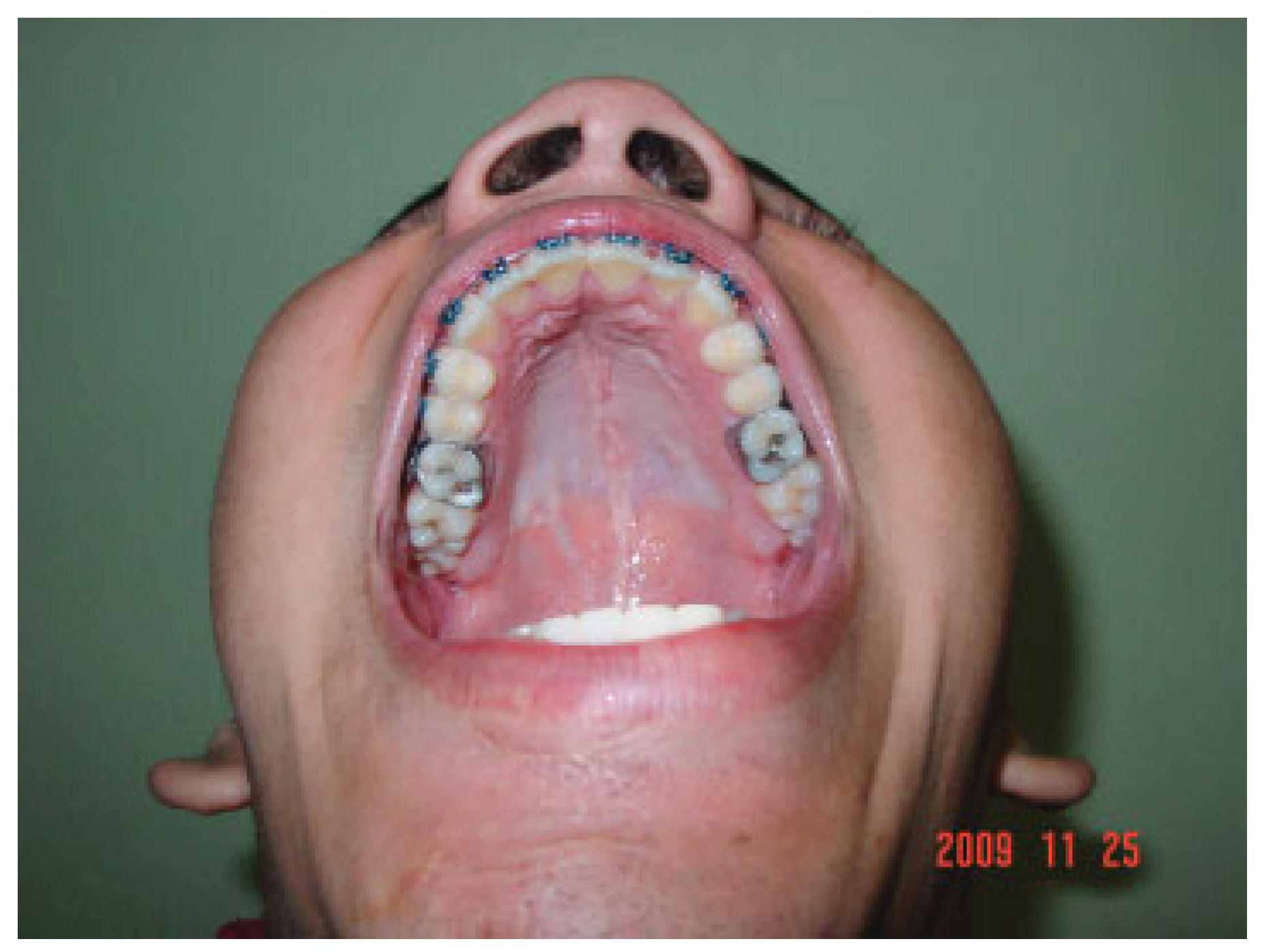
Palatal fractures are not common as an isolated diagnosis in patients with craniofacial trauma. They are usually associated with midfacial or panfacial fractures, and they are reported to be associated with 8 to 13.2% of cases of Le Fort fractures [
1,
2,
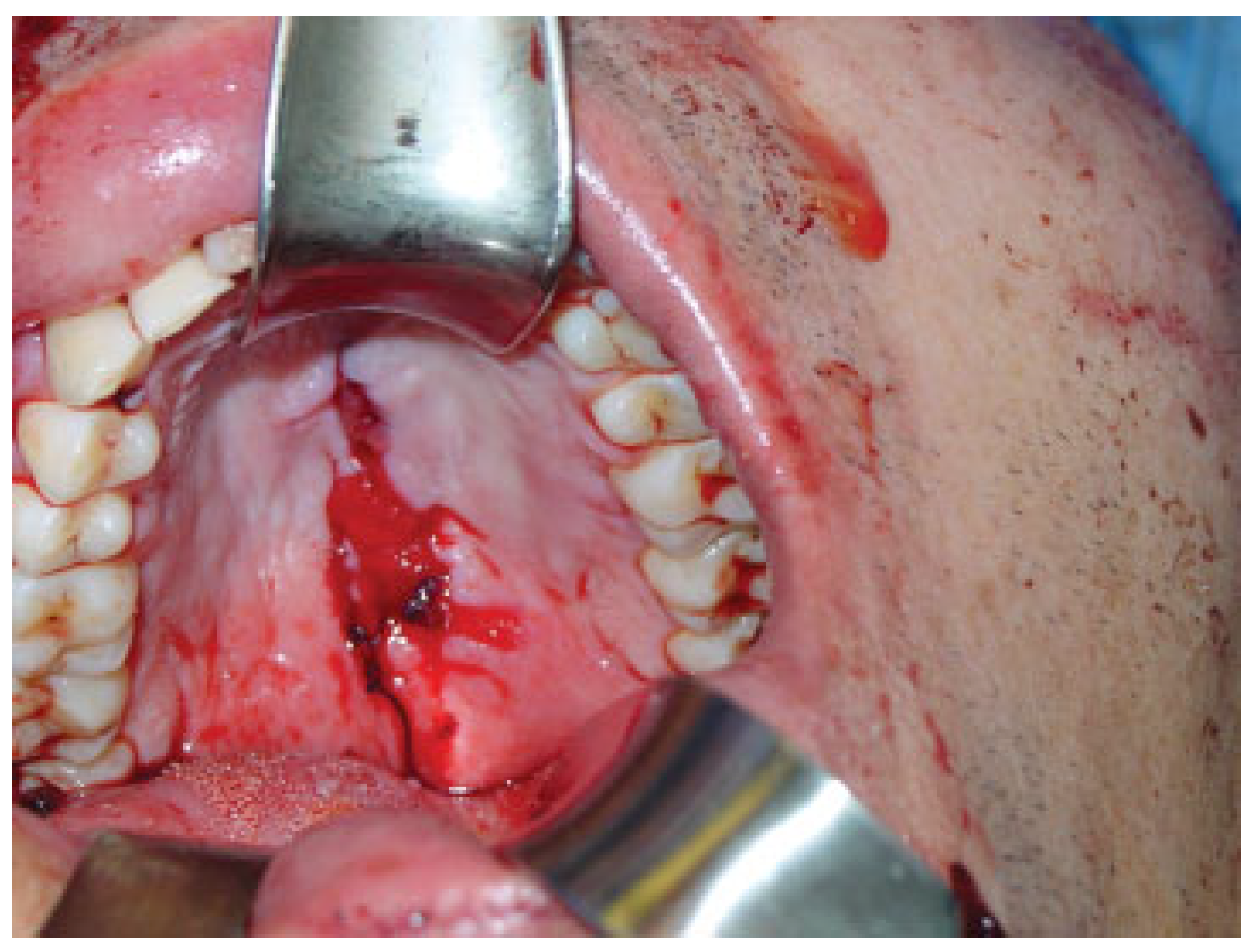
3]. Clinical signs suggestive of these fractures should be intentionally sought, such as palatal ecchymosis in closed fractures and lacerations of the upper lip or the palatal mucosa, loss of incisor teeth, or disruption of the occlusal relation in dislocated fractures (
Figure 1,
Figure 2 and
Figure 3). Computed tomography (CT) scans performed with thin sections, every 1.0 to 1.5 mm, display the fracture clearly.
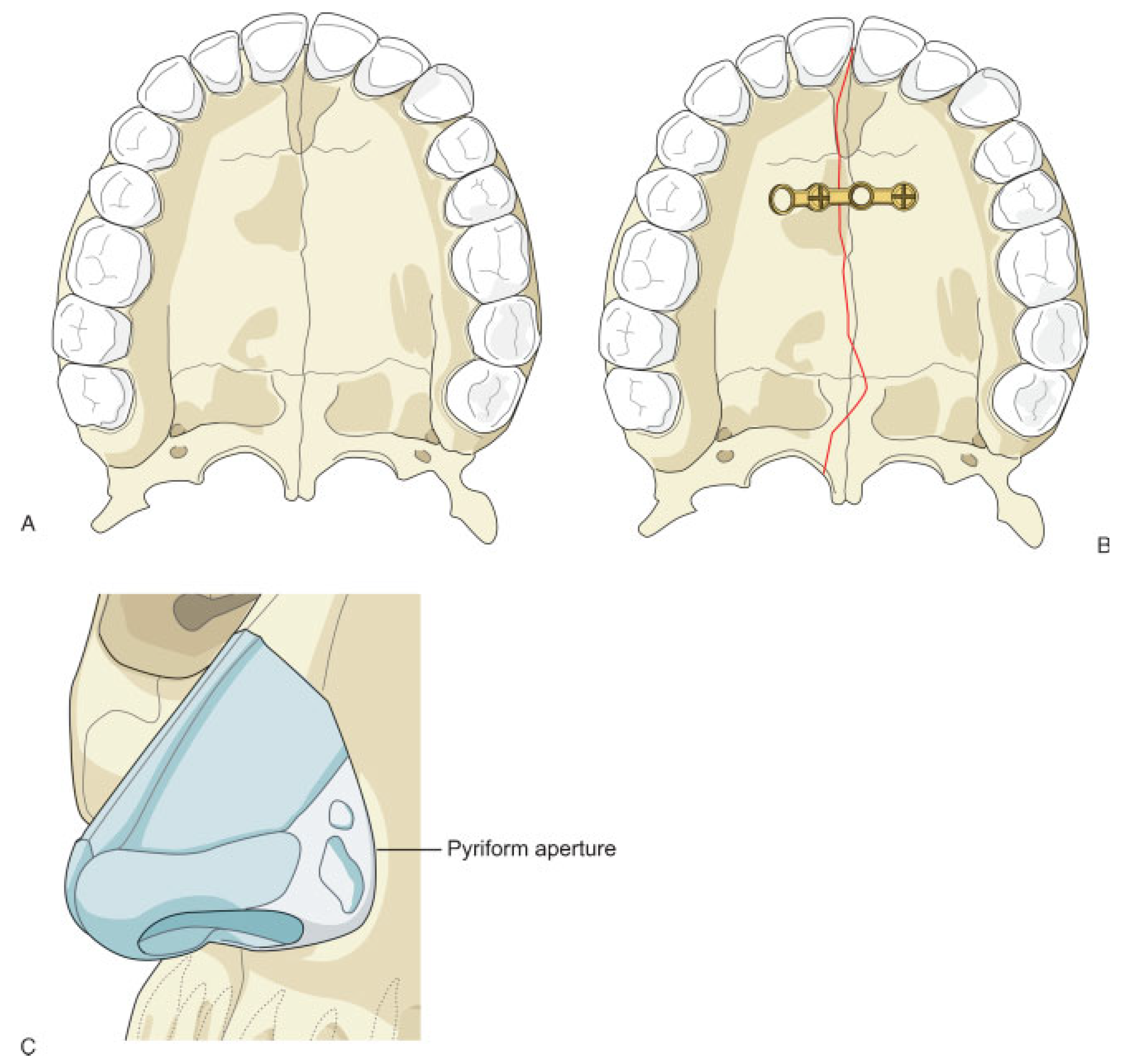
Treatment options for palatal fractures range from orthodontic braces, acylated arch bars, and arch bars for maxillomandibular fixation to internal fixation, with plates and screws placed under the palate mucosa and periosteum, together with pyriform aperture or alveolar plating plus LeFort level I buttress reconstruction (
Figure 4 and
Figure 5).
We propose the use of medium- or high-profile locking plates placed over the palatal mucosa an external fixator for palatal fractures, together with treatment for any associated facial fractures (
Figure 6). This approach achieves adequate stability, reduces the risk of bone and mucosal necrosis, and promotes healing of mucosal wounds in case of open fractures.
Treatment of Palatal Fractures
Treatment of palatal fractures is planned and performed with the goal of restoring the transverse width of the palate, the anteroposterior projection of the maxillary arch, and the patient’s pretraumatic occlusal plane, as well as maintaining horizontal stability of the midface. Despite a widely accepted classification, there are no solid indications for use of the various treatment approaches that may be used.
As early as 1983, Manson et al. noted the instability arising from conventional methods of fixation and suggested that more precise and predictable results could be achieved with a combination of techniques for open reduction and internal fixation, such as an arch bar and a palatal splint [
4,
5]. More recently, he and other authors have considered that the comprehensive treatment of palatal fractures should include plating the alveolus and pyriform aperture and using rigid fixation of the medial and lateral buttresses of the maxilla, and the palatal vault. They stress that treatment should be individualized depending on the fracture pattern [
3,
6].
Open palatal fractures may cause profuse bleeding that should be controlled by reducing the fracture. Control of bleeding may be temporarily achieved by placing arch bars on the maxilla, with interdental wiring around the teeth involved in the fracture, or interdental maxillary 8-shaped wiring placed around molars from one side to the other. The latter may be also used as an ancillary technique in fracture reduction (tension band principle) prior to osteosynthesis, as it aids in restoring palatal width (
Figure 7).
Methods and Materials
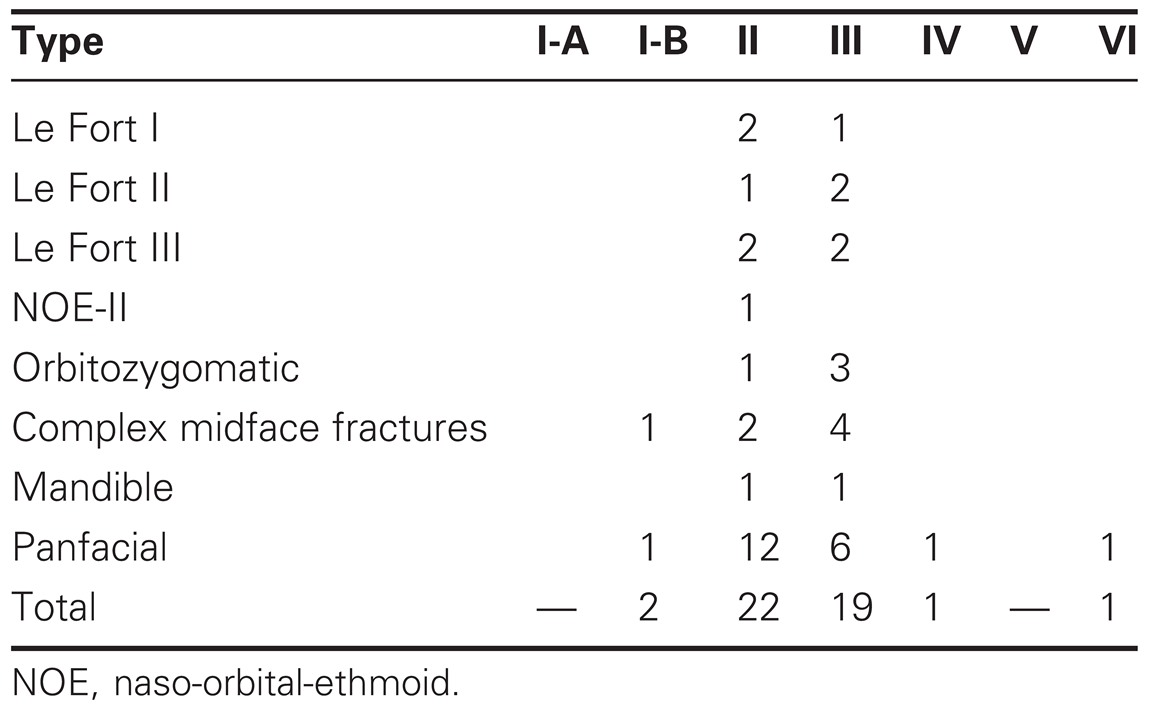
Forty-five consecutive patients with palatal fractures of various types, classified according to Hendrickson et al. [
1]. were treated with 2.0-mm locking plates and screws (Unilock®, Synthes, Paoli, PA). Plates were placed over the palatal mucosa, using the osteosynthesis as an external fixator, in contrast with nonlocking systems, which require raising mucoperiosteal flaps to place them in close contact to bone.
The inclusion period for such treatment was from October 2005 through April 2009. The patients included 41 males and four females, with ages ranging from 4 to 56 years old (average, 33.2). Three patients who did not complete 12 weeks of postoperative followup were excluded.
By far, the most common cause for fractures was motor vehicle accident (42 patients), followed by work accidents (one patient), firearm injury (one patient), and attempted suicide by jumping (one patient). Palate fractures were open in 23 patients and closed in 22. All patients had associated facial fractures. Fracture distribution according to the classification by Hendrickson, as well as frequency of associated facial fractures, are shown in
Table 1.
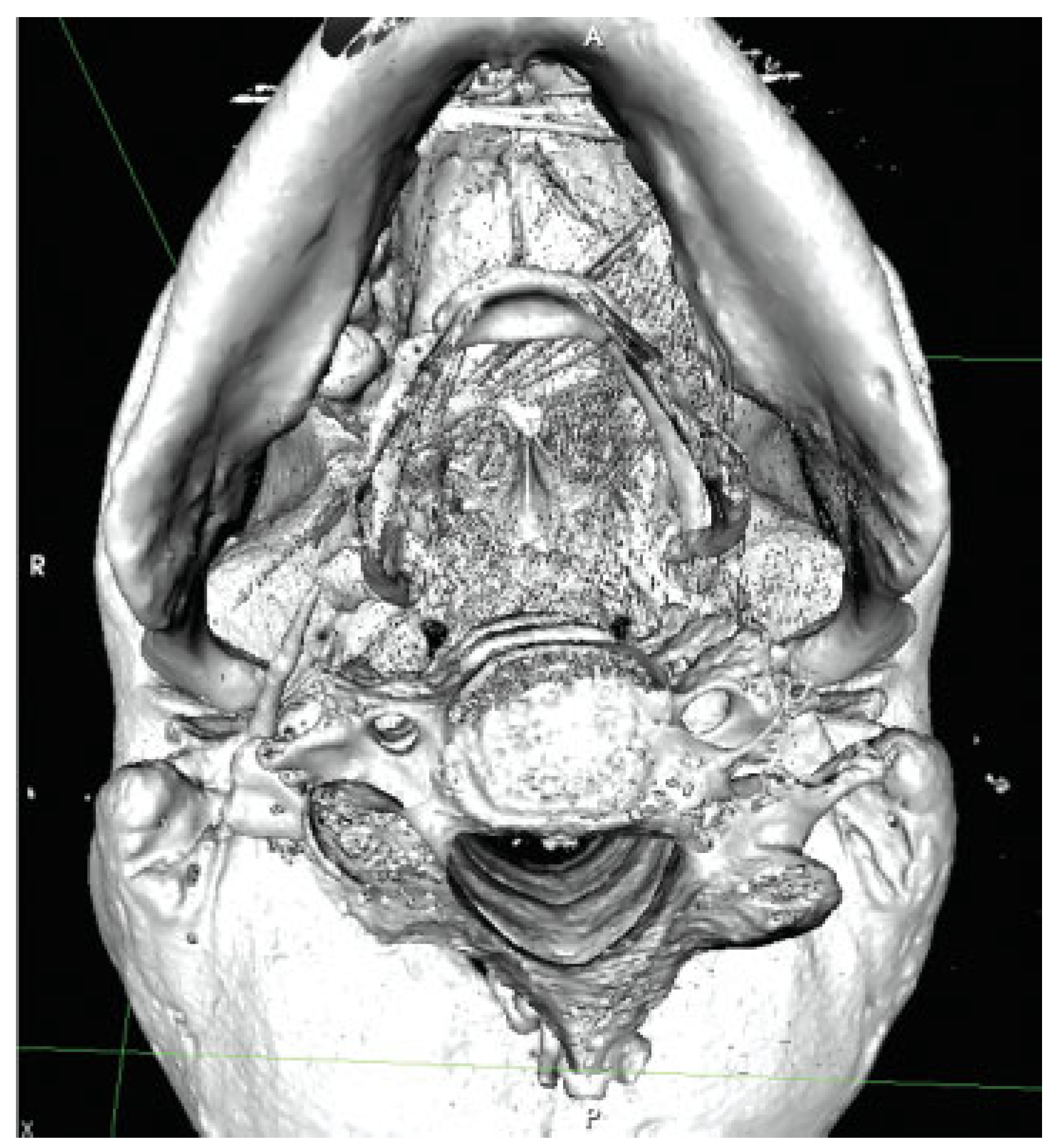
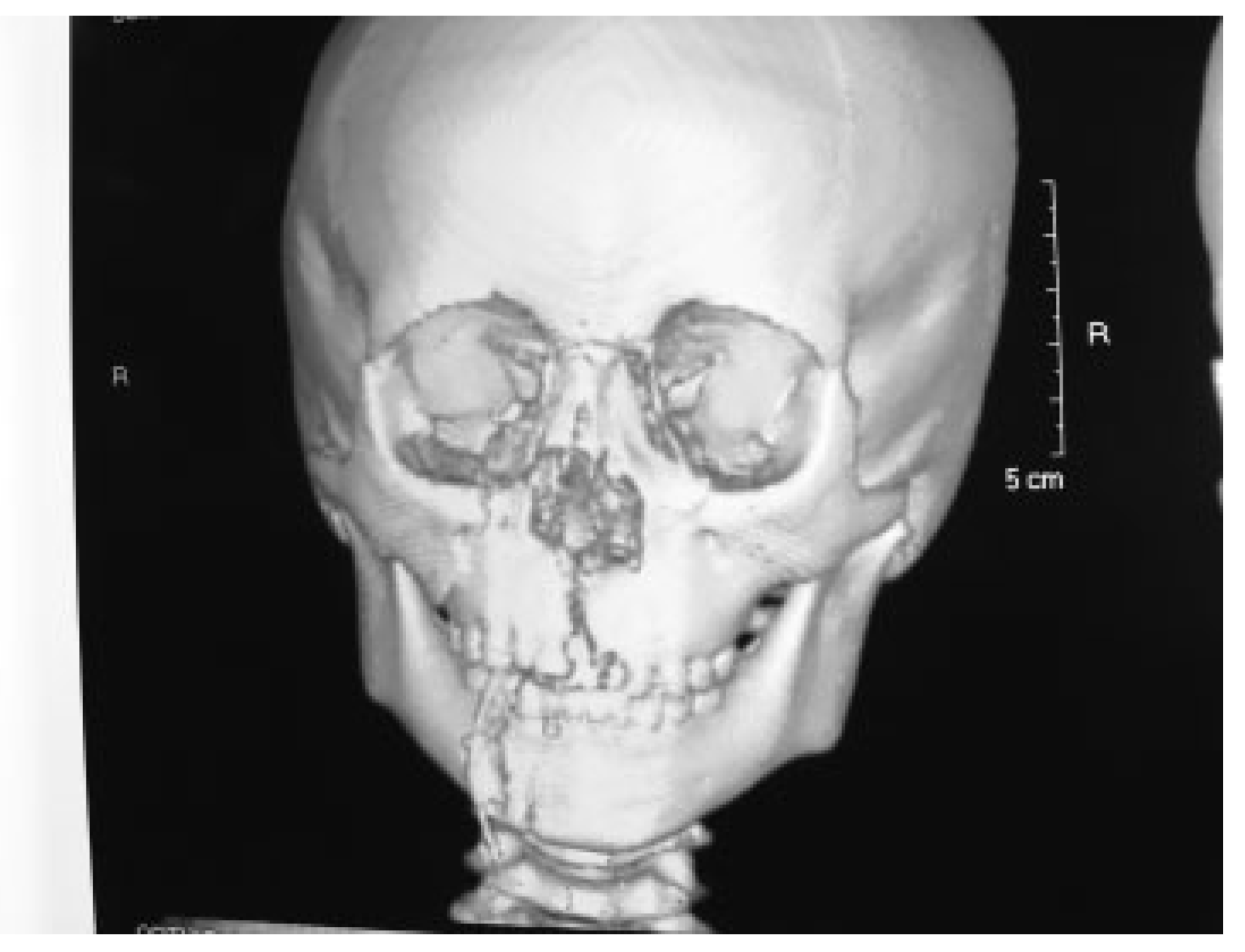
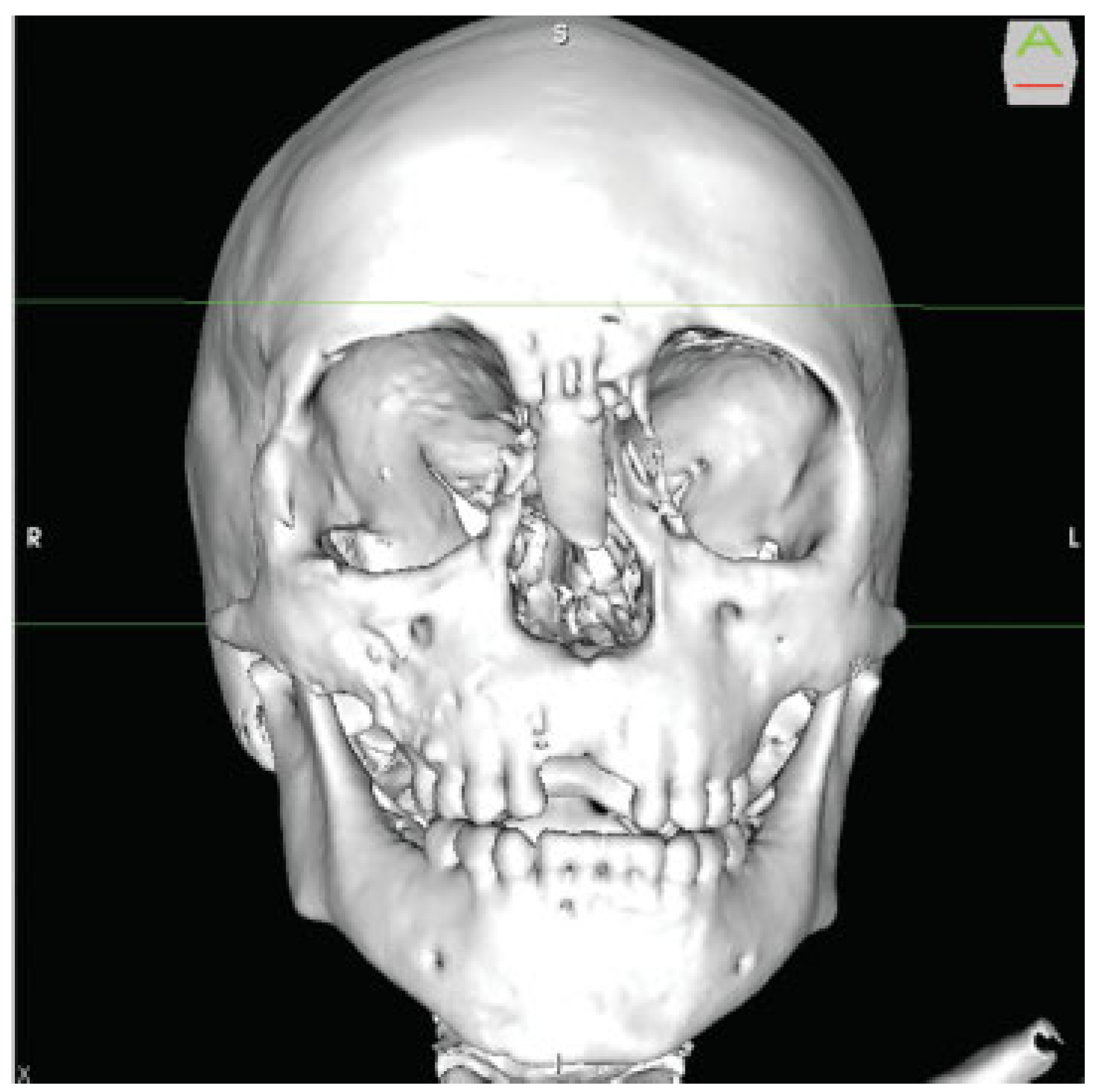
The diagnosis was made by careful clinical examination and CT scans. These were generally performed at a 1.3-mm interval between sections and were analyzed with the OsiriX (Pixmeo, Geneva, Switzerland) DICOM viewer [
7]. to assess the axial, coronal, and sagittal planes, as well as 3-D images (
Figure 8 and
Figure 9). Once the clinical and imaging diagnoses were made, a surgical plan was proposed.
Considering the associated facial fractures, the first priority of surgical treatment was the upper third of the face (‘‘up to down’’ and ‘‘out to in’’ approach). Before performing fixation of the vertical buttresses of the maxilla, dental occlusion was restored. In some cases in which it was difficult to lessen the transversal widening of the palate, transverse, 8-shaped interdental wiring at the level of the molars was used to reduce the displacement (principle of the tension band), which helped to restore the occlusion.
Once the transverse diameter of the palate was restored, a 2.0-mm high-profile locking plate, usually with six holes but in some cases with five, was placed over the palate mucosa and fixed with two screws, 2 mm in diameter and 10 mm long. Whenever possible, the screws were placed over the alveolar ridges, where bone is adequately thick and dense. Care was taken to avoid injury to the dental root during drilling or placement of the screws (
Figure 10).
Dental occlusion was reassessed by checking dental contacts; next, if there were any fractures of the medial and lateral buttresses of the maxilla or mandibular fractures, they were reduced and stabilized.
In no case was postoperative maxillomandibular fixation left in place. In patients with open palate fractures, no sutures or flaps were used to close the exposed areas. The edges of the mucosal wounds were simply approximated before placing the plate (
Figure 11,
Figure 12 and
Figure 13).
In pediatric patients, bioresorbable plates were used to repair fractures in the upper third of the face and the midface. Palatal fractures were treated in the same way and with the same implants as in adults, as well as osteosynthesis in the pyriform aperture (i.e., with 1.3-mm titanium plates and screws;
Figure 14,
Figure 15 and
Figure 16). Mandibular fractures in these patients were also treated with 2.0-mm medium-profile locking plates and titanium screws, 2 mm in diameter and 6 mm long.
Results
The average time from injury to surgery was 72 hours. All patients were clinically assessed and had a CT scan (with 1.3-mm sections) performed in the immediate postoperative period, and later on at 4, 8, 12, and 26 weeks after surgery (
Figure 17). Plates and screws for palate fixation were removed at 12 weeks, when CT scans provided evidence of fracture healing (
Figure 18). Besides removing the palatal plates, other metallic implants were also removed from the mandible and the pyriform aperture in pediatric patients at 12 weeks after surgery.
All palatal fractures healed by 12 weeks, with no cases of mucosal necrosis, bone exposure, fistulae, or infections (
Figure 19 and
Figure 20).
Discussion
Palatal fractures may be easily overlooked, especially closed fractures, where there is no injury to the mucosa. Palatal fractures are often associated with midface or panfacial fractures. Thus they should be deliberately searched for by thorough physical examination and a technically adequate CT scan with thin sections.
There is no general agreement on the best indications for osteosynthesis in the palatal vault, which has traditionally meant the placement of subperiosteal plates and screws. This technique involves the risk of bone segment necrosis, which has led some authors to define a ‘‘safe region’’ for palatal incisions [
1]. The risk of dentoalveolar necrosis may also prevent the use of the transverse vestibular approach in case of fracture of the maxillary buttresses. In some situations, use of a vertical vestibular incision over the medial and lateral maxillary buttresses has been recommended [
1].
There is also the possibility of exposure of osteosynthesis material in the mid- or long term. For all these reasons, many authors still recommend the treatment of palatal fractures by using palatal splints, arch bars or maxillomandibular fixation [
4,
6].
For the last few decades, treatment of facial fractures has sought to achieve anatomic reduction by means of stable osteosynthesis, which avoids the need for maxillomandibular fixation in the immediate postoperative period. This promotes early mobility and provides better function and favorable cosmetic appearance. Treatment of palatal fractures by maxillomandibular fixation contradicts these principles of modern treatment of facial fractures [
4,
8,
9].
The advent of low-contact locking systems for osteosynthesis has solved several technical problems. Low contact helps avoid vascular damage of the bone cortical upon which the systems are placed, whereas locking plates maintain angular stability, which prevents failure of osteosynthesis resulting from screw loosening due to the axial loads acting upon nonlocking fixation systems. Furthermore, locking systems achieve better surgical results even on poor-quality bone [
10].
In view of the above, plus the possibility to benefit from the mechanical and biological advantages of locking systems in a difficult-to-treat area, such as the palate, we decided to use 2.0-mm locking plates and screws. When used for mandibular fractures, these systems are considered an internal fixator; thus, we opted to place them over the mucosa to avoid damaging mucosal blood supply while providing adequate healing of fractures and avoiding subperiosteal dissection in the palate.
The most common types of fractures in our series of 45 consecutive patients were type II (22 patients; 48%) and III (19 patients; 42%), according to the classification by Hendrickson et al. [
1]. This was consistent with our previously published series of patients treated from 2000 through 2004 [
11]. The vast majority of fractures (42; 93%) were caused by motor vehicle accidents. All fractures seen in children and adolescents were type II, although this type of fracture was also common in adult patients.
This approach to treatment was used in adult patients and also in the pediatric group. In all age groups, fractures had healed by 12 weeks, as confirmed by CT scans. No complications such as necrosis of the bone or the mucosa, bone fistulae, or local infection occurred.
An additional positive finding in the treatment of our patients was that, in open fractures, mucosal lacerations healed uneventfully, with no mid- or long-term complications, by the placement of the plate. This shows the advantage of stabilizing not only the bone but also the soft tissues (i.e., the mucosa).
Conclusions
In summary, we consider that the use of 2.0-mm locking medium- or high-profile system an excellent option for the treatment of palatal fractures. This system, originally designed as an internal fixator for the mandible, offers mechanical and biological advantages that help provide an adequate stability to palatal fractures while preserving blood supply to the bone and mucosa, with no limitation to the use of the superior vestibular approach in patients with fractures of the maxillary buttresses. Since plates are removed after 12 weeks, they are suitable for both adults and pediatric patients. Furthermore, it is worth noting that the placement of the osteosynthesis is fast and safe.