Matrix WaveTM System for Mandibulo-Maxillary Fixation—Just Another Variation on the MMF Theme? Part I: A Review on the Provenance, Evolution and Properties of the System
Abstract
1. Introduction
2. Evolution–Provenance
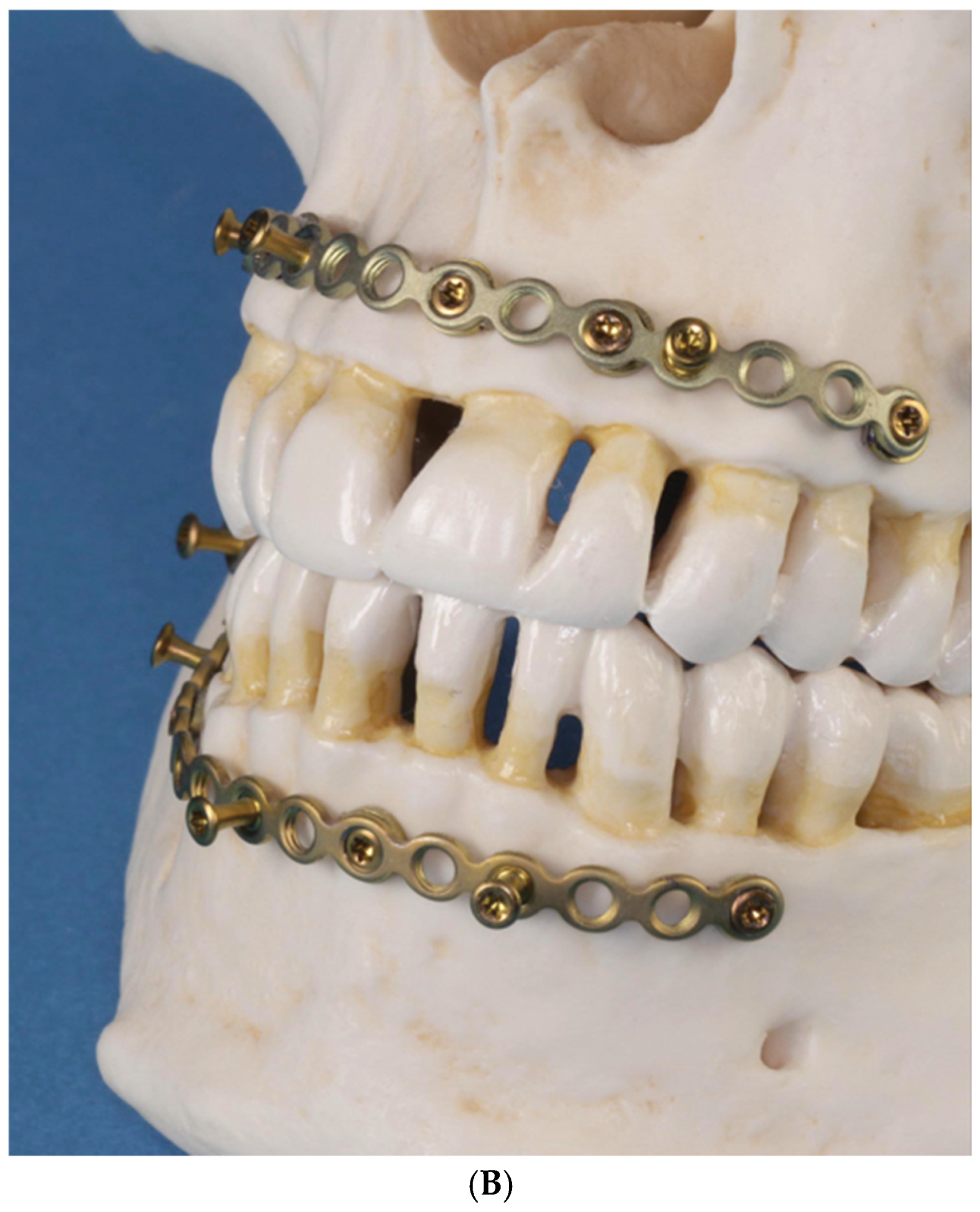
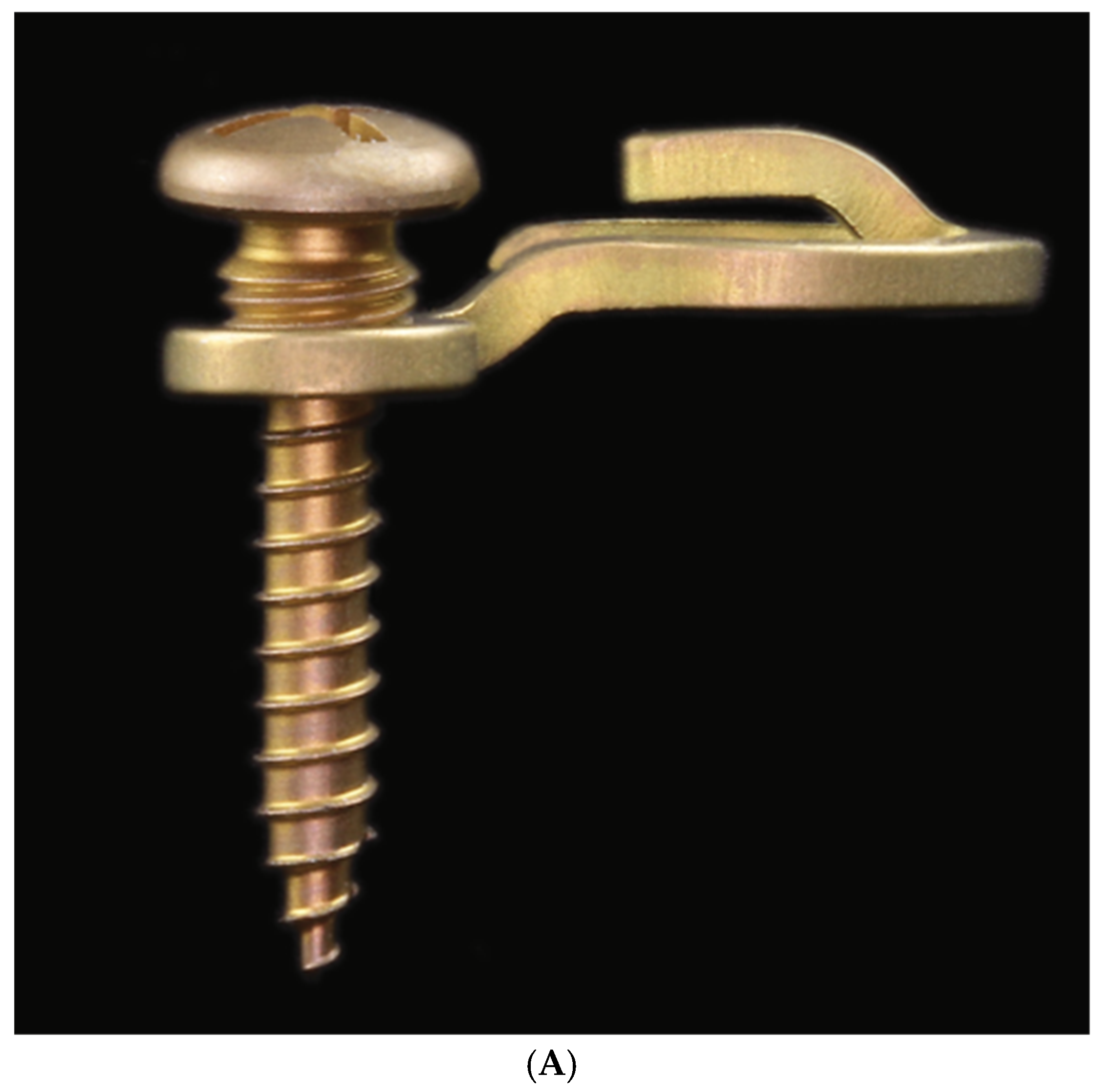
2.1. Locking Adaption Plate and MMF Nuts
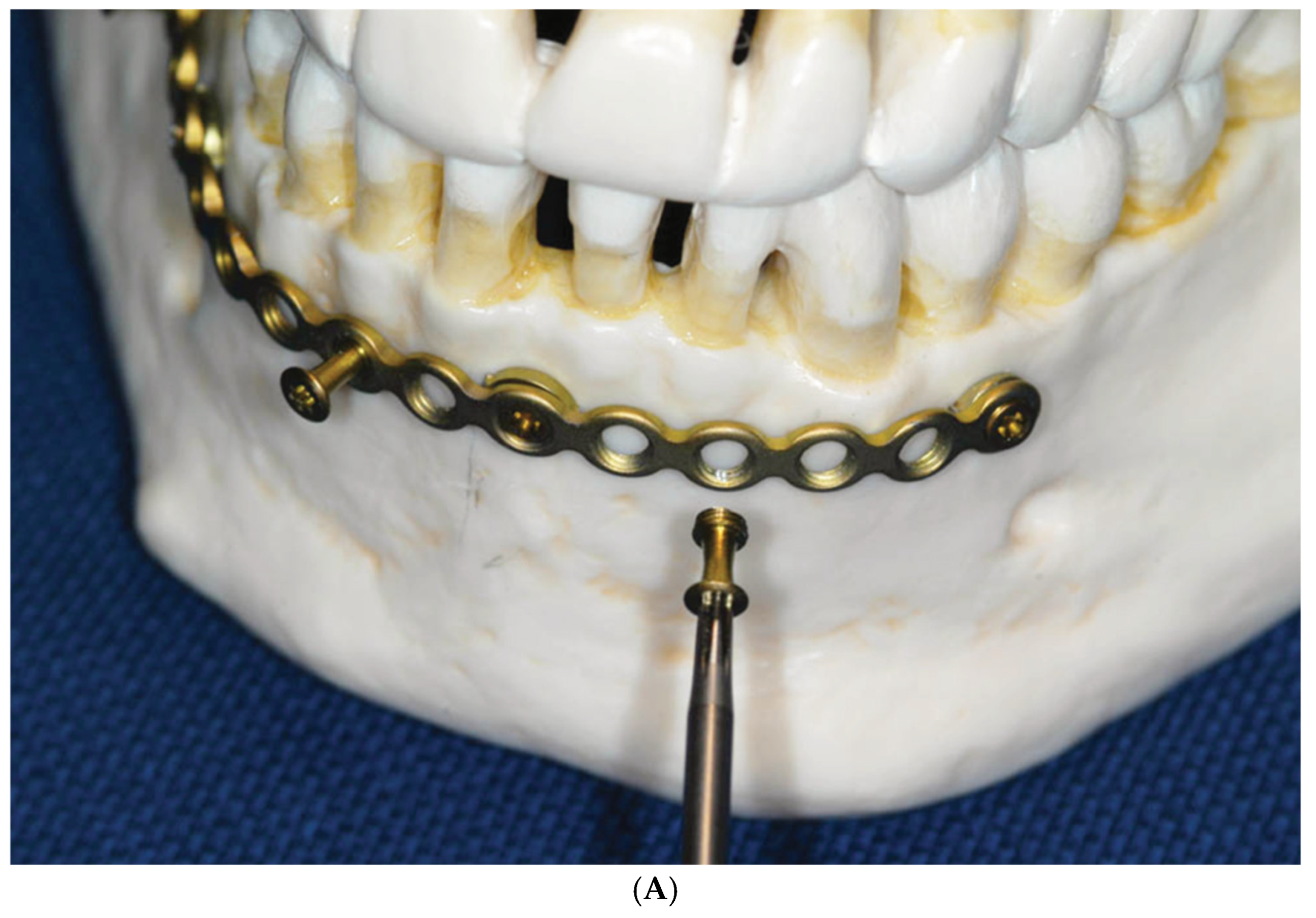
2.2. Predecessor—First-Wave Plate Version
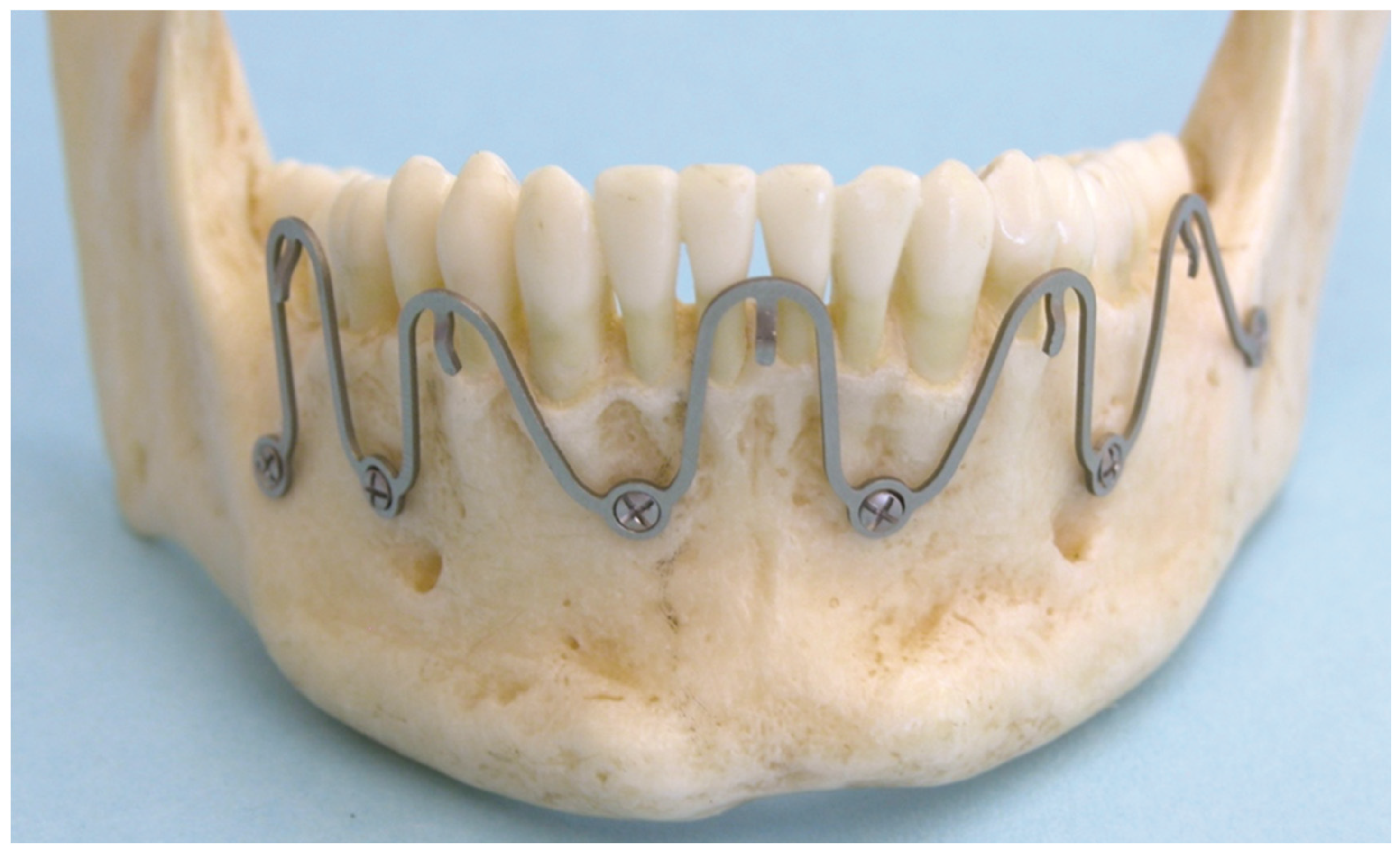
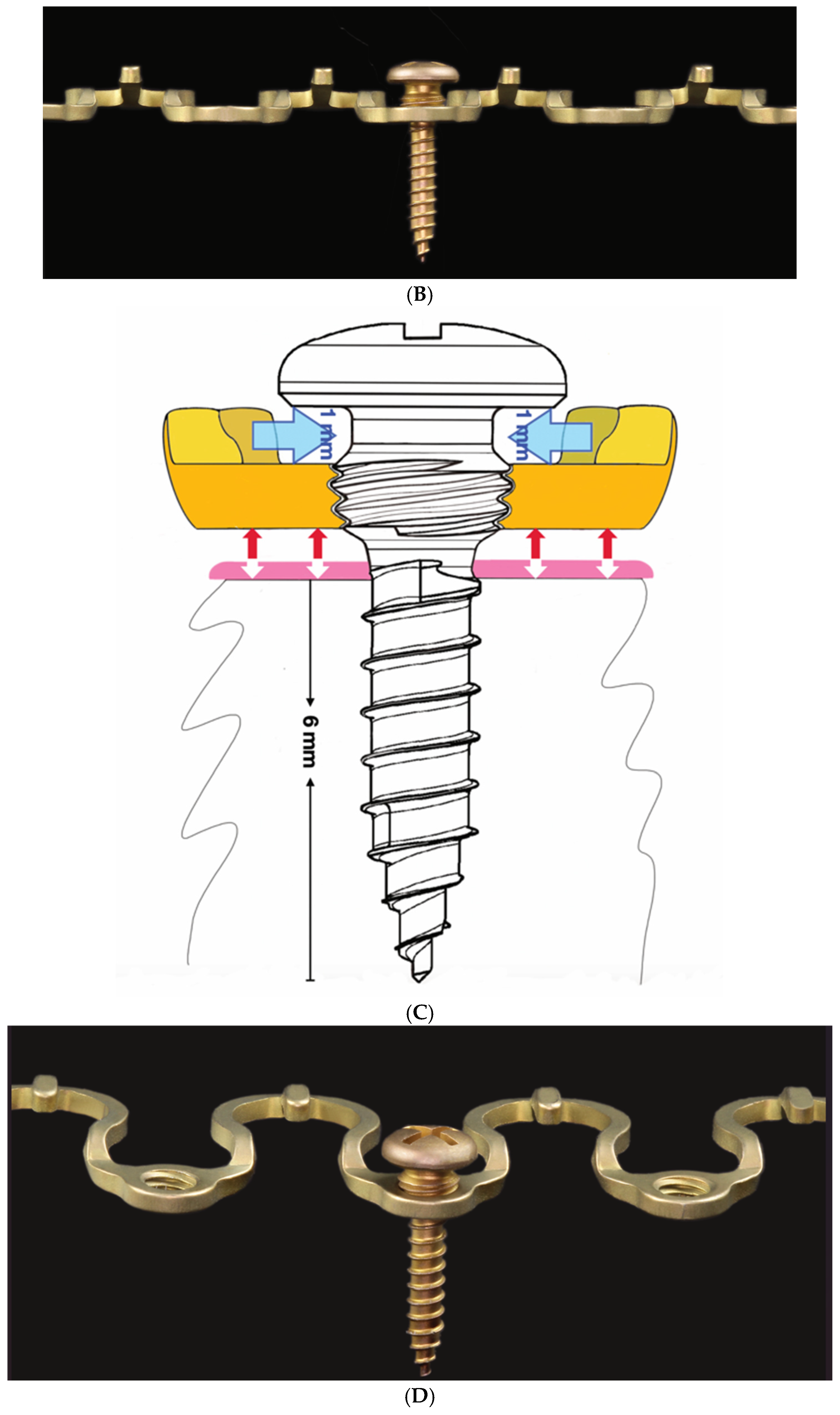
2.3. Matrix Wave System—Final Design and Technical Description
3. Methods
3.1. Matrix Wave Plate—Segmentation and Malleability
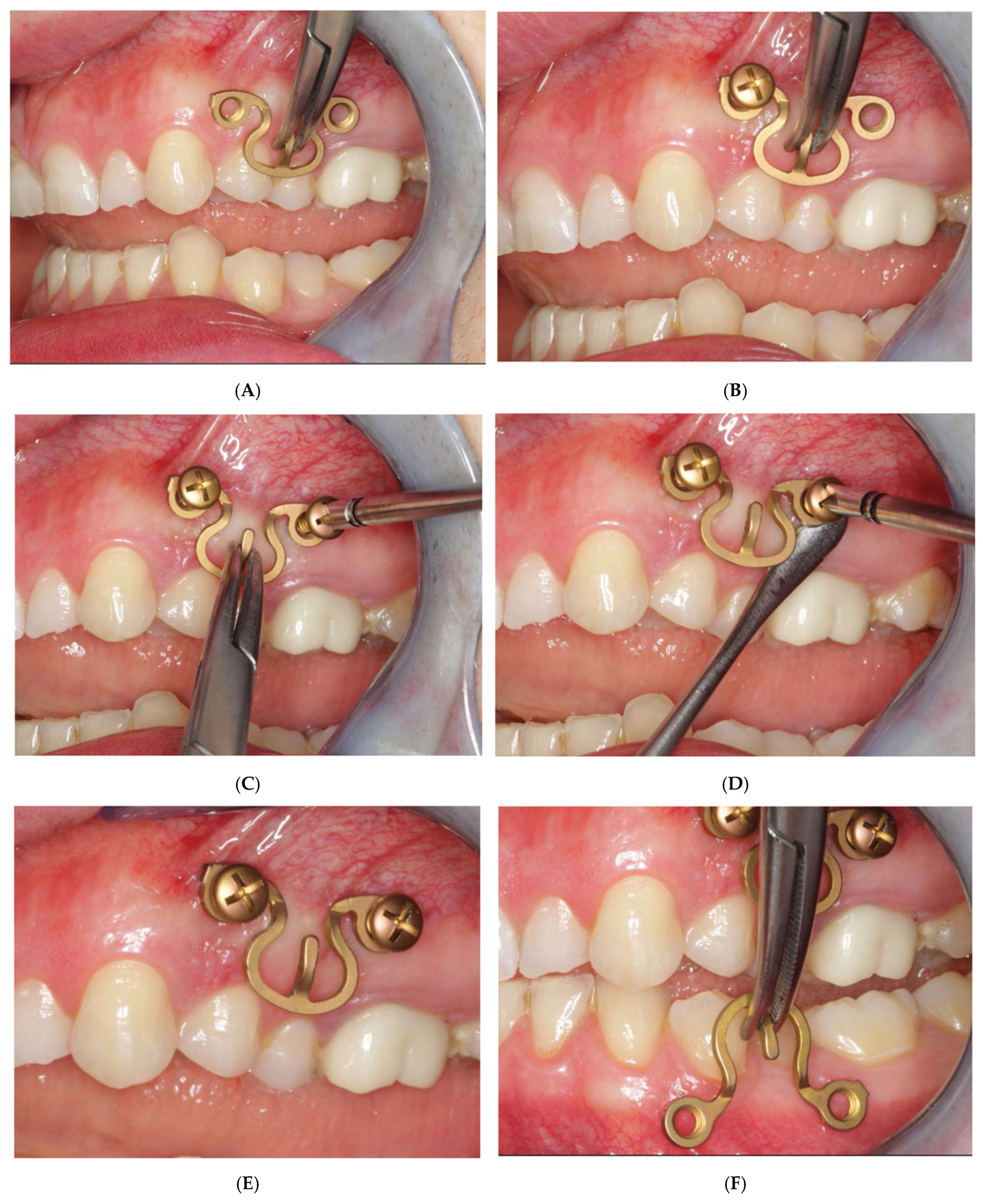
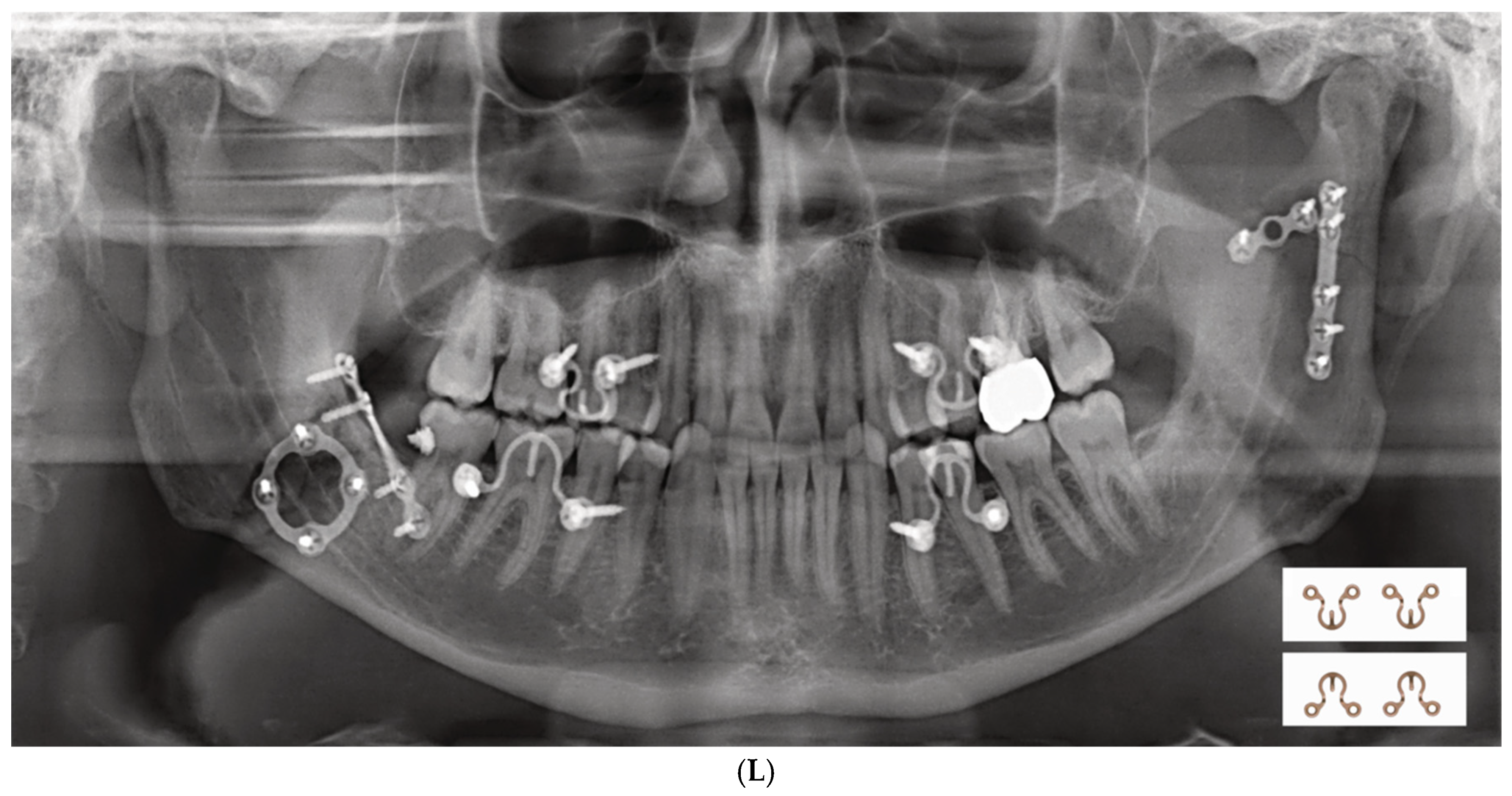
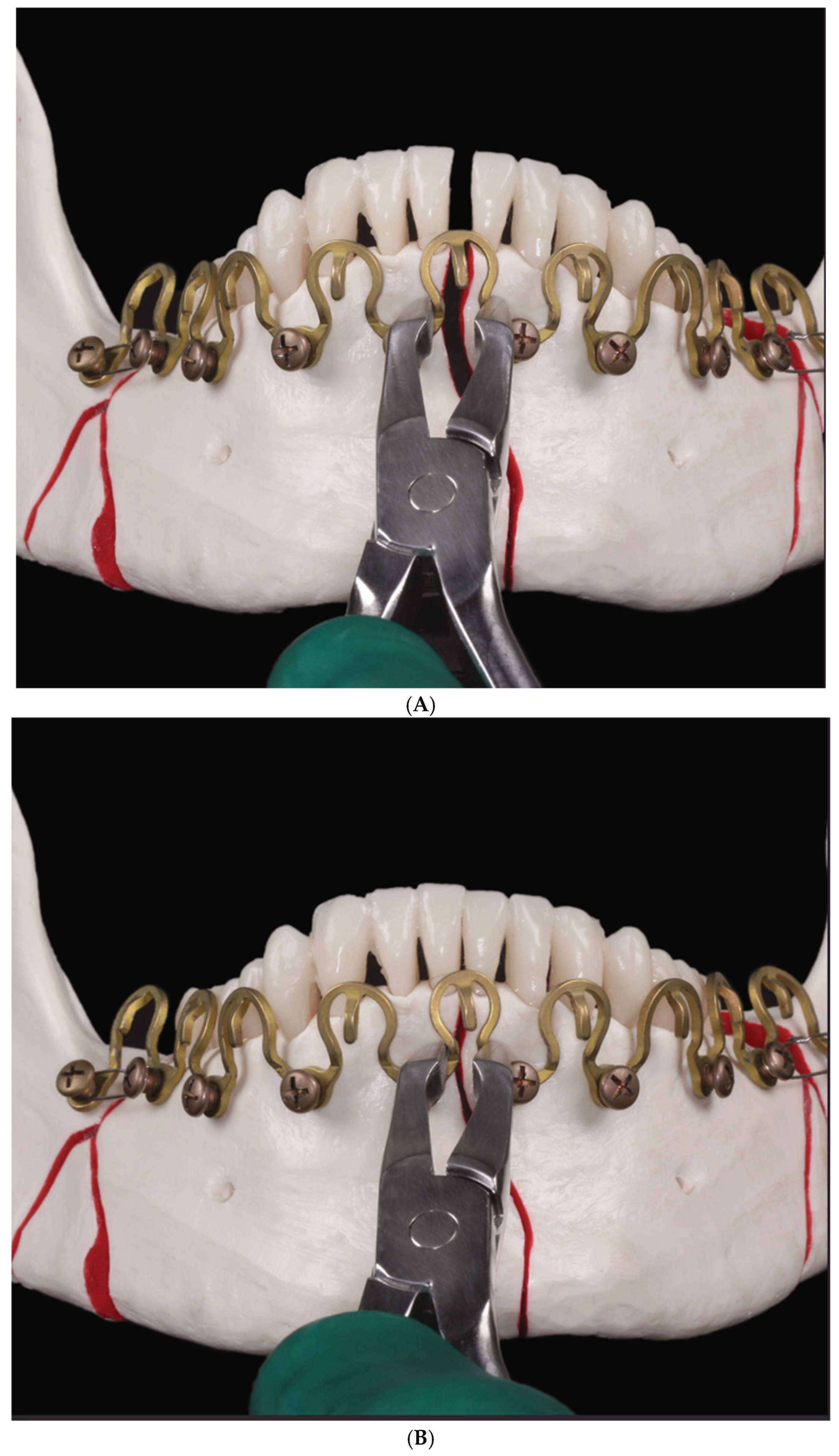
3.2. Matrix WaveTM Plate MMF System—Mode of Application
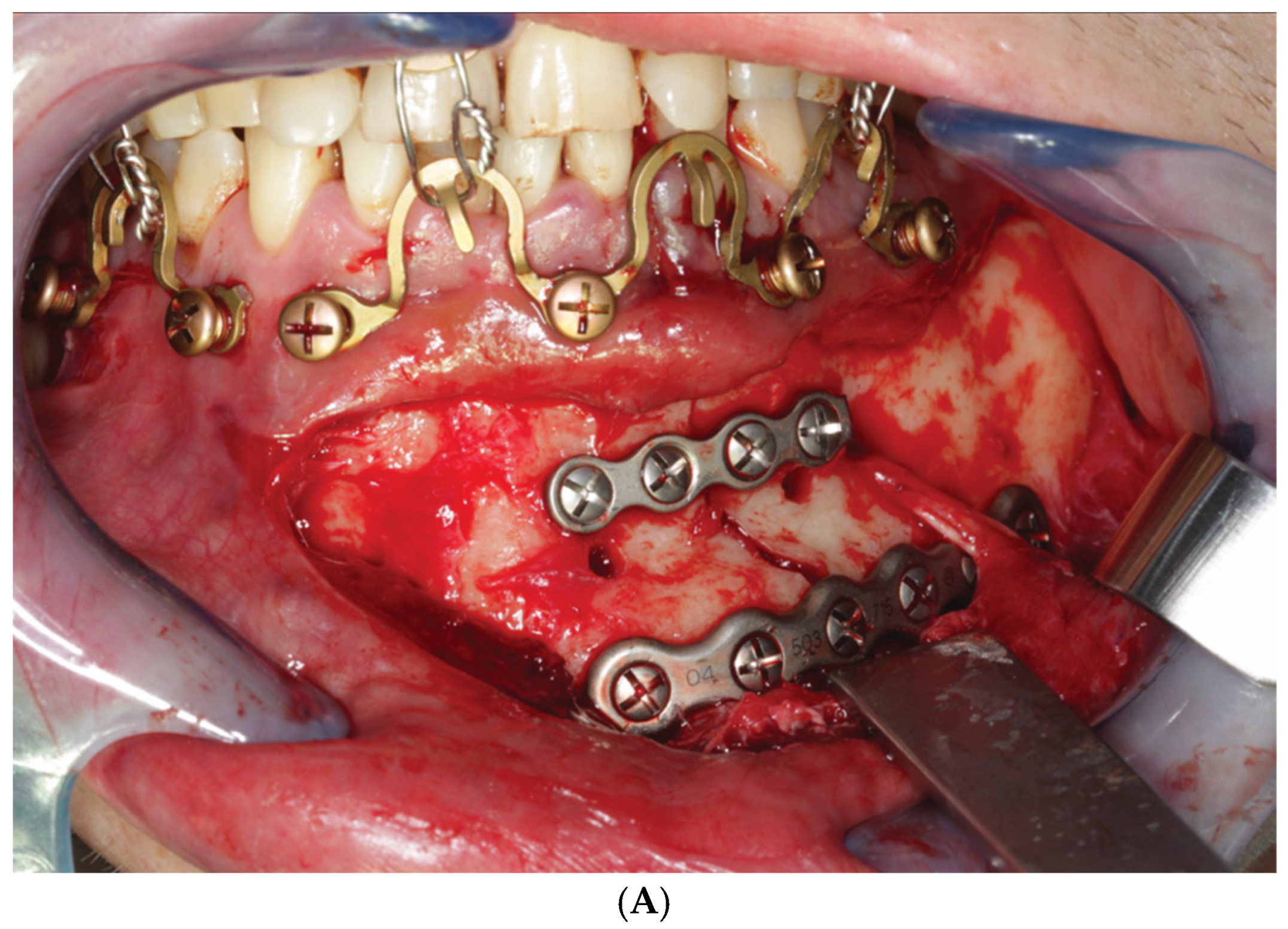
3.3. ‘In-Situ-Bending’ for Fracture Reduction
4. Discussion
4.1. Locking Adaptation Plate and MMF Nuts
- Adaptability of screw attachment location to prevent tooth root damage by screw;
- Insertion;
- Protection against compression of the buccal gingiva/attached mucosa;
- Vertical apposition of the plate/arch bar at a level non-irritant and atraumatic to periodontal tissues conjointly with the prevention of undesirable biomechanical effects;
- Flexible selection of interarch connection points (i.e., ‘wire hooks’);
- Reduction/adjustment of fragments;
- Tension band function in osteosynthesis of mandibular fractures;
- Potential advantages of a modular system.
4.2. Predecessor—First-Wave Plate Version
4.3. Second Wave Plate Version: Matrix WaveTM MMF System
- No scientific evidence for differences in stability of the anchorage, restitution ofpreinjury occlusal relationships and contacts as well as patient’s quality of life.
- MMF screws—shorter operating times at application and removal.
- EABs—lower risk for iatrogenic tooth injuries, greater risk for skin punctures/wirestick injuries.
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ernst, F. Die zahnärztliche Behandlung der Unterkieferfrakturen. In Die Chirurgie. Eine Zusammenfassende Darstellung der Allgemeinen und Speziellen Chirurgie; Kirschner, M., Ed.; Urban & Schwarzenberg: Berlin, Germany, 1927; pp. 842–852. [Google Scholar]
- Ernst, F. Die Schienenverbande bei Unter- und Oberkieferbrüchen. In Handbuch der Zahnheilkunde: Die Chirurgischen Erkrankungen der Mundhöhle, der Zähne und Kiefer; Bruhn, C., Kantorowicz, A., Partsch, C.P., Eds.; J.F. Bergmann: Wiesbaden, Germany, 1932; pp. 115–130, Kapitel 16, Abschnitt. [Google Scholar]
- Ivy, R.H. Observations of fracture of mandible. J. Am. Med. Assoc. 1922, 79, 295. [Google Scholar] [CrossRef]
- Ivy, R.H.; Curtis, L. Fractures of the Jaws, 1st ed.; Lea and Febiger: Philadelphia, PA, USA, 1931. [Google Scholar]
- Risdon, F. The treatment of fractures of the jaws. Can. Med. Assoc. J. 1929, 20, 260–262. [Google Scholar] [PubMed]
- Stout, R.A. Intermaxillary wiring and intermaxillary elastic traction and fixation. In Military Surgical Manuals National Research Council: Manual of Standard Practice of Plastic and Maxillofacial Surgery; Medical Department U.S. Army, Ed.; W.B. Saunders Co.: Philadelphia, PA, USA, 1943; p. 272. [Google Scholar]
- Obwegeser, H. Über eine einfache Methode der freihändigen Drahtschienung von Kieferbrüchen. Osterr. Z. Stomatol. 1952, 49, 652. [Google Scholar] [PubMed]
- Otten, J.E. Modifizierte Methode zur intermaxillären Fixation [Modified methods for intermaxillary immobilization]. Dtsch. Zahnaerztl Z. 1981, 36, 91–92. [Google Scholar]
- Arthur, G.; Berardo, N. A simplified technique of maxillomandibular fixation. J. Oral Maxillofac. Surg. 1989, 47, 1234. [Google Scholar] [CrossRef]
- Rinehart, G.C. Mandibulomaxillary fixation with bone anchors and quick-release ligatures. J. Craniofac Surg. 1998, 9, 215–221. [Google Scholar] [CrossRef]
- Gilmer, T.L. A case of fracture of lower jaw with remarks on treatment. Arch. Dent. 1887, 4, 388. [Google Scholar]
- Sauer, C. Herstellung eines neuen Verbandes bei Unterkieferbrüchen. Dtsch. Vjschr Zahnheilk 1881, 21, 362–375. [Google Scholar]
- Sauer, C. Notverband bei Kieferbrüchen mit Eisendraht. Dtsch. Mschr Zahnheilk 1889, 7, 381–392. [Google Scholar]
- Hauptmeyer, F. Die Behandlung der Brüche des Unter- und Oberkiefers mittels Zahnschienen. In Handbuch der Zahnheilkunde; Partsch, C., Bruhn, C., Kantorowicz, A., Eds.; Bergmann J.F.: Wiesbaden, Germany, 1917; pp. 104–145. [Google Scholar]
- Aderer, H.; Jelenko, J.F. Fracture. Splint. Patent No: US1638006, 9 August 1927. [Google Scholar]
- Erich, J.B. Treatment of fractures of the upper jaw. J. Am. Dent. Assoc 1942, 29, 783–793. [Google Scholar] [CrossRef]
- Erich, J.B.; Austin, L.T. Medicine USNDBo, Surgery. Traumatic Injuries of Facial Bones: An Atlas of Treatment; W.B. Saunders: Philadelphia, PA, USA, 1944. [Google Scholar]
- Schuchardt, K. Ein Vorschlag zur Verbesserung der Drahtschienenverbände. Dtsch. Zahn Mund. Kieferheilk 1956, 24, 39–44. [Google Scholar]
- Schuchardt, K.; Kapovits, M.; Spiessl, B. Technik und Anwendung des Drahtbogenkunsstoffverbandes. Dtsch. Zahnarztl. Z. 1961, 16, 1241–1249. [Google Scholar]
- Stanhope, E. Acrylated arch bars. Br. J. Oral Surg. 1969, 7, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Hallermann, W.; Seto, I.; Smolka, W. A titanium arch bar for maxillomandibular fixation in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 2006, 64, 989–992. [Google Scholar] [CrossRef]
- Baurmash, H.D. Bonding as an overdue replacement of the wiring of arch bars—Letter to the editor. J. Oral Maxillofac. Surg. 2006, 64, 1701–1702. [Google Scholar] [CrossRef]
- McCaul, J.A.; Devlin, M.F.; Lowe, T. A new method for temporary maxillo-mandibular fixation. Int. J. Oral Maxillofac. Surg. 2004, 33, 502–503. [Google Scholar] [CrossRef]
- Pigadas, N.; Whitley, S.P.; Roberts, S.A.; McAlister, K.; Ameerally, P.; Avery, C.M. A randomized controlled trial on cross-infection control in maxillofacial trauma surgery: A comparison of intermaxillary fixation techniques. Int. J. Oral Maxillofac. Surg. 2008, 37, 716–722. [Google Scholar] [CrossRef]
- Cousin, G.C. Wire-free fixation of jaw fractures. Br. J. Oral Maxillofac. Surg. 2009, 47, 521–524. [Google Scholar] [CrossRef]
- Johnson, A.W. Dental occlusion ties: A rapid, safe, and non-invasive maxillo-mandibular fixation technology. Laryngoscope Investig. Otolaryngol. 2017, 2, 178–183. [Google Scholar] [CrossRef]
- Jenzer, A.C.; Malz, C.; Fillmore, J.; Wolford, L.M.; Warner, M.R.; Ivory, J.W.; Swift, J.Q. The Role of Dental Occlusion Ties to Achieve Stable Maxillomandibular Fixation During Temporomandibular Joint Replacement. J. Oral Maxillofac. Surg. 2022, 80, 1731–1739. [Google Scholar] [CrossRef]
- Druelle, C.; Touzet-Roumazeille, S.; Raoul, G.; Ferri, J.; Nicot, R. How to produce pre-shaped rigid arch bars using low-cost 3D printing technology—A technical note. J. Stomatol. Oral Maxillofac. Surg. 2017, 118, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Tache, A.; Huys, S.E.F.; Mommaerts, M.Y. CADCAM Arch Bars: A technical note. Craniomaxillofacial Trauma. Reconstr. Open 2021, 6, 24727512211047042. [Google Scholar] [CrossRef]
- de Queiroz, S.B. Modification of arch bars used for intermaxillary fixation in oral and maxillofacial surgery. Int. J. Oral Maxillofac. Surg. 2013, 42, 481–482. [Google Scholar] [CrossRef] [PubMed]
- Suresh, V.; Sathyanarayanan, N.; Venugopalan, V.; Beena, A.T. A simple maneuvre for promising results—Opening the winglets of an arch bar for placement of screws: A Technical note. GJRA 2015, 4, 368–369. [Google Scholar]
- Hassan, S.; Farooq, S.; Kapoor, M.; Shah, A. Comparative evaluation of modified Erich’s arch bar, conventional Erich’s arch bar and intermaxillary fixation screws in maxillo-mandibular fixation: A prospective clinical study. Int. J. Med. Res. Prof. 2018, 4, 41–45. [Google Scholar] [CrossRef]
- Rothe, T.M.; Kumar, P.; Shah, N.; Shah, R.; Kumar, A.; Das, D. Evaluation of efficacy of intermaxillary fixation screws versus modified arch bar for intermaxillary fixation. Natl. J. Maxillofac. Surg. 2018, 9, 134–139. [Google Scholar] [CrossRef]
- Rothe, T.M.; Kumar, P.; Shah, N.; Shah, R.; Mahajan, A.; Kumar, A. Comparative evaluation of efficacy of conventional arch bar, intermaxillary fixation screws, and modified arch bar for intermaxillary fixation. J. Maxillofac. Oral Surg. 2019, 18, 412–418. [Google Scholar] [CrossRef]
- Pathak, P.; Thomas, S.; Bhargava, D.; Beena, S. A prospective comparative clinical study on modified screw retained arch bar (SRAB) and conventional Erich’s arch bar (CEAB). Oral Maxillofac. Surg. 2019, 23, 285–289. [Google Scholar] [CrossRef]
- Venugopalan, V.; Satheesh, G.; Balatandayoudham, A.; Duraimurugan, S.; Balaji, T.S. A comparative randomized prospective clinical study on modified Erich arch bar with conventional Erich arch bar for maxillomandibular fixation. Ann. Maxillofac. Surg. 2020, 10, 287–291. [Google Scholar] [CrossRef]
- Kohler, K.; Pinto, J.; Johnston, T.S.; Papay, F.A., Jr. Maxillomandibular Fixation. Devices. Patent No. US 10,470,806 B2, 12 November 2019. [Google Scholar]
- Frigg, R.; Richter, J.; Leuenberger, S.; Cornelius, C.P.; Hamel, R.J. Flexible Maxillo Mandibular Fixation. Device. Patent No. US 2011,0152946 A1, 23 June 2011. [Google Scholar]
- Woodburn, W.N.; Griffith, W.; Barber, J.R.; Parranto, G. U.S. Patent No. US9,820,77 B2, 23 June 2018.
- Cornelius, C.P.; Hardeman, J. Craniomaxillofacial—MatFlexible Maxillo- Mandibular Fixation Devicerix Wave MMF. AOTK Syst. Innov. 2015, 1, 19–21. [Google Scholar]
- Cornelius, C.P.; Ehrenfeld, M. The Use of MMF Screws: Surgical Technique, Indications, Contraindications, and Common Problems in Review of the Literature. Craniomaxillofac Trauma. Reconstr. 2010, 3, 55–80. [Google Scholar] [CrossRef] [PubMed]
- Kiwanuka, E.; Iyengar, R.; Jehle, C.C.; Mehrzad, R.; Kwan, D. The use of Synthes MatrixWAVE bone anchored arch bars for closed treatment of multiple concurrent mandibular fractures. J. Oral Biol. Craniofac Res. 2017, 7, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., 3rd; Tharanon, W. Facial width problems associated with rigid fixation of mandibular fractures: Case reports. J. Oral Maxillofac. Surg. 1992, 50, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhang, Y.; An, J.G.; He, Y. Width-controlling fixation of symphyseal/parasymphyseal fractures associated with bilateral condylar fractures with 2 2.0-mm miniplates: A retrospective investigation of 45 cases. J. Oral Maxillofac. Surg. 2016, 74, 315–327. [Google Scholar] [CrossRef]
- Gerbino, G.; Boffano, P.; Bosco, G.F. Symphyseal mandibular fractures associated with bicondylar fractures: A retrospective analysis. J. Oral Maxillofac. Surg. 2009, 67, 1656–1660. [Google Scholar] [CrossRef]
- Spiessl, B. Application of the tension band principle in the Mandible, Tension band plate Part I, Basic principles, 4.1.2.1–4.1.2.4, pp 34. In Internal Fixation of the Mandible—A Manual of AO/ASIF Principles; Springer: Berlin/Heidelberg, Germany, 1989. [Google Scholar]
- Wang, R.C.; Keech, D.R.; Elkins, T.P.; Russell, P. The tension wire method: A simple, effective means of mandibular fixation. Arch. Otolaryngol. Head. Neck Surg. 1998, 124, 448–452. [Google Scholar] [CrossRef][Green Version]
- Hasegawa, A.; Leake, D. A new arch bar for oral surgery. Int. J. Oral Surg. 1981, 10, 462–464. [Google Scholar] [CrossRef]
- Kornman, K.S.; Holt, S.C.; Robertson, P.B. The microbiology of ligature-induced periodontitis in the cynomolgus monkey. J. Periodontal Res. 1981, 16, 363–371. [Google Scholar] [CrossRef]
- Tatakis, D.N.; Kumar, P.S. Etiology and pathogenesis of periodontal diseases. Dent. Clin. N. Am. 2005, 49, 491–516. [Google Scholar] [CrossRef]
- Pedemonte, C.; Valenzuela, K.; González, L.E.; Vargas, I.; Noguera, A. Types of intermaxillary fixation and their interaction with palatine fracture reduction. J. Oral Maxillofac. Surg. 2019, 77, 2083.e1–2083.e8. [Google Scholar] [CrossRef]
- Gray, J. The mechanism of locomotion in snakes. J. Exp. Biol. 1946, 23, 101–120. [Google Scholar] [CrossRef] [PubMed]
- Jayne, B.C. What Defines Different Modes of Snake Locomotion? Integr. Comp. Biol. 2020, 60, 156–170. [Google Scholar] [CrossRef] [PubMed]
- Park, K.N.; Oh, S.M.; Lee, C.Y.; Kim, J.Y.; Yang, B.E. Design and application of hybrid maxillomandibular fixation for facial bone fractures. J. Craniofac Surg. 2013, 24, 1801–1805. [Google Scholar] [CrossRef] [PubMed]
- Falci, S.G.; Douglas-de-Oliveira, D.W.; Stella, P.E.; Santos, C.R. Is the Erich arch barthe best intermaxillary fixation method in maxillofacial fractures? A systematic review. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e494–e499. [Google Scholar] [CrossRef]
- Schneider, A.M.; David, L.R.; DeFranzo, A.J.; Marks, M.W.; Molnar, J.A.; Argenta, L.C. Use of specialized bone screws for intermaxillary fixation. Ann. Plast. Surg. 2000, 44, 154–157. [Google Scholar] [CrossRef]
- Ho, K.S.; Tan, W.K.; Loh, H.S. Case reports: The use of intermaxillary screws to achieve intermaxillary fixation in the treatment of mandibular fractures. Ann. Acad. Med. Singap. 2000, 29, 534–537. [Google Scholar]
- Maurer, P.; Syska, E.; Eckert, A.W.; Berginski, M.; Schubert, J. Die FAMI-Schraube fur die temporare intermaxillare Fixation. Erfahrungsbericht zur Indikationserweiterung [The FAMI screw for temporary intermaxillary fixation. Report of experiences for extending indications]. Mund. Kiefer Gesichtschir 2002, 6, 360–362. [Google Scholar] [CrossRef]
- Hoffmann, A.; Mast, G.; Ehrenfeld, M. Verwendung von IMF-Schrauben zur mandibulo-maxillären Fixation. OP-J. 2003, 19, 70–75. [Google Scholar] [CrossRef]
- Fabbroni, G.; Aabed, S.; Mizen, K.; Starr, D.G. Transalveolar screws and the incidence of dental damage: A prospective study. Int. J. Oral Maxillofac. Surg. 2004, 33, 442–446. [Google Scholar] [CrossRef]
- Roccia, F.; Tavolaccini, A.; Dell’Acqua, A.; Fasolis, M. An audit of mandibular fractures treated by intermaxillary fixation using intraoral cortical bone screws. J. Craniomaxillofac Surg. 2005, 33, 251–254. [Google Scholar] [CrossRef]
- Imazawa, T.; Komuro, Y.; Inoue, M.; Yanai, A. Mandibular fractures treated with maxillomandibular fixation screws (MMFS method). J. Craniofac Surg. 2006, 17, 544–549. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Coletti, D.P.; Salama, A.; Caccamese, J.F., Jr. Application of intermaxillary fixation screws in maxillofacial trauma. J. Oral Maxillofac. Surg. 2007, 65, 1746–1750. [Google Scholar] [CrossRef] [PubMed]
- Kauke, M.; Safi, A.F.; Timmer, M.; Nickenig, H.J.; Zöller, J.; Kreppel, M. FAMI Screws for Mandibulo-Maxillary fixation in mandibular fracture treatment—Clinico-radiological evaluation. J. Craniomaxillofac Surg. 2018, 46, 566–572. [Google Scholar] [CrossRef]
- Mostoufi, B.; Sands, J.; Patel, M.; Warburton, G.; Caccamese, J. Fracture propagation associated with intermaxillary fixation screws in maxillofacial trauma. Int. J. Oral Maxillofac. Surg. 2020, 49, 491–495. [Google Scholar] [CrossRef]
- Nandini, G.D.; Balakrishna, R.; Rao, J. Self tapping screws v/s Erich arch bar for inter maxillary fixation: A comparative clinical study in the treatment of mandibular fractures. J. Maxillofac. Oral Surg. 2011, 10, 127–131. [Google Scholar] [CrossRef]
- Satish, M.; Rahman, N.M.; Reddy, V.S.; Yuvaraj, A.; Muliyar, S.; Razak, P.A. Use of cortical bone screws in maxillofacial surgery—A prospective study. J. Int. Oral Health 2014, 6, 62–67. [Google Scholar]
- Karthick, S.; Prabhu, M.N.; Arva, K. Comparison of Arch Bar, Eyelets and Transmucosal Screws for Maxillo Mandibular Fixation in Jaw Fratcure. Biomed. Pharmacol. J. 2017, 10, 497–508. [Google Scholar] [CrossRef]
- Kumar, P.; Menon, G.; Rattan, V. Erich arch bar versus hanger plate technique for intermaxillary fixation in fracture mandible: A prospective comparative study. Natl. J. Maxillofac. Surg. 2018, 9, 33–38. [Google Scholar] [CrossRef]
- Rai, A.; Datarkar, A.; Borle, R.M. Are maxillomandibular fixation screws a better option than Erich arch bars in achieving maxillomandibular fixation? A randomized clinical study. J. Oral Maxillofac. Surg. 2011, 69, 3015–3018. [Google Scholar] [CrossRef]
- van den Bergh, B.; Blankestijn, J.; van der Ploeg, T.; Tuinzing, D.B.; Forouzanfar, T. Conservative treatment of a mandibular condyle fracture: Comparing intermaxillary fixation with screws or arch bar. A randomised clinical trial. J. Craniomaxillofac Surg. 2015, 43, 671–676. [Google Scholar] [CrossRef]
- Sandhu, Y.K.; Padda, S.; Kaur, T.; Dhawan, A.; Kapila, S.; Kaur, J. Comparison of efficacy of transalveolar screws and conventional dental wiring using Erich arch bar for maxillomandibular fixation in mandibular fractures. J. Maxillofac. Oral Surg. 2018, 17, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, I.A.; Al-Moraissi, E.A.; Galvão, E.L.; Falci, S.G.M. Erich arch bars vs. intermaxillary fixation screws for mandibular fracture reduction during ORIF: A randomized clinical trial. Clin. Oral Investig. 2023, 27, 6063–6071. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.; Jr Baratieri, C.; Araujo, M.T.; Souza, M.M.; Maia, L.C. Root damage associated with intermaxillary screws: A systematic review. Int. J. Oral Maxillofac. Surg. 2012, 41, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Delbet-Dupas, C.; Pham Dang, N.; Mondié, J.M.; Barthélémy, I. Blocage maxillo-mandibulaire peropératoire des fractures de mandibule: Arcs ou vis de blocage? [Intermaxillary intraoperative fixation of mandibular fractures: Arch bars or fixation screws?]. Rev. Stomatol. Chir. Maxillofac. Chir. Orale 2013, 114, 315–321. [Google Scholar] [CrossRef]
- Qureshi, A.A.; Reddy, U.K.; Warad, N.M.; Badal, S.; Jamadar, A.A.; Qurishi, N. Intermaxillary fixation screws versus Erich arch bars in mandibular fractures: A comparative study and review of literature. Ann. Maxillofac. Surg. 2016, 6, 25–30. [Google Scholar] [CrossRef]
- Kopp, R.W.; Crozier, D.L.; Goyal, P.; Kellman, R.M.; Suryadevara, A.C. Decade review of mandible fractures and arch bar impact on outcomes of nonsubcondylar fractures. Laryngoscope 2016, 126, 596–601. [Google Scholar] [CrossRef]
- Fernandes, I.A.; Lopes, A.B.; Fonseca, P.G.; da Silva Torres, A.; Rodrigues, A.B.; Galvão, E.L.; Falci, S.G. Comparison between Erich arch bars and intermaxillary screws in maxillofacial fractures involving the dental occlusion: A meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 83–95. [Google Scholar] [CrossRef]
- Park, H.I.; Choi, Y.J.; Lee, J.H. The assessment of intermaxillary fixation and open reduction using skeletal anchorage system compared with arch bar in mandible fractures based on CT image. J. Craniofac Surg. 2023, 34, 1493–1495. [Google Scholar] [CrossRef]
- Kumaresan, R.; Ponnusami, K.; Karthikeyan, P. Custom-Made Finger Guard to Prevent Wire-Stick Injury to the Operator’s Finger while Performing Intermaxillary Fixation. Craniomaxillofac Trauma. Reconstr. 2014, 7, 327–329. [Google Scholar] [CrossRef]
- Brandtner, C.; Borumandi, F.; Krenkel, C.; Gaggl, A. Blunt wires in oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 2015, 53, 301–302. [Google Scholar] [CrossRef]
- Kendrick, D.E.; Park, C.M. Reply: Stryker SMARTLock Hybrid Maxillo- mandibular Fixation System: Clinical application, complications, and radiographic findings. Plast Reconstr Surg 2016, 138, 949e. [Google Scholar] [CrossRef] [PubMed]
- Roeder, R.A.; Guo, L.; Lim, A.A. Is the SMARTLock Hybrid Maxillomandibular Fixation System comparable to intermaxillary fixation screws in closed reduction of condylar fractures? Ann Plast Surg 2018, 81 (Suppl. S1), S35–S38. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.S.; Graham, R.M. Perils of intermaxillary fixation screws. Br. J. Oral Maxillofac. Surg. 2020, 58, 728–730. [Google Scholar] [CrossRef] [PubMed]
- Sankar, H.; Rai, S.; Jolly, S.S.; Rattan, V. Comparison of efficacy and safety of hybrid arch bar with Erich arch bar in the management of mandibular fractures: A randomized clinical trial. Craniomaxillofac Trauma. Reconstr. 2023, 16, 94–101. [Google Scholar] [CrossRef]
- Cornelius, C.-P.; Liokatis, P.G.; Doerr, T.; Matic, D.; Fusetti, S.; Rasse, M.; Gellrich, N.C.; Heiland, M.; Schubert, W.; Buchbinder, D. Matrix WaveTM system for mandibulo-maxillary fixation—Just another variation on the MMF theme ?—Part II: In context to selfmade hybrid Erich arch bars and commercial hybrid MMF systems—Review of the literature and analysis of design features. Craniomaxillofac Trauma Reconstr. 2025. submitted. [Google Scholar]














Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cornelius, C.-P.; Liokatis, P.G.; Doerr, T.; Matic, D.; Fusetti, S.; Rasse, M.; Gellrich, N.C.; Heiland, M.; Schubert, W.; Buchbinder, D. Matrix WaveTM System for Mandibulo-Maxillary Fixation—Just Another Variation on the MMF Theme? Part I: A Review on the Provenance, Evolution and Properties of the System. Craniomaxillofac. Trauma Reconstr. 2025, 18, 32. https://doi.org/10.3390/cmtr18030032
Cornelius C-P, Liokatis PG, Doerr T, Matic D, Fusetti S, Rasse M, Gellrich NC, Heiland M, Schubert W, Buchbinder D. Matrix WaveTM System for Mandibulo-Maxillary Fixation—Just Another Variation on the MMF Theme? Part I: A Review on the Provenance, Evolution and Properties of the System. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(3):32. https://doi.org/10.3390/cmtr18030032
Chicago/Turabian StyleCornelius, Carl-Peter, Paris Georgios Liokatis, Timothy Doerr, Damir Matic, Stefano Fusetti, Michael Rasse, Nils Claudius Gellrich, Max Heiland, Warren Schubert, and Daniel Buchbinder. 2025. "Matrix WaveTM System for Mandibulo-Maxillary Fixation—Just Another Variation on the MMF Theme? Part I: A Review on the Provenance, Evolution and Properties of the System" Craniomaxillofacial Trauma & Reconstruction 18, no. 3: 32. https://doi.org/10.3390/cmtr18030032
APA StyleCornelius, C.-P., Liokatis, P. G., Doerr, T., Matic, D., Fusetti, S., Rasse, M., Gellrich, N. C., Heiland, M., Schubert, W., & Buchbinder, D. (2025). Matrix WaveTM System for Mandibulo-Maxillary Fixation—Just Another Variation on the MMF Theme? Part I: A Review on the Provenance, Evolution and Properties of the System. Craniomaxillofacial Trauma & Reconstruction, 18(3), 32. https://doi.org/10.3390/cmtr18030032






