Subcranial Approach in Pediatric Craniofacial Surgery
Abstract
:Methods
- Bicoronal incision, elevation of the frontal flap up to the nasal dorsum, with visualization of the lower edge of the nasal bones, and release of the supraorbital nerves
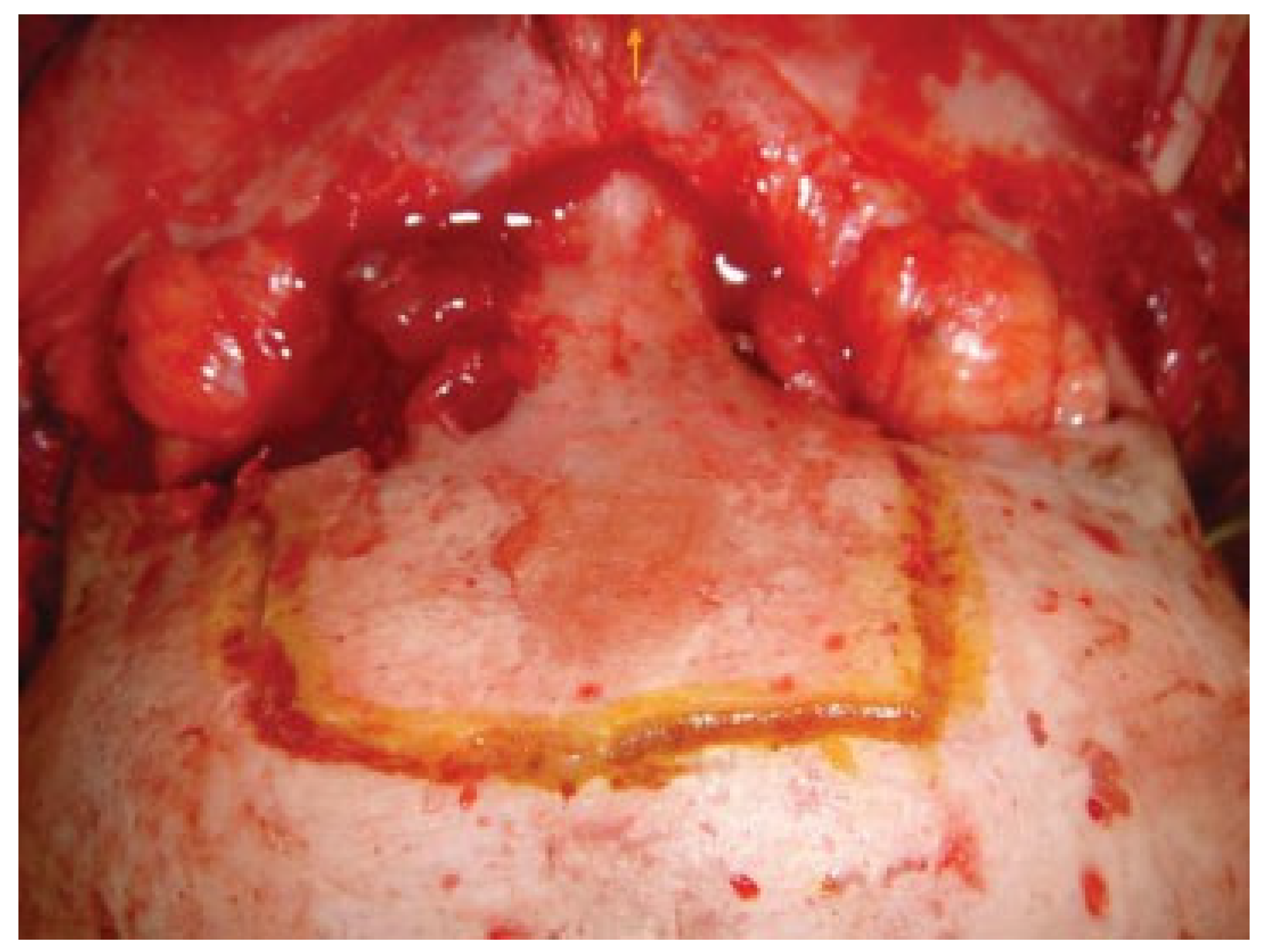
- Bone carving of a plaque that includes the central region of the frontal bone, with its external limits in the supraorbital nerves (Figure 1)
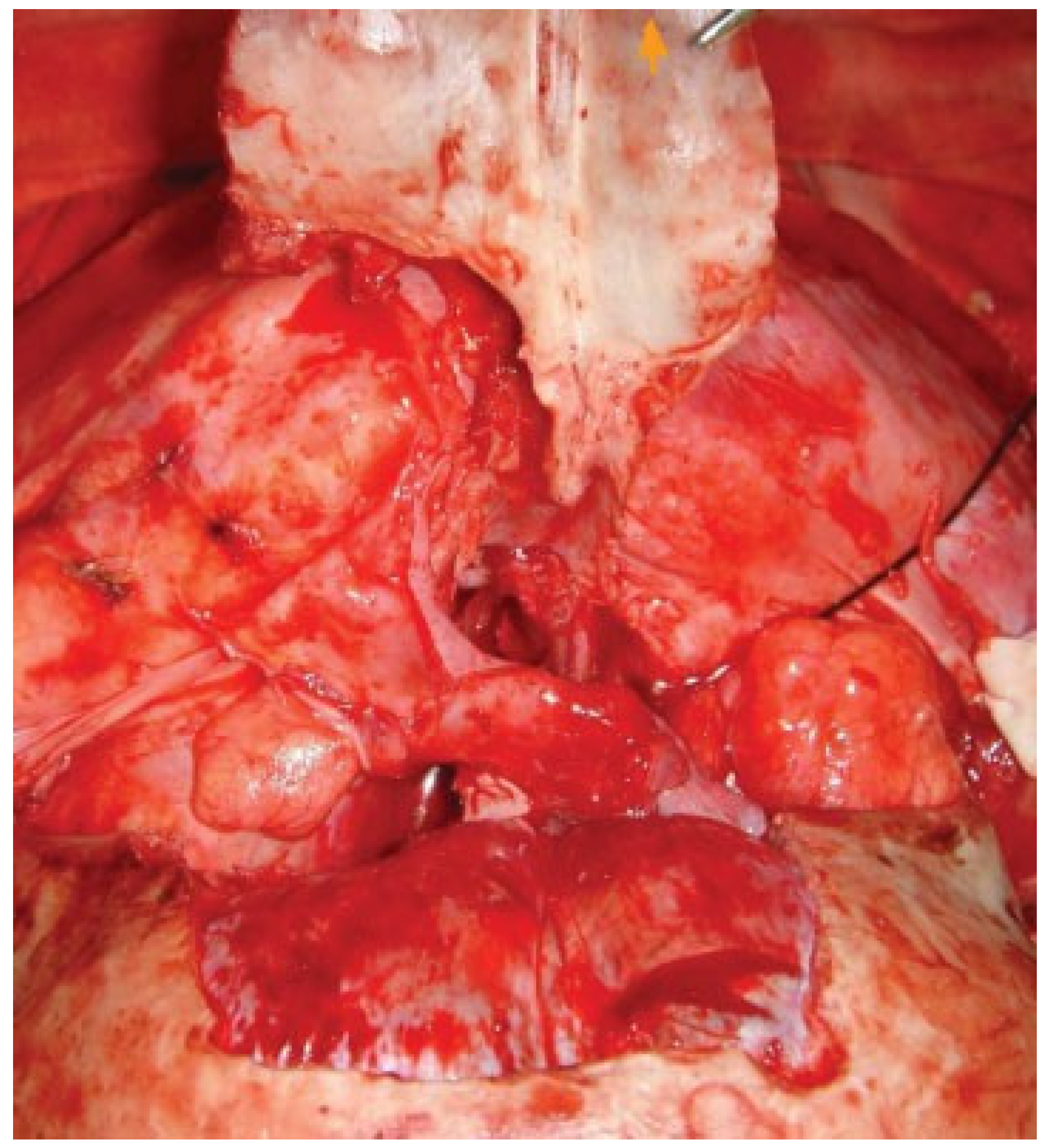
- Lifting bone plaque, leaving, if possible, the periostium attached to the lower end of nasal bone (Figure 2)
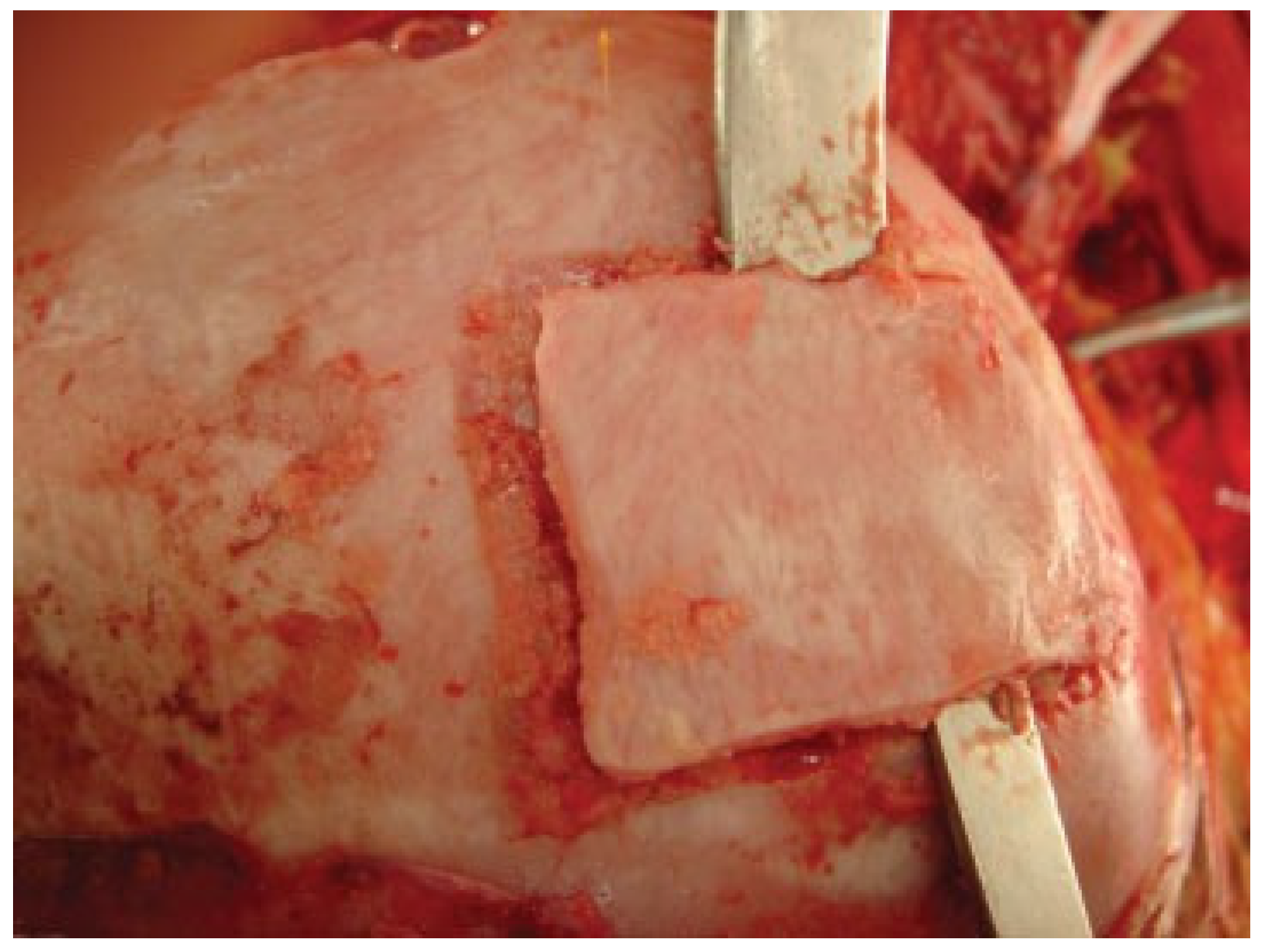
- Treatment of tumor/trauma and eventual reconstruction of the orbital wall or floor of the anterior cranial fossa with a bone graft (Figure 3)
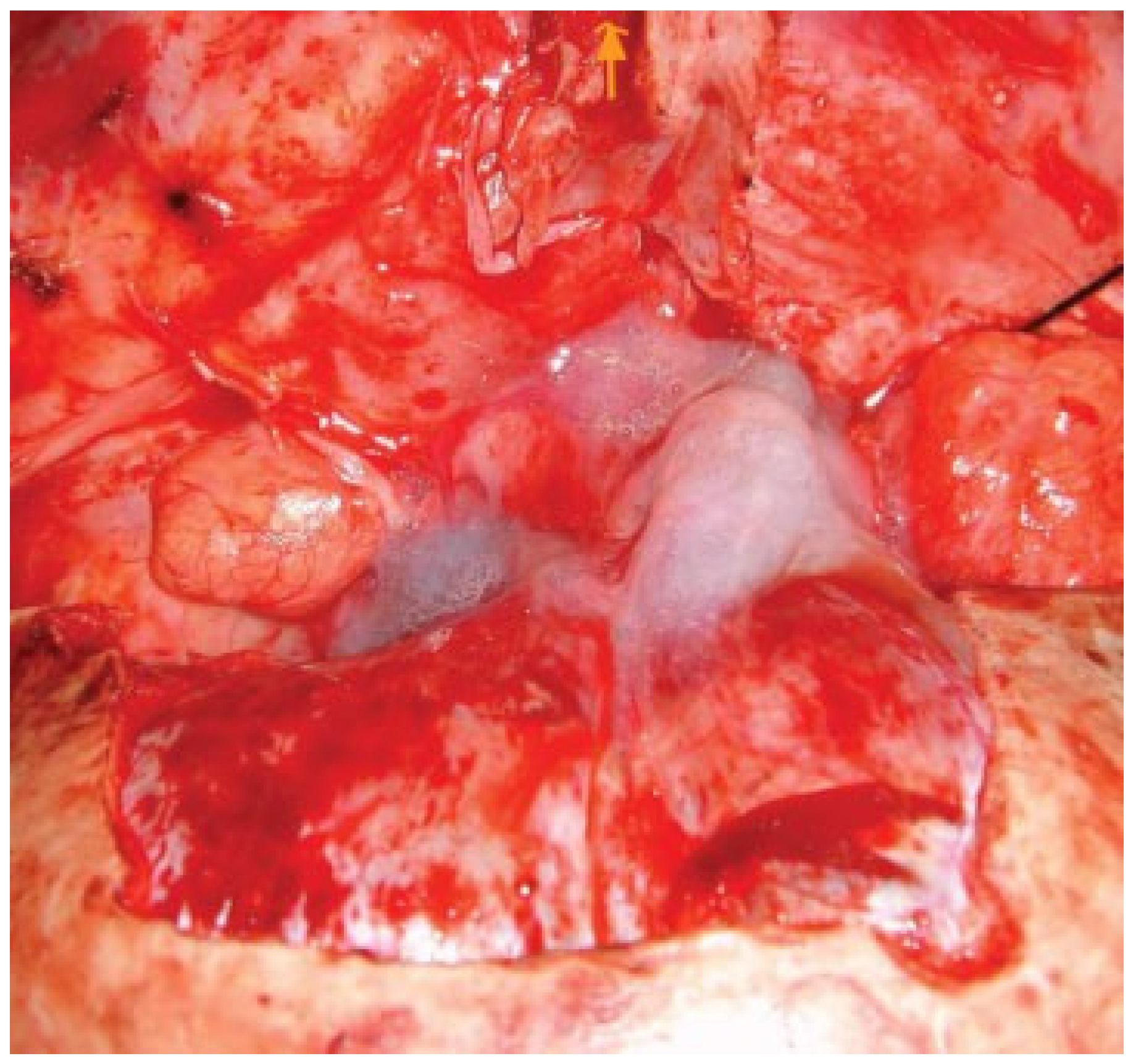
- Sealing of the surgical area with galea flap and fibrin glue (Figure 4)
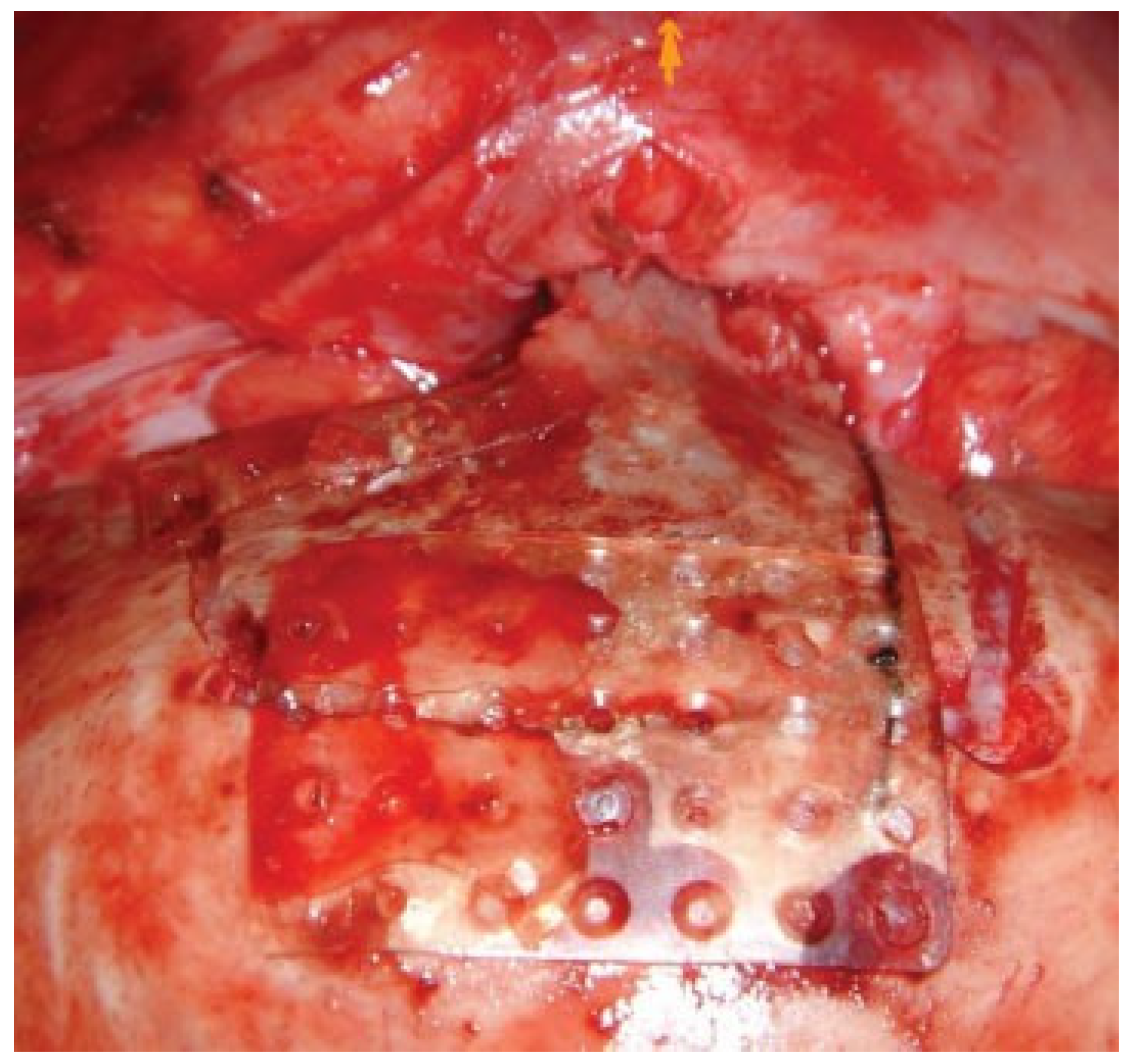
- Repositioning and fixation of the bone plaque (we preferred bioabsorbable mesh) ( Figure 5 )
- Repositioning and closure of the frontal flap
Discussion
Conclusions
References
- Raveh, J.; Redli, M.; Markwalder, T.M. Operative management of 194 cases of combined maxillofacial-frontobasal fractures: Principles and surgical modifications. J. Oral. Maxillofac. Surg. 1984, 42, 555–564. [Google Scholar] [PubMed]
- Raveh, J.; Vuillemin, T. The surgical one-stage management of combined cranio-maxillo-facial and frontobasal fractures. Advantages of the subcranial approach in 374 cases. J. Craniomaxillofac. Surg. 1988, 16, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Raveh, J.; Vuillemin, T. Subcranial-supraorbital and temporal approach for tumor resection. J. Craniofacial Surg. 1990, 1, 53–59. [Google Scholar]
- Raveh, J.; Vuillemin, T. Advantages of an additional subcranial approach in the correction of craniofacial deformities. J. Craniomaxillofac. Surg. 1988, 16, 350–358. [Google Scholar]
- Raveh, J.; Laedrach, K.; Speiser, M.; Chen, J.; Vuillemin, T.; Seiler, R.; Ebeling, U. The subcranial approach for fronto-orbital and anteroposterior skull-base tumors. Arch. Otolaryngol. Head Neck Surg. 1993, 119, 385–393. [Google Scholar]
- Kellman, R.M.; Goyal, P.; Rodziewicz, G.S. The transglabellar subcranial approach for nasal dermoids with intracranial extension. Laryngoscope 2004, 114, 1368–1372. [Google Scholar] [CrossRef]
- Goyal, P.; Kellman, R.M.; Tatum, S.A., III. Transglabellar subcranial approach for the management of nasal masses with intracranial extension in pediatric patients. Arch. Facial Plast. Surg. 2007, 9, 314–317. [Google Scholar] [CrossRef]
- Gil, Z.; Constantini, S.; Spektor, S.; Abergel, A.; Khafif, A.; Beni-Adani, L.; Leonor, T.-L.; DeRowe, A.; Fliss, D.M. Skull base approaches in the pediatric population. Head Neck 2005, 27, 682–689. [Google Scholar]
- Jung, T.M.; TerKonda, R.P.; Haines, S.J.; Strome, S.; Marentette, L.J. Outcome analysis of the transglabellar/subcranial approach for lesions of the anterior cranial fossa: A comparison with the classic craniotomy approach. Otolaryngol. Head Neck Surg. 1997, 116 Pt 1, 642–646. [Google Scholar] [CrossRef]
- Kellman, R.M.; Marentette, L. The transglabellar/subcranial approach to the anterior skull base: A review of 72 cases. Arch. Otolaryngol. Head Neck Surg. 2001, 127, 687–690. [Google Scholar] [CrossRef]
- Raveh, J.; Vuillelmin, T. Advantages of the subcranial approach in craniofacial surgery. In Rigid Fixation of the Craniofacial Skeleton; Yaremchuk, M., Gruss, J., Manson, P., Eds.; Butterworth-Heinemann: Boston, MA, USA, 1992; p. 56. [Google Scholar]
- Fliss, D.M.; Zucker, G.; Amir, A.; Gatot, A. The combined subcranial and midfacial degloving technique for tumor resection: Report of three cases. J. Oral. Maxillofac. Surg. 2000, 58, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Fliss, D.M.; Abergel, A.; Cavel, O.; Margalit, N.; Gil, Z. Combined subcranial approaches for excision of complex anterior skull base tumors. Arch. Otolaryngol. Head Neck Surg. 2007, 133, 888–896. [Google Scholar]
- Weiss, D.D.; Robson, C.D.; Mulliken, J.B. Transnasal endoscopic excision of midline nasal dermoid from the anterior cranial base. Plast. Reconstr. Surg. 1998, 102, 2119–2123. [Google Scholar] [PubMed]
- Moore, C.E.; Ross, D.A.; Marentette, L.J. Subcranial approach to tumors of the anterior cranial base: Analysis of current and traditional surgical techniques. Otolaryngol. Head Neck Surg. 1999, 120, 387–390. [Google Scholar] [PubMed]
- Shlomi, B.; Chaushu, S.; Gil, Z.; Chaushu, G.; Fliss, D.M. Effects of the subcranial approach on facial growth and development. Otolaryngol. Head Neck Surg. 2007, 136, 27–32. [Google Scholar]
- Fliss, D.M.; Zucker, G.; Amir, A.; Gatot, A.; Cohen, J.T.; Spektor, S. The subcranial approach for anterior skull base tumors. Oper. Tech. Otolaryngol. Head Neck Surg. 2000, 11, 238–253. [Google Scholar]
- Fliss, D.M.; Gil, Z.; Spektor, S.; Leider-Trejo, L.; Abergel, A.; Khafif, A.; Amir, A.; Gur, E.; Cohen, J.T. Skull base reconstruction after anterior subcranial tumor resection. Neurosurg. Focus. 2002, 12, e10. [Google Scholar]
- To, E.W.; Pang, P.C.; Chan, D.T.; Lam, J.M. Subcranial anterior skull base dural repair with galeal frontalis flap. Br. J. Plast. Surg. 2001, 54, 457–460. [Google Scholar]
- Laedrach, K.; Lukes, A.; Raveh, J. Reconstruction of skull base and fronto-orbital defects following tumor resection. Skull Base 2007, 17, 59–72. [Google Scholar]
- Fliss, D.M.; Zucker, G.; Cohen, A.; Amir, A.; Sagi, A.; Rosenberg, L.; Leiberman, A.; Gatot, A.; Reichenthal, E. Early outcome and complications of the extended subcranial approach to the anterior skull base. Laryngoscope 1999, 109, 153–160. [Google Scholar]
- Shohet, M.R.; Laedrach, K.; Guzman, R.; Raveh, J. Advances in approaches to the cranial base: Minimizing morbidity. Facial Plast. Surg. 2008, 24, 129–134. [Google Scholar] [CrossRef] [PubMed]




| Diagnosis | Age | Sex | Follow-up (y) | Complications |
|---|---|---|---|---|
| Naso-orbital meningioma | 7 y | F | 12 | Orbital recurrence; frontal alteration |
| Nasal dermoid cyst | 3 y, 6 mo | F | 3 | No complications |
| Nasal dermoid cyst | 2 y, 3 mo | F | 2 | No complications |
| Nasal dermoid cyst | 4 y | M | 3 | Local infection; reoperation |
| Nasal dermoid cyst | 4 y, 2 mo | M | 1 | No complications |
| Vascular tumor (nonspecific) | 9 y | F | — | Death at 10 d postsurgery (stroke) |
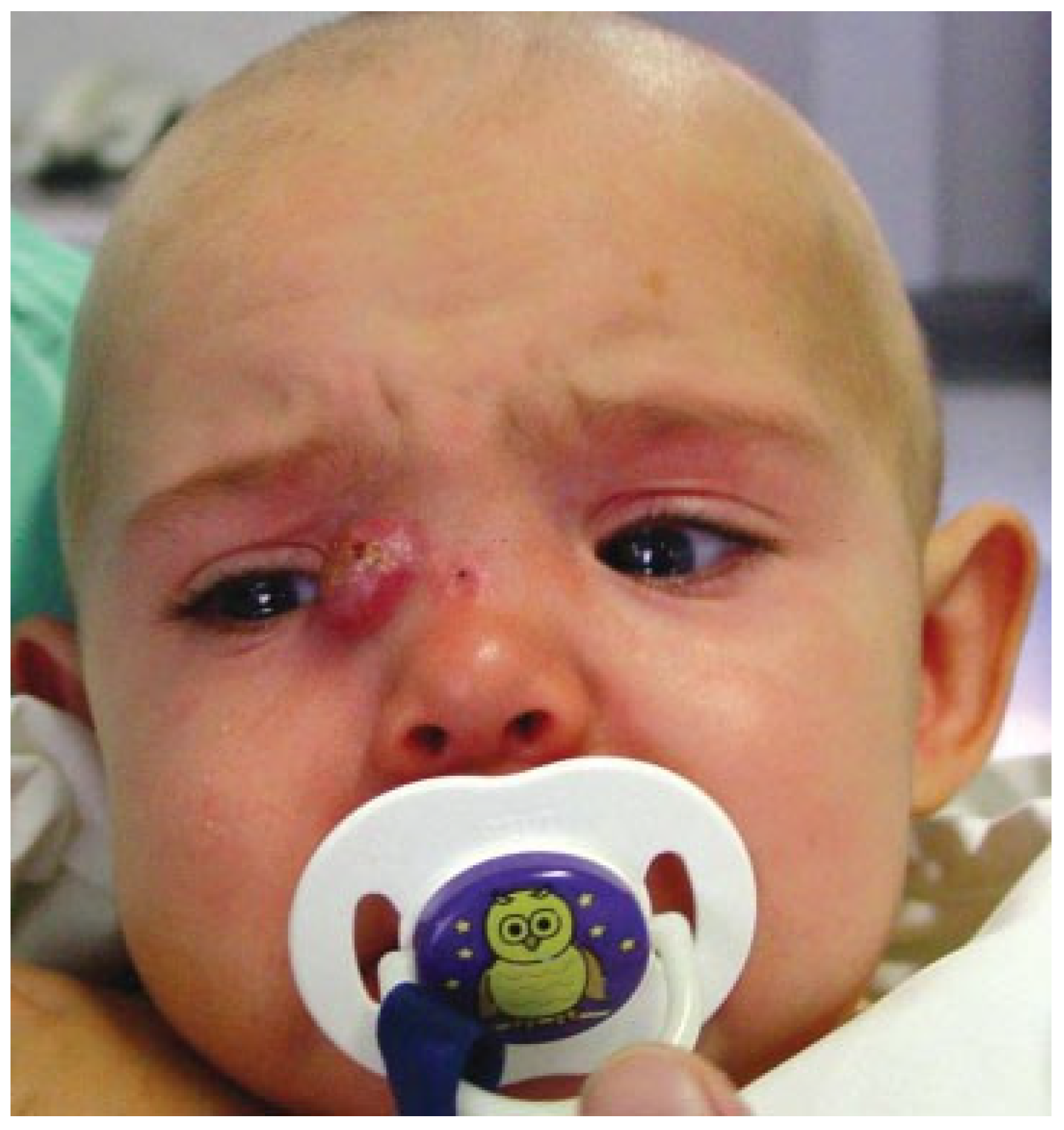
| Nasal dermoid cyst | 20 m | F | 5 | Nasal discharge; medical treatment |
| Orbital fibrous dysplasia | 3 y, 5 mo | F | 3 | No complications |
| Frontal mucocele | 14 y | M | 8 | No complications |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2010 by the author. The Author(s) 2010.
Share and Cite
Ciechomski, J.; Aufgang, R.; Villanueva, L.; Demarchi, V. Subcranial Approach in Pediatric Craniofacial Surgery. Craniomaxillofac. Trauma Reconstr. 2010, 3, 231-235. https://doi.org/10.1055/s-0030-1268521
Ciechomski J, Aufgang R, Villanueva L, Demarchi V. Subcranial Approach in Pediatric Craniofacial Surgery. Craniomaxillofacial Trauma & Reconstruction. 2010; 3(4):231-235. https://doi.org/10.1055/s-0030-1268521
Chicago/Turabian StyleCiechomski, Jorge, Ruben Aufgang, Lucrecia Villanueva, and Victoria Demarchi. 2010. "Subcranial Approach in Pediatric Craniofacial Surgery" Craniomaxillofacial Trauma & Reconstruction 3, no. 4: 231-235. https://doi.org/10.1055/s-0030-1268521
APA StyleCiechomski, J., Aufgang, R., Villanueva, L., & Demarchi, V. (2010). Subcranial Approach in Pediatric Craniofacial Surgery. Craniomaxillofacial Trauma & Reconstruction, 3(4), 231-235. https://doi.org/10.1055/s-0030-1268521



