Abstract
Study Design: Retrospective study. Objective: To evaluate patient demographics, surgical management, and complications of orbital and orbitozygomaticomaxillary complex (OZMC) fractures treated at a district hospital in Norway. Methods: The medical records of patients with orbital fractures treated at Aalesund hospital between January 2002 and July 2017 were reviewed. Data on demographics, signs and symptoms, cause of injury, fracture type, associated fractures, surgical management, and complications were collected. Results: A total of 36 patients were reviewed. Males predominated (1:4.1), and fractures occurred mostly in patients 40–59 years (mean 41.8 years). Interpersonal violence was the leading cause of injury, followed by falls. Alcohol was significantly associated with assault caused fractures (P= .001). Orbitozygomaticomaxillary fractures were the most frequent, followed by pure orbital fractures. Clinical findings included periorbital ecchymosis (72%), swelling (56%), sensory nerve dysfunction (53%), diplopia (22%), and restricted eye motility (22%). Commotio cerebri was observed in more than half of our sample and 47% had other facial bone fractures. Referral to tertiary hospitals was done in 19% of the cases. The main treatment done was open reduction and internal fixation (ORIF) (45%). Infection was diagnosed in 17% and managed with antibiotics. Conclusions: The incidence of orbital and OZMC fractures in Moere and Romsdal county in western Norway was low, occurring mainly in males over 40 years. The mechanism of injury was predominantly interpersonal violence and falls. A high proportion of the sample had minor traumatic brain injury (mTBI).
Introduction
Injury is a global problem of public health concern and is one of the main causes of morbidity and mortality, accounting for 10% of the Global Burden of Disease. [1] Trauma to the facial skeleton is common worldwide with varying epidemiology depending on geographic location, socioeconomic, and cultural factors. In developing countries, road traffic accidents are the main cause of facial injuries, while assault/interpersonal violence is the main etiological factor in developed countries. Other causes include falls, sports, and domestic accidents. Facial fractures, in general, are more prevalent in men predominantly in their second and third decades. [2,3,4] Victims of facial injuries can sustain scars, disfigurement, or severe psychological distress. [5] Furthermore, facial injury is associated with high socioeconomic costs due to the increasing costs of hospitalization and time lost to work. [4]
Fractures of the orbit, isolated or in association with other facial fractures, are the most common fractures in severely injured persons accounting for approximately 40% of all facial fractures. [6] The floor of the orbit is extremely thin and therefore easily fractured, accounting for most of the orbital fractures. These fractures may be classified as pure or impure. Pure, also named isolated orbital fractures, involve only the internal orbital walls and impure orbital fractures are those that involve the orbital rim or other facial bones such as the zygoma, maxilla, and ethmoid bone. [7] Pure fractures of the orbital floor or medial wall are usually caused by blunt trauma to the globe, the orbital rim, or both. [8] The contents of the orbit are displaced (blown out) into the maxillary sinus in orbital floor fractures or medially into the ethmoidal sinus in medial wall fractures. The fractured bony tissue may spring back and entrap the periorbital contents (fat and/or muscle tissue) resulting in a trapdoor fracture. This phenomenon causes restricted eye movements and is often encountered in children. [9] Open door fractures or comminuted fractures are the most common type of isolated orbital wall fractures and are characterized by displaced bits of bone. Deranged eye motility may occur in open door fractures due to impingement of periorbital tissues. [10] In orbitozygomaticomaxillary complex (OZMC) fractures, the zygoma is the main site of force absorption. These fractures may have similar affection of the orbital globe support structures and extraocular musculature as pure orbital fractures, but in addition, the clinical features may include midfacial widening, loss of malar projection, and trismus. [11]
Aalesund hospital is the main regional referral hospital in Moere and Romsdal, a county in western Norway. The Department of Oral and Maxillofacial at Aalesund hospital is the main treatment center in the region for the management of orbital fractures and covers a predominantly rural population of approximately 265 000. [12] There are only few previous studies on orbital fractures from Norway, mainly from urban centers. [13,14,15] The aim of this study was to describe the incidence, etiology, age and gender distribution, treatment, and complications of orbital and OZMC fractures managed at Aalesund hospital from January 1, 2002 to July 31, 2017. It is to the best of our knowledge the only study on the management of orbital fractures from rural Norway.
Material and Methods
Data were collected from journals of patients treated for orbital and orbitozygomaticomaxillary fractures at Aalesund hospital in the period January 1, 2002 to July 31, 2017 after approval by the institutional ethical review board and the Regional Ethics Committee (REC central, REK 2018/ 1183). All identified persons (n = 134) were contacted in writing to request their approval to participate in the study.
The cohort of subjects with orbital and orbitozygomaticomaxillary fractures were identified using the International Classification of Diseases version 10 (ICD10). The following data were collected for analysis: type of fracture, personal information (age, gender, occupation), factors associated with the trauma (use of stimulants, etiological mechanism, time and season of injury), management (surgical or conservative treatment, timing of surgery, use of antibiotics, surgical technique, reconstruction material used), and outcome/complications after treatment. Data were analyzed using Stata/SE 16.1 (2021) in collaboration with a statistician (T-Å . M) affiliated with Aalesund hospital.
Results
A total of 134 patients received a written request to participate in this study of whom 41% (55/134) responded positively. Of these 55 responders, 36 had orbital or OZMC fractures. The other 19 were excluded due to fractures not involving the orbit (isolated arch fractures, temporal bone fractures, sinus wall, or other midfacial fracture) or orbital fractures treated elsewhere.
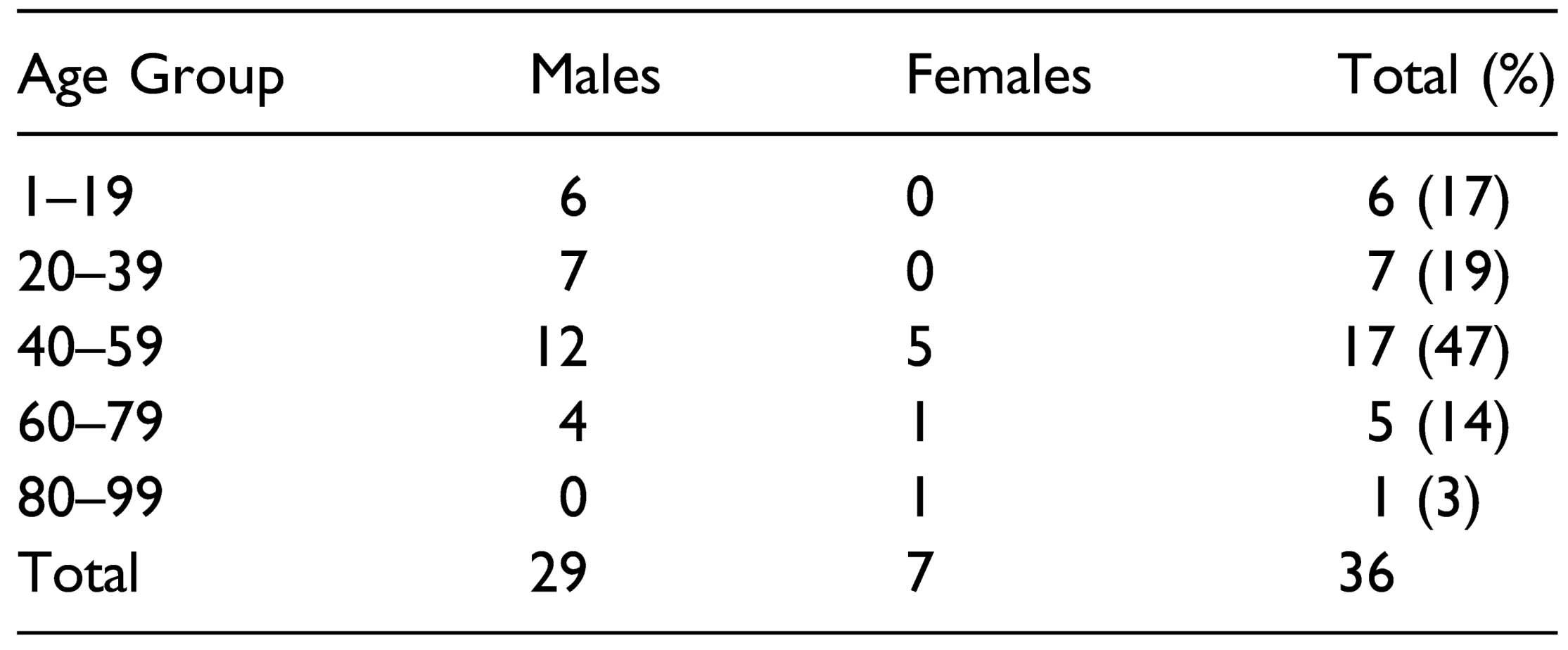
The patients’ ages ranged from 10 to 84 years, with the mean age being 41.8 ± 17.5 years and the median age 44.5 years. The female to male ratio was 1:4.1. Females (56 ± 3.4 years) were significantly older than males (38.4 ± 16.7 years; P < .05). The peak age for orbital and OZMC fractures was 40–59 years accounting for 47% of the study sample (Table 1).

Table 1.
Distribution of Age and Gender in Patients With Orbital and OZMC Fractures.
Most of the patients above 20 years were married or in cohabitation (68%; n =13/19), 2 patients were divorced, and 4 were living alone. Of those with known occupational status (19/36), 58% (n = 11) were employed, 21% (n = 4) were students or trainees, 11% were retired, and 2 patients (11%) were on disability benefits. A history of alcoholism was explicitly noted in only 2 patient journals. In 13 patient records, history of alcohol use was missing. However, alcohol was significantly associated with injury particularly in cases of interpersonal violence (P = .001). The use of recreational drugs was not mentioned in any patient records. Smoking was reported in only 8% (3/36).
Four patients (11%) had depression/anxiety or attentiondeficit-hyperactivity disorder (ADHD). Other comorbidities were mainly cardiovascular diseases in 19% (7/36) or a variety of systemic diseases in 19% (7/36), such as inflammatory bowel disease, asthma, rheumatic disease, migraine, or hypothyroidism. 11% (4/36) had more than one comorbidity. We found no association between orbital or OZMC fractures and any comorbidity.
Slightly over half of our study sample (53%; 19/36) had orbital fractures and 47% (n = 17) had OZMC fractures. Three individuals had bilateral orbital fractures making a total of 39 fractures. The distribution of fractures is shown in Figure 1. We found no significant difference between fractures on the right (n = 15/36) vs the left side (n = 18/36) or any association (P > .05) between fracture type and sex or age.
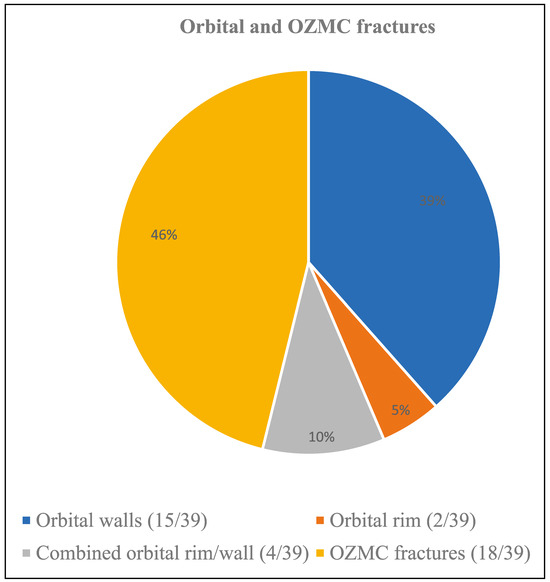
Figure 1.
Distribution of orbital and orbitozygomaticomaxillary complex fractures (n = 39).
86% (31/36) of persons in our study sustained their fractures during non-occupational/leisure activities such as house maintenance, winter outdoor activities, or nightlife. Falls of all kinds as a group (31%, n =11/36) was the most common cause of injury followed by interpersonal violence (28%, n= 10/36) (Figure 2). Falls were further subdivided into falls at ground level (6/36) and falls from heights (5/36). Causes of injury included hit by a tree during logging, a pitchfork penetrating the orbit, hit by own knee during alpine skiing and fall on a sofa.
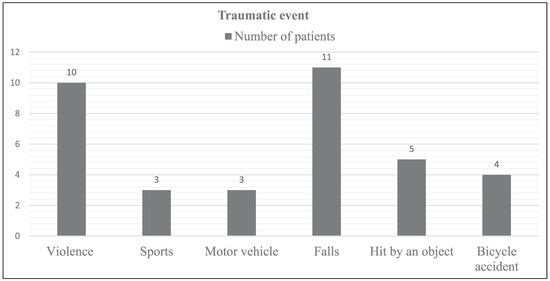
Figure 2.
Distribution of fractures by etiology (n = 36).
There was a significant association between age and etiology (P < .05). Patients being involved in trauma caused by assaults or sports-related accidents were younger (29.9 ± 13.5 years) than those sustaining their injuries after being hit by objects, traffic accidents, or falls (48.5 ± 15.9 years). There was also a significant association between gender and etiology (P < .05), with more men being involved in falls and assaults.
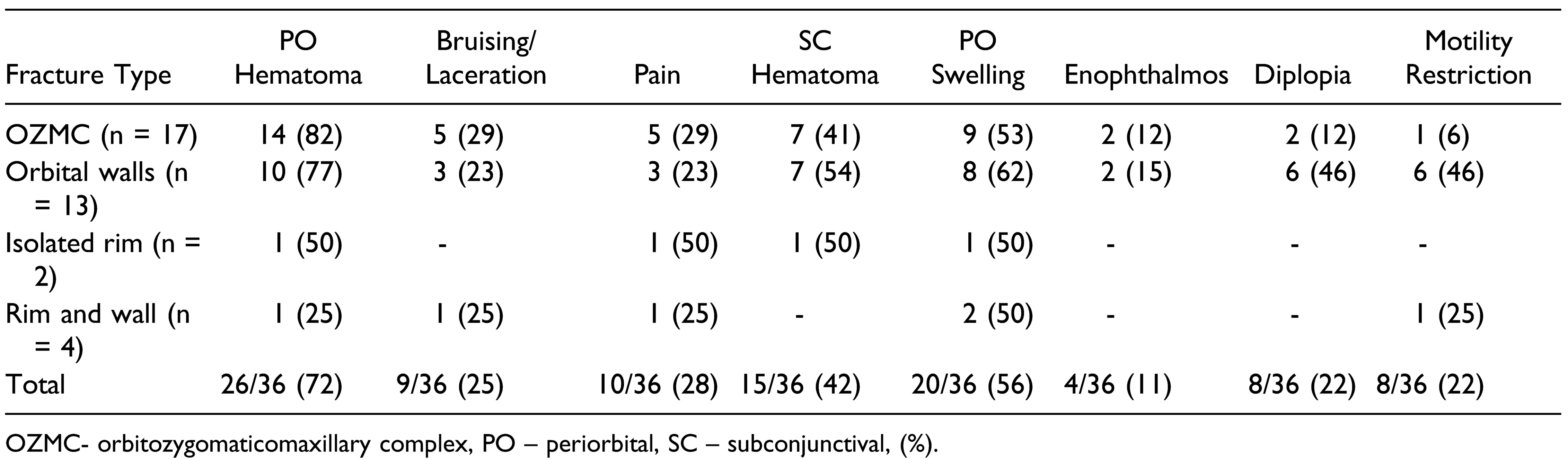
Periorbital hematoma (72%) and swelling (56%) were the most prevalent periorbital clinical findings in our study. Common symptoms and findings are presented in Table 2. Motility restriction was significantly associated with isolated orbital wall fractures (P < .05). Two patients (6%, n = 2/36) had severely deranged eye motility. One of whom suffered permanent loss of vision after a pitchfork eye penetrating injury.

Table 2.
Commonly Registered Findings and Symptoms in the Periorbital Region.
Trismus was recorded in 14% (n = 5/36) of our sample and only in patients with OZMC fractures. Slightly over half of the cases (53%; 19/36) had an infraorbital nerve sensory aberration such as hypoesthesia (95%) or hyperalgesia (5%). Sensory dysfunction was observed in 59% (10/17) of patients with OZMC fractures and 47% (9/19) with orbital fractures. There was no significant association between fracture type and sensory dysfunction. However, there was a significant association between sensory dysfunction and older ages (P < .05), with the mean age being 44.8 ± 15.0 years in the group of patients with sensory dysfunction compared to 33.5 ± 23.0 years in the patients without such injury.
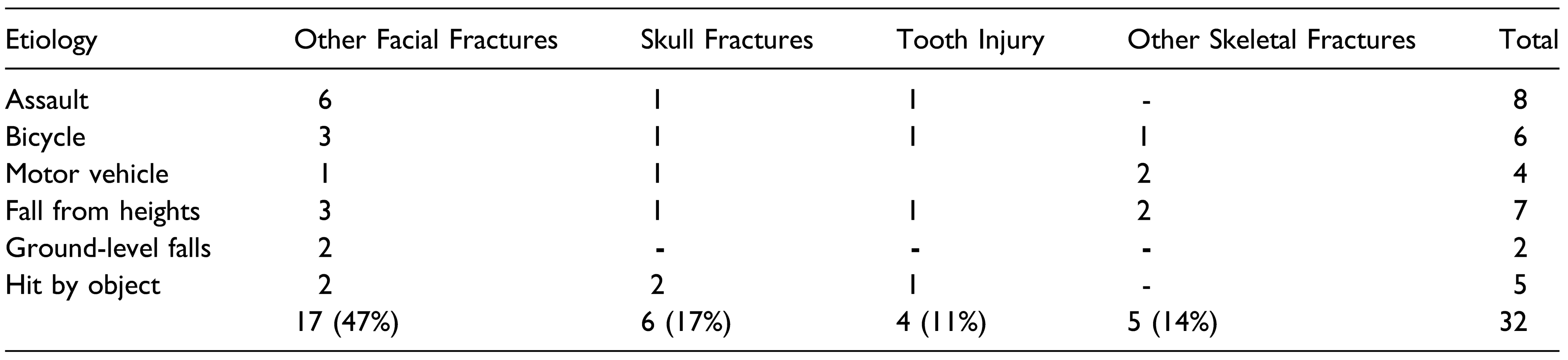
Concussion/commotio cerebri was reported in approximately half of our patients (53%; n = 19/36), with about a quarter (n = 9/36) presenting with either amnesia or loss of consciousness. Loss of consciousness was undetermined or not reported in 28% (n = 10/36). Other head injury related symptoms such as nausea and vomiting (42%; n = 15/36), headache (28%; n 10/36) and rhinorrhea (6%; n = 2/36) were observed in our sample. Six of our patients (17%) had also a skull fracture. Three patients (8%, n = 3/36) had focal brain injuries one of whom had intracerebral hematoma. The 2 others had either subarachnoidal or epidural bleeding. Head CT scans were taken in 61% (n = 22/36) of the cases. Occlusal changes were noticed in 11% (n = 4/36), all of whom had also fractures of either the maxilla or the mandible. Associated fractures related to etiology are shown in Table 3. Almost a third of our sample (31%; 11/36) had other maxillary fractures such as maxillary sinus wall fractures or Le Fort 1 fractures. 11% had frontal sinus fractures (n = 4/36) and 11% (n = 4/36) had mandibular fractures. Of the OZMC fractures 12% (n = 2/17) had also fractures of the coronoid process. Nasal fractures were seen in 19% (n = 7/36) of the patients. Damage to the lacrimal apparatus was seen in 6% (n = 2/36).

Table 3.
Etiology and Associated Fractures.
One patient (3%) had 3 or more fractures besides facial fractures. The severest trauma in our sample occurred after a motorcycle accident which led to intrabdominal bleeding, several fractures of the facial skeleton and of the extremities.
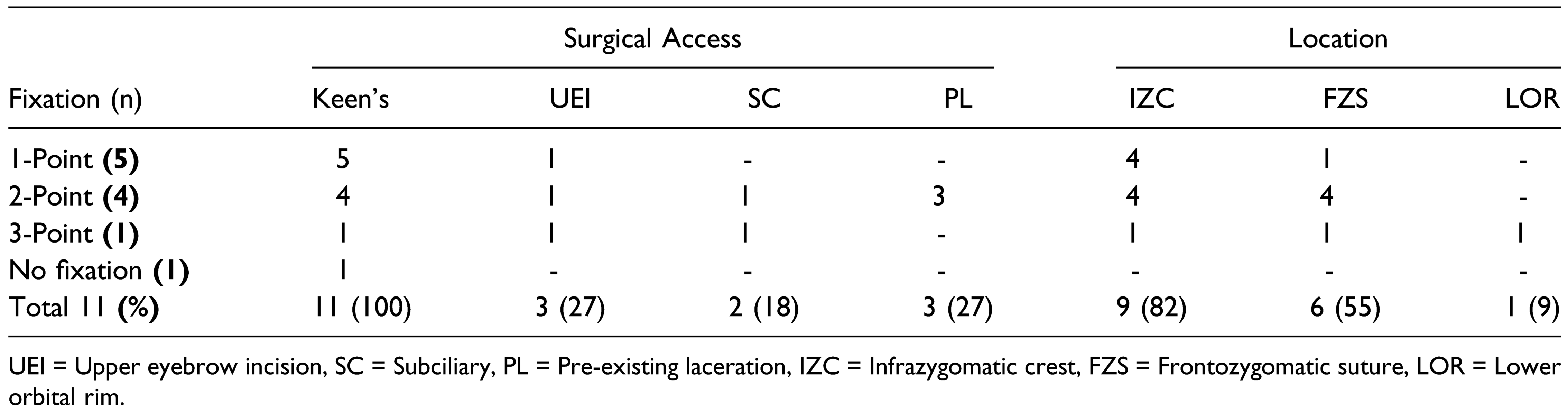
About one-fifth (7/36) of the cohort was referred to a university hospital. One of these patients had urgent orbital decompression due to optic neuritis before referral. It was performed with lateral canthotomy and inferior cantholysis. Because of the severity of the injury the patient lost vision in the left eye. Of the remaining 29 patients managed at Aalesund hospital, 16 had orbital fractures and 13 OZMC fractures. 44% (7/16) of patients with orbital fractures required surgery of whom 4/7 (57%) had orbital reconstruction. Conservative treatment was deemed necessary in more than one third (38%; n = 11/29) of subjects. The rest of the patients underwent open reduction and internal fixation (ORIF). There was no entrapment syndrome or need of orbital reconstruction in any child. The subciliary incision was preferred in all the orbital floor reconstructions. However, a different reconstruction material was used each time, that is, autologous bone fragment, polydioxanone (PDS), porous polyethylene, titanium mesh, or polyethylene titanium implants. Including one patient with OZMC fracture, orbital floor reconstruction was done in 17% (n = 5/29) of the total number of patients managed in Aalesund. 85% (11/13) of our patients with OZMC fractures were operated at Aalesund hospital. All these fractures were unilateral and were treated with open reduction with or without fixation (Table 4). 36% (4/11) of these patients had marked orbital floor dislocation one of whom required orbital floor reconstruction in addition to ORIF. The period from trauma to surgery varied from 4.1 ± 4.2 days for ORIF to 12 ± 3.5 days for orbital wall reconstruction (except one patient with 220 days between trauma and orbital reconstruction due to patient delay in seeking medical treatment).

Table 4.
Treated Orbitozygomaticomaxillary Fractures – Surgical Access, Location, and Number of Fixation Points.
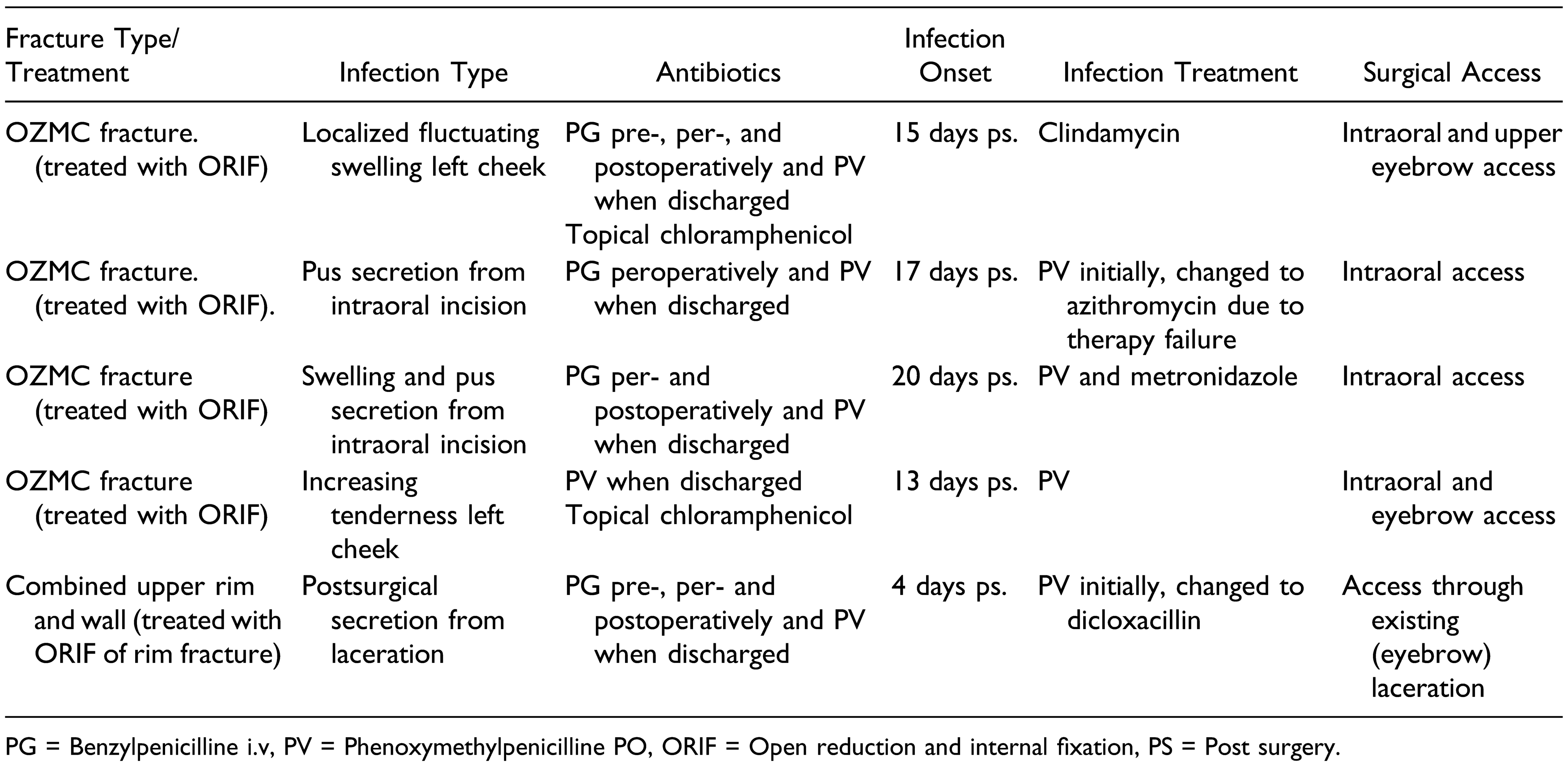
All OZMC operated patients had corticosteroids given peroperatively, usually intravenous (IV) dexamethasone 8– 12 mg or intramuscular betamethasone 12 mg. Systemic antibiotics were used in a prophylactic manner in 66% (n = 19/29) of our sample, and in 94% (n =17/18) of the surgically managed patients. The only topical antibiotic given was chloramphenicol eye ointment or drops. A total number of 5 patients developed postoperative infection (28%; 5/18) and required either per oral (PO) or IV antibiotic treatment (Table 5).

Table 5.
Overview of Postoperative Infections.
The mean number of controls after discharge from hospital was 2.3 ± 2.0 in general, and 3 ± 1.5 for operated patients. Patients operated for OZMC fractures with ORIF were followed up for the longest time after surgery (275.9 ± 363.8 days) with a median of 103, range 13–1021, mainly because of postoperative infection and complaints related to osteosynthesis materials. The period of follow-up was dictated by posttraumatic patient complaints.
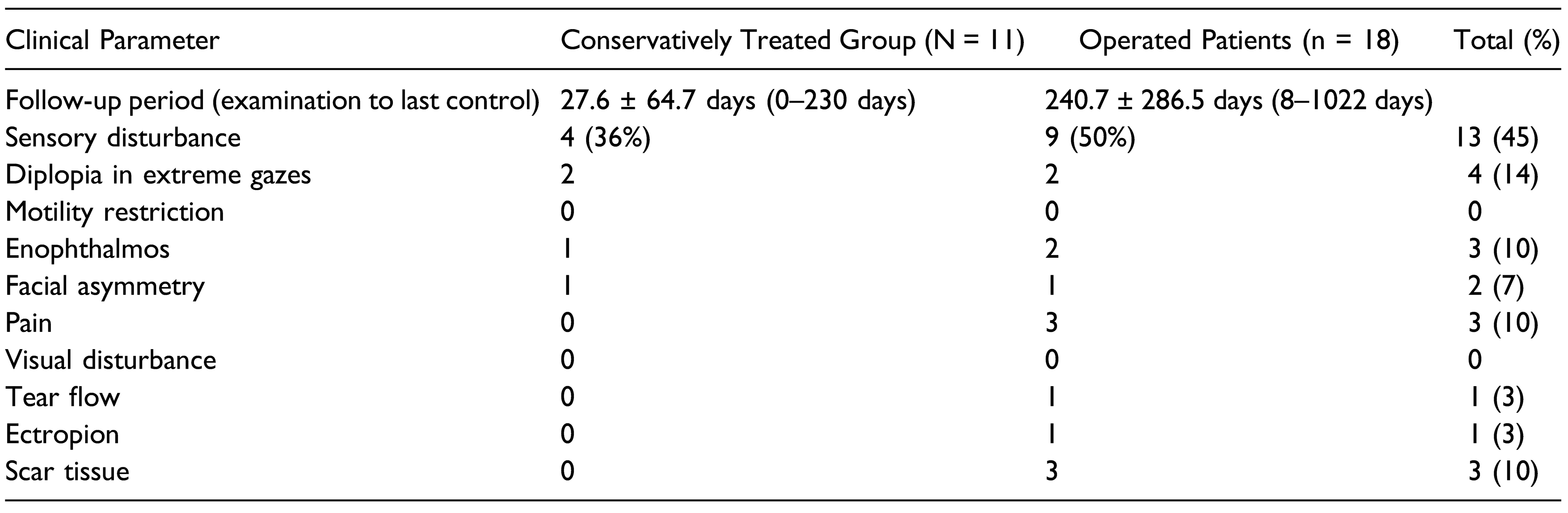
Complications due to trauma and/or surgery as registered at the last control are summarized in Table 6. Sensory disturbances were reported in 13/29 (45%) patients. One of these patients had reconstruction of the lacrimal apparatus and another had removal of osteosynthesis material due to discomfort.

Table 6.
Overview of Follow-Up and Residual Symptoms/Findings at Final Consultation.
Discussion
This retrospective study showed a low incidence of about 2.5 cases/year of orbital and OZMC fractures managed at Aalesund hospital, which covers a predominantly rural population. This is much lower than in urban areas in Norway [16,17] and other parts of the world which show incidences in the range of 40–200 patients per year. [6,18,19] There are few studies on maxillofacial trauma from rural regions globally [20,21,22] and this study, to the best of our knowledge, is the first report on orbital fractures from rural Norway. Differences in incidence and pattern of maxillofacial trauma between rural and urban centers are important in the planning and execution of health and training policies. In our study, males were significantly younger and 4 times more likely to sustain orbital or OZMC fractures than females. This is in concordance with previous reports on maxillofacial fractures. [2,6,18] However, the peak age (40– 60 years) for orbital fractures in our study was much higher than in other studies. [6,7,18] This may be explained by demographic differences in our county compared to urban centers. [23] Furthermore, etiological factors in maxillofacial trauma such as interpersonal violence, motor vehicle accidents and falls often follow age group-specific trends. [6] Our results indicate that orbital fractures in our region are mostly related to falls or interpersonal violence, and that OZMC fractures are the most common followed by pure orbital fractures. An involvement of OZMC in about half of our patients is similar to other studies. [24,25] Falls and interpersonal violence were almost equally involved in the mechanism of injury. The involvement of motor vehicle accidents as an etiological factor was lower than in other studies. [6,26,27] In general, fractures caused by high-energy trauma were few and may be explained by the under representation of young adults in the county and by the fact that these injuries are often directly transported to a university hospital.
Most of our patients sustained their injuries during leisure/non-occupational related activities mainly as a result of interpersonal violence or falls. Work related accidents are generally not a major factor in maxillofacial injuries. [7,18] Our rate of assault-related orbital and zygomaticomaxillary was lower than in the capital city. [2,28] This may be related to demographic differences between the capital and our county. [23] Falls as a reason for trauma is higher in our study compared to other reports [7,18] and may be explained by a higher proportion of older patient who are more prone to falls.
About half of our patients had posttraumatic sensory dysfunction of the infraorbital nerve. We did not find any association between fracture type and sensory dysfunction. However, patients with sensory dysfunction were significantly older. This may be due to the reduced potential for regeneration/healing with age. A previous study found more hypoesthesia in adult than pediatric patients with orbital trapdoor fractures and suggested that this may be related to thinner soft tissue in the malar region and an increased vulnerability to direct contusion of the infraorbital nerve bundle. [9]
An association with other facial fractures in almost half of our sample is higher than other studies. [6,18,27] This may again be age related since our patients were generally older and thus more likely to sustain multiple injuries due to structural and functional alterations with aging. All the nonhead/facial fractures were sustained after high altitude falls or transport-related trauma and agrees with previous studies. [3,6] There were few serious intracranial injuries in our material. However, at least half of the patients had minor traumatic brain injury (mTBI), including commotio cerebri. Diagnosis and management of mild traumatic brain injury is of great importance, especially in patients with premorbid psychological factors. Both posttraumatic stress disorder (PTSD) and major depressive disorders (MDD) may be exacerbated by mild traumatic brain injury. [29] The mechanisms for this mental health sequel of mTBI is not clear, but may be due to mechanical damage or neuroinflammation. [29] Intracranial injury has been reported in patients with orbital wall fractures and was associated with ground-level falls, higher age, superior orbital wall, and frontal bone fractures. [30] Therefore, the need for a head CT should be seriously considered in persons who have sustained orbital and orbitozygomaticomaxillary fractures.
In our study, alcohol was associated with trauma especially caused by interpersonal violence. Previous studies from Norway have shown a strong association between alcohol and facial trauma. [17,31] Alcohol intoxication leads to inflated confidence, faulty judgment, poor coordination, and aggressive behavior. [32] Therefore, persons under the influence of alcohol are more prone to assaults, traffic accidents and falls, which may cause severe and often multiple facial skeleton fractures.
In this study, the orbital floor was only reconstructed if there was dislocation with significant enophthalmos or muscle impingement with affection of eye motility. A different orbital floor reconstruction material was used each time. The diversity in orbital floor reconstruction materials may reflect the long-time span of the study. We recommend the use of one or a limited number of materials so that surgeons may acquire proficiency and experience in the material(s) of choice. The timing of surgery for orbital reconstruction was 10–16 days post trauma, except for patients with concomitant OZMC fractures. A time of at least 14 days is recommended before a decision to operate is taken because of periorbital swelling and hemorrhage possibly masking an enophthalmos, or edema giving temporarily muscle dysfunction and motility deficits. [33] Waiting longer than 2 weeks before surgery may lead to a higher risk of posttraumatic fibrotic tissue. [33] However, many authors propose that observation and late surgery is not always associated with a bad outcome, and it has been recommended that orbital fractures without acute indications or early enophthalmos may be observed and surgery performed later if needed. [34,35,36]
The main patient complaints after management were sensory dysfunction and diplopia in extreme gazes. Reoperation was done in about one-tenth of the sample because of discomfort related to osteosynthetic materials and lacrimal apparatus damage. Sensory dysfunction is the most disturbing impairment after zygomatic trauma. [37] Hypoesthesia of the infraorbital nerve may remain for up to 1 year after orbital wall trauma. [38] There were more persisting nerve disturbances following operative compared to nonsurgical therapies for persons with orbital blowout fractures and midfacial fractures. [38,39] In our retrospective study the recording of posttraumatic symptoms was not consistent and the short time of follow-up may explain a higher residual sensory dysfunction in the non-surgical group.
The limitations of this study include a small sample size, its retrospective nature with non-standardized recording and follow-up of patients. The necessity of obtaining written consent from all identified patients before inclusion led to loss of patients. However, although our sample is small, we believe it is representative and contributes information on orbital and orbitozygomaticomaxillary from a rural part of Norway. In conclusion, the incidence of these fractures in Moere and Romsdal county in western Norway was very low occurring mainly in males over 40 years. The mechanism of injury was predominantly interpersonal violence and falls. Alcohol was strongly associated with fractures caused by assaults. A high proportion of our sample had mTBI. Clinicians should be aware of this, particularly in persons with previous psychological disorders.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
We thank Dr Tor Åge Myklebust for his support on data analysis. We thank the Department of Maxillofacial Surgery at Aalesund hospital for allowing us to assess the patient material.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Note
| 1 | Present address of Ingvild Årøen Lein is The Dept. of Oral and Maxillofacial Surgery, Clinic of Ear-Nose-Throat, Eye and Maxillofacial Surgery, St. Olavs Hospital, Trondheim University Hospital, Norway. |
References
- Kassebaum, N.J.; Arora, M.; Barber, R.M.; et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016, 388, 1603–1658. [Google Scholar]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. European maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Craniomaxillofac Surg. 2015, 43, 62–70. [Google Scholar] [PubMed]
- Lee, K.H.; Qiu, M. Characteristics of alcohol-related facial fractures. J Oral Maxillofac Surg. 2017, 75, 786.e1–786e7. [Google Scholar] [CrossRef]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011, 69, 2613–2618. [Google Scholar]
- Joy, D.; Probert, R.; Bisson, J.I.; Shepherd, J.P. Posttraumatic stress reactions after injury. J Trauma 2000, 48, 490–494. [Google Scholar] [PubMed]
- Ellis E 3rd el-Attar, A.; Moos, K.F. An analysis of 2, 067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg. 1985, 43, 417–428. [Google Scholar]
- Bartoli, D.; Fadda, M.T.; Battisti, A.; et al. Retrospective analysis of 301 patients with orbital floor fracture. J Craniomaxillofac Surg. 2015, 43, 244–247. [Google Scholar] [CrossRef]
- Nagasao, T.; Miyamoto, J.; Jiang, H.; Tamaki, T.; Kaneko, T. Interaction of hydraulic and buckling mechanisms in blowout fractures. Ann Plast Surg. 2010, 64, 471–476. [Google Scholar]
- Takahashi, Y.; Sabundayo, M.S.; Miyazaki, H.; Mito, H.; Kakizaki, H. Orbital trapdoor fractures: Different clinical profiles between adult and paediatric patients. Br J Ophthalmol. 2018, 102, 885–891. [Google Scholar]
- Alinasab, B.; Qureshi, A.R.; Stjarne, P. Prospective study on ocular motility limitation due to orbital muscle entrapment or impingement associated with orbital wall fracture. Injury. 2017, 48, 1408–1416. [Google Scholar]
- Ellis, E., 3rd; Perez, D. An algorithm for the treatment of isolated zygomatico-orbital fractures. J Oral Maxillofac Surg. 2014, 72, 1975–1983. [Google Scholar] [PubMed]
- Møre og Romsdal County Municipality. Population Development in Moere and Romsdal. Accessed 21 March 2021. https://fylkesstatistikk.mrfylke.no/2019/demografi/ folketalsutvikling.
- Anda, S.; ElsÅs, T.; Harstad, H.K. The missing rectus: A CT observation from blow-out fracture of the orbital floor. J Comput Assist Tomogr. 1987, 11, 895–897. [Google Scholar] [PubMed]
- ElsÅs, T.; Anda, S. Orbital CT in the management of blow-out fractures of the orbital floor. Acta Ophthalmol. 1990, 68, 710–714. [Google Scholar]
- Nordgaard, J.O. Persistent sensory disturbances and diplopia following fractures of the zygoma. Arch Otolaryngol. 1976, 102, 80–82. [Google Scholar]
- Doving, M.; Galteland, P.; Eken, T.; et al. Dentoalveolar injuries, bicycling accidents and helmet use in patients referred to a Norwegian Trauma Centre: A 12-year prospective study. Dent Traumatol. 2021, 37, 240–246. [Google Scholar] [PubMed]
- Helgeland, E.; Dahle, I.M.; Leira, J.I.; Loro, L.L. Maxillofacial fractures surgically managed at Aalesund Hospital between 2002 and 2009. Craniomaxillofac Trauma Reconstr. 2015, 8, 321–325. [Google Scholar]
- Chi, M.J.; Ku, M.; Shin, K.H.; Baek, S. An analysis of 733 surgically treated blowout fractures. Ophthalmologica. Ophthalmologica. 20210, 224, 167–175. [Google Scholar]
- Zingg, M.; Laedrach, K.; Chen, J.; et al. Classification and treatment of zygomatic fractures: A review of 1, 025 cases. J Oral Maxillofac Surg. 1992, 50, 778–790. [Google Scholar]
- Schroeder, W.A., Jr. Maxillofacial trauma in two rural level II trauma centers. Mo Med. 1989, 86, 35–39. [Google Scholar]
- Ugboko, V.I.; Odusanya, S.A.; Fagade, O.O. Maxillofacial fractures in a semi-urban Nigerian teaching hospital. A review of 442 cases. Int J Oral Maxillofac Surg. 1998, 27, 286–289. [Google Scholar]
- Batista, A.M.; Marques, L.S.; Batista, A.E.; Falci, S.G.; Ramos-Jorge, M.L. Urban-rural differences in oral and maxillofacial trauma. Braz Oral Res. 2012, 26, 132–138. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Norwegian Central government agency. Marital Status, Distribution of Age and Gender in Counties and the Norwegian Population. 1986 2021. Accessed 21 March 2021. https://www.ssb.no/statbank/table/03031/.
- Manolidis, S.; Weeks, B.H.; Kirby, M.; Scarlett, M.; Hollier, L. Classification and surgical management of orbital fractures: Experience with 111 orbital reconstructions. J Craniofac Surg. 2002, 13, 726–737; discussion 738. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.R.; Singh, N.R.; Oztel, M.; Vangaveti, V.N.; Rahmel, B.B.; Ramalingam, L. Ophthalmological injuries associated with fractures of the orbitozygomaticomaxillary complex. Br J Oral Maxillofac Surg. 2018, 56, 221–226. [Google Scholar] [CrossRef]
- Blumer, M.; Kumalic, S.; Gander, T.; et al. Retrospective analysis of 471 surgically treated zygomaticomaxillary complex fractures. J Craniomaxillofac Surg. 2018, 46, 269–273. [Google Scholar] [CrossRef]
- van Hout, W.M.; Van Cann, E.M.; Koole, R.; Rosenberg, A.J. Surgical treatment of unilateral zygomaticomaxillary complex fractures: A 7-year observational study assessing treatment outcome in 153 cases. J Craniomaxillofac Surg. 2016, 44, 1859–1865. [Google Scholar] [CrossRef]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. Assault-related maxillofacial injuries: The results from the European Maxillofacial Trauma (EURMAT) multicenter and prospective collaboration. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015, 119, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; Jain, S.; Giacino, J.T.; et al. Risk of posttraumatic stress disorder and major depression in civilian patients after mild traumatic brain injury: A TRACK-TBI Study. JAMA Psychiatr. 2019, 76, 249–258. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, Y.J.; Seo, D.W.; et al. Incidence of intracranial injury in orbital wall fracture patients not classified as traumatic brain injury. Injury. 2018, 49, 963–968. [Google Scholar] [CrossRef]
- Ziegler, C.; Skaland, Ø. Maxillofacial fractures: Overview of epidemiology and treatment bases to patient clientele to St. Olavs University in Trondheim. Kirurgen. 2013, 4, 217–219. [Google Scholar]
- Bushman, B.J.; Cooper, H.M. Effects of alcohol on human aggression: An integrative research review. Psychol Bull. 1990, 107, 341–354. [Google Scholar] [CrossRef]
- Burnstine, M.A. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol. 2003, 14, 236–240. [Google Scholar]
- Kersten, R.C.; Vagefi, M.R.; Bartley, G.B. Orbital “blowout” fractures: Time for a new paradigm. Ophthalmology. 2018, 125, 796–798. [Google Scholar] [CrossRef]
- Scawn, R.L.; Lim, L.H.; Whipple, K.M.; et al. Outcomes of orbital blow-out fracture repair performed beyond 6 weeks after injury. Ophthalmic Plast Reconstr Surg. 2016, 32, 296–301. [Google Scholar]
- Jansen, J.; Dubois, L.; Maal, T.J.J.; et al. A nonsurgical approach with repeated orthoptic evaluation is justified for most blowout fractures. J Craniomaxillofac Surg. 2020, 48, 560–568. [Google Scholar]
- Kaukola, L.; Snall, J.; Roine, R.; Sintonen, H.; Thoren, H. Healthrelated quality of life of patients with zygomatic fracture. Med Oral Patol Oral Cir Bucal. 2017, 22, e636–e642. [Google Scholar]
- Alinasab, B.; Borstedt, K.J.; Rudstro¨ m, R.; et al. New algorithm for the management of orbital blowout fracture based on prospective study. Craniomaxillofac Trauma Reconstr. 2018, 11, 285–295. [Google Scholar]
- Kloss, F.R.; Stigler, R.G.; Brandsta¨tter, A.; et al. Complications related to midfacial fractures: Operative versus nonsurgical treatment. Int J Oral Maxillofac Surg. 2011, 40, 33–37. [Google Scholar]
© 2022 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).