Globe Intussusception Following Orbital Trauma: Case Series and Review of Literature
Abstract
1. Introduction
2. Method
- Population (P): Patients with traumatic globe dislocation or prolapse of the eyeball into adjacent paranasal sinuses (maxillary or ethmoid), as reported in English-language literature between 1971 and 2024.
- Intervention (I): Surgical retrieval and repositioning of the globe, with or without orbital floor and wall reconstruction.
- Comparison (C): Different surgical approaches and reconstructive techniques (direct traction, transconjunctival, transmaxillary, Caldwell–Luc, or combined methods).
- Outcome (O): Anatomical globe repositioning, structural integrity, and functional visual recovery post-intervention.
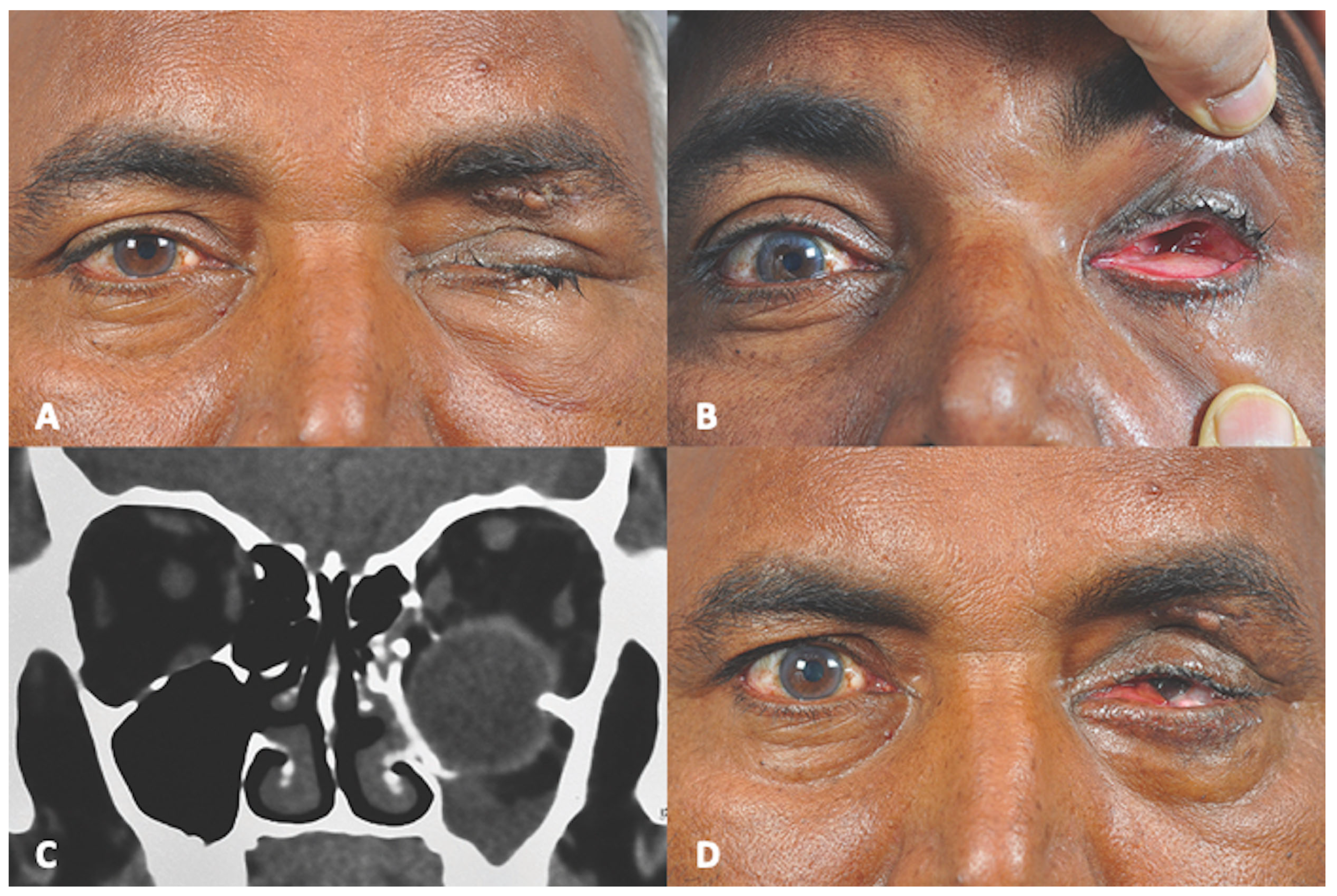
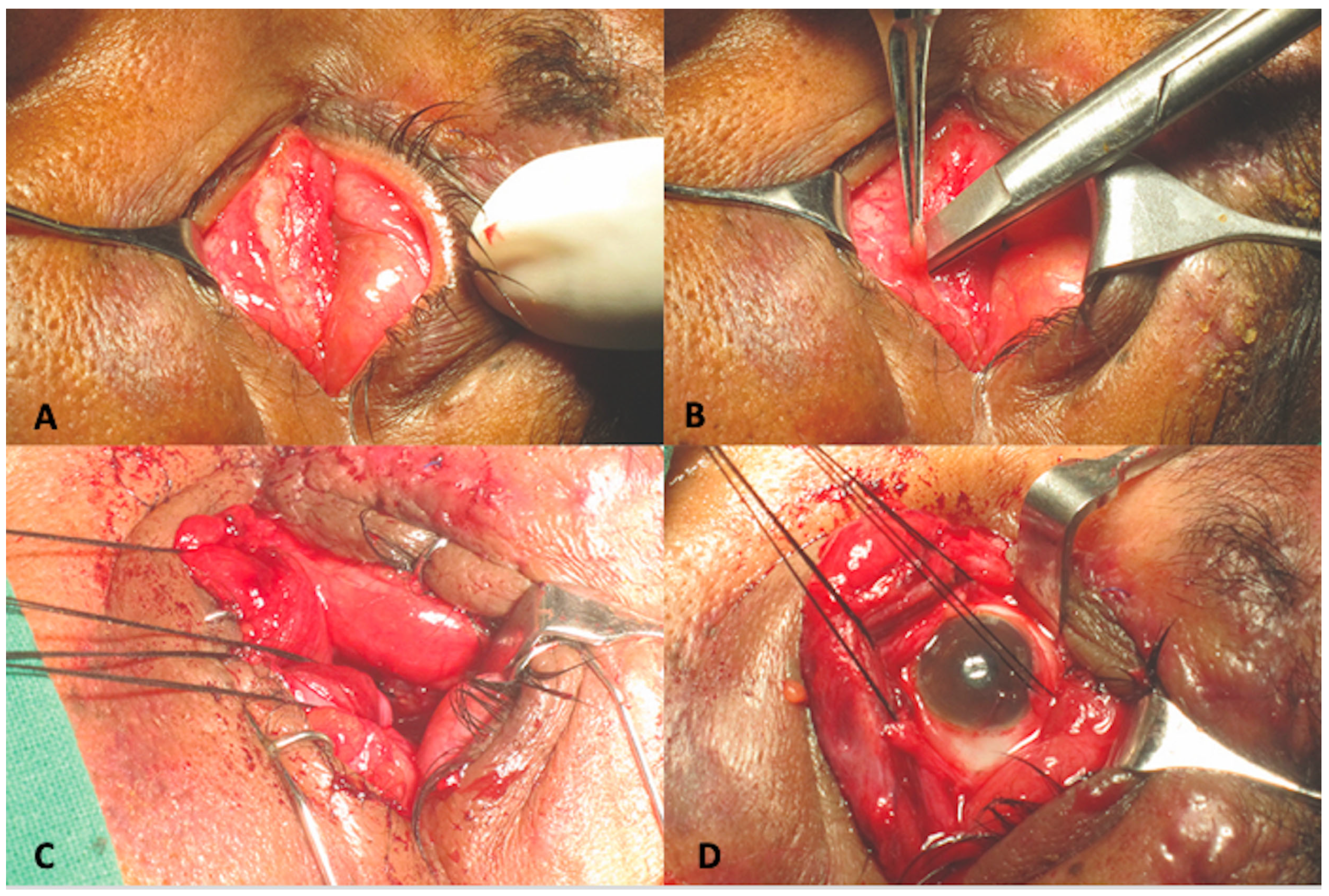
2.1. Case 1
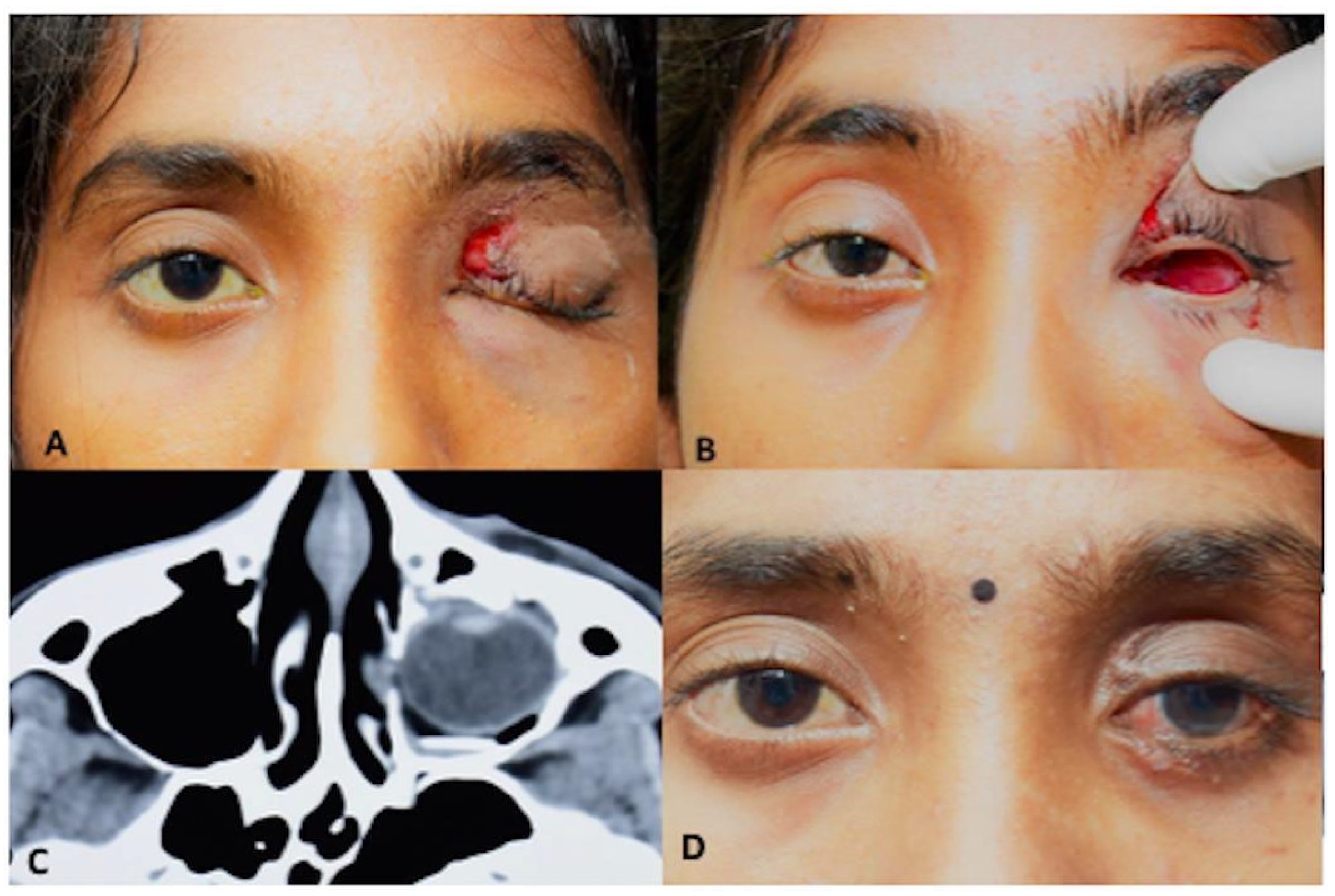
2.2. Case 2
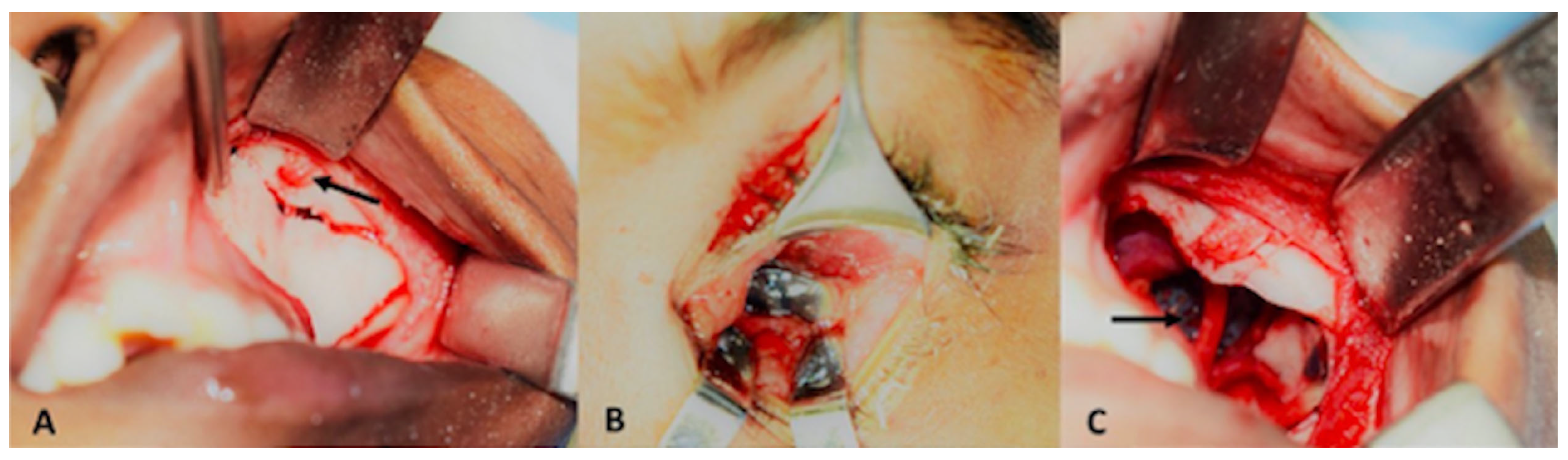
2.3. Case 3
3. Results
4. Discussion
- Population (P):
- Intervention (I):
- Comparison (C):
- Outcome (O):
- Early recognition and imaging are critical to differentiate true enucleation from concealed intussusception.
- Prompt surgical retrieval, preferably within 24 h, improves anatomical and functional outcomes.
- Choice of approach should be tailored to the type of displacement, with conjunctival intussusception warranting a full peritomy and extraocular muscle tagging.
- Urgent reconstruction with available materials (titanium, porous polyethylene, or autogenous bone) is essential to restore orbital architecture.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ATV | All-Terrain Vehicle |
| M | Male |
| F | Female |
| NA | Not Applicable |
References
- Lawrence, G.H.; Ulfelder, H. Intussusception; a review of experience at the Massachusetts General Hospital, 1937–1951. N. Engl. J. Med. 1952, 247, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Haggerty, C.J.; Roman, P. Repositioning of a traumatically displaced globe with maxillary antrostomy: Review of the literature and treatment recommendations. J. Oral. Maxillofac. Surg. 2013, 71, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Baek, S. Traumatic dislocation of the globe into the maxillary sinus associated with extraocular muscle injury. Graefes Arch. Clin. Exp. Ophthalmol. 2005, 243, 1280–1283. [Google Scholar] [CrossRef] [PubMed]
- Heilbig, H.; Iseli, H.P. Traumatic rupture of the globe cause by cow horns. Eur. J. Ophthalmol. 2002, 12, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.I.; Thomas, R.; Alexander, T.A. An Unusual case of bull gore injury. Aust. N. Z. J. Ophthalmol. 1986, 14, 377–379. [Google Scholar] [CrossRef]
- Emery, J.M.; Noorden, G.K.; Sclernitzauer, D.A. Orbital floor fractures: Long-term followup of cases with and without surgical repair. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1971, 75, 802–812. [Google Scholar]
- Stasior, O.G. The Wendell L: Hughes lecture. Complications of ophthalmic plastic surgery and their prevention. Trans. Sect. Ophthalmol. Am. Acad. Ophthalmol. Otolaryngol. 1976, 81, 543–552. [Google Scholar]
- Berkowitz, R.A.; Putterman, A.M.; Patel, D.B. Prolapse of the globe into the maxillary sinus after orbital floor fracture. Am. J. Ophthalmol. 1982, 91, 253–257. [Google Scholar] [CrossRef]
- Risco, J.M.; Stratas, B.A.; Knott, R.H. Prolapse of the globe into the ethmoid sinus. Am. J. Ophthalmol. 1984, 97, 659–660. [Google Scholar] [CrossRef]
- Smit, T.I.; Koorneeff, L.; Zonneveld, F.W. A total orbital floor fracture with prolapse of the globe into the maxillary sinus manifesting as post enucleation socket syndrome. Am. J. Ophthalmol. 1990, 110, 569–570. [Google Scholar] [CrossRef]
- Ziccardi, V.B.; Patterson, G.T.; Ramasastry, S.; Sotereanos, G.C. Management of a severe zygomatico-orbital fracture with dislocation of the globe into the antrum. J. Craniofac. Surg. 1993, 4, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Moon, M.; Pietris, G.; Shapter, M. Dislocation of the globe into the ethmoid sinuses. Aust. N. Z. J. Ophthalmol. 1997, 25, 175–176. [Google Scholar] [CrossRef]
- Pelton, R.W.; Rainey, A.M.; Lee, A.G. Traumatic subluxation of the globe into the maxillary sinus. AJNR Am. J. Neuroradiol. 1998, 19, 1450–1451. [Google Scholar] [PubMed]
- Tung, T.C.; Chen, Y.R.; Santamaria, E.; Chen, C.T.; Lin, C.J.; Tsai, T.R. Dislocation of anatomic structures into the maxillary sinus after craniofacial trauma. Plast. Reconstr. Surg. 1998, 101, 1904–1908. [Google Scholar] [CrossRef] [PubMed]
- Saleh, T.; Leatherbarrow, B. Traumatic prolapse of the globe into the maxillary sinus diagnosed as traumatic enucleation of the globe. Eye 1999, 13, 678–680. [Google Scholar] [CrossRef]
- Tranfa, F.; Di Matteo, G.; Di Salle, F.; Strianese, D.; Bonavolontà, G. Traumatic displacement of the globe into the ethmoid sinus. Am. J. Ophthalmol. 2000, 130, 253–254. [Google Scholar] [CrossRef]
- Okabe, H.; Kimura, K.; Sonoda, S.; Sakamoto, T. Displacement of globe into ethmoid sinus by orbital medial wall fracture with good recovery of vision. Jpn. J. Ophthalmol. 2005, 49, 426–428. [Google Scholar] [CrossRef]
- Müller-Richter, U.D.; Kohlhof, J.K.; Driemel, O.; Wagener, H.; Reichert, T.E. Traumatic dislocation of the globe into the maxillary sinus. Int. J. Oral. Maxillofac. Surg. 2007, 36, 1207–1210. [Google Scholar] [CrossRef]
- Abrishami, M.; Aletaha, M.; Bagheri, A.; Salour, S.H.; Yazdani, S. Traumatic subluxation of the globe into the maxillary sinus. Ophthal Plast. Reconstr. Surg. 2007, 23, 156–158. [Google Scholar] [CrossRef]
- Kreiner, B.; Amer, R.; Sharfi, G.; Solomon, A.; Ilsar, M. Traumatic displacement of the globe into the paranasal sinuses: Case report and guidelines for treatment. J. Oral. Maxillofac. Surg. 2008, 66, 826–830. [Google Scholar] [CrossRef]
- Ramstead, C.; McCabe, J.; Alkahtani, M.; Leong-Sit, J.; Morhart, M. Traumatic dislocation of the globe into the maxillary sinus. Can. J. Ophthalmol. 2008, 43, 364–366. [Google Scholar] [CrossRef]
- Jellab, B.; Baha, A.T.; Moutaouakil, A.; Khoumiri, R.; Raji, A.; Ghannane, H.; Amkaoui, M.A.; Ait Benali, S. Management of a severe cranio-orbito-facial trauma with a dislocation of the globe into the maxillary sinus. Bull. Soc. Belge Ophtalmol. 2008, 309–310, 37–41. [Google Scholar]
- Akhaddar, A.; Elmostarchid, B.; Boucetta, M. Images in emergency medicine. Traumatic intraorbital stone with globe displacement into the maxillary sinus. Emerg. Med. J. 2010, 27, 828. [Google Scholar] [CrossRef]
- Gulati, A.; Gupta, B.; Singh, I. An unusual orbital blow-out fracture: A case report. Orbit 2011, 30, 10–12. [Google Scholar] [CrossRef]
- Zhang-Nunes, S.X.; Jarullazada, I.; Mancini, R. Late central visual recovery after traumatic globe displacement into the maxillary sinus. Ophthal. Plast. Reconstr. Surg. 2012, 28, 17–19. [Google Scholar] [CrossRef]
- Xu, B.; Xu, X.L.; Yan, J. Treatment of traumatic globe dislocated completely into the maxillary sinus. Int. J. Ophthalmol. 2013, 6, 106–107. [Google Scholar] [CrossRef]
- Amaral, M.B.; Nery, A.C. Traumatic globe dislocation into the paranasal sinuses: Literature review and treatment guidelines. J. Craniomaxillofac. Surg. 2016, 44, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.M.; Fries, F.B.; Hendrix, P.; Brinker, T.; Loukas, M.; Tubbs, R.S. Orbital Blowout Fracture with Complete Dislocation of the Globe into the Maxillary Sinus. Cureus 2017, 9, 1728. [Google Scholar] [CrossRef] [PubMed]
- Noman, S.A.; Shindy, M.I. Immediate surgical management of traumatic dislocation of the eye globe into the maxillary sinus: Report of a rare case and literature review. Craniomaxillofacial Trauma Reconstr. 2017, 10, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.S.; Noronha, O.V.; Mukherjee, B. Timing of surgery in traumatic globe dislocation. Indian J. Ophthalmol. 2017, 65, 767–770. [Google Scholar] [CrossRef]
- Bastos, R.M.; Taparello, C.; Tres, R.; Sawazaki, R. Orbital blowout fracture with globe displacement into the maxillary sinus: A case report and literature review. J. Oral. Maxillofac. Surg. 2021, 79, 204.e1-204.e12. [Google Scholar] [CrossRef] [PubMed]
- Onaran, Z.; Şimşek, G.; Konuk, O. Traumatic dislocation of the globe into the ethmoid sinus. Turk. J. Ophthalmol. 2021, 51, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Gobeaut, M.; Merle, H.; Rocher, M.; Robert, P.Y.; Beral, L. Traumatic incarceration of the globe into the maxillary sinus: A case report. J. Fr. Ophtalmol. 2022, 45, e33–e35. [Google Scholar] [CrossRef] [PubMed]
- Steel, D.A.; Mortimer, T.; Bater, M.C. Severe orbital blow-out fracture: Complete displacement of the globe into the maxillary sinus. BMJ Case Rep. 2023, 16, e254055. [Google Scholar] [CrossRef]
- Vergez, P.; Vernhet, E.; Daien, V.; De Boutray, M. Traumatic dislocation of the globe into the maxillary sinus with early recovery of visual acuity: Case report and review of the literature on management. J. Fr. Ophtalmol. 2024, 47, 104078. [Google Scholar] [CrossRef]
- Bergeron, L.; Bonapace-Potvin, M.; Bergeron, F. Printing in Time for Cranio-Maxillo-Facial Trauma Surgery: Key Parameters to Factor in. Craniomaxillofac. Trauma Reconstr. 2023, 16, 121–129. [Google Scholar] [CrossRef]
- Burger, T.; Fan, K.; Brokmeier, J.; Thieringer, F.M.; Berg, B.I. Orbital Floor Fractures: Treatment and Diagnostics—A Survey Among Swiss, German and Austrian Maxillofacial Units. Craniomaxillofac. Trauma Reconstr. 2024, 17, NP60–NP67. [Google Scholar] [CrossRef]


| Sr No. | Authors | Age | Sex | Etiology of Trauma | Involvement of Sinus | Time to Presentation | Globe Repositioning | Orbital Reconstruction | Visual Acuity |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Emery et al., 1971 [6] | NA | NA | NA | Maxillary Sinus | NA | Direct traction | NA | NA |
| 2 | Emery et al., 1971 [6] | NA | NA | NA | Maxillary Sinus | Same day | Direct traction | NA | NA |
| 3 | Stasior, 1976 [7] | NA | M | Fire hose nozzle injury | Right Maxillary Sinus | NA | Trans-maxillary manual repositioning | No | Recovery 20/60 |
| 4 | Berkowitz et al., 1981 [8] | 24 | F | Punch with fist | Left Maxillary Sinus | Same day | Trans-maxillary manual repositioning | Silicone implant | Recovery 20/20 |
| 5 | Risco et al., 1984 [9] | 40 | M | Blunt trauma (hit with a wood block) | Left ethmoid sinus | 5 days | Direct traction- trans-nasal repositioning | No | Light perception: recurrence of globe displacement |
| 6 | Singh et al., 1986 [5] | 32 | M | Bull horn | NA | Direct traction | No | 6/36 | |
| 7 | Smit et al., 1990 [10] | 21 | F | Windshield injury | Right Maxillary Sinus | 5 years | NA | Teflon plate | No |
| 8 | Ziccardi et al., 1993 [11] | 25 | M | Traffic accident | Left Maxillary Sinus | Same day | Sub-ciliary + Trans-maxillary | Autologous bone | 20/50 |
| 9 | Moon et al., 1997 [12] | 40 | M | Blunt instrument injury | Right Ethmoid Sinus | 2 days | Direct Traction | No | No |
| 10 | Pelton et al., 1998 [13] | 19 | M | Traffic accident | Left Maxillary Sinus | Same day | Trans-maxillary manual repositioning | NA | NA |
| 11 | Tung et al., 1998 [14] | 17 | M | Traffic accident | Right Maxillary Sinus | - | Direct repositioning-sub-ciliary approach | Autogenous bone graft | No |
| 12 | Saleh & Leatherbarrow, 1999 [15] | 29 | M | Blunt trauma | Left Maxillary Sinus | 2 Months | Enucleation | No | No |
| 13 | Tranfa et al., 2000 [16] | 58 | M | Fall of a tree branch | Left Ethmoid Sinus | Same day | Direct Traction | No | Recovery 20/100 |
| 14 | Kim and Baek, 2005 [3] | 68 | M | Traffic accident | Right Maxillary Sinus | Same day | Direct traction- transconjunctival | Porous polyethylene | No |
| 15 | Okabe et al., 2005 [17] | 37 | M | Injury with a piece of wood | Left Ethmoid Sinus | Same day | Direct Traction | No reconstruction of medial orbital wall | Recovery 20/15 restricted motility |
| 16 | Müller-Richter et al., 2007 [18] | 62 | M | Blunt trauma by machine | Right Maxillary Sinus | Same day | Trans-maxillary manual repositioning | Balloon catheter left inside the sinus | Recovery 20/20 |
| 17 | Abrishami et al., 2007 [19] | 18 | M | Traffic accident | Right Maxillary Sinus | 7 days | Direct repositioning sub-ciliary approach | Porous polyethylene | No |
| 18 | Kreiner et al., 2008 [20] | 50 | M | Wall collapse injury | Left Maxillary Sinus | Same day | Direct traction | Silicone sheet | No |
| 19 | Ramstead et al., 2008 [21] | 32 | M | Stepped by a bull | Left Maxillary Sinus | Same day | NA | Titanium mesh | Recovery 20/200 |
| 20 | Jellab et al., 2008 [22] | 24 | M | Traffic accident | Left Maxillary Sinus | Same day | NA | Autogenous bone | Light perception |
| 21 | Jellab et al., 2008 [22] | 50 | F | Traffic accident | Left Maxillary Sinus | Same day | No repositioning | No | NA |
| 22 | Akhaddar et al., 2010 [23] | 62 | M | Traffic accident | Right Maxillary Sinus | NA | NA | NA | NA |
| 23 | Gulati et al., 2011 [24] | 10 | M | Bicycle accident | Right Maxillary Sinus | NA | Trans-maxillary | Balloon Catheter inside sinus | Recovered 6/16 |
| 24 | Zhang-Nunes et al., 2012 [25] | 20 | M | Traffic accident | Right Maxillary Sinus | Same day | NA | Sialistic sheet | Recovery 20/25 |
| 25 | Xu et al., 2013 [26] | 46 | F | Traffic accident | Right Maxillary Sinus | NA | Direct reposition | Titanium mesh | Light perception |
| 26 | Haggerty and Roman, 2013 [2] | 35 | M | Traffic accident | Left Maxillary Sinus | Same day | Trans-maxillary manual repositioning | Titanium mesh | Light perception |
| 27 | Amaral and Nery, 2015 [27] | 44 | M | Struck by gym weight | Left Maxillary Sinus | 4 days | Trans-maxillary manual repositioning | Titanium mesh | Recovery 20/50 |
| 28 | Wang JM et al., 2017 [28] | 15 | M | Accident riding ATV | Left Maxillary Sinus | NA | NA | Titanium mesh | No |
| 29 | Noman SA and Shindy MI, 2017 [29] | 24 | F | Blunt wooden object | Right Maxillary Sinus | Same day | Trans-maxillary approach | Titanium Mesh | Recover 20/40 |
| 30 | Alam et al., 2017 [30] | 45 | F | Trauma with door | Right Maxillary Sinus | 3 days | Direct repositioning | Titanium mesh | VA: counting fingers to 1 m |
| 31 | Bastos et al., 2021 [31] | 27 | M | Punch in the eye | Right Maxillary Sinus | Same day | Trans-maxillary approach | 14 days after repositioning of globe, reconstruction with titanium | No VA |
| 32 | Onaran et al., 2021 [32] | 36 | F | Blunt trauma on door handle | Left Ethmoid Sinus | Same day | Gentle intranasal digital manipulation | 4 months after repositioning, with porous polyethylene implant | VA 20/20 |
| 33 | Gobeaut et al., 2022 [33] | 54 | F | Fall from height | Right Maxillary Sinus | 1 day | Direct traction and trans-maxillary approach | Resorbable polydiaxone osteosynthesis implant (PDS) | VA 20/125 |
| 34 | Steel DA et al., 2023 [34] | - | M | Traffic Accident | Left Maxillary Sinus | Same day | Trans-maxillary | Titanium mesh | No perception of light |
| 35 | Vergez P et al., 2024 [35] | 67 | M | Fall from a height | Left Maxillary Sinus | Same day | Direct Traction | Titanium mesh | 20/50 |
| Total Number | Age Range | Gender | Etiology of Trauma | Involvement of Sinus | Time to Presentation | Globe Repositioning | Orbital Reconstruction | Visual Acuity |
|---|---|---|---|---|---|---|---|---|
| 35 | 10–68 Years | Male: 25 Female: 8 Not mentioned: 2 | Traffic accident: 14 Others: 9 NA: 2 | Maxillary Sinus: 30 Ethmoid Sinus: 5 | Range: Same day to 5 years | Direct reposition: 15 Transmaxillary: 12 NA: 6 No reposition: 1 Enucleation: 1 | Titanium: 9 Silicone: 3 Porous poly-ethylene: 3 PDS: 1 Bone: 3 No reconstruction: 9 Others: 3, NA: 4 | Functional Vision improved: 15 Finger counting 1 m: 1 Light perception: 4 Not improved: 10 NA: 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desai, A.; Dendukuri, G.; Naik, M. Globe Intussusception Following Orbital Trauma: Case Series and Review of Literature. Craniomaxillofac. Trauma Reconstr. 2025, 18, 44. https://doi.org/10.3390/cmtr18040044
Desai A, Dendukuri G, Naik M. Globe Intussusception Following Orbital Trauma: Case Series and Review of Literature. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(4):44. https://doi.org/10.3390/cmtr18040044
Chicago/Turabian StyleDesai, Akruti, Gautam Dendukuri, and Milind Naik. 2025. "Globe Intussusception Following Orbital Trauma: Case Series and Review of Literature" Craniomaxillofacial Trauma & Reconstruction 18, no. 4: 44. https://doi.org/10.3390/cmtr18040044
APA StyleDesai, A., Dendukuri, G., & Naik, M. (2025). Globe Intussusception Following Orbital Trauma: Case Series and Review of Literature. Craniomaxillofacial Trauma & Reconstruction, 18(4), 44. https://doi.org/10.3390/cmtr18040044





