Clinical Experience with a Less Invasive Surgical Transparotid Approach and Trapezoidal Plate for Neck and Base Condylar Fractures: A Retrospective Study
Abstract
Introduction
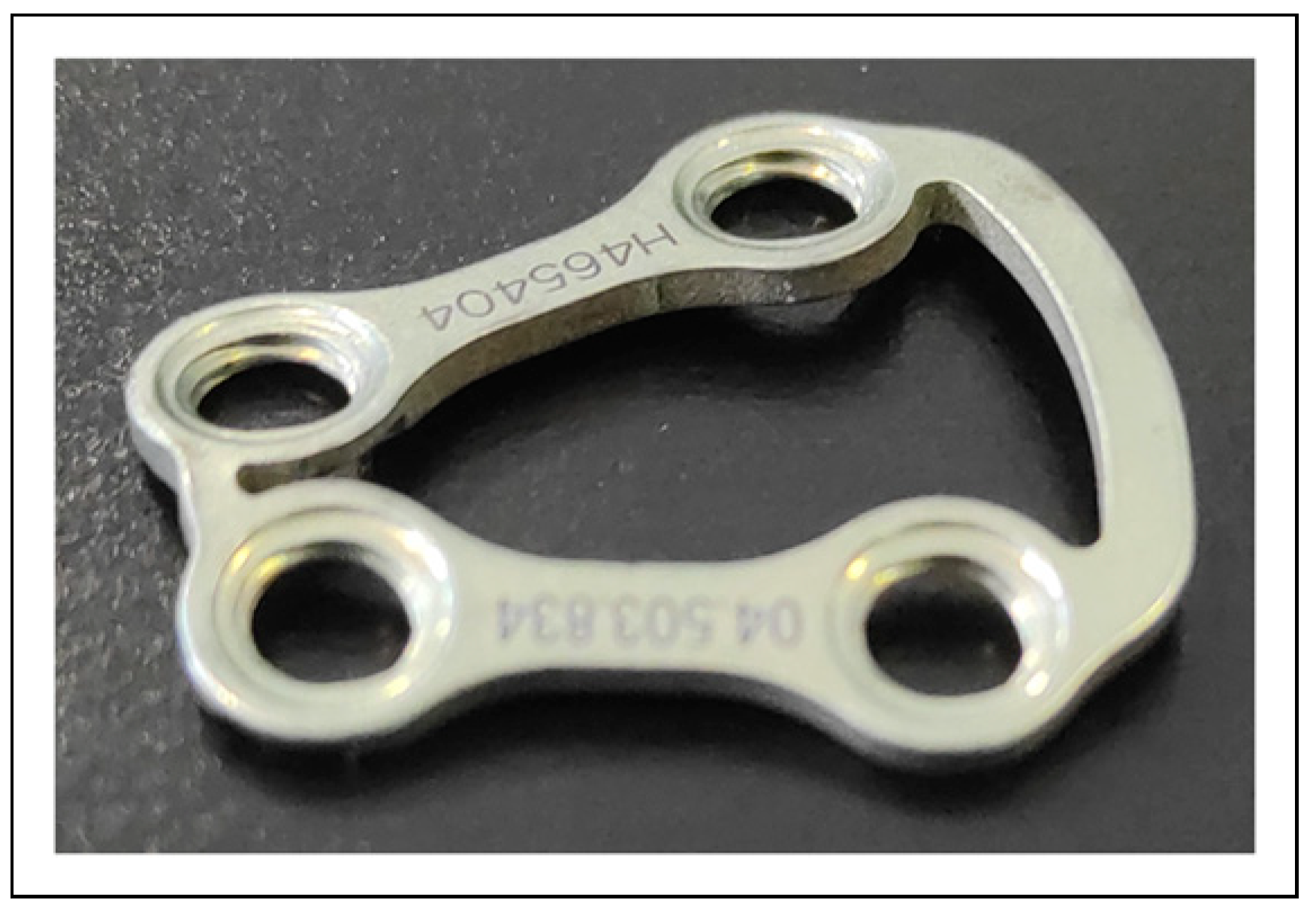
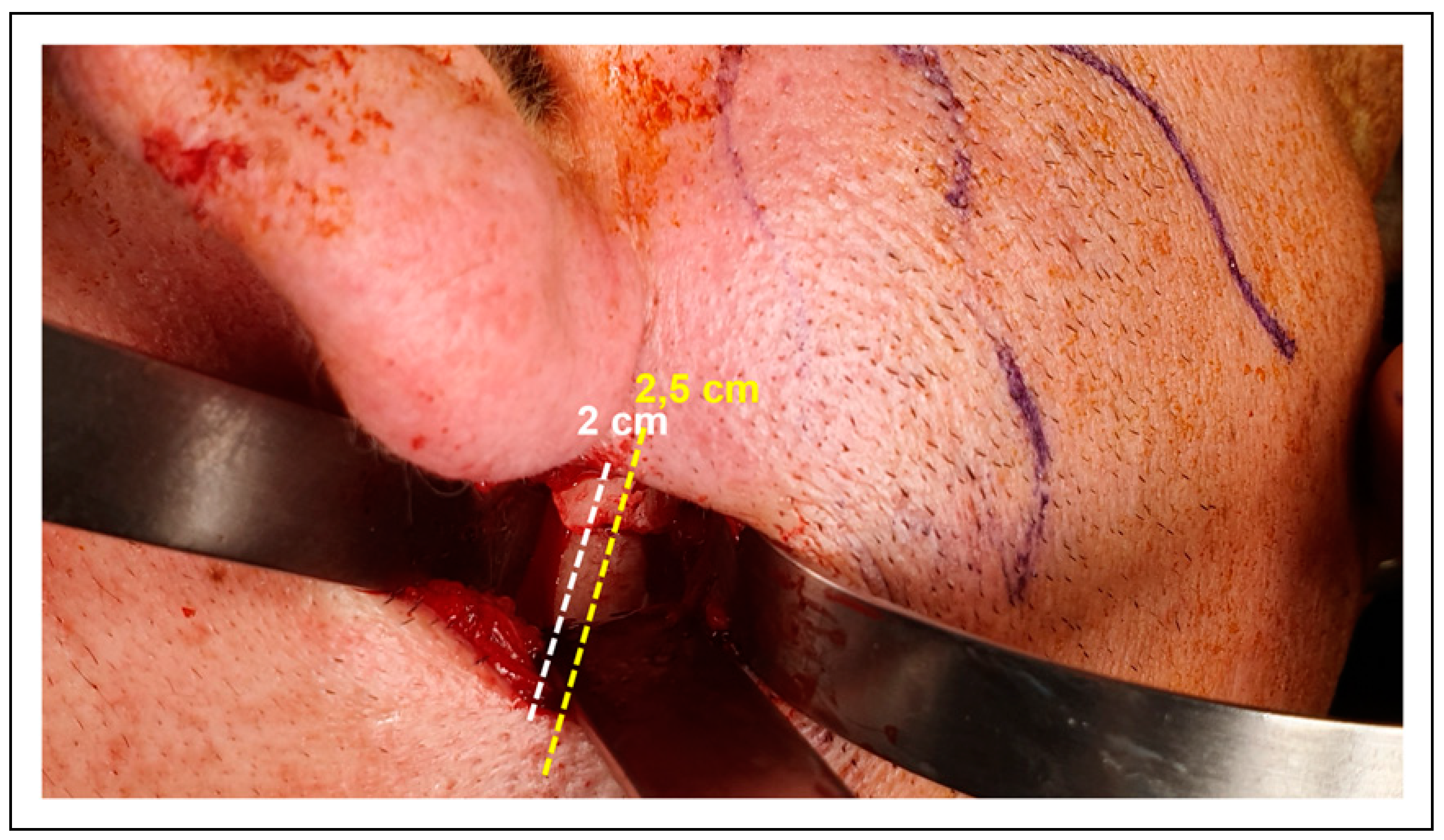
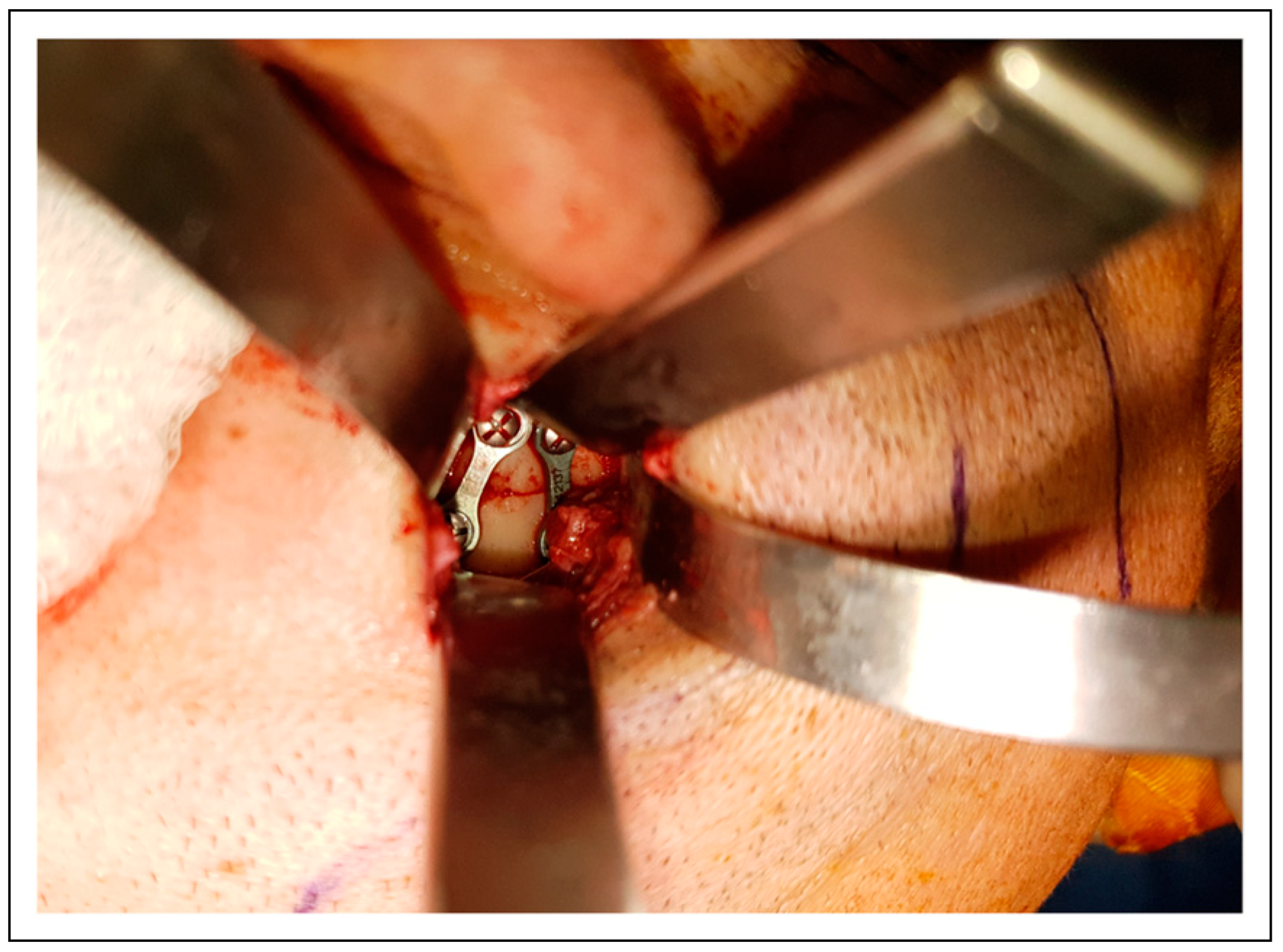
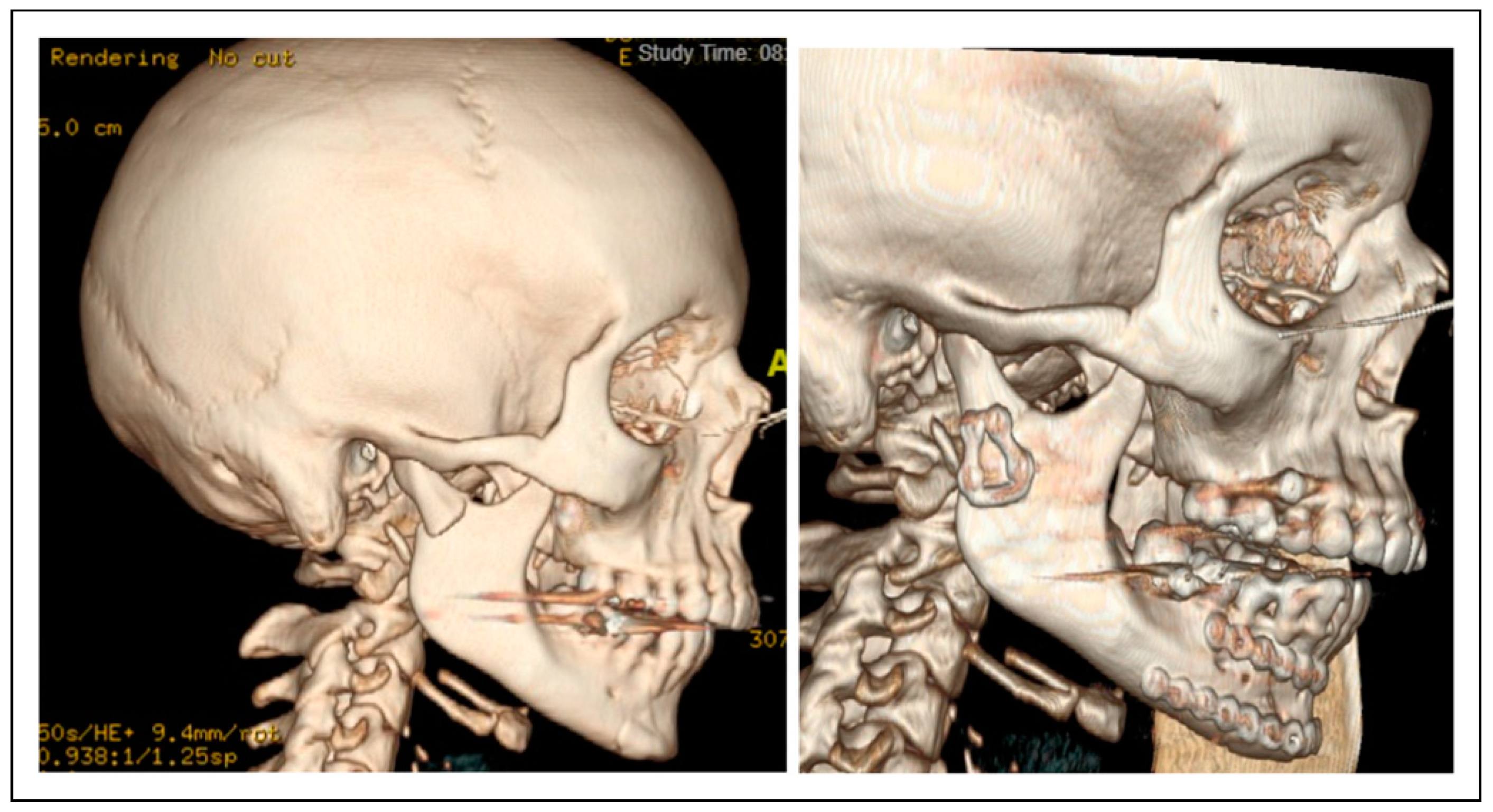
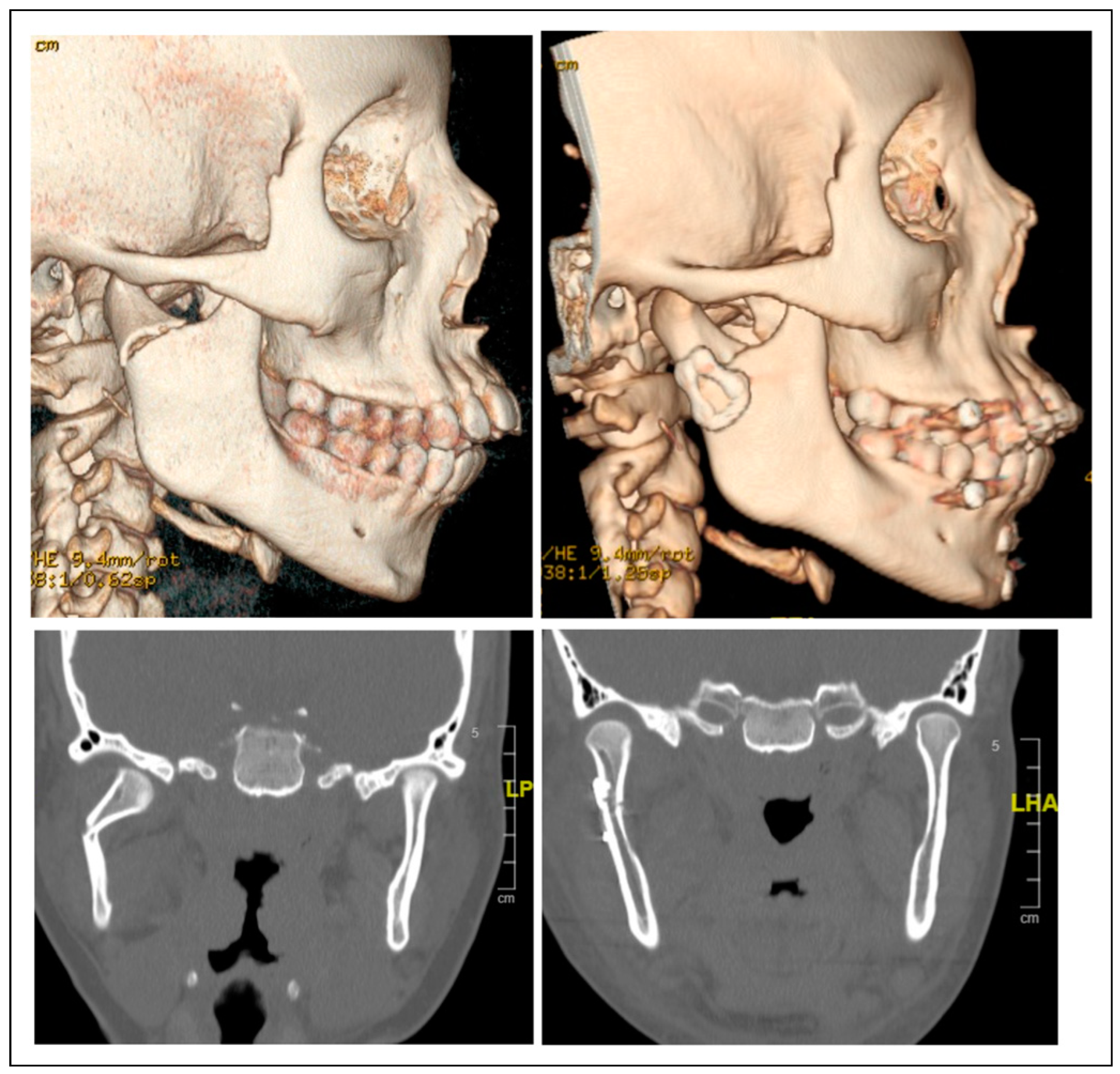
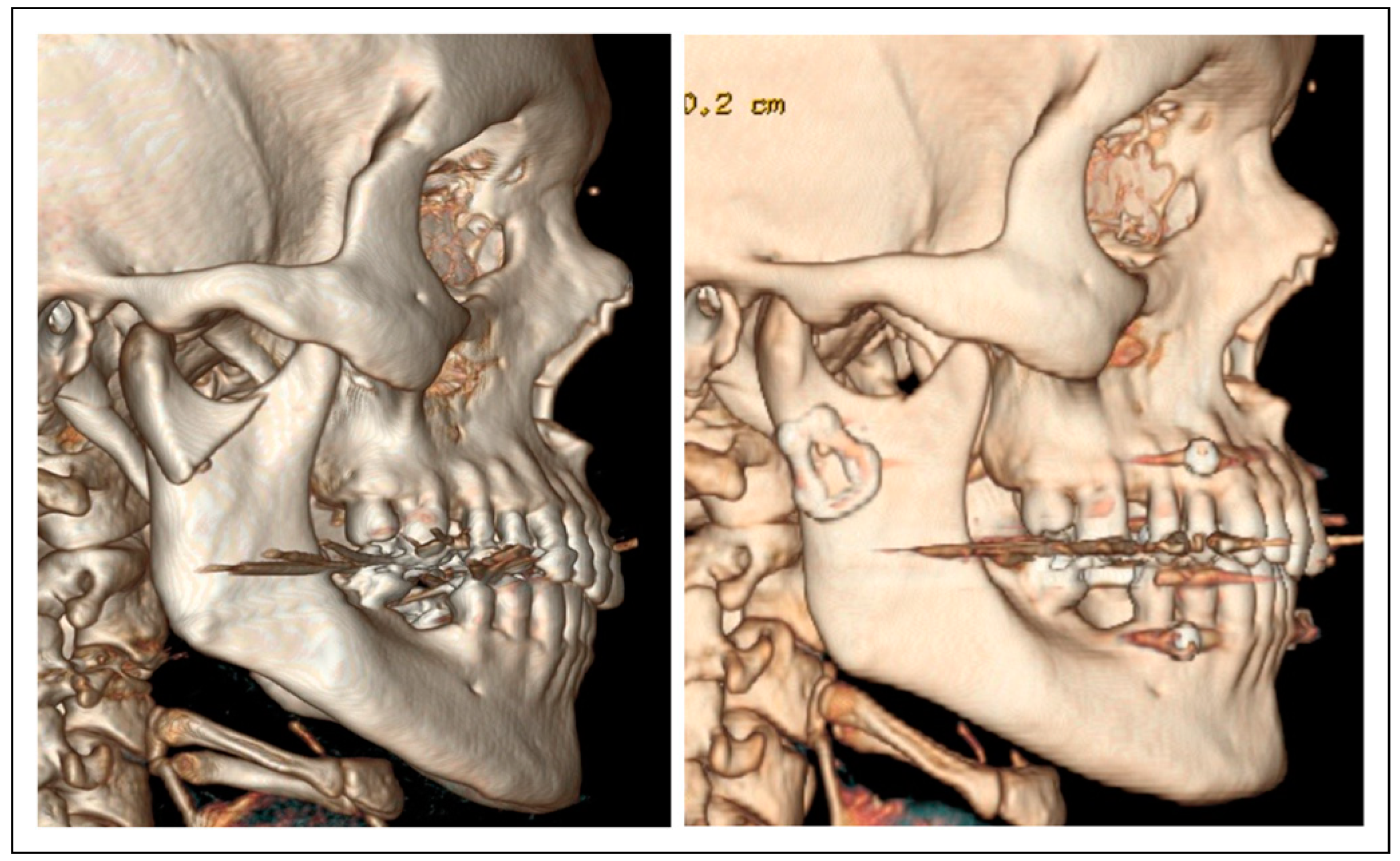
Patients and Methods
Results
Discussion
Conclusions
Funding
Conflicts of Interest
Ethical Statement
References
- Afrooz, P.; Bykowski, M.R.; James, I.; Daniali, L.N.; Clavijo-Alvarez, J.A. The epidemiology of mandibular fractures in the United States, Part 1: a review of 13,142 cases from the US National trauma data bank. J Oral Maxillofac Surg. 2015, 73, 2361–2366. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Cornelius, C.; Rasse, M.; Torre, D.D.; Audige´, L. The comprehensive AOCMF classification system: condylar process fractures—Level 3 Tutorial. Craniomaxillofac Trauma Reconstr. 2014, 7 (Suppl. 1), S44–S58. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Chossegros, C.; Blanc, J.; et al. Position paper from the IBRA Symposium on surgery of the head—The 2nd International Symposium for condylar fracture osteosynthesis, Marseille, France 2012. J Cranio-Maxillo-Fac Surg. 2012, 42, 1234–1249. [Google Scholar] [CrossRef] [PubMed]
- Rozeboom, A.; Dubois, L.; Bos, R.; Spijker, R.; de Lange, J. Open treatment of condylar fractures via extraoral approaches: a review of complications. J Cranio-Maxillo-Fac Surg. 2018, 46, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Lauer, G.; Pradel, W.; Schneider, M.; Eckelt, U. A new 3-dimensional plate for transoral endoscopic-assisted osteosynthesis of condylar neck fractures. J Oral Maxillofac Surg. 2007, 65, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Leonhardt, H.; Franke, A.; Nowak, A.; McLeod, N.; Lauer, G. Clinical experience and results with a rhombic plate for transoral endoscopically-assisted osteosynthesis of fractures of the condylar neck. Br J Oral Maxillofac Surg. 2019, 57, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Lechler, C.; Probst, F.; Cornelius, C.P.; Smolka, W. Open reduction and internal fixation of mandibular condylar base and neck fractures using strut plates. J Oral Maxillofac Surg. 2018, 76, 1494–1503. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, M.; Pant, H.; Singh, M.; Vashistha, A.; Kaur, G. Evaluation of trapezoidal-shaped 3-D plates for internal fixation of mandibular subcondylar fractures in adults. J Oral Biol Craniofac Res. 2015, 5, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Smolka, W.; Liokatis, P.; Cornelius, C.P. Open reduction and internal fixation of unilateral mandibular condylar base and neck fractures using a lambda plate: selection criteria for application. J Oral Maxillofac Surg. 2020, 78, 979–985. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Serhir, L.; Boutemi, P. Experimental evaluation of three osteosynthesis devices used for stabilizing condylar fractures of the mandible. J Cranio-Maxillo-Fac Surg. 2006, 34, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Cortelazzi, R.; Altacera, M.; Turco, M.; Antonicelli, V.; De Benedittis, M. Development and clinical evaluation of MatrixMANDIBLE subcondylar plates system (Synthes). Craniomaxillofac Trauma Reconstr. 2015, 8, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, M.; Bhatt, K.; Yadav, R.; Mandal, J.; Bhutia, O.; Roychoudhury, A. Fixation of subcondylar fractures of the mandible: a randomized clinical trial comparing one trapezoidal plate with two miniplates. Int J Oral Maxillofac Surg. 2021, 50, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Darwich, M.A.; Albogha, M.H.; Abdelmajeed, A.; Darwich, K. Assessment of the biomechanical performance of 5 plating techniques in fixation of mandibular subcondylar fracture using finite element analysis. J Oral Maxillofac Surg. 2016, 74, 794.e1–794.e8. [Google Scholar] [CrossRef] [PubMed]
- Lisiak-Myszke, M.; Marciniak, D.; Bielin´ski, M.; Sobczak, H.; Garbacewicz, Ł.; Drogoszewska, B. Application of finite element analysis in oral and maxillofacial surgery-A literature review. Materials 2020, 13, 3063. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Yamamoto, K.; Sugiura, T.; Horita, S.; Matsusue, Y.; Kirita, T. Computed tomography–based 3-dimensional finite element analyses of various types of plates placed for a virtually reduced unilateral condylar fracture of the mandible of a patient. J Oral Maxillofac Surg. 2017, 75, e1–e1239. [Google Scholar] [CrossRef] [PubMed]
- Shantavasinkul, P.; Akkus, O.; Palomo, J.M.; Baumgaertel, S. Surface strain distribution of orthodontic miniscrews under load. Am J Orthod Dentofac Orthop. 2016, 150, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Zink, S.; Chatelain, B.; Wilk, A. Clinical experience with osteosynthesis of subcondylar fractures of the mandible using TCP plates. J Cranio-Maxillo-Fac Surg. 2008, 36, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Zrounba, H.; Lutz, J.C.; Zink, S.; Wilk, A. Epidemiology and treatment outcome of surgically treated mandibular condyle fractures. A five years retrospective study. J Cranio-Maxillo-Fac Surg. 2014, 42, 879–884. [Google Scholar] [CrossRef] [PubMed]
© 2024 by the author. The Author(s) 2024.
Share and Cite
Cortez Fuentes, C.; Astorga Mori, F.; Valladares Pérez, S.; Gahona Gutiérrez, O.; Sepúlveda Troncoso, G.; Dallaserra Albertini, M.; Vargas Buratovic, J.P. Clinical Experience with a Less Invasive Surgical Transparotid Approach and Trapezoidal Plate for Neck and Base Condylar Fractures: A Retrospective Study. Craniomaxillofac. Trauma Reconstr. 2024, 17, 64. https://doi.org/10.1177/19433875241242938
Cortez Fuentes C, Astorga Mori F, Valladares Pérez S, Gahona Gutiérrez O, Sepúlveda Troncoso G, Dallaserra Albertini M, Vargas Buratovic JP. Clinical Experience with a Less Invasive Surgical Transparotid Approach and Trapezoidal Plate for Neck and Base Condylar Fractures: A Retrospective Study. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):64. https://doi.org/10.1177/19433875241242938
Chicago/Turabian StyleCortez Fuentes, Carlos, Felipe Astorga Mori, Salvador Valladares Pérez, Osvaldo Gahona Gutiérrez, Gerson Sepúlveda Troncoso, Matias Dallaserra Albertini, and Juan Pablo Vargas Buratovic. 2024. "Clinical Experience with a Less Invasive Surgical Transparotid Approach and Trapezoidal Plate for Neck and Base Condylar Fractures: A Retrospective Study" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 64. https://doi.org/10.1177/19433875241242938
APA StyleCortez Fuentes, C., Astorga Mori, F., Valladares Pérez, S., Gahona Gutiérrez, O., Sepúlveda Troncoso, G., Dallaserra Albertini, M., & Vargas Buratovic, J. P. (2024). Clinical Experience with a Less Invasive Surgical Transparotid Approach and Trapezoidal Plate for Neck and Base Condylar Fractures: A Retrospective Study. Craniomaxillofacial Trauma & Reconstruction, 17(4), 64. https://doi.org/10.1177/19433875241242938


