Optimizing Maxillomandibular Position in Orthognathic Surgery: Introducing the T Concept in Treatment Planning
Abstract
1. Introduction
2. The T Concept
3. The Chin Rationale
4. Step-by-Step Planning
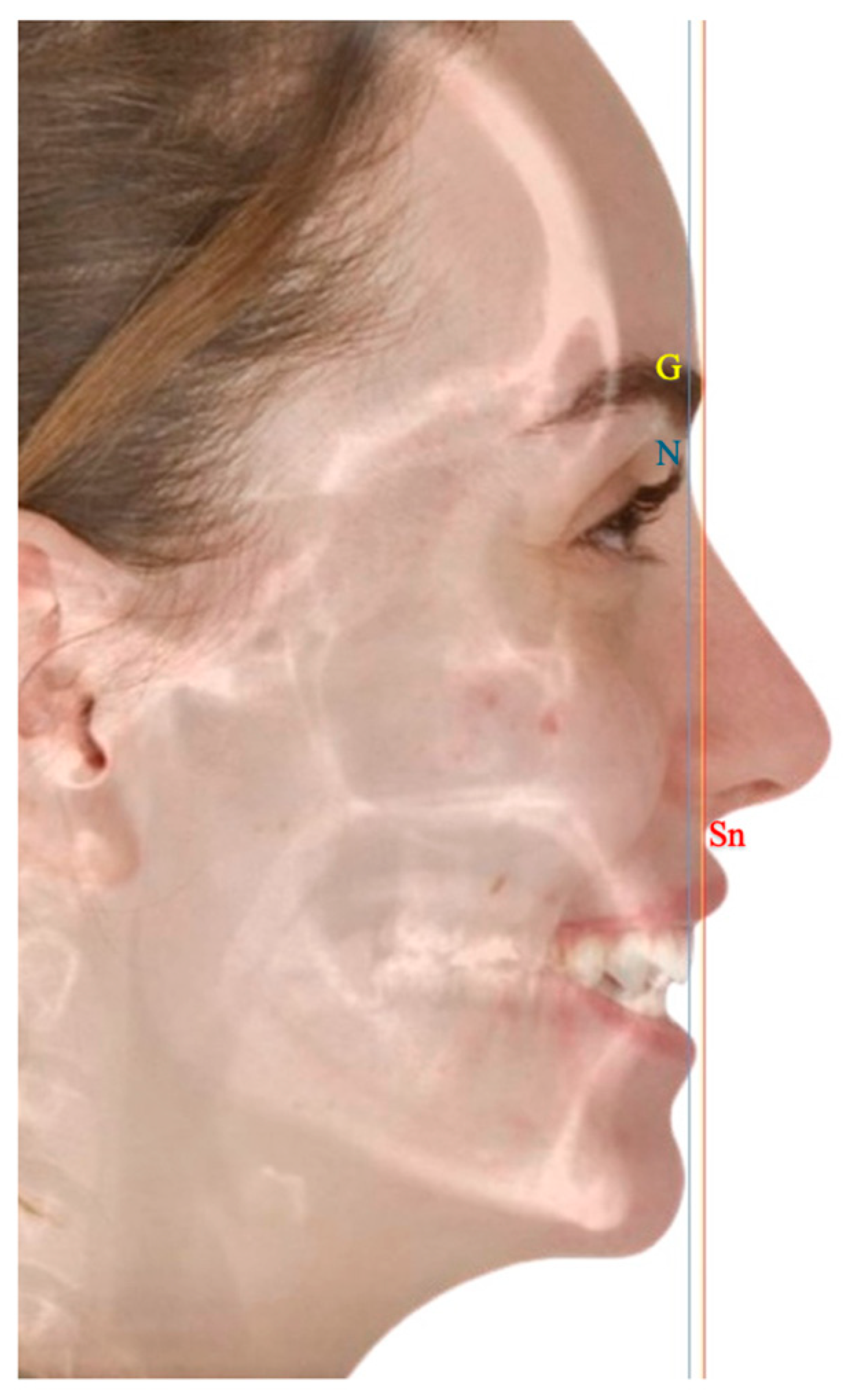
4.1. Phase-One
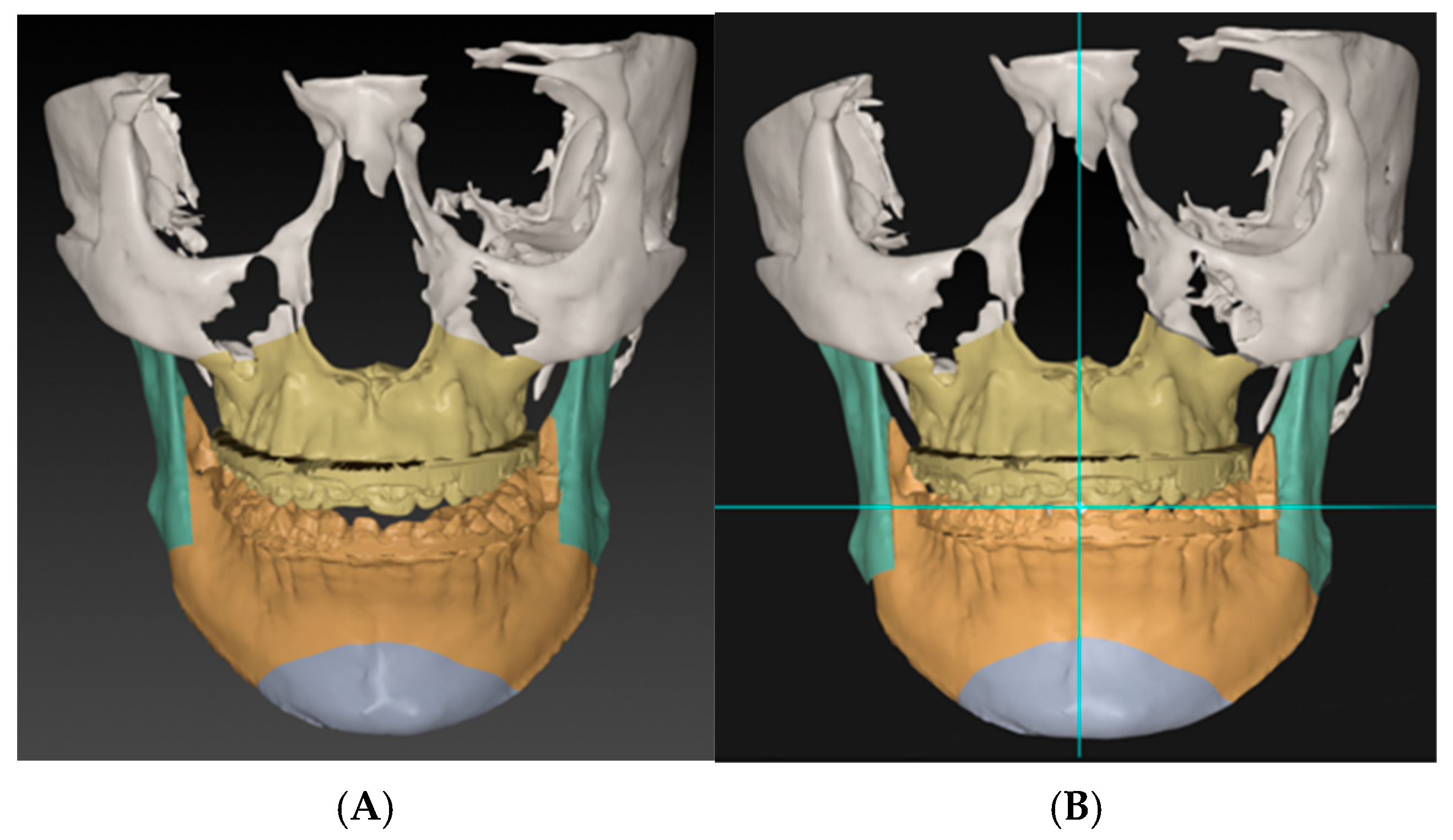
4.2. Phase-Two
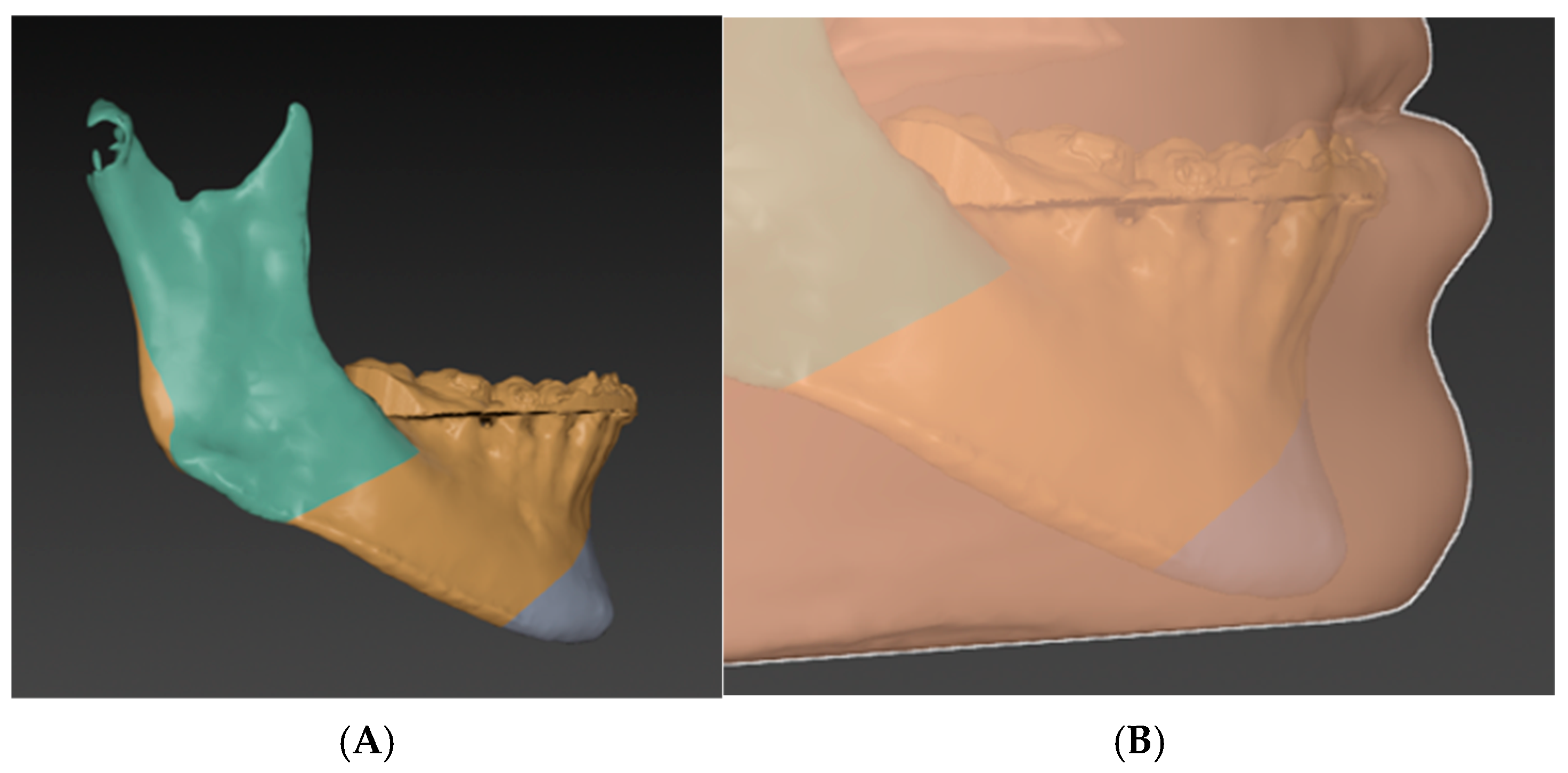
4.3. Phase-Three
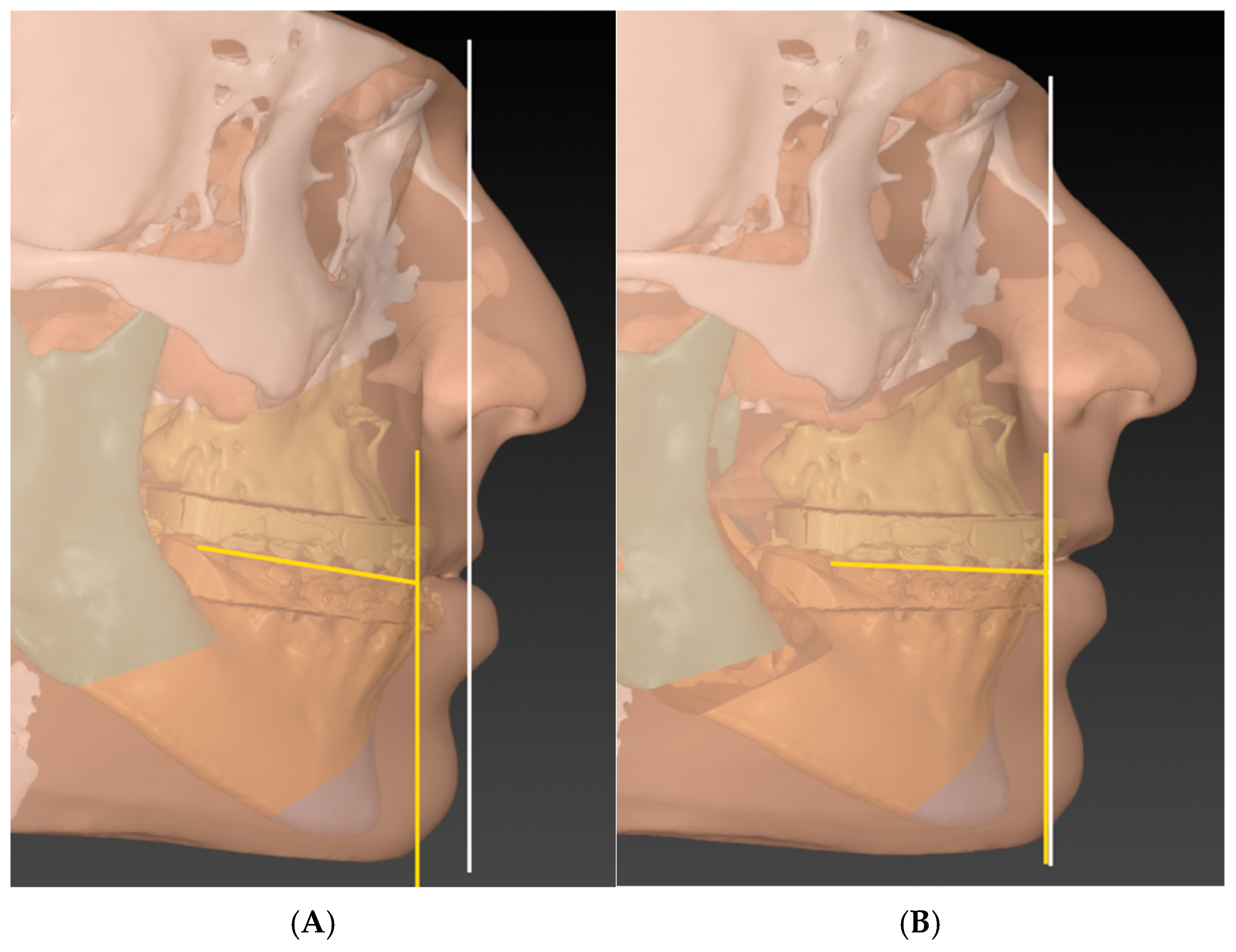
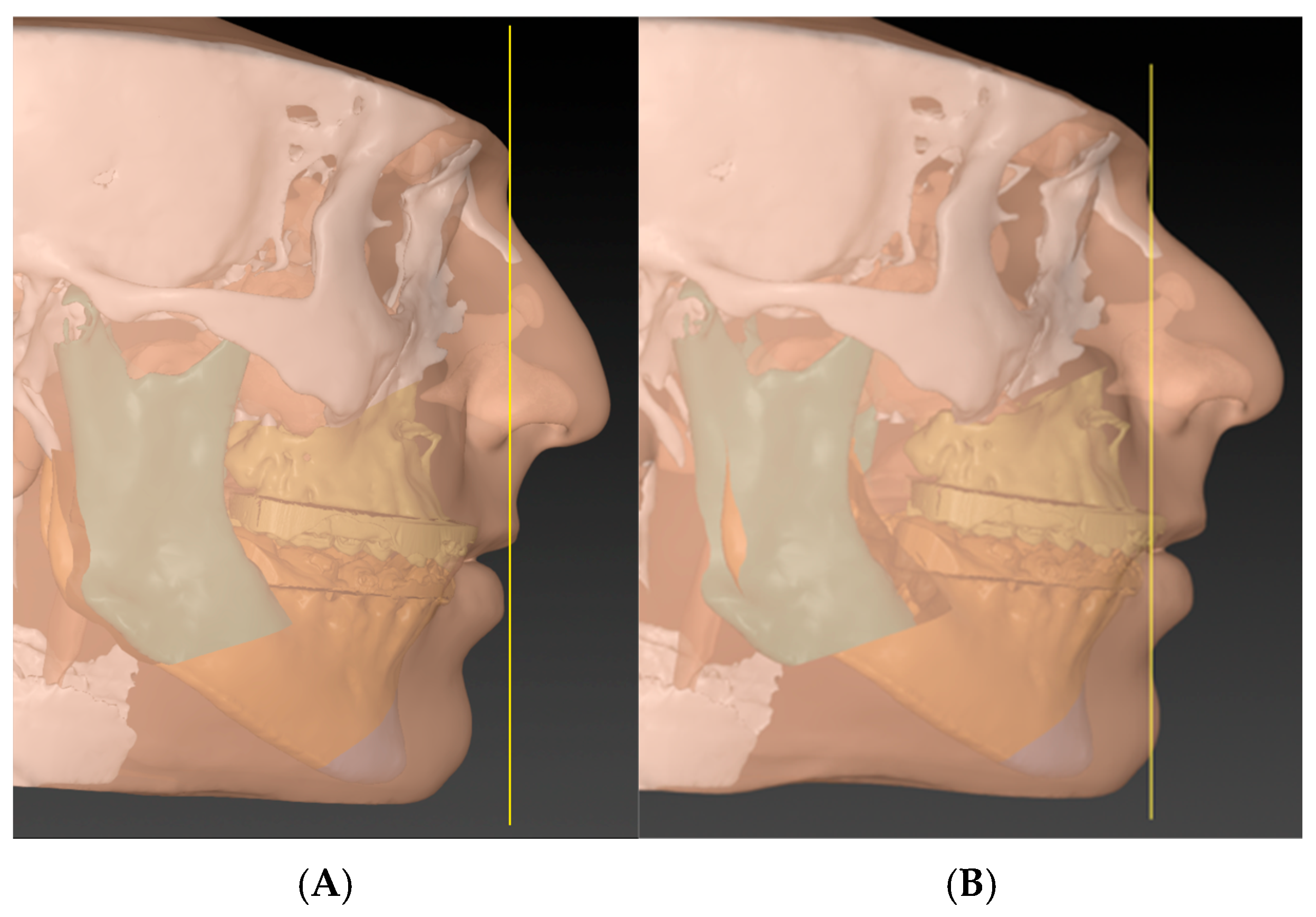
4.4. Phase-Four (T Concept)
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MMC | Maxillomandibular complex |
| GALL | Goal Anterior Limit Line |
| OP-MP Angle | Occlusal Plane–Mandibular Plane angle |
References
- Posnick, J.C. Orthognathic Surgery Principles and Practice, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2022; pp. 61–66. ISBN 978-0-323-79183-0. [Google Scholar]
- Hernández-Alfaro, F.; Valls Ontañón, A. Orthofacial Surgery: Aesthetic & Functional Surgery of the Facial Skeleton and Mask, 1st ed.; Springer Nature: Cham, Switzerland, 2024; pp. 1–4. ISBN 978-3-031-76185-0. [Google Scholar]
- Proffit, W.R.; White, R.P.; Sarver, D.M. Contemporary Treatment of Dentofacial Deformity; Mosby: Philadelphia, MO, USA, 2003; ISBN 978-0-323-01697-1. [Google Scholar]
- Kotuła, J.; Kuc, A.E.; Lis, J.; Kawala, B.; Sarul, M. New Sagittal and Vertical Cephalometric Analysis Methods: A Systematic Review. Diagnostics 2022, 12, 1723. [Google Scholar] [CrossRef]
- Hernández-Alfaro, F.; Vivas-Castillo, J.; Belle de Oliveira, R.; Hass-Junior, O.; Giralt-Hernando, M.; Valls-Ontañón, A. Barcelona Line. A Multicentre Validation Study of a Facial Projection Reference in Orthognathic Surgery. Br. J. Oral Maxillofac. Surg. 2022, 6, 3–11. [Google Scholar] [CrossRef]
- Baik, C.Y.; Ververidou, M. A New Approach of Assessing Sagittal Discrepancies: The Beta Angle. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 100–105. [Google Scholar] [CrossRef]
- Jacobson, A. The “Wits” Appraisal of Jaw Disharmony. Am. J. Orthod. 1975, 67, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, R.M. Cephalometric Analysis and Synthesis. Angle Orthod. 1961, 31, 141–156. [Google Scholar]
- Riedel, R.A. The Relation of Maxillary Structures to Cranium in Malocclusion and in Normal Occlusion. Angle Orthod. 1952, 22, 142–145. [Google Scholar]
- Ackerman, J.L.; Proffit, W.R.; Sarver, D.M. The Emerging Soft Tissue Paradigm in Orthodontic Diagnosis and Treatment Planning. Clin. Orthod. Res. 1999, 2, 49–52. [Google Scholar] [CrossRef]
- Arnett, G.W.; Jelic, J.S.; Kim, J.; Cummings, D.R.; Beress, A.; Worley, C.M.; Chung, B.; Bergman, R. Soft Tissue Cephalometric Analysis: Diagnosis and Treatment Planning of Dentofacial Deformity. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 239–253. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.T.; Waschak, J.; Borzabadi-Farahani, A.; Murphy, N.C. Longitudinal Study of Cephalometric Soft Tissue Profile Traits between the Ages of 6 and 18 Years. Angle Orthod. 2014, 84, 48–55. [Google Scholar] [CrossRef]
- Swennen, G.R.J.; Mollemans, W.; Schutyser, F. Three-Dimensional Treatment Planning of Orthognathic Surgery in the Era of Virtual Imaging. J. Oral Maxillofac. Surg. 2009, 67, 2080–2092. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.B.; Goldstein, J.A.; Seruya, M. Outcomes in Computer-Assisted Surgical Simulation for Orthognathic Surgery. J. Craniofacial Surg. 2012, 23, 509–513. [Google Scholar] [CrossRef]
- Quast, A.; Santander, P.; Witt, D.; Damm, A.; Moser, N.; Schliephake, H.; Meyer-Marcotty, P. Traditional Face-Bow Transfer versus Three-Dimensional Virtual Reconstruction in Orthognathic Surgery. Int. J. Oral Maxillofac. Surg. 2019, 48, 347–354. [Google Scholar] [CrossRef]
- Farrell, B.B.; Franco, P.B.; Tucker, M.R. Virtual Surgical Planning in Orthognathic Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 459–473. [Google Scholar] [CrossRef]
- Ho, C.-T.; Lin, H.-H.; Liou, E.J.W.; Lo, L.-J. Three-Dimensional Surgical Simulation Improves the Planning for Correction of Facial Prognathism and Asymmetry: A Qualitative and Quantitative Study. Sci. Rep. 2017, 7, 40423. [Google Scholar] [CrossRef] [PubMed]
- Melhem-Elias, F.; Reis, B.A.Q.; Afonso, F.A.C.; Barretto, M.D.A.; Deboni, M.C.Z. An Innovative Universal Protocol for Orthognathic Surgery Three-Dimensional Virtual Simulation. Int. J. Oral Maxillofac. Surg. 2023, 52, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.-Y.; Lin, H.-H.; Lo, L.-J.; Ho, C.-T. Postoperative Outcomes of Two- and Three-Dimensional Planning in Orthognathic Surgery: A Comparative Study. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 1101–1111. [Google Scholar] [CrossRef]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of Virtual Planning in Orthognathic Surgery: A Systematic Review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Arnett, G.W.; Bergman, R.T. Facial Keys to Orthodontic Diagnosis and Treatment Planning—Part II. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 395–411. [Google Scholar] [CrossRef]
- Hernandez-Alfaro, F. Upper Incisor to Soft Tissue Plane (UI-STP): A New Reference for Diagnosis and Planning in Dentofacial Deformities. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e779–e781. [Google Scholar] [CrossRef]
- Klein, K.P.; Kaban, L.B.; Masoud, M.I. Orthognathic Surgery and Orthodontics Inadequate Planning Leading to Complications or Unfavorable Results. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 71–82. [Google Scholar] [CrossRef]
- Swennen, G. (Ed.) 3D Virtual Treatment Planning of Orthognathic Surgery: A Step-by-Step Approach for Orthodontists and Surgeons, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2017; ISBN 978-3-662-47388-7. [Google Scholar]
- Andrews, L.F.; Andrews, W.A. The Six Elements of Orofacial Harmony. Andrews J. Orthodotinc Orofac. Harmon. 2000, 1, 13–22. [Google Scholar]
- Da-Silva, H.F.; Marinho, L.F.; Souza, G.A.; Sverzut, A.T.; Olate, S.; Asprino, L.; de-Moraes, M. About Chin (Genioplasty) Surgery. Int. J. Morphol. 2020, 38, 1120–1127. [Google Scholar] [CrossRef]
- George, J.A.; Kannan, A.; Kailasam, V. Long-Term Hard and Soft Tissue Response Following Isolated Genioplasty: A Systematic Review. Oral Maxillofac. Surg. 2022, 26, 195–203. [Google Scholar] [CrossRef]
- Ramanathan, M.; Panneerselvam, E.; Parameswaran, A.; Kanno, T. Genioplasty in Contemporary Orthognathic Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2023, 35, 97–114. [Google Scholar] [CrossRef]
- Dalmeijer, S.W.R.; Riet, T.C.T.V.; Ho, J.-P.T.F.; Becking, E. Evaluating Genioplasty Procedures: A Systematic Review and Roadmap for Future Investigations. Craniomaxillofacial Trauma Reconstr. 2025, 18, 5. [Google Scholar] [CrossRef]
- Khamashta-Ledezma, L.; Naini, F.B. Prospective Assessment of Maxillary Advancement Effects: Maxillary Incisor Exposure, and Upper Lip and Nasal Changes. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 454–464. [Google Scholar] [CrossRef]
- McCollum, A.G.H.; Reyneke, J.P.; Wolford, L.M. An Alternative for the Correction of the Class II Low Mandibular Plane Angle. Oral Surg. Oral Med. Oral Pathol. 1989, 67, 231–241. [Google Scholar] [CrossRef]
- Reyneke, J.P.; Evans, W.G. Surgical Manipulation of the Occlusal Plane. Int. J. Adult Orthod. Orthognath. Surg. 1990, 5, 99–110. [Google Scholar]
- Wolford, L.M.; Chemello, P.D.; Hilliard, F.W. Occlusal Plane Alteration in Orthognathic Surgery. J. Oral Maxillofac. Surg. 1993, 51, 730–740. [Google Scholar] [CrossRef] [PubMed]
- Van Den Bempt, M.; Vinayahalingam, S.; Han, M.D.; Bergé, S.J.; Xi, T. The Role of Muscular Traction in the Occurrence of Skeletal Relapse after Advancement Bilateral Sagittal Split Osteotomy (BSSO): A Systematic Review. Orthod. Craniofacial Res. 2022, 25, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wan, Z.; Shen, S.G.; Gui, H.; Zhang, P.; Shen, S. Evaluation of the Postoperative Stability of a Counter-Clockwise Rotation Technique for Skeletal Class II Patients by Using A Novel Three-Dimensional Position-Posture Method. Sci. Rep. 2019, 9, 13196. [Google Scholar] [CrossRef]
- Liebregts, J.; Baan, F.; Van Lierop, P.; De Koning, M.; Bergé, S.; Maal, T.; Xi, T. One-Year Postoperative Skeletal Stability of 3D Planned Bimaxillary Osteotomies: Maxilla-First versus Mandible-First Surgery. Sci. Rep. 2019, 9, 3000. [Google Scholar] [CrossRef]
- Schwartz, K.; Rodrigo-Domingo, M.; Jensen, T. Skeletal Stability after Large Mandibular Advancement (>10 Mm) with Bilateral Sagittal Split Osteotomy and Skeletal Elastic Intermaxillary Fixation. J. Oral Maxillofac. Res. 2016, 7, e5. [Google Scholar] [CrossRef] [PubMed]
- Palla, B.; Graca, S.; Licht, S.; Han, M.; Miloro, M. How Much Variation Exists Amongst Experienced Surgeons in Orthognathic Surgical Planning? Br. J. Oral Maxillofac. Surg. 2025, 63, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Steinbacher, D.M. Aesthetic Orthognathic Surgery and Rhinoplasty; Wiley Blackwell: Hoboken, NJ, USA, 2019; ISBN 978-1-119-18697-7. [Google Scholar]
- Naini, F.B. Facial Aesthetics: Concepts & Clinical Diagnosis; Wiley-Blackwell: Chichester West Sussex, UK, 2011; ISBN 978-1-118-78656-7. [Google Scholar]
- Jansma, J.; Schepers, R.H. Adjunctive Aesthetic Procedures in Orthognathic Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2023, 35, 139–152. [Google Scholar] [CrossRef] [PubMed]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyahya, A.; Bin Jasser, S. Optimizing Maxillomandibular Position in Orthognathic Surgery: Introducing the T Concept in Treatment Planning. Craniomaxillofac. Trauma Reconstr. 2025, 18, 45. https://doi.org/10.3390/cmtr18040045
Alyahya A, Bin Jasser S. Optimizing Maxillomandibular Position in Orthognathic Surgery: Introducing the T Concept in Treatment Planning. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(4):45. https://doi.org/10.3390/cmtr18040045
Chicago/Turabian StyleAlyahya, Abdulmalik, and Saud Bin Jasser. 2025. "Optimizing Maxillomandibular Position in Orthognathic Surgery: Introducing the T Concept in Treatment Planning" Craniomaxillofacial Trauma & Reconstruction 18, no. 4: 45. https://doi.org/10.3390/cmtr18040045
APA StyleAlyahya, A., & Bin Jasser, S. (2025). Optimizing Maxillomandibular Position in Orthognathic Surgery: Introducing the T Concept in Treatment Planning. Craniomaxillofacial Trauma & Reconstruction, 18(4), 45. https://doi.org/10.3390/cmtr18040045





