Abstract
The Tessier number 5 cleft is a rare craniofacial anomaly. Although there are case reports outlining various methods of primary surgical repair and outcomes, few cases reveal long-term follow-up or discuss secondary reconstruction. This article presents the case of a man born with a unilateral Tessier number 5 cleft who presented to our institution at the age of 41 after more than 25 previous surgeries. Over the course of 11 years, he had several surgeries including an orbital repositioning through a combined intraand extracranial approach, an orbital enucleation, and an anterolateral thigh flap. The patient was fitted with an orbital prosthesis and a satisfactory aesthetic result was achieved.
Number 5 Tessier clefts generally start medial to the commissure of the mouth and lateral to the philtral column (Figure 1). The cleft continues lateral to the anatomically normal nasal ala, onto the cheek, and extends through the lower eyelid. The lower eyelid has a coloboma in the middle third, with shortening of the distance between the lower eyelid and the mouth. The medial canthus is usually in a normal position, and the lateral canthus is deformed and malpositioned. The nasal ala is normal in structure but may be rotated toward the ipsilateral medial canthus. There is significant deficiency in the midface soft tissue. On the bony level, the cleft starts in the alveolus in the premolar region behind the canine. It extends upward, with the infraorbital nerve generally lying medial to the cleft. The cleft finally ends in the lateral portion of the inferior orbital floor. The bony deficiency of the inferior orbital floor and rim results in inferior displacement of the globe [1,2].

Figure 1.
Artist’s rendition of Tessier number 5 cleft.
Case Report
A 41-year-old man presented to our hospital with a past history of a left-sided Tessier craniofacial cleft number 5 (Figure 2). During the first two decades of his life, he had endured over 25 operative procedures for correction of his facial cleft, but finally conceded to his significant facial deformity. Twenty years later, he decided to continue with the reconstructive process. At the time of his first visit to our institution, he had marked orbital dystopia with inferior positioning of the left globe, minimal bony support of the orbital floor and left maxilla, and a blind left eye (Figure 3). A computed tomography scan of the facial bones revealed a hypoplastic left maxillary sinus with a posteriorly displaced anterior wall, a posteriorly displaced left zygomatic arch, an inferior depression of the orbital globe with no evidence of an inferior orbital rim, a small left middle cranial fossa, and a hard palate that was tilted cephalically on the affected side.
Figure 2.
Family photo of the patient shortly after birth.
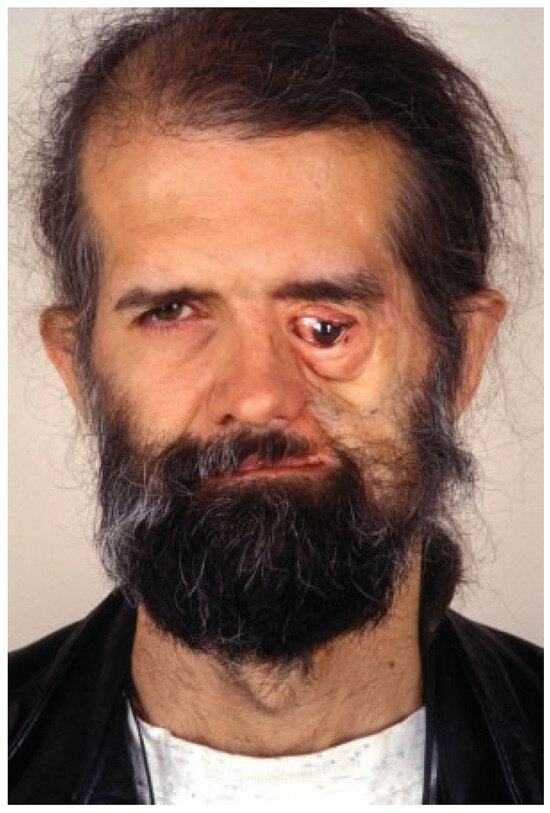
Figure 3.
The patient on presentation.
Over the next 10 years, he underwent multiple procedures at our institution. The initial procedure was at age 42 and included repositioning of his left orbit. This was an intraand extracranial procedure by the craniofacial and neurosurgical teams. First, a coronal incision was made and the left orbit was subperiosteally dissected free medially, laterally, and superiorly. The facial cleft was visualized in the inferior bony orbit, and the infraorbital rim and orbital floor were mostly absent. A left frontal craniotomy was performed for exposure of the roof of the orbit, with removal of the posterior wall of the frontal sinus. Osteotomies of the roof and medial and lateral walls of the orbit (extending into the facial cleft) were done. A left parietal craniectomy was subsequently performed for harvesting cranial bone. One bone graft was used to reconstruct the orbital rim and another to reconstruct the orbital floor and to raise the orbit. A lateral canthoplasty was performed, and a flap from the nasal facial groove was advanced onto the cheek for soft tissue coverage (Figure 4).
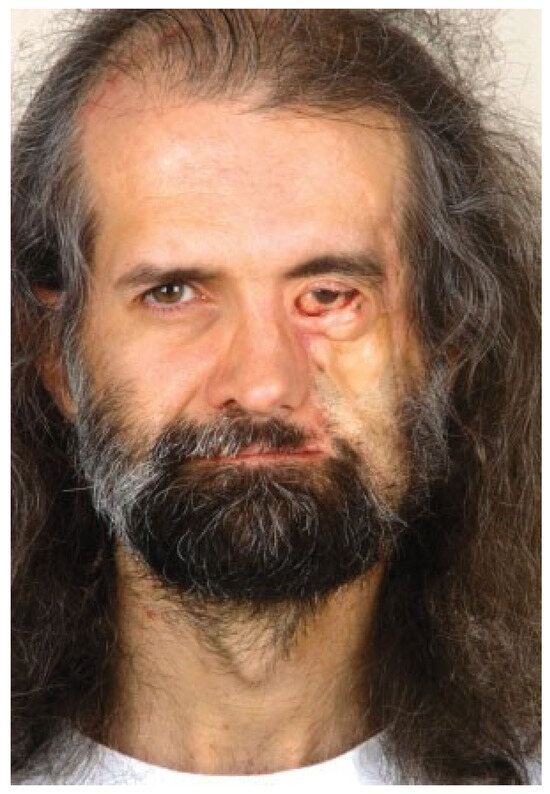
Figure 4.
The patient after the orbital repositioning.
Over the next several months, the patient underwent several procedures attempting to correct his ectropion and the cheek soft tissue deficiency. These included the insertion of three tissue expanders and subsequent advancement of adjacent tissues together with excision of a significant portion of the scarred lower eyelid and cheek. Other attempts at reconstruction of the lower eyelid included a medial canthoplasty, lateral canthoplasty, transposition flap from the upper eyelid, transposition flap from the side of the nose and cheek, and a postauricular skin graft. However, these multiple reconstructive procedures failed to correct the significant scarring and deformity in the cheek and lower eyelid. He subsequently had a left dacryocystorhinostomy that improved his nasolacrimal duct obstruction. Finally, a cranioplasty with calcium phosphate bone cement was performed for contour defect of the left frontoparietal area.
The patient was then lost to follow-up and returned 7 years later inquiring about further reconstructive options (Figure 5). He complained of feeling ‘‘flat’’ in the left cheek area and was dissatisfied with the appearance of his left eye. In addition, he had pain due to the significant conjunctivitis he had developed. At this point, he finally agreed to proceed with enucleation of his nonfunctioning eye as well as reconstruction of the left face and cheek to correct his major soft tissue deficit. A left orbital enucleation was then performed together with augmentation of the orbital rim with rib grafts and an anterolateral thigh free flap for soft tissue augmentation (Figure 6). The rib grafts were obtained and secured to the anterior maxilla, orbital rim, and lateral orbital wall. The anterolateral thigh flap vessels were anastomosed to the left facial artery and vein.

Figure 5.
Seven years after the orbital repositioning, the patient still complained of a significant aesthetic deformity with ectropion and cheek bone and soft tissue deficiency.
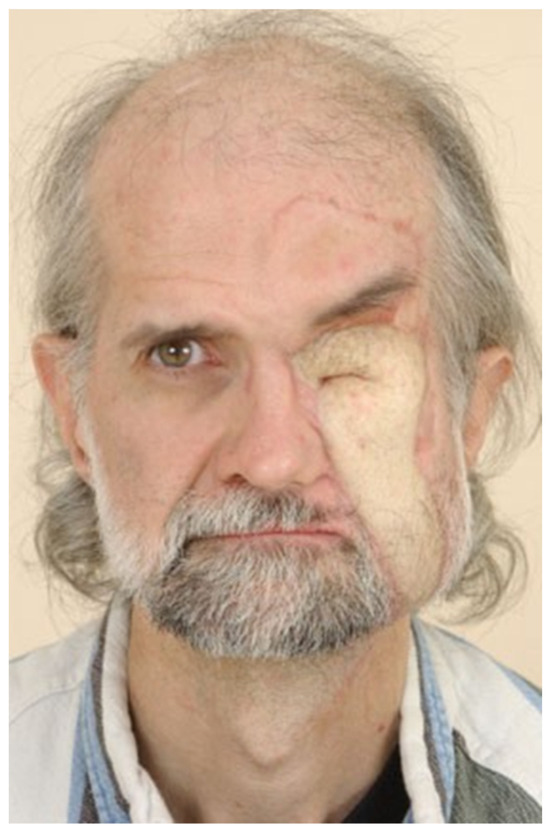
Figure 6.
The anterolateral thigh flap in place.
The patient underwent several revisions thereafter including thinning and liposuction of the anterolateral thigh flap, excision of part of the skin island of the flap, Z-plasty for repositioning of the left eyebrow of the flap, and full-thickness skin graft from the right groin to the upper orbital area. The patient was fitted with a prosthetic eye 8 months after the flap was performed (Figure 7 and Figure 8). More than 3 years after his last surgery, the patient is satisfied with his appearance and is tolerating the prosthesis well. No further surgeries are currently planned.
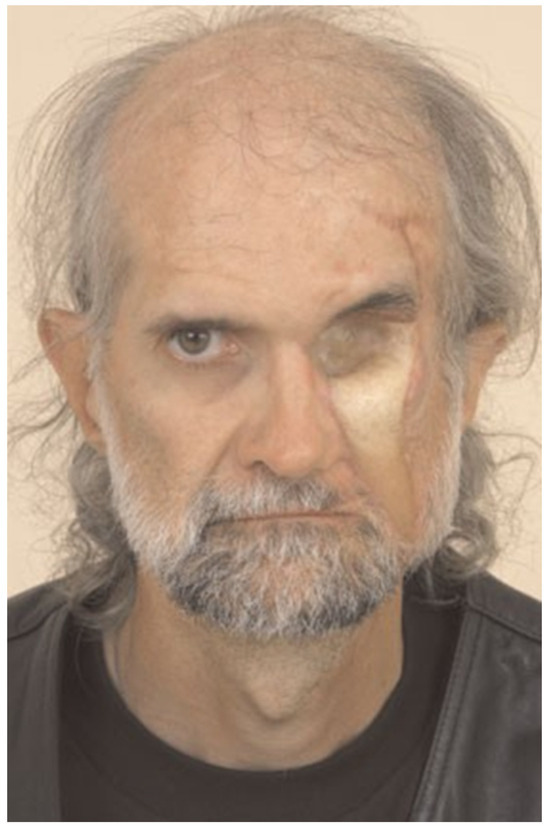
Figure 7.
The orbital socket prepared for the prosthesis.
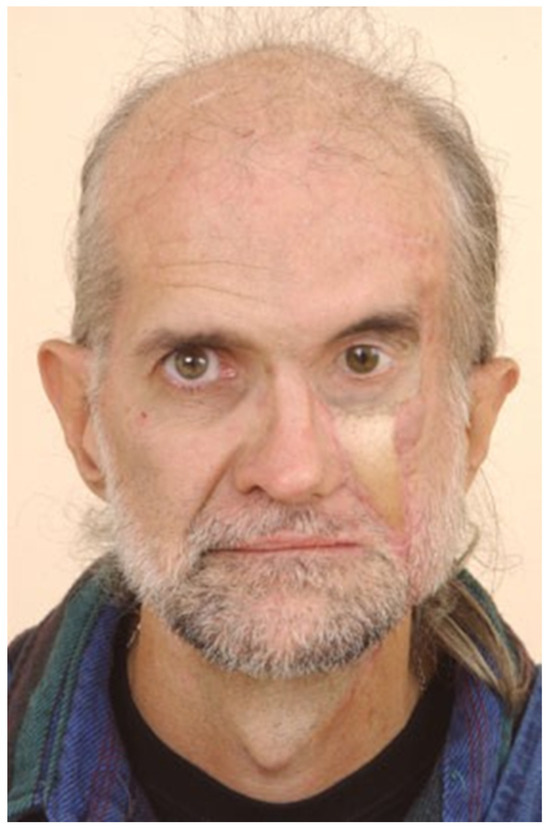
Figure 8.
Final outcome with the prosthesis in place.
Discussion
Craniofacial clefts are atypical congenital malformations occurring in ~1 to 5 per 100,000 live births [1,2,3,4,5,6,7]. The number 5 cleft of the Tessier classification system is an extraordinarily rare facial cleft, representing ~0.25% of all facial clefts [8,9]. Due to the low incidence and prevalence of this abnormality, there are a limited number of reported cases in the English-language literature, which infrequently include long-term follow-up. We hereby present a long-term follow-up report on managing late deformities associated with this craniofacial malformation 40 years following initial surgical management.
Like most craniofacial deformities, establishing a bony skeleton of appropriate dimensions and in the proper location will facilitate subsequent soft tissue reconstruction and enhance the aesthetic and functional outcomes [7]. Adhering to this philosophy, we initially performed intracranial repositioning of the left orbit together with iliac crest bone graft to reconstruct the orbital rim and floor. A known disadvantage of bone grafts is the unpredictable rate of bone resorption. It is hard to pinpoint the cause (bone resorption versus displacement), but several years after the original bony reconstruction, the orbital floor needed further augmentation by rib grafts.
Successful management of ectropion depends on the underlying etiology. In general, ectropion can be attributed to either lower-lid laxity, lack of lower eyelid support, tissue deficiency, or a combination of these factors. Minor cases of ectropion can be managed using traditional techniques such as lower-lid resection or lateral tarsal strip. Additional support for the lower eyelid can be achieved by augmenting the inferior tarsal plate with spacer grafts. However, in more severe cases with deficiency of eyelid tissues, as is typical in facial clefts, tissues must be imported into the lower eyelids [10]. The cheek advancement flap, first described by van der Meulen in 1985, has been advocated because of its efficacy and favorable scarring [7,8]. Other potential regional flaps are the median forehead flap and the nasolabial flap [7,11]. Tissue expansion has been promoted by Menard and colleagues, aiming to recruit adjacent healthy tissues [12,13]. The expansion allows for good skin color and texture match and ideally a tension-free closure [12].
In our patient, a lateral canthoplasty and a nasolabial flap were initially used but with limited success. It was apparent that the patient needed an aggressive removal of the scarred soft tissues and import of additional skin. This was attempted using tissue expanders, postauricular full-thickness graft, upper-eyelid flap, and cheek flaps. Multiple expansions and serial excisions were attempted but with a limited success. Free flaps have the advantage of providing unscarred skin that can be tailored to the demands of the defect, and therefore seemed to be the most logical solution to this problem [14,15]. In our case, this allowed correction of the ectropion, vascularized coverage of the rib grafts, and healthy lining of the bony orbit to accommodate the future prosthesis.
We achieved correction of the ectropion and augmentation of atrophied malar soft tissue with an anterolateral thigh flap. The anterolateral thigh flap is supplied by perforating vessels arising from the descending branch of the lateral circumflex femoral artery [16].
This flap is advantageous in that it can be harvested as a two-team approach, has a long vascular pedicle with suitable vessel diameter, can be sensate by including the lateral femoral cutaneous nerve, and can be tailored to suit variable defects [17]. Its major disadvantages include flap bulkiness (especially if the deep fascia is included in the flap) and color mismatch [18]. Our patient did require thinning and recontouring of his anterolateral thigh flap. In addition, serial excision of the skin island of the flap permitted a good aesthetic result.
The patient was counseled that because of his dissatisfaction with the appearance of his left eye, persistent ectropion, and the nonfunctioning globe, that the best aesthetic results could be obtained with an orbital implant. The primary benefit of enucleation and placement of an orbital prosthetic is enhanced cosmesis. Removal of a nonfunctioning globe can also be accomplished with evisceration where the sclera, Tenon’s capsule, conjunctiva, and optic nerve are preserved. Although the benefits of evisceration include diminished orbital fat atrophy and implant migration, there is the devastating complication of sympathetic ophthalmia, which can cause bilateral loss of vision [19,20]. This occurs when ocular antigens are released during evisceration, which incites an autoimmune response resulting in granulomatous uveitis in the normal eye. The autoimmune response is likely maintained because of the remaining ocular structures and antigens present in evisceration but removed in enucleation. The advantages of enucleation must be balanced against the disadvantages, which include intraoperative hemorrhage and postoperative infection or wound dehiscence [19]. Different prostheses are available to camouflage as a normal eye depending on the extent of the deformity. Scleral shells are fitted thin prosthesis placed directly over the globe. These shells are managed similarly to contact lenses and include the sclera and iris. Although these cosmetic scleral shells avoid potential operative complications, attentive hygienic maintenance is required, and the possibility exists for corneal irritation and patient discomfort. Additionally, facial cleft patients represent a unique challenge to designing appropriately fitting lenses due to contour irregularities of the ocular surface and the deficient eyelids [19]. An ocular prosthesis replaces the eyeball per se, and an orbital prosthesis replaces the eyeball and part of the surroundings (e.g., the eyelids). In our patient an orbital prosthesis was used. The globe is acrylic resin, and the surrounding orbital prosthesis is composed of silicone-based organic polymer custom colored to reflect the patient’s skin tone and texture. The main disadvantage is low tensile strength predisposing the periphery of the prosthesis to considerable wear and tear. An orbital prosthesis is held in place with an adhesive, as opposed to an orbital implant, which is anchored into the bone. This adhesive accelerates the breakdown of the implant and should ideally be changed several times daily. In addition to hygienic maintenance, the orbital prosthesis can loosen or become detached, causing significant embarrassment to the patient. An orbital implant avoids these disadvantages but requires another surgical procedure along with sufficient bone quality to anchor the implant, which may not be present in facial cleft patients [21]. Orbital implants carry a risk of extrusion, migration, infection, and bony resorption (creating a lax socket) [21,22]. The latter yields an improperly fitting implant that can cause chronic inflammation, which eventually results in a contracted socket requiring surgical intervention [21,23,24]. In addition, because all forms of prosthetics require long-term care, many patients opt to use a black patch or no prosthesis, limiting their use of the prosthetics to social occasions or family photos.
In conclusion, we present a late presentation of a facial cleft number 5 and the patient’s journey through multiple reconstructive attempts. In retrospect, it is clear that more aggressive procedures (i.e., radical excision of scarred tissues, free flaps, orbital enucleation) proved to be more effective and time efficient. This case illustrates the importance of collaboration between the craniofacial surgeon, the microsurgeon, and the prosthetist to achieve an aesthetic outcome.
References
- Tessier, P. Anatomical classification facial, cranio-facial and latero-facial clefts. J. Maxillofac. Surg. 1976, 4, 69–92. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, H.K., Jr. The kaleidoscopic world of rare craniofacial clefts: Order out of chaos (Tessier classification). Clin. Plast. Surg. 1976, 3, 529–572. [Google Scholar] [PubMed]
- David, D.J.; Moore, M.H.; Cooter, R.D. Tessier clefts revisited with a third dimension. Cleft Palate J. 1989, 26, 163–184; discussion 184–185. [Google Scholar]
- Resnick, J.I.; Kawamoto, H.K., Jr. Rare craniofacial clefts: Tessier No. 4 clefts. Plast. Reconstr. Surg. 1990, 85, 843–849; discussion 850–852. [Google Scholar] [CrossRef]
- Thorne, C.H. Craniofacial clefts. Clin. Plast. Surg. 1993, 20, 803–814. [Google Scholar] [CrossRef]
- Eppley, B.L.; van Aalst, J.A.; Robey, A.; Havlik, R.J.; Sadove, A.M. The spectrum of orofacial clefting. Plast. Reconstr. Surg. 2005, 115, 101e–114e. [Google Scholar]
- van der Meulen, J.C.H. Oblique facial clefts: Pathology, etiology, and reconstruction. Plast. Reconstr. Surg. 1985, 76, 212–224. [Google Scholar]
- da Silva Freitas, R.; Alonso, N.; Shin, J.H.; Busato, L.; Dall’Oglio Tolazzi, A.R.; de Oliveria e Cruz, G.A. The Tessier number 5 facial cleft: Surgical strategies and outcomes in six patients. Cleft Palate-Craniofac. J. 2009, 46, 179–186. [Google Scholar]
- Galante, G.; Dado, D.V. The Tessier number 5 cleft: A report of two cases and a review of the literature. Plast. Reconstr. Surg. 1991, 88, 131–135. [Google Scholar]
- Stretch, J.R.; Poole, M.D. Nasolacrimal abnormalities in oblique facial clefts. Br. J. Plast. Surg. 1990, 43, 463–467. [Google Scholar]
- Longaker, M.T.; Lipshutz, G.S.; Kawamoto, H.K., Jr. Reconstruction of Tessier No. 4 clefts revisited. Plast. Reconstr. Surg. 1997, 99, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Menard, R.M.; Moore, M.H.; David, D.J. Tissue expansion in the reconstruction of Tessier craniofacial clefts: A series of 17 patients. Plast. Reconstr. Surg. 1999, 103, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Aköz, T.; Erdoǧan, B.; Görgü, M.; Kutlay, R.; Daǧ, F. Bilaterally involved Tessier No. 4 cleft: Case report. Cleft Palate Craniofac. J. 1996, 33, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Tweed, A.E.J.; Manktelow, R.T.; Zuker, R.M. Facial contour reconstruction with free flaps. Ann. Plast. Surg. 1984, 12, 313–320. [Google Scholar] [CrossRef]
- Longaker, M.T.; Siebert, J.W. Microsurgical correction of facial contour in congenital craniofacial malformations: The marriage of hard and soft tissue. Plast. Reconstr. Surg. 1996, 98, 942–950. [Google Scholar] [CrossRef]
- Mäkitie, A.A.; Beasley, N.J.; Neligan, P.C.; Lipa, J.; Gullane, P.J.; Gilbert, R.W. Head and neck reconstruction with anterolateral thigh flap. Otolaryngol. Head Neck Surg. 2003, 129, 547–555. [Google Scholar] [CrossRef]
- Chen, C.M.; Chen, C.H.; Lai, C.S.; Lin, S.D.; Huang, I.Y.; Shieh, T.Y. Anterolateral thigh flaps for reconstruction of head and neck defects. J. Oral. Maxillofac. Surg. 2005, 63, 948–952. [Google Scholar] [CrossRef]
- Mureau, M.A.M.; Posch, N.A.S.; Meeuwis, C.A.; Hofer, S.O. Anterolateral thigh flap reconstruction of large external facial skin defects: A follow-up study on functional and aesthetic recipientand donor-site outcome. Plast. Reconstr. Surg. 2005, 115, 1077–1086. [Google Scholar] [CrossRef]
- Dortzbach, R.K.; Woog, J.J. Choice of procedure. Enucleation, evisceration, or prosthetic fitting over globes. Ophthalmology 1985, 92, 1249–1255. [Google Scholar] [CrossRef]
- Green, W.R.; Maumenee, A.E.; Sanders, T.E.; Smith, M.E. Sympathetic uveitis following evisceration. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1972, 76, 625–644. [Google Scholar]
- Shoamanesh, A.; Pang, N.K.; Oestreicher, J.H. Complications of orbital implants: A review of 542 patients who have undergone orbital implantation and 275 subsequent PEG placements. Orbit 2007, 26, 173–182. [Google Scholar] [PubMed]
- Chalasani, R.; Poole-Warren, L.; Conway, R.M.; Ben-Nissan, B. Porous orbital implants in enucleation: A systematic review. Surv. Ophthalmol. 2007, 52, 145–155. [Google Scholar] [PubMed]
- Cepela, M.; Teske, S. Orbital implants. Curr. Opin. Ophthalmol. 1996, 7, 38–42. [Google Scholar] [PubMed]
- Christmas, N.J.; Gordon, C.D.; Murray, T.G.; et al. Intraorbital implants after enucleation and their complications: A 10-year review. Arch. Ophthalmol. 1998, 116, 1199–1203. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2011 by the author. The Author(s) 2011.