Comparison of Strengths of Mandibular Angle Fractures Following Different Plate Designs: A Human Cadaver Study
Abstract
Introduction
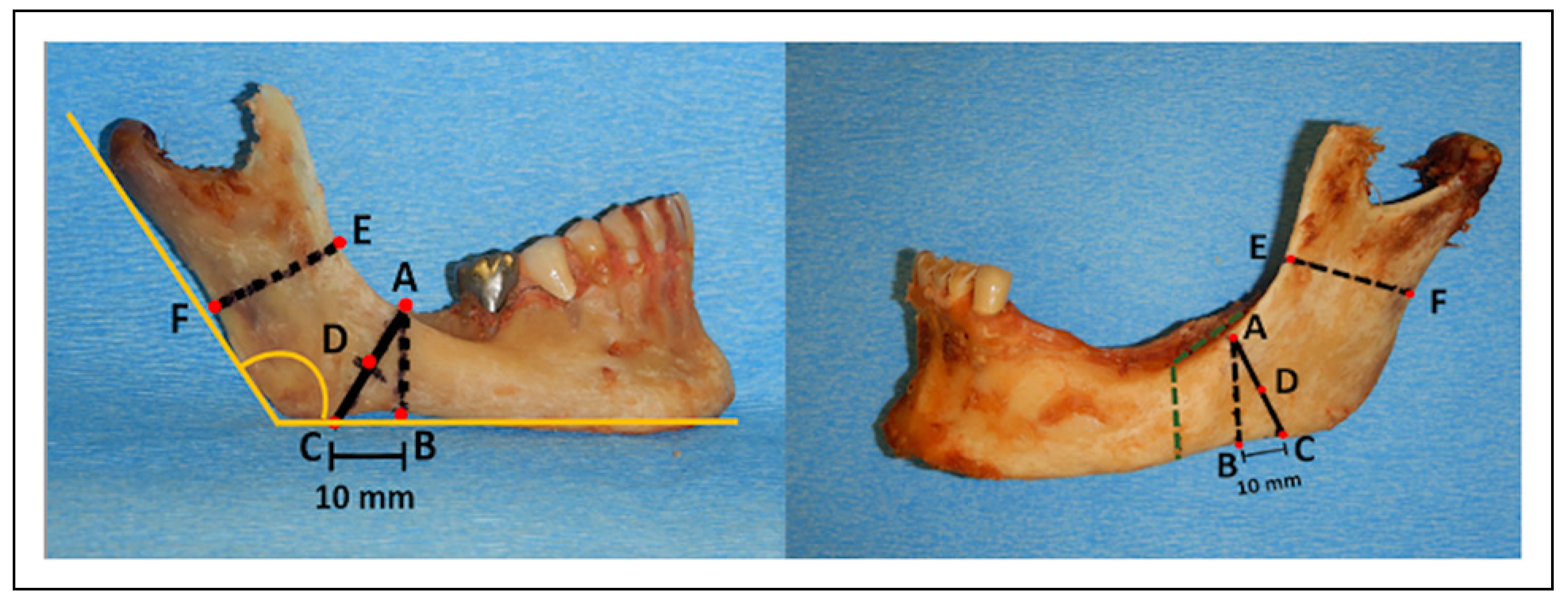
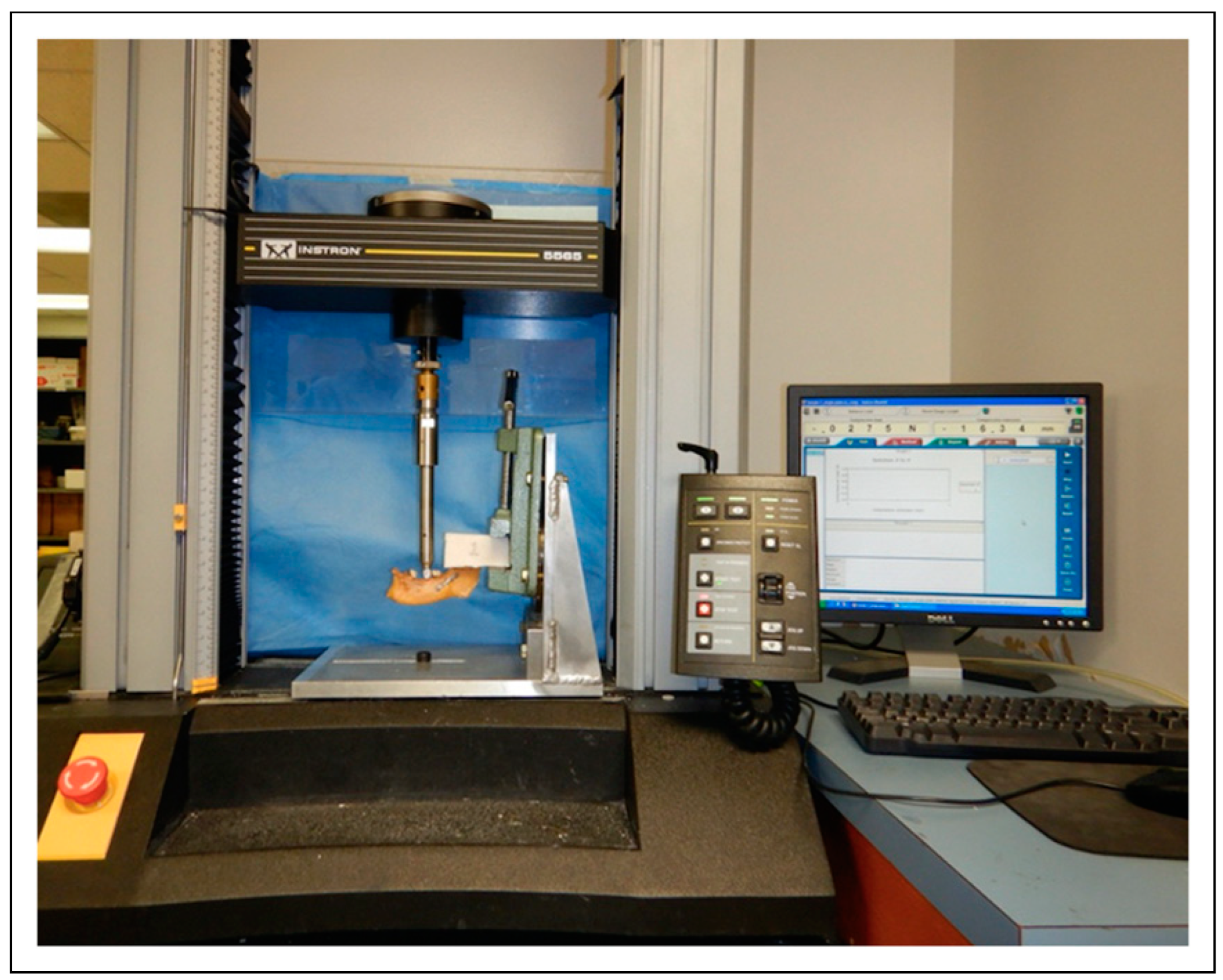
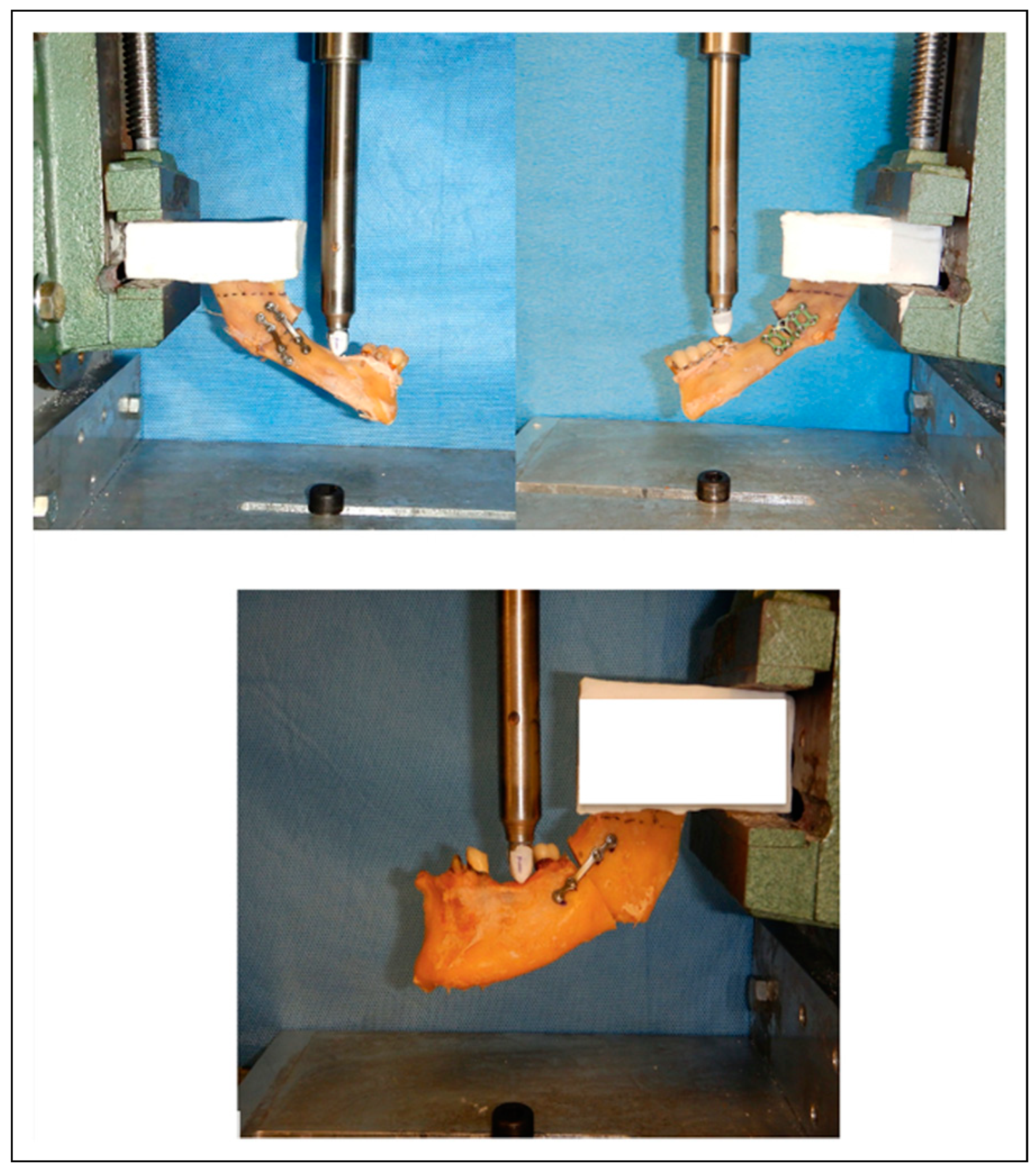
Materials and Methods
Study Design
Variables
Data Collection Methods
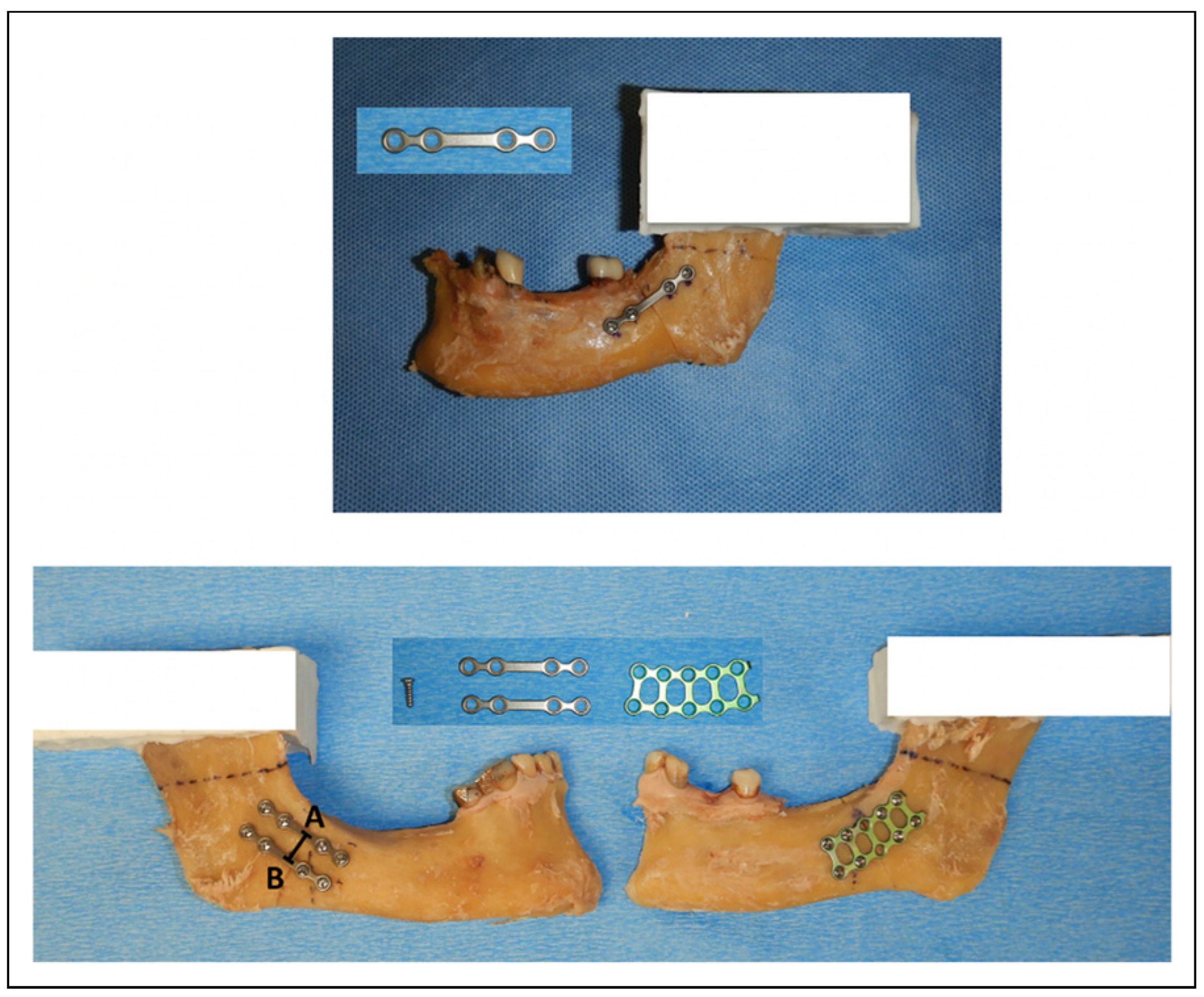
- (1)
- Left hemimandibles (n = 15): one titanium 2.0 mm, 4-hole noncompression plate, 4 monocortical titanium fixation screws with 7.0 mm in length (KLS Martin, Freiburg, Germany) along lateral aspect of the mandible near the external oblique ridge. Following testing, these specimens plate was removed and the 3D plate (as below) was adapted.
- (2)
- Left hemimandibles (n = 15): a 3D curved titanium 2.0 mm, 10-hole noncompression plate, 8 monocortical titanium fixation screws with 7.0 mm in length (KLS Martin, Freiburg, Germany) along the lateral aspect of the mandible. The distance between upper and lower bar of 3D plate was 7.5 mm.
- (3)
- Right hemimandibles (n = 15): two titanium 2.0 mm, 4-hole noncompression plate, 8 monocortical titanium fixation screws with 7.0 mm in length (KLS Martin, Freiburg, Germany) along the upper and lower border of the lateral aspect of the mandible. The distance between midpoint of upper and lower plates were measured twice and averaged.
Statistical Analysis
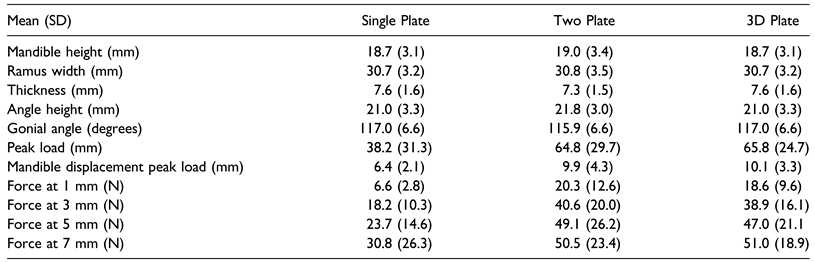
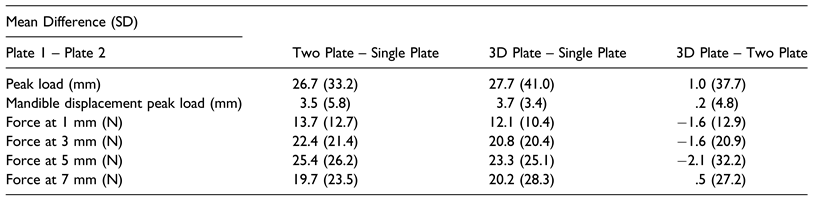
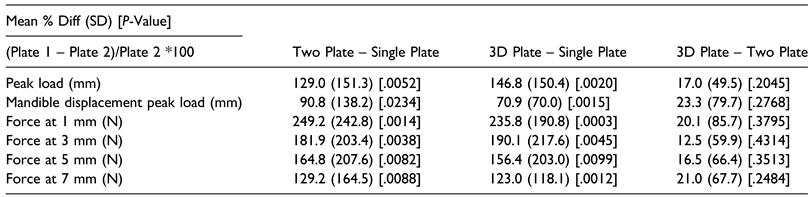
Results
3D Plate vs Single Plate
Single Plate vs Two Plate
Two Plate vs 3D Plate
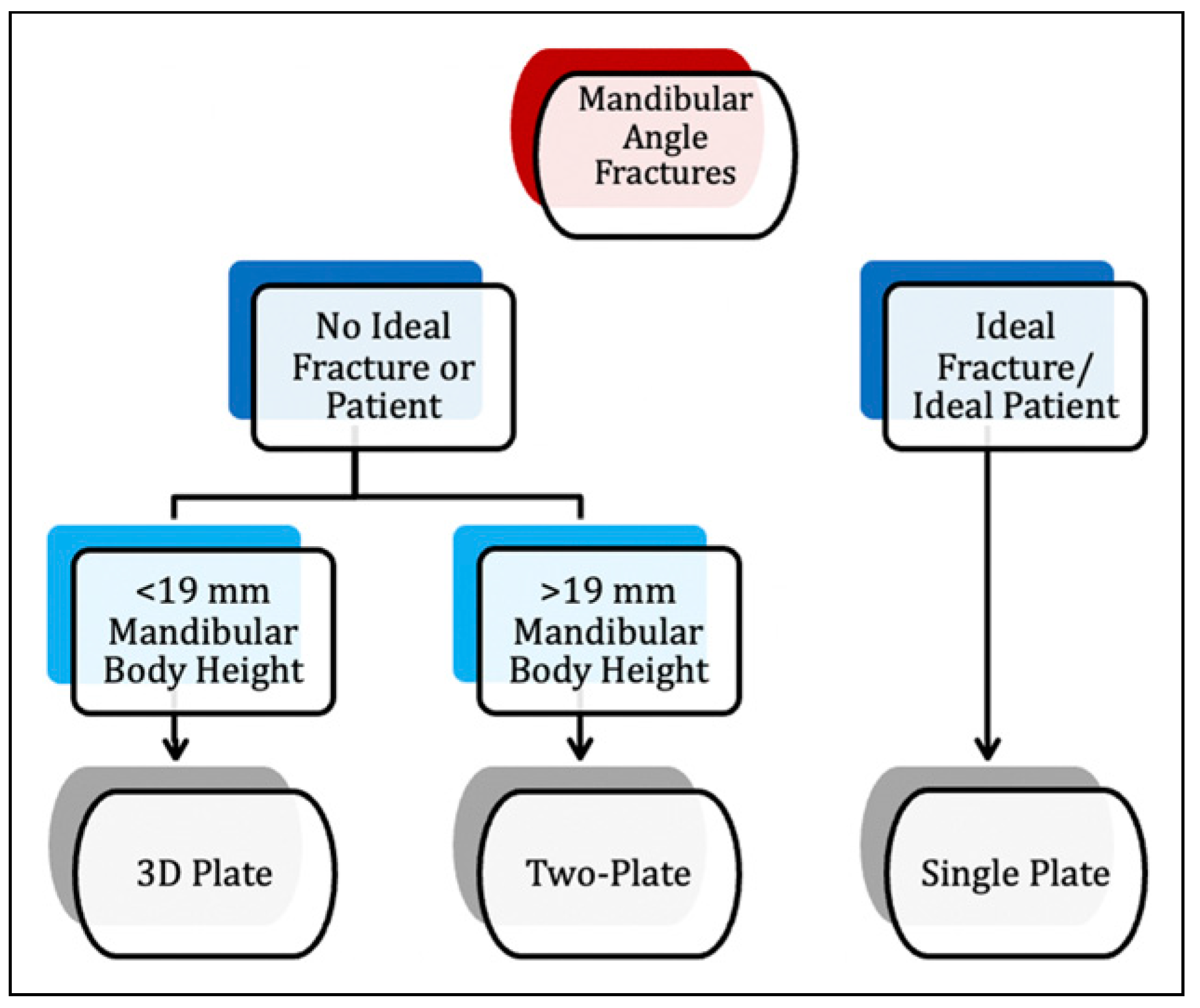
Discussion
3D Plate vs Single Plate
Single Plate vs Two Plate
Two Plate vs 3D Plate
Final
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Afrooz, P.N.; Bykowski, M.R.; James, I.B.; Daniali, L.N.; Clavijo-Alvarez, J.A. The epidemiology of mandibular fractures in the United States, part 1: a review of 13,142 cases from the US National Trauma Data Bank. J Oral Maxillofac Surg. 2015, 73, 2361–2366. [Google Scholar] [PubMed]
- Ellis, E.; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985, 59, 120–129. [Google Scholar]
- King, R.E.; Scianna, J.M.; Petruzzelli, G.J. Mandible fracture patterns: a suburban trauma center experience. Am J Otolaryngol. 2004, 25, 301–307. [Google Scholar]
- Champy, M.; Loddé, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978, 6, 14–21. [Google Scholar] [PubMed]
- Chen, C.L.; Zenga, J.; Patel, R.; Branham, G. Complications and reoperations in mandibular angle fractures. JAMA Facial Plast Surg. 2018, 20, 238–243. [Google Scholar] [CrossRef]
- Fonseca, R.J. Oral and Maxillofacial Surgery; Saunders: Philadelphia, PA, USA, 2000. [Google Scholar]
- Al-Moraissi, E.A.; El-Sharkawy, T.M.; El-Ghareeb, T.I.; Chrcanovic, B.R. Three-dimensional versus standard miniplate fixation in the management of mandibular angle fractures: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2014, 43, 708–716. [Google Scholar]
- Vineeth, K.; Lalitha, R.M.; Prasad, K.; Ranganath, K.; Shwetha, V.; Singh, J. “A comparative evaluation between single non-compression titanium miniplate and three dimensional titanium miniplate in treatment of mandibular angle fracture”--a randomized prospective study. J Craniomaxillofac Surg. 2013, 41, 103–109. [Google Scholar] [PubMed]
- Munante-Cardenas, J.L.; Passeri, L.A. Biomechanical comparison of four mandibular angle fracture fixation techniques. Craniomaxillofac Trauma Reconstr. 2015, 8, 123–128. [Google Scholar]
- Semeghini Guastaldi, F.P.; Hochuli-Vieira, E.; Guastaldi, A.C. Biomechanical study in polyurethane mandibles of different metal plates and internal fixation techniques, employed in mandibular angle fractures. J Craniofac Surg. 2014, 25, 2246–2250. [Google Scholar]
- Pereira-Filho, V.A.; Oliveira, L.F.; Reis, J.M.; Gabrielli, M.A.; Neto, R.S.; Monnazzi, M.S. Evaluation of three different osteosynthesis methods for mandibular angle fractures: vertical load test. J Craniofac Surg. 2016, 27, 1770–1773. [Google Scholar]
- Haug, R.H.; Fattahi, T.T.; Goltz, M. A biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg. 2001, 59, 1199–1210. [Google Scholar] [CrossRef] [PubMed]
- Lyrio, M.C.N.; Monnazzi, M.S.; De Moraes, M.; Hochuli-Vieira, E.; Reis, J.M.N.; Pereira, V.A. Comparison of compressive strength between three different plates for mandibular angle fractures fixation. J Craniomaxillofac Surg. 2014, 42, E277–E280. [Google Scholar]
- Kalfarentzos, E.F.; Deligianni, D.; Mitros, G.; Tyllianakis, M. Biomechanical evaluation of plating techniques for fixing mandibular angle fractures: the introduction of a new 3D plate approach. Oral Maxillofac Surg. 2009, 13, 139–144. [Google Scholar] [PubMed]
- Wittenberg, J.M.; Mukherjee, D.P.; Smith, B.R.; Kruse, R.N. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg. 1997, 26, 68–73. [Google Scholar] [CrossRef]
- Alkan, A.; Celebi, N.; Ozden, B.; Bas, B.; Inal, S. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007, 104, 752–756. [Google Scholar] [CrossRef]
- de Medeiros, R.C.; Sigua, E.A.; Navarro, P.; Olate, S.; Albergaria Barbosa, J.R. In Vitro mechanical analysis of different techniques of internal fixation of combined mandibular angle and body fractures. J Oral Maxillofac Surg. 2016, 74, 778–785. [Google Scholar] [CrossRef]
- Guimond, C.; Johnson, J.V.; Marchena, J.M. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg. 2005, 63, 209–214. [Google Scholar]
- Sawatari, Y.; Marwan, H.; Alotaibi, F.; Christensen, J.; Gannon, J.; Peleg, M. The use of three-dimensional strut plates for the management of mandibular angle fractures: a retrospective analysis of 222 patients. Int J Oral Maxillofac Surg. 2016, 45, 1410–1417. [Google Scholar]
- Al-Moraissi, E.A.; Ellis, E. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2014, 72, 2197–2211. [Google Scholar] [CrossRef]
- Wusiman, P.; Abasi, K.; Maimaitishawuti, D.; Moming, A. Management of mandibular angle fractures using one miniplate or two miniplate fixation system: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2019, 77, 1673.e1. [Google Scholar]
- Liu, Y.; Wei, B.; Li, Y.X.; et al. The 3-dimensional miniplate is more effective than the standard miniplate for the management of mandibular fractures: a meta-analysis. Eur J Med Res. 2017, 14, 22. [Google Scholar] [CrossRef] [PubMed]
- Wusiman, P.; Nie, B.; Li, W.D.; Moming, A. Management of mandibular angle fractures using 3-dimensional or standard miniplates: a systematic review and meta-analysis. J Craniomaxillofac Surg. 2019, 47, 622–628. [Google Scholar] [CrossRef]
- Dayi, E.; Omezli, M.M. Review of biomechanical experimental studies on different plating techniques of mandibular condyle fractures. Ann Maxillofac Surg. 2011, 1, 48–52. [Google Scholar] [PubMed]
- Fedok, F.G.; Van Kooten, D.W.; DeJoseph, L.M.; et al. Plating techniques and plate orientation in repair of mandibular angle fractures: an in vitro study. Laryngoscope. 1998, 108 Pt 1, 1218–1224. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Street, C.C.; Goltz, M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg. 2002, 60, 1319–1326. [Google Scholar] [CrossRef]
- Sittitavornwong, S.; Ashley, D.; Denson, D.; et al. Assessment of the integrity of adult human mandibular angle. Craniomaxillofac Trauma Reconstruction Open. 2019, 3, e18–e23. [Google Scholar]
- Sittitavornwong, S.; Denson, D.; Ashley, D.; Walma, D.C.; Potter, S.; Freind, J. Integrity of a single superior border plate repair in mandibular angle fracture: a novel cadaveric human mandible model. J Oral Maxillofac Surg. 2018, 76, 2611.e1–2611.e8. [Google Scholar]
- Yamaji, M.A.; Oliveira Neto, P.J.; Ribeiro Mde, C.; et al. Evaluation of in vitro resistance of different 2.0-mm titanium plates on the mandibular angle sectioning. Oral Maxillofac Surg. 2015, 19, 65–70. [Google Scholar] [CrossRef]
- Bregagnolo, L.A.; Bertelli, P.F.; Ribeiro, M.C.; Sverzut, C.E.; Trivellato, A.E. Evaluation of in vitro resistance of titanium and resorbable (poly-L-DL-lactic acid) fixation systems on the mandibular angle fracture. Int J Oral Maxillofac Surg. 2011, 40, 316–321. [Google Scholar] [CrossRef]
- Panneerselvam, E.; Prasad, P.J.; Balasubramaniam, S.; Somasundaram, S.; Raja, K.V.; Srinivasan, D. The influence of the mandibular gonial angle on the incidence of mandibular angle fracture-a radiomorphometric study. J Oral Maxillofac Surg. 2017, 75, 153–159. [Google Scholar] [CrossRef]
- Wallner, J.; Reinbacher, K.; Feichtinger, M.; et al. Osteosynthesis using cannulated headless Herbert screws in mandibular angle fracture treatment: a new approach? J Craniomaxillofac Surg. 2017, 45, 526–539. [Google Scholar] [CrossRef] [PubMed]
- Elias, Y.B.; Shilo, D.; Emodi, O.; Noy, D.; Rachmiel, A. The relation between morphometric features and susceptibility to mandibular angle fractures. J Craniofac Surg. 2018, 29, E663–E665. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H.; Kim, K.N.; Kang, H.S. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995, 79, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Kuik, K.; De Ruiter, M.H.T.; De Lange, J.; Hoekema, A. Fixation methods in sagittal split ramus osteotomy: a systematic review on in vitro biomechanical assessments. Int J Oral Maxillofac Surg. 2019, 48, 56–70. [Google Scholar] [CrossRef] [PubMed]
 |
 |
 |
© 2024 by the authors. The Author(s) 2024.
Share and Cite
Squier, B.R.; Kongsong, W.; Cofield, S.S.; Bignault, S.; Sittitavornwong, S. Comparison of Strengths of Mandibular Angle Fractures Following Different Plate Designs: A Human Cadaver Study. Craniomaxillofac. Trauma Reconstr. 2024, 17, 295-305. https://doi.org/10.1177/19433875231225707
Squier BR, Kongsong W, Cofield SS, Bignault S, Sittitavornwong S. Comparison of Strengths of Mandibular Angle Fractures Following Different Plate Designs: A Human Cadaver Study. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):295-305. https://doi.org/10.1177/19433875231225707
Chicago/Turabian StyleSquier, Brendan R., Wichuda Kongsong, Stacey S. Cofield, Samuel Bignault, and Somsak Sittitavornwong. 2024. "Comparison of Strengths of Mandibular Angle Fractures Following Different Plate Designs: A Human Cadaver Study" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 295-305. https://doi.org/10.1177/19433875231225707
APA StyleSquier, B. R., Kongsong, W., Cofield, S. S., Bignault, S., & Sittitavornwong, S. (2024). Comparison of Strengths of Mandibular Angle Fractures Following Different Plate Designs: A Human Cadaver Study. Craniomaxillofacial Trauma & Reconstruction, 17(4), 295-305. https://doi.org/10.1177/19433875231225707




