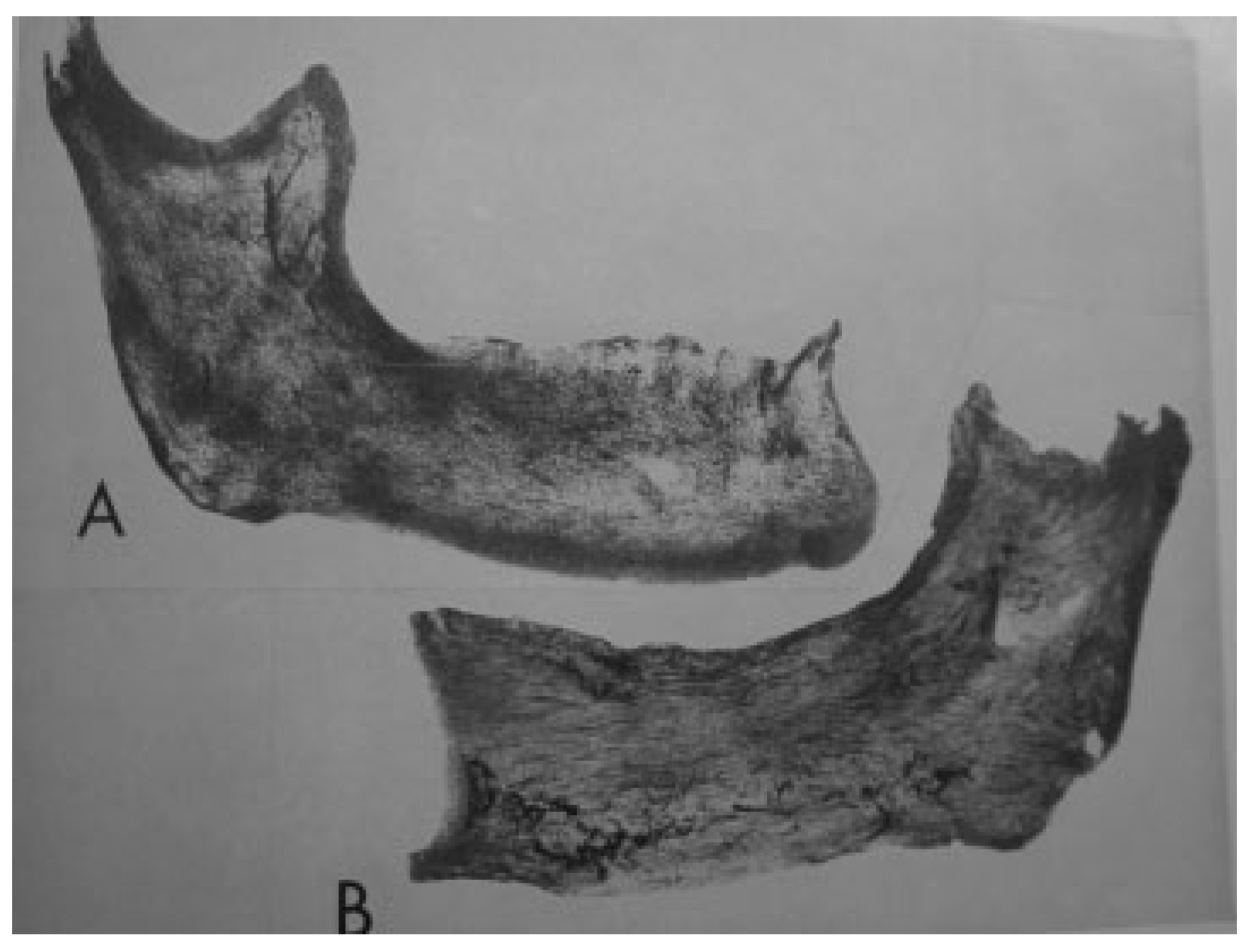
- The endosteal blood supply may fail or be slow to recanalize.
- An otherwise routine incision in the mandibular vestibule may render the bone relatively avascular and put survival of the anterior segment of the mandible at risk.
Acknowledgments
References
- Dingman, R.O.; Natvig, P. Surgery of Facial Fractures; W.B. Saunders Company: Philadelphia, PA, USA, 1964; pp. 133–210. [Google Scholar]
- Schilli, W. Mandibular fractures. In Manual of Internal Fixation in the Cranio-Facial Skeleton; Prein, J., Ed.; Springer-Verlag: Berlin, Germany, 1998; pp. 57–92. [Google Scholar]
- Libersa, C. Etude anatomique de l’artere dentaire inferierure chez le foetus et chez l’adulte. Rev Stomatol (Paris) 1951, 4, 246. [Google Scholar]
- Brun, P. Quelques points d’anatomie sur la vascularisation arterielle du maxillaire inferieur. Rev Odontostomatol (Bordeaux) 1955, 13, 98. [Google Scholar]
- Goss, C.M. Gray’s Anatomy of the Human Body; Lea & Febiger: Philadelphia, PA, USA, 1959; pp. 628–630. [Google Scholar]
- Castelli, W. Vascular architecture of the human adult mandible. J Dent Res 1963, 42, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Kettunen, K. Arteriographic visualization of the alveolar (inferior dental) artery of the mandible. Br J Radiol 1965, 38, 599–601. [Google Scholar] [CrossRef] [PubMed]
- Castelli, W.A.; Nasjleti, C.E.; Díaz-Pérez, R. Interruption of the arterial inferior alveolar flow and its effects on mandibular collateral circulation and dental tissues. J Dent Res 1975, 54, 708–715. [Google Scholar] [CrossRef]
- Poirot, G.; Delattre, J.F.; Palot, C.; Flament, J.B. The inferior alveolar artery in its bony course. Surg Radiol Anat 1986, 8, 237–244. [Google Scholar] [CrossRef]
- Norton, N.S. Netter’s Head and Neck Anatomy for Dentistry; W.B. Saunders: Philadelphia, PA, USA, 2007; pp. 373–374. [Google Scholar]
- Cryer, M.H. Internal Anatomy of the Face, 2nd ed.; Lea & Febiger: Philadelphia, PA, USA, 1916; pp. 59–75. [Google Scholar]
- Knapp, D.E.; Avery, J.K.; Costich, E.R. A technique for the study of the internal structure of calcified tissues. J Dent Res 1958, 37, 880–885. [Google Scholar] [CrossRef]
- Dempster, W.T.; Enlow, D.H. Patterns of vascular channels in the cortex of the human mandible. Anat Rec 1959, 135, 189–205. [Google Scholar] [CrossRef]
- Cohen, L. Methods of investigating the vascular architecture of the mandible. J Dent Res 1959, 38, 920–931. [Google Scholar] [CrossRef]
- Huelke, D.F. The production of mandibular fractures: a study in high-speed cinematography. J Dent Res 1961, 40, 743. [Google Scholar]
- Huelke, D.F.; Patrick, L.M. Mechanics in the production of mandibular fracture: strain-gauge measurements of impacts to the chin. J Dent Res 1964, 43, 437–446. [Google Scholar] [CrossRef]
- Rudderman, R.H.; Phillips, P.H.; Mullen, R. Human facial finite analysis—redefining structural dynamics. In Proceedings of the University of Kentucky AO Foundation Visiting Professorship, Lexington, KY, USA, 27–28 April 2007. [Google Scholar]
- Huelke, D.F. Mandibular fractures and associated cervical spine injuries: revelations of high-speed film and other studies. In Proceedings of the Facial Fracture Surgery Symposium, Plastic Surgery Educational Foundation, Atlanta, GA, USA, 23–25 April 1987. [Google Scholar]
- Hudson, D.A.; Knottenbelt, J.D.; Krige, J.E. Closed degloving injuries: results following conservative surgery. Plast Reconstr Surg 1992, 89, 853–855. [Google Scholar] [CrossRef]
- Dula, D.J.; Leicht, M.J.; Moothart, W.E. Degloving injury of the mandible. Ann Emerg Med 1984, 13, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Letts, R.M. Degloving injuries in children. J Pediatr Orthop 1986, 6, 193–197. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, D.W.; Clark, M.V.; Lowe, J.W.; Harrington, M.S. Oral trauma in children: a hospital survey. Oral Surg Oral Med Oral Pathol 1989, 68, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Minten, L.; Hovius, S.E.; Gilbert, P.M. Degloving injuries. A retrospective study at the University Hospital Rotterdam. Acta Chir Belg 1992, 92, 209–212. [Google Scholar]
- Hudson, D.A.; Knottenbelt, J.D.; Krige, J.E. Closed degloving injuries: results following conservative surgery. Plast Reconstr Surg 1992, 89, 853–855. [Google Scholar] [CrossRef]
- Nelson, J.M.; Sawyer, M.A. Degloving injury from a helicopter rotor strike. Mil Med 1995, 160, 644–645. [Google Scholar] [CrossRef]
- Shockledge, R.; Mackie, I. Oral soft tissue trauma: gingival degloving. Endod Dent Traumatol 1996, 12, 109–111. [Google Scholar] [CrossRef]
- Rempel, J.H. Missed closed degloving injuries: late presentation as a contour deformity. Plast Reconstr Surg 1998, 101, 1159–1160. [Google Scholar] [CrossRef]
- McLaughlin, P.P. Degloving injury to mental protuberance: a case report. Int J Paediatr Dent 2000, 10, 234–236. [Google Scholar] [CrossRef] [PubMed]
- Revuelta, R.; Sándor, G.K. Degloving injury of the mandibular mucosa following an extreme sport accident: a case report. J Dent Child (Chic) 2005, 72, 104–106. [Google Scholar] [PubMed]
- Cadenat, H.; Barthélémy, R.; Combelles, R.; Fabié, M.; Maneaud, M. Importance of mandibular vascularization in maxillofacial surgery. Rev Stomatol Chir Maxillofac 1972, 73, 60–65. [Google Scholar] [PubMed]
- Epker, B.N. Vascular considerations in orthognathic surgery. I. Mandibular osteotomies. Oral Surg Oral Med Oral Pathol 1984, 57, 467–472. [Google Scholar] [CrossRef]


| Fracture(s) of the Anterior Segment with Partial or Total Disruption of Endosteal Blood Supply | |
|---|---|
| A | B |
| Traumatic degloving of buccal cortex, with partial or total disruption of mental, facial, and superior labial vessels Vestibular incision, if needed; broad exposure of bone fragments Manipulation and direct stabilization of fracture segments | Traumatic degloving of lingual cortex, with partial or total disruption of lingual, mylohyoid, and deep lingual vessels Submental incision; limited elevation of the buccal periosteum Manipulation and direct stabilization of fracture segments |
© 2011 by the author. The Author(s) 2011.
Share and Cite
Pollock, R.A.; Huber, K.M.; Van Sickels, J.E. Degloving Injuries of the Oral Cavity Change the Operative Approach to Fractures of the Anterior Segment of the Mandible. Craniomaxillofac. Trauma Reconstr. 2011, 4, 137-143. https://doi.org/10.1055/s-0031-1286116
Pollock RA, Huber KM, Van Sickels JE. Degloving Injuries of the Oral Cavity Change the Operative Approach to Fractures of the Anterior Segment of the Mandible. Craniomaxillofacial Trauma & Reconstruction. 2011; 4(3):137-143. https://doi.org/10.1055/s-0031-1286116
Chicago/Turabian StylePollock, Richard A., Katherine M. Huber, and Joseph E. Van Sickels. 2011. "Degloving Injuries of the Oral Cavity Change the Operative Approach to Fractures of the Anterior Segment of the Mandible" Craniomaxillofacial Trauma & Reconstruction 4, no. 3: 137-143. https://doi.org/10.1055/s-0031-1286116
APA StylePollock, R. A., Huber, K. M., & Van Sickels, J. E. (2011). Degloving Injuries of the Oral Cavity Change the Operative Approach to Fractures of the Anterior Segment of the Mandible. Craniomaxillofacial Trauma & Reconstruction, 4(3), 137-143. https://doi.org/10.1055/s-0031-1286116



