Introduction
Nonmelanoma skin cancer (NMSC) is the most common malignancy in the US, with an estimated 5 million cases and 3 million people undergoing treatment yearly [
1]. Mohs micrographic surgery (MMS) is a technique dermatologists use to remove skin cancer to maximize clearance of cancer while minimizing damage to surrounding tissue, and, therefore, is often performed on areas such as the face where preservation of healthy skin is extremely important [
2].
Just as the preservation of healthy tissue on the face is imperative, so is the successful reconstruction of these defects, minimizing wound-healing complications and cosmetic or functional deformities. Many patient factors can impact wound healing, including diabetes, obesity, use of steroids/immunomodulators, smoking, and prior radiation [
3]. In the facial reconstructive literature, data conflicts on whether specific medical comorbidities, defects, or surgical factors are associated with postoperative complications.
Some studies have shown that smoking increases complication rates [
4,
5,
6]; however, others have shown that this is only true in patients who smoke heavily around the time of surgery and that rates of necrosis are similar among patients who smoke less than a pack per day, former smokers, and those who never smoked prior to surgery [
7]. It is also unclear whether certain anticoagulants can increase the risk of complications. One study found that clopidogrel in combination with aspirin increased the risk of complications [
8] while other studies found no significant increase in patients who took anticoagulants [
5,
9].
As for defect characteristics, more extensive and deeper defects are clearly associated with more complications [
4,
5,
6,
8], but there is conflicting data over which areas are associated with more complications. Some studies found that nasal defects had the most complications [
9], while others found that periocular defects required the most revisions [
10]. Several studies also found no significant difference between the defect sites [
5,
11]. The use of interpolated flaps, especially in conjunction with cartilage grafts, is associated with increased complications [
4,
5,
11], but it is unclear whether other types of flaps like bilobed and rhombic flaps are also associated with increased complications since one study showed they were [
9] while others have not [
4,
5,
11]. Other factors, like the time from MMS to reconstruction, have also been associated with increased complication rates in some studies [
11] but not in others [
12].
While many studies are published on the safety and efficacy of MMS, few studies examine which patient, defect, or surgical characteristics affect outcomes of the reconstruction and complication rates, and those that do report conflicting results. This study aims to assess patient, defect, and surgical factors associated with complications and revision procedures in patients undergoing post-MMS facial reconstructions to add to this body of literature.
Methods
A retrospective single-institution cohort study of post-MMS facial reconstructions occurring between January 1, 2015 and December 31, 2020 was conducted in the Department of Otolaryngology—Head and Neck Surgery at our institution. The study was approved by our Institutional Review Board. Inclusion criteria included all patients undergoing reconstruction of a facial defect as a result of MMS. MMS could occur either within or outside of the institution. Exclusion criteria included if the date of MMS was unknown, a cancer excision method other than MMS was undertaken (such as wide local excision), and melanoma skin cancer type as those patients did not undergo standard MMS.
Data collected included patient demographics and comorbidities, surgical factors such as defect characteristics and reconstruction details, time from MMS to repair, and postoperative outcomes such as complications, minor and major revisions, and patient- and physician-reported outcomes. Complications documented included infection, hematomas, seromas, and wound healing issues such as skin sloughing, flap dehiscence, and flap necrosis. A minor revision was performed in the office and included procedures such as debridement of skin sloughing, drainage of small seromas, scar revision, and minor flap debulking. Major revisions were procedures that needed to be performed in the operating room such as drainage of a large hematoma, insetting a new flap in the case of flap failure, or more major flap debulking/repositioning that could not be performed in the office.
Statistical analysis included descriptive statistics and multivariable logistical regression to assess patient, defect, and procedural characteristics associated with complications and revisions. To avoid overfitting the regression model [
13], univariate logistic regressions were performed first to identify potentially significant variables (
P < .05). Those variables were then included in a multivariable logistic regression if applicable. All data analysis was performed with IBM SPSS Statistics, version 28 (Armonk, NY).
Results
Included for analysis were 245 defects in 220 patients.
Table 1 summarizes the demographic data. The median age of patients was 66 years (range 24-95). Most patients (65%) were female. Comorbidity data included 54.6% of patients with hypertension, 15.0% with diabetes, 44.6% taking anticoagulation, and 20.9% with another comorbidity. Most patients (55.0%) were never smokers, whereas 32.7% were former smokers, and 12.4% were current smokers. A majority of defects (89.4%) were due to basal cell carcinoma (BCC), and 10.6% were due to squamous cell carcinoma (SCC).
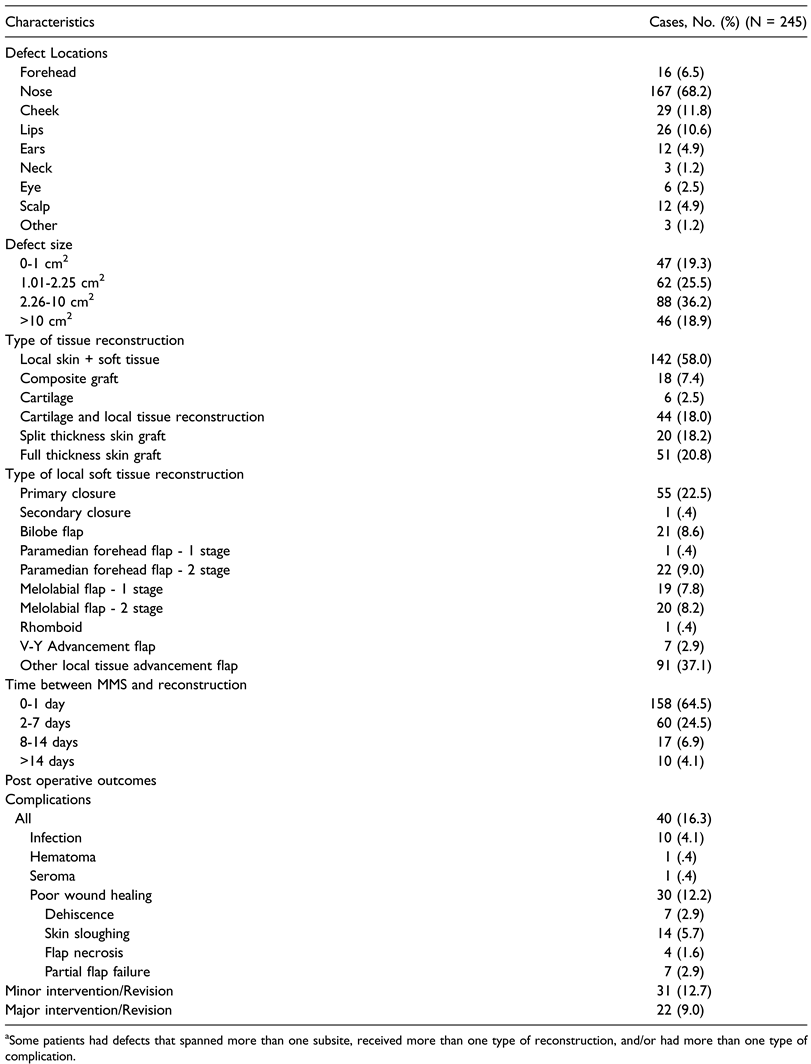
Defect and reconstruction characteristics are summarized in
Table 2. Most cases involved the nose (68.2%). Most defects were between 1.01-2.25 cm
2 (25.5%) or 2.26- 10 cm
2 (36.2%). There were similar numbers of very small 0-1 cm
2 defects (19.3%) and very large >10 cm
2 defects (18.9%). A majority of defects (n = 142, 58.0%) were reconstructed with local soft tissue reconstruction, of which 55 (22.5%) utilized primary closure, 21 (8.6%) utilized bilobed flaps, 22 (9.0%) utilized two-staged paramedian forehead flaps, 19 (7.8%) utilized single-staged melolabial flaps, 20 (8.2%) utilized two-staged melolabial flaps, and 91 (37.1%) utilized other local tissue advancement flap methods. 68 (27.8%) also required cartilage or composite grafting.
Most (64.5%) were reconstructed within a day, while 60 (24.5%) were reconstructed between 2 and 7 days. Much fewer underwent delayed reconstruction, with 17 (6.9%) occurring between 8-14 days and 10 (4.1%) occurring after two weeks. Patients followed up for a median of 127 days, ranging between 0-1329 days. Overall, there were 40 (16.3%) cases with complications, 10 (4.1%) cases of infection, and 30 (12.2%) cases of poor wound healing. Some cases had more than one type of complication. During the follow-up period, 31 (12.7%) minor in-office revisions were performed, and 22 (9.0%) major operating room revisions were performed.
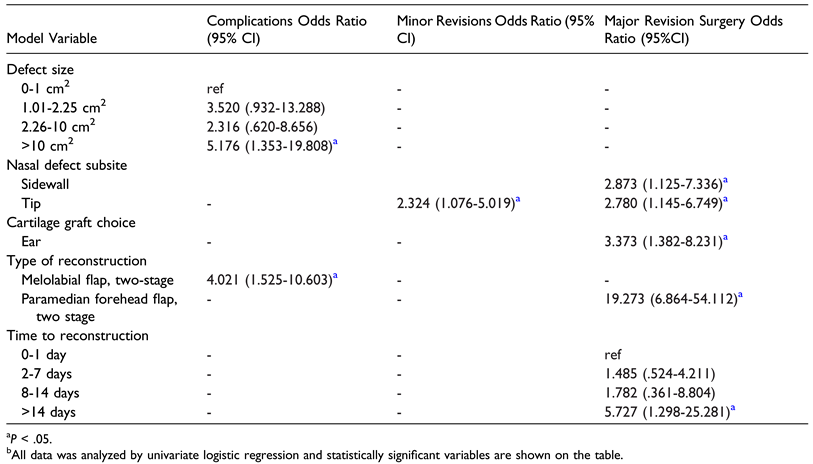
Table 3 summarizes the results of the statistically significant variables after univariate logistic regression analyses for factors associated with complications, minor revisions, and major revisions. All variables from
Table 1 and
Table 2 were assessed, but only statistically significant values were reported. Pooled overall complications were associated with defect size >10 cm
2 (odds ratio (OR) 5.176, 95% confidence interval (CI) 1.353-19.808) and two-staged melolabial flap procedures (OR 4.021, 95% CI 1.525- 10.603). For minor revisions, nasal tip defects were the only statistically significant factor (OR 2.324, 95% CI 1.076- 5.019). Finally, reconstructions occurring >14 days post MMS (OR 5.727, 95% CI 1.298-25.281), nasal sidewall defects (OR 2.873, 95% CI 1.125-7.336), nasal tip defects (OR 2.780, 95% CI 1.145-6.749), ear cartilage grafts (OR 3.373, 95% CI 1.382-8.231), and two-staged paramedian forehead flaps (OR 19.273, 95% CI 6.864-54.112) were associated with major revision surgery.
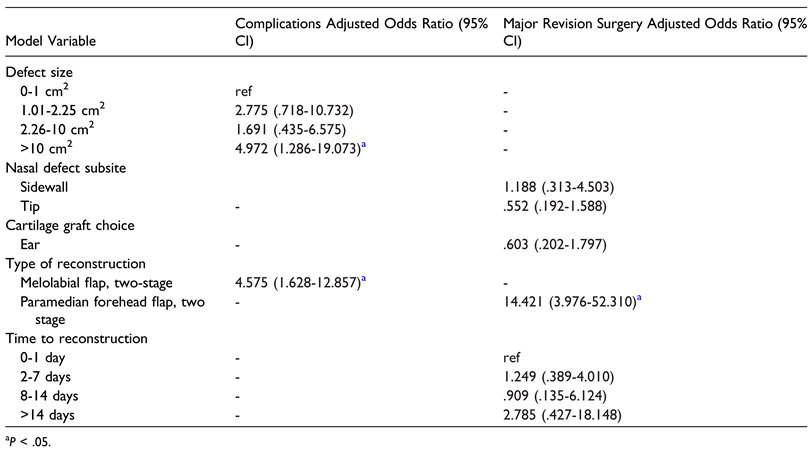
Table 4 displays results of the multivariable logistic regression model used to assess for independent risks factors for complications or major revisions. Both defect size >10 cm
2 (adjusted odds ratio (aOR) 4.972, 95% CI 1.286-19.073) and two-staged melolabial flap procedures (aOR 4.575, 95% CI 1.628-12.857) were independently associated with complications. Major revision surgery was independently associated with two-staged paramedian forehead flaps (aOR 14.421, 95% CI 3.976-52.310).
There was no significant increase in complication rates in patients who had any of the comorbidities collected (hypertension, diabetes, obesity, anticoagulation, immunomodulating drug usage, and history of radiation therapy).
Discussion
Primary outcomes of this study included that about 16% of reconstructions had some form of complication, with 9% requiring major revisions in the operating room and 12.7% requiring minor revisions in the office. These results are in agreement with complication rates reported in the literature spanning 1%–19% [
11]. While many of these more minor complications resolve with time, they may still be a significant concern to patients in this highly visible and cosmetically sensitive area.
Large defects (>10 cm
2) and two-staged melolabial flaps were associated with more complications. All these factors point to greater severity of the defect and complexity of the reconstruction. Interpolated flaps, such as the melolabial flap, are generally utilized in cases of larger defects where local tissue advancement is not feasible or where transfer of better vascularized tissue to the wound bed is needed [
14,
15,
16]. Risks, however, include distal tip necrosis, bulkiness of the flap, and other contour or functional deformities as well as poor scarring of both the recipient and donor site and facial asymmetry [
17,
18,
19].
Of all potential risk factors, only defects of the nasal tip subsite were associated with an increased rate of minor revisions. Factors which may explain this relationship include cosmetic considerations, sensitivity to swelling, and structural complexity. Given the centrality and prominence of the nose on the face, patient expectations regarding postoperative aesthetics and function are often high [
20]. This may increase the likelihood of minor revisions to meet said expectations. Another important factor to consider is that the nasal tip is more prone to edema due to the thin, superficial lymphatic drainage over the musculoaponeurotic layer of the nose compared to other facial areas, as well as thicker skin here [
21]. This swelling can prompt steroid injections or massage to hasten resolution. Tissue tension is also high in the nasal tip area given the limited skin pliability over the septum and cartilaginous crura, making it more susceptible to deviation or asymmetry after reconstruction [
22]. This complex anatomy increases the difficulty of the reconstruction and lends the area to be more susceptible to minor contour irregularities and skin necrosis, necessitating minor revisions.
Major revisions warranting a return to the operating room occurred more frequently in patients with nasal sidewall and tip defects, ear cartilage grafts, delayed timing of reconstruction >14 days post MMS, and two-staged paramedian forehead flaps. The literature has previously established that, while delayed reconstruction beyond five days following MMS can be performed without significant morbidity, there is still an association with increased postoperative complications the longer the delay persists [
11,
12]. These results are supported in this retrospective analysis, as reconstructions occurring over 14 days after MMS were over five times as likely to lead to major revision surgery compared to those which occurred within 0-1 days. Notably, the effect of paramedian forehead flaps was the only statistically significant association with major revision surgery in both univariate and multivariable analysis. Potential reasons for this association include considerable bulk for the flap in its intended donor site, typically the nose, increasing the odds of nasal airway obstruction, or the complex reconstructive technique required for the procedure including multiple staging and a longer healing process. Defects necessitating a two-staged paramedian forehead flap would inherently pose a higher risk of complications due to their size and more extensive reconstruction as well.
Ultimately, the associations established from this study are highly clinically relevant to the practice of facial plastic and reconstructive surgery. They bolster the ability of surgeons to provide informed consent to patients who typically consult surgeons before their skin cancer is excised. Surgeons can use these results to better risk-stratify patients for certain complications and explain the plan for the likely course of postoperative care. With this knowledge, patients can make better decisions about which reconstructive options align with their values and have realistic expectations for their postoperative course. These efforts can increase trust in the physician-patient relationship.
Overall, while this study provides information on which factors are associated with complications and revision surgeries, several patients were lost to follow-up or had very few follow-up visits. Importantly, many outcome variables were not reliably charted, especially regarding patient- reported assessment of outcomes. Other limitations of this study include its retrospective nature as well as only having data from a single academic institution. The limited dataset led to relatively underpowered analyses, which is likely why there were few statistically significant associations in the multivariate models demonstrated.
Future directions include analyzing nasal MMS reconstruction outcomes specifically, as some complications, such as nasal obstruction, are unique to nasal reconstructions. Additionally, patient-reported outcomes are an important measure of aesthetic outcomes, but they were not analyzed in this study since they were rarely included in charts. Future studies may examine how these measures can be reported more consistently and what scales would best assess these outcomes.
Conclusion
Among a cohort of patients undergoing facial reconstruction after Mohs micrographic surgery, the rate of complications was comparable to those reported in the literature; defects larger than 10 cm2 and two-staged melolabial flaps were associated with increased complications. Nasal tip defects were associated with minor revisions. Major revisions were associated with nasal sidewall and tip defects, ear cartilage grafts, delayed reconstruction, and two-staged paramedian forehead flaps. This data provides valuable pre- and post- operative assessment information for patients and physicians. Future studies assessing patient-reported outcomes through validated scales and measures would complement this research.