A 3D Printed Hydroxyapatite Implant for Temporal Hollowing Reconstruction: A Patient-Specific Approach
Abstract
1. Introduction
2. Case Presentation
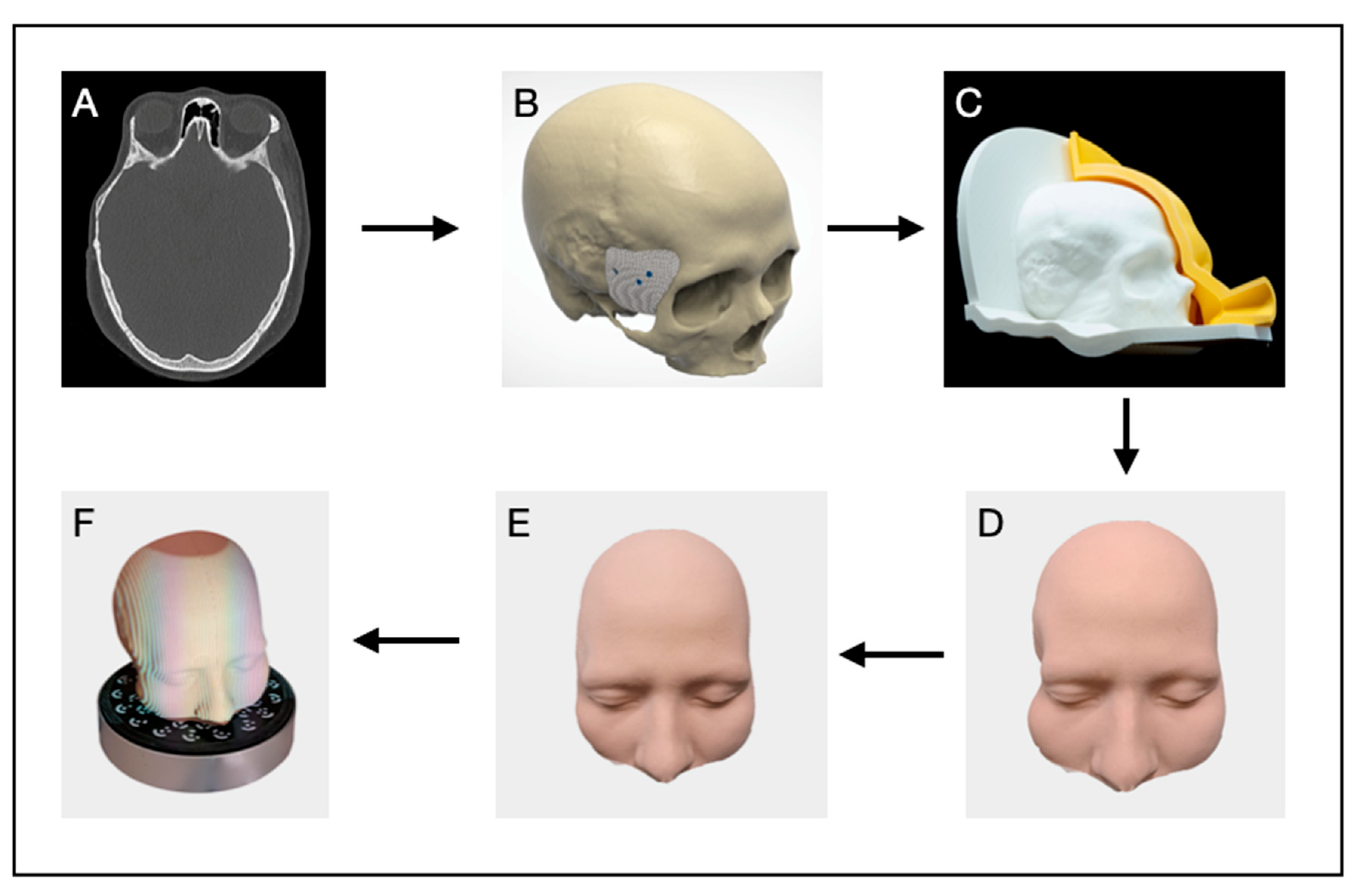
2.1. Digital Planning
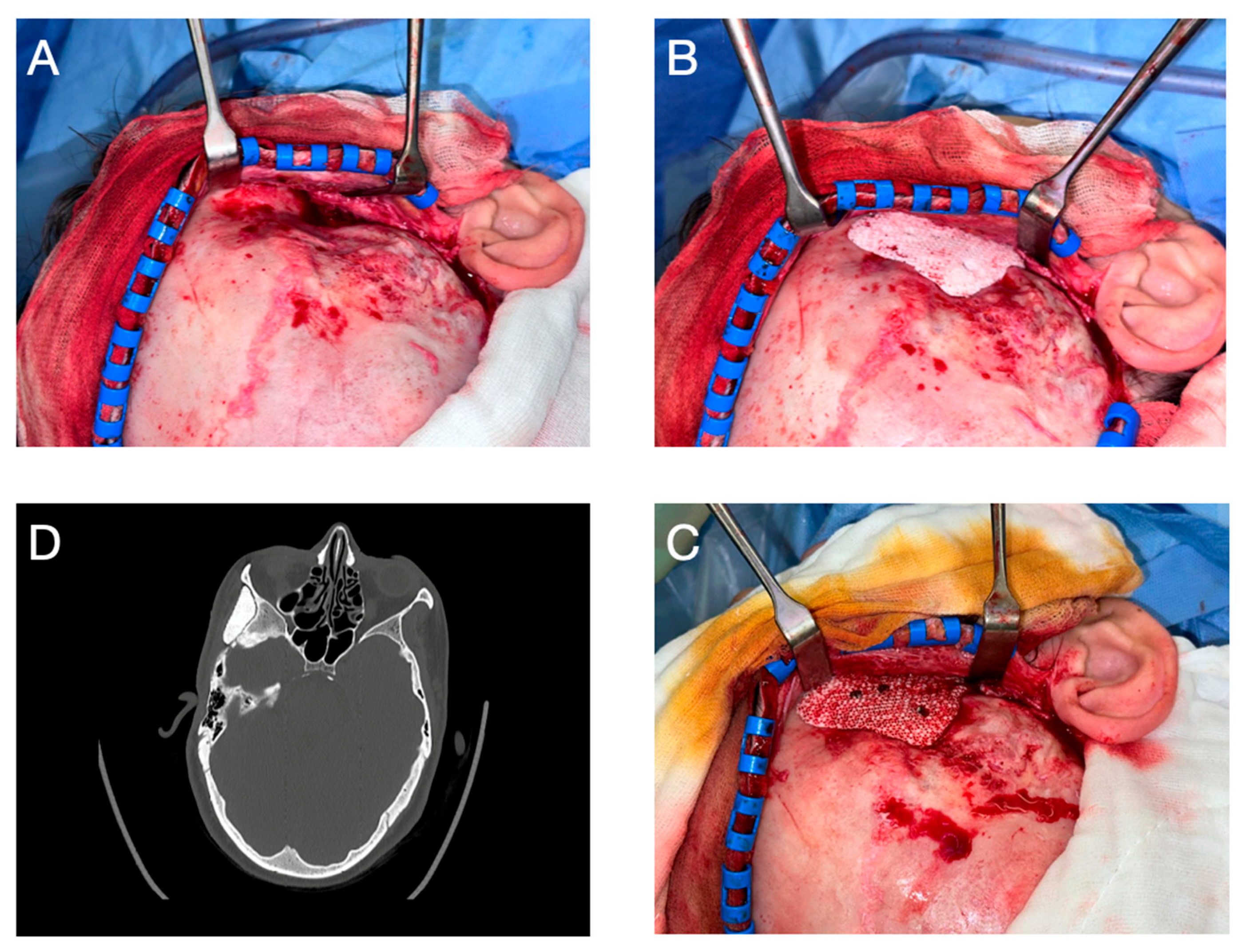
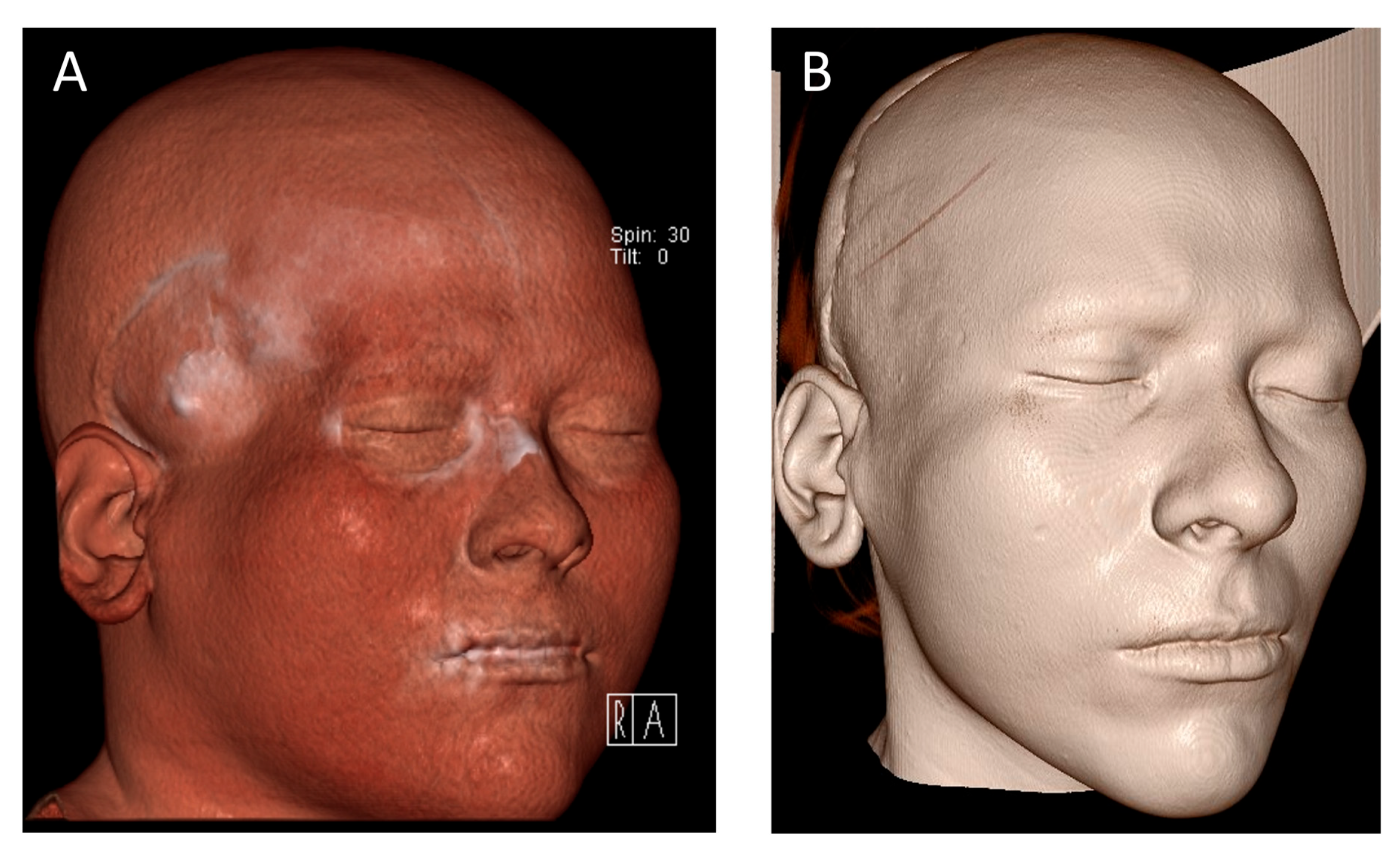
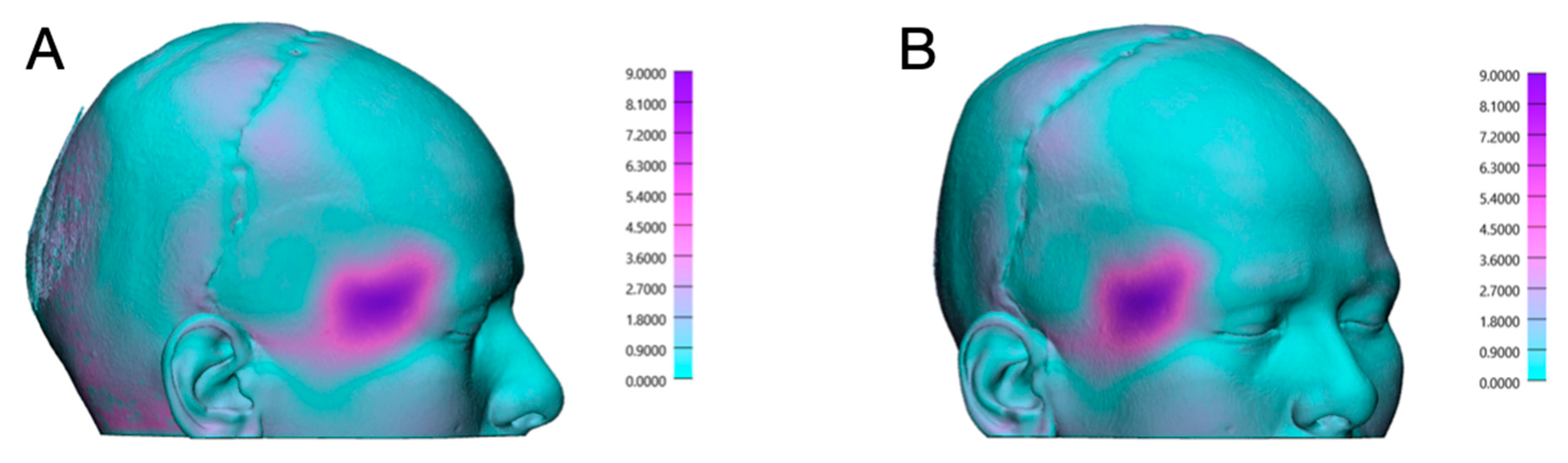
2.2. Surgery
3. Discussion
3.1. PSIs in Oral and Maxillofacial Surgery
3.2. Choice of Material
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laloze, J.; Brie, J.; Chaput, B.; Usseglio, J. Depression after temporal muscle flap: A systematic review of the literature. J. Cranio-Maxillofac. Surg. 2019, 47, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Kameda-Smith, M.M.; Jung, Y.; D’Arco, F.; Hewitt, R.; Aquilina, K.; Jeelani, N.U.O. Pediatric Congenital Anterior Skull Base Encephaloceles and Surgical Management: A Comparative Review of 22 Patients Treated Transnasally, Transcranially, or Combined Approach with a Review of the Literature. Neurosurgery 2024, 95, 859–876. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.D.; Witek, L.; Torroni, A.; Flores, R.L.; Demissie, D.B.; Young, S.; Cronstein, B.N.; Coelho, P.G. The role of 3D printing in treating craniomaxillofacial congenital anomalies. Birth Defects Res. 2018, 110, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Systermans, S.; Cobraiville, E.; Camby, S.; Meyer, C.; Louvrier, A.; Lie, S.A.; Schouman, T.; Siciliano, S.; Beckers, O.; Poulet, V.; et al. An innovative 3D hydroxyapatite patient-specific implant for maxillofacial bone reconstruction: A case series of 13 patients. J. Cranio-Maxillofac. Surg. 2024, 52, 420–431. [Google Scholar] [CrossRef] [PubMed]
- de Bengy-Puyvallée, L.; Poisbleau, D.; Herman, F.; Cobraiville, E.; Giot, J.P.; Galmard, L. Voluminous fronto-parietal osteomas: Guided resection with patient-specific cutting guides and reconstruction with a 3D printed hydroxyapatite implant. Ann. 3D Print. Med. 2025, 17, 100189. [Google Scholar] [CrossRef]
- Verbist, M.; Vandevelde, A.L.; Geusens, J.; Sun, Y.; Shaheen, E.; Willaert, R. Reconstruction of Craniomaxillofacial Bone Defects with 3D-Printed Bioceramic Implants: Scoping Review and Clinical Case Series. J. Clin. Med. 2024, 13, 2805. [Google Scholar] [CrossRef] [PubMed]
- Carbonaro, R.; Ghiringhelli, G.; Amendola, F.; Vaienti, L.; Maduri, R.; Zingaretti, N.; Zanotti, B. Cranioplasty with Hydroxyapatite Implants: A Multidisciplinary Approach of Neurosurgeon and Plastic Surgeons to Improve Surgical Technique and Clinical Outcome. J. Craniofac. Surg. 2024. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Martini, L.; Staffa, G.; Giavaresi, G.; Salamanna, F.; Parrilli, A.; Serchi, E.; Pressato, D.; Arcangeli, E.; Fini, M. Long-term results following cranial hydroxyapatite prosthesis implantation in a large skull defect model. Plast. Reconstr. Surg. 2012, 129, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Jonkergouw, J.; Vijfeijken, S.E.C.M.; Nout, E.; Theys, T.; Casteele, E.V.d.; Folkersma, H.; Depauw, P.R.A.M.; Becking, A.G. Outcome in patient-specific PEEK cranioplasty: A two-center cohort study of 40 implants. J. Cranio-Maxillofac. Surg. 2016, 44, 1266–1272. [Google Scholar] [CrossRef] [PubMed]
- Kauke-Navarro, M.; Knoedler, L.; Knoedler, S.; Deniz, C.; Safi, A.F. Surface modification of PEEK implants for craniofacial reconstruction and aesthetic augmentation—Fiction or reality? Front. Surg. 2024, 11, 1351749. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahed, M.S.; Ali, S.; Abdelwahed, A.S.K.; Aziz, M.M.; Bassiouny, M.S.; Ahmed, M.S. Cranioplasty using patient specific implants Polyether ether ketone versus ultra-high molecular weight polyethylene: A prospective study. J. Cranio-Maxillofac. Surg. 2024, 52, 1299–1310. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Kim, J.Y.; Lew, D.H. Use of rapidly hardening hydroxyapatite cement for facial contouring surgery. J. Craniofac. Surg. 2010, 21, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Wongsirisuwan, M. Customized anterior temporal augmentation for treating anterior temporal hollowing (ATH) by 3D-printed cranioplasty. Neurochirurgie 2024, 70, 101528. [Google Scholar] [CrossRef] [PubMed]
- Gosain, A.K. Hydroxyapatite cement paste cranioplasty for the treatment of temporal hollowing after cranial vault remodeling in a growing child. J. Craniofac. Surg. 1997, 8, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Zaed, I.; Cardia, A.; Stefini, R. From Reparative Surgery to Regenerative Surgery: State of the Art of Porous Hydroxyapatite in Cranioplasty. Int. J. Mol. Sci. 2022, 23, 5434. [Google Scholar] [CrossRef] [PubMed]

| Material | Advantages | Disadvantages | References |
|---|---|---|---|
| Hydroxyapatite (HA) | Excellent biocompatibility; osseointegration; radiopacity similar to bone; low infection rate. | Brittle; limited use in load-bearing areas; higher cost. | [4,6] |
| Polyether ether ketone (PEEK) | Good biocompatibility; radiolucent; strong and durable; customizable. | No osseointegration; higher cost; potential for inflammatory response. | [9,10] |
| Polymethyl methacrylate (PMMA) | Cost-effective; easy intraoperative handling; radiolucent. | High infection risk; no integration with bone; potential fragmentation. | [11] |
| Titanium | High strength; excellent biocompatibility; suitable for load-bearing applications. | Radiographic artifact; thermal conductivity; non-resorbable; difficult to contour. | [9] |
| Autologous fat grafting | Biocompatible; natural contour restoration; minimal rejection risk. | Unpredictable resorption; often requires touch-ups. | [1] |
| Dermal-fat grafts/free flaps | Good tissue match; potentially permanent volume replacement. | Donor site morbidity; longer surgical time; resorption risk. | [1] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifert, L.B.; Aigner, A.; Abazi, S.; Beyer, M.; Zubizarreta-Oteiza, J.; Sharma, N.; Thieringer, F.M. A 3D Printed Hydroxyapatite Implant for Temporal Hollowing Reconstruction: A Patient-Specific Approach. Craniomaxillofac. Trauma Reconstr. 2025, 18, 28. https://doi.org/10.3390/cmtr18020028
Seifert LB, Aigner A, Abazi S, Beyer M, Zubizarreta-Oteiza J, Sharma N, Thieringer FM. A 3D Printed Hydroxyapatite Implant for Temporal Hollowing Reconstruction: A Patient-Specific Approach. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(2):28. https://doi.org/10.3390/cmtr18020028
Chicago/Turabian StyleSeifert, Lukas B., Alexander Aigner, Sead Abazi, Michel Beyer, Jokin Zubizarreta-Oteiza, Neha Sharma, and Florian M. Thieringer. 2025. "A 3D Printed Hydroxyapatite Implant for Temporal Hollowing Reconstruction: A Patient-Specific Approach" Craniomaxillofacial Trauma & Reconstruction 18, no. 2: 28. https://doi.org/10.3390/cmtr18020028
APA StyleSeifert, L. B., Aigner, A., Abazi, S., Beyer, M., Zubizarreta-Oteiza, J., Sharma, N., & Thieringer, F. M. (2025). A 3D Printed Hydroxyapatite Implant for Temporal Hollowing Reconstruction: A Patient-Specific Approach. Craniomaxillofacial Trauma & Reconstruction, 18(2), 28. https://doi.org/10.3390/cmtr18020028







